

Association Between Centralization and Directional Preference
and Functional and Pain Outcomes in Patients With Neck PainThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Orthop Sports Phys Ther. 2014 (Feb); 44 (2): 68–75 ~ FULL TEXT
OPEN ACCESS Susan L. Edmond, PT, DSc, OCS, Guillermo Cutrone, PT, DSc, OCS, Cert MDT, FAAOMPT, Mark Werneke, PT, MS, Dip MDT, Jason Ward, MPT, MDT, Cert MDT, David Grigsby, MPT, MDT, Cert MDT, Jon Weinberg, PT, Dip MDT, William Oswald, DPT, Cert MDT, Dave Oliver, PT, Dip MDT, Troy McGill, PT, MS, Dip MDT, Dennis L. Hart, PT, PhD
Rutgers,
The State University of New Jersey,
Newark, NJ.STUDY DESIGN: Retrospective cohort.
OBJECTIVES: In subjects with neck pain, the present study aimed (1) to describe the prevalence of centralization (CEN), noncentralization (non-CEN), directional preference (DP), and no directional preference (no DP); (2) to determine if age, sex, fear-avoidance beliefs about physical activity, number of comorbid conditions, or symptom duration varies among subjects who demonstrate CEN versus non-CEN and DP versus no DP; and (3) to determine if CEN and/or DP are associated with changes in function and pain.
BACKGROUND: CEN and DP are prevalent among patients with low back pain and should be considered when determining treatment strategies and predicting outcomes; however, these findings are not well investigated in patients with neck pain.
METHODS: Three hundred four subjects contributed data. CEN and DP prevalence were calculated, as was the association between CEN and DP, and age, sex, number of comorbid conditions, fear-avoidance beliefs, and symptom duration. Multivariate models assessed whether CEN and DP predicted change in function and pain.
RESULTS: CEN and DP prevalence were 0.4 and 0.7, respectively. Younger subjects and those with fewer comorbid conditions were more likely to centralize; however, subjects who demonstrated DP were more likely to have acute symptoms. Subjects who centralized experienced, on average, a 3.6-point (95% confidence interval: -0.3, 7.4) improvement in function scores, whereas subjects with a DP averaged a 5.4-point (95% confidence interval: 0.8, 10.0) improvement. Neither CEN nor DP was associated with pain outcomes.
CONCLUSION: directional preference (DP) and, to a lesser extent, centralization (CEN) represent evaluation categories that are associated with improvements in functional outcomes.
From the FULL TEXT Article:
Introduction
Researchers have suggested that classifying patients into subgroups based on clinical characteristics and matching these subgroups to management strategies improve patient outcomes of physical therapy interventions. [5, 10, 26, 37] Classification of patients with neck pain has been recommended as a research priority. [5, 16] Nevertheless, there is insufficient information regarding how to classify these patients to inform physical therapy interventions that optimize outcomes.
Two examination procedures used to classify patients with spinal pain have been studied: centralization (CEN) and directional preference (DP). These examination procedures, which are derived from Mechanical Diagnosis and Therapy methods, inform clinical decisions and guide patient management. A classification method that combines CEN and DP principles, called the “patient response method,” has subsequently been proposed and recommended for use with patients with nonserious lumbar spine pain.36
A number of studies have demonstrated that in relation to low back pain, CEN and DP are of clinical value. CEN has been shown to predict decreased disability, [9, 28, 32–34, 37] return to work, [17, 23, 32, 35] and reduced pain. [9, 23, 32–34, 37] In several studies, prescribing exercises matched to the patient’s DP has improved low back pain outcomes. [2, 20–23] In 1 study (level 3 evidence), [8] the authors suggested that the patient response method delineated and improved the prediction of pain and function outcomes in patients with low back pain. [36]
CEN is operationally defined as spinal pain that is progressively abolished in a distal-to-proximal direction in response to therapeutic movement and positioning strategies, without consideration of intensity. [24, 26, 34, 37] DP is determined by whether spine and/or referred spinal pain located in the most distal body part decreases in intensity, abolishes, or centralizes, and/or whether subjects demonstrate an improvement in range of motion in response to a repeated-movement or positional-loading strategy. [25] Individuals not meeting these criteria are considered to have non-CEN and no DP, respectively.
The decision rules for judging CEN and DP are therefore similar but not synonymous. When CEN is present, DP must also be present. In contrast, DP might occur in the absence of CEN (eg, a patient’s lower-leg pain may decrease in intensity but not change in location with a specific repeated-movement or positional-loading strategy). CEN has also been shown to occur in the cervical spine. The prevalence of CEN, identified using the same operational definition described above, was reported to be 0.3, [24] 0.4, [6] and 0.2 [37] in prior studies. In the latter study, [37] prevalence decreased among more chronic and older subjects. The prevalence of DP among subjects with neck pain has not been reported in prior literature and remains unknown.
Several studies have addressed the predictive value of CEN, using the aforementioned definition, in subjects with cervical impairments. CEN has been shown to be predictive of reduced disability [33, 34] and pain. [33, 34, 37] In 1 of these studies, [37] however, CEN was not associated with changes in disability.
There are no studies that have examined the clinical effectiveness of DP or the patient response method in patients with cervical impairments. It is therefore unknown if subgrouping patients by pain responses using CEN and DP would improve the clinical interpretation of patient outcomes, as previously demonstrated in patients with lumbar impairments. [36]
Based on the lack of information regarding the prevalence and clinical utility of DP in patients with neck pain and previous recommendations for examining both CEN and DP pain responses when evaluating patients with low back pain, [36] a logical next step would be to investigate the clinical relevance of CEN and DP as classification criteria for the management of patients with cervical impairments. Therefore, the objectives of the present study were(1) to describe the prevalence of DP and no DP observed during the initial evaluation of patients with nonspecific neck pain whose symptoms centralize versus those whose symptoms do not centralize during their initial examination;
(2) to explore whether the prevalence of CEN and DP is affected by age, sex, fear-avoidance beliefs about physical activities, number of comorbid conditions, and symptom duration; and
(3) to determine if classifying patients at intake by DP or no DP, separately and in combination with CEN or non-CEN, is associated with changes in functional status and pain intensity at discharge from rehabilitation.We hypothesized that the prevalence of DP would be higher than the prevalence of CEN, and that both categorization strategies would be influenced by the subject’s age and symptom duration. In addition, we hypothesized that classification by DP and CEN would improve the ability to estimate prognosis for function and pain outcomes, as previously demonstrated in subjects with lumbar impairments. [36] The present study adds to the current literature by examining the prevalence and characteristics of CEN and DP, and the association between changes in functional outcomes and pain responses based on categorization by CEN and DP, among patients with neck pain.
Methods
This retrospective cohort study analyzed data from 328 subjects with neck pain who contributed data to Focus On Therapeutic Outcomes, Inc (Knoxville, TN), an international medical rehabilitation data-management company. [29, 30] Subjects represented a convenience sample of patients seen from July 2007 through December 2010 who had complete data and could be classified as having CEN or non-CEN at intake. Subjects with no pain or relevant referred symptoms immediately before repeatedmovement testing were excluded from our sample because they were not eligible for categorization as CEN or non-CEN.
These 328 subjects were classified and treated by 8 physical therapists (mean age, 43 years; range, 32–61 years; 8 male) who routinely utilized Mechanical Diagnosis and Therapy methods when treating patients with spinal pain. Four therapists had received additional postgraduate training and had credentials in Mechanical Diagnosis and Therapy. The average number of years of clinical experience was 16 (range, 9–41). Practice settings were diverse: 3 therapists were employed in hospital-based outpatient clinics, 4 therapists worked in 3 different private practices, and 1 therapist worked in 2 military orthopaedic outpatient clinics. Not all physical therapists collected data during the entire study period, as 3 physical therapists started data collection in the summer of 2009 and 4 were either transferred between clinics or had nonpatient responsibilities that interrupted data collection.
Subjects were classified as having CEN or non-CEN at intake. These categories have been recommended for routine use and operationally described for patients with lumbar impairments. [37] Briefly, patients were classified by quantifying changes in pain location observed during the initial physical therapy visit. At this time, they underwent a standard physical examination according to Mechanical Diagnosis and Therapy assessment methods, [26] without consideration of symptom intensity, using a body diagram and numeric overlay template. [37] This template has been previously described [9, 34] and shown to have acceptable reliability (χ = 0.9–1.0). [34] Subjects were instructed by the examiner to shade in all areas on a body diagram where they were experiencing spinal pain and referred symptoms. Body diagrams were completed in sitting before and after end-range, repeated neck movements and/or positioning techniques. The overlay template was placed over the body diagrams, which allowed quantification of the anatomical location of pain. To be classified as having CEN, a reduction of at least 1 pain location level after testing was required. If pain location increased or remained the same after repeated-movement tests, the pain response non-CEN was recorded. Subjects with no pain or relevant referred symptoms immediately before repeatedmovement testing were excluded from analyses because they were not eligible for categorization as CEN or non-CEN.
Subjects were also classified by demonstration of DP at intake. Specifically, DP was present if the subject’s most distal pain intensity decreased or abolished, or the subject’s cervical range of motion improved in response to repeated endrange movement tests or positionalloading strategies. [26] A subjective report of a specific preference for activities and movements, such as looking up (extension preference) or looking down (flexion preference), was used to guide the evaluation process, but objective confirmation during the initial evaluation was required for DP classification.
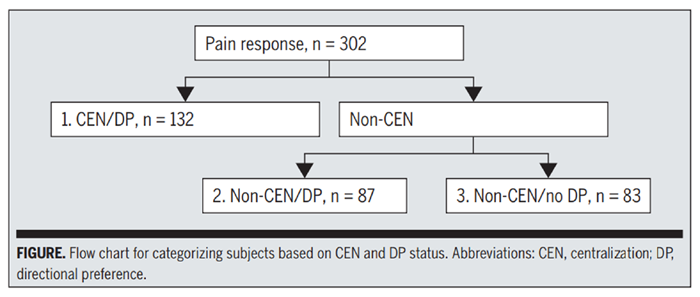
Figure 1 The information on CEN and DP was subsequently combined to determine patient response method categories as follows. A DP is always observed for patients whose symptoms centralize. Therefore, when categorizing subjects with DP based on whether they also centralize, a subject who centralized would be categorized as having CEN/DP. For subjects whose symptoms did not centralize, the examination continued to judge DP using additional criteria: if a DP was identified under these circumstances, then the patient was classified as having non-CEN/ DP. If no DP was identified, the subject was classified as having non-CEN/no DP (Figure).
Subjects classified as having DP irrespective of CEN were treated with specifically matched exercises and/or manual techniques based on the subject’s DP. [26] For example, if a subject’s symptoms centralized using extension movements or positioning in extension, the subject was prescribed retraction stretches (a lower cervical extension movement) and/or global neck extension stretches. For subjects who were categorized as non-CEN/ no DP, an individualized rehabilitation plan was developed at the discretion of the treating physical therapist. To improve adherence to their home exercise program and to enhance return to function with good pain-control techniques, all subjects, irrespective of categorization, were encouraged to become actively involved in their recovery process. No attempt was made to standardize care beyond these guidelines.
Prior to the initial examination, all subjects answered a series of questions, including patient demographics, fearavoidance beliefs about physical activity assessed with the Fear-Avoidance Beliefs Questionnaire physical activities subscale (FABQ-PA), symptom duration, functional status, and pain intensity. This information was used to create categories for age (18–44, 45–64, 65 or greater years), FABQ-PA score (less than 15/24, 15/24 or greater), [11] and symptom duration (calendar days between date of condition onset and date of initial evaluation, categorized as acute [0–21 days], subacute [22–90 days], and chronic [greater than 90 days]).
The subjects’ functional status was quantified at intake and discharge with the 36-item Functional Health Status (FHS-36) questionnaire, a physical function health status measure. The FHS-36 has been described in detail elsewhere. [15] Measures range from 0 (low functioning) to 100 (high functioning) on a linear metric. Data support the empirical item hierarchy, unidimensionality, reproducibility of item calibrations, and content and construct validity of the FHS-36. [13, 15] In addition, 80% of the FHS-36 measures had standard errors of 2 or 3 FHS36 units, or minimal detectable changes of 5 to 7 units. [15] Furthermore, the FHS-36 was reported to be sensitive to functional change during treatment for patients with cervical impairments (effect size, 0.9). [14]
Maximal pain intensity reported by the subject during the past 24 hours was assessed using an 11–point numeric pain rating scale, ranging from 0 (no pain) to 10 (worst imaginable pain). The numeric pain rating scale has been reported to be reliable and valid in this population, [7, 38] and has been shown to have a minimal detectable improvement of 4.1 points in subjects with cervical radiculopathy. [38] The Focus On Therapeutic Outcomes, Inc Institutional Review Board for the Protection of Human Subjects and the Rutgers, The State University of New Jersey Institutional Review Board approved this project. The requirement for informed consent was waived by both Institutional Review Boards.
Data Analysis
Data were analyzed using SAS Version 9.2 (SAS Institute Inc, Cary, NC). Descriptive statistics, the association between CEN and DP, as well as age, sex, number of comorbid conditions, FABQPA, and symptom duration were calculated. The association between each of these demographic measures and CEN and DP was evaluated using logistic regression analyses.
Linear regression models were used to evaluate the association between CEN and DP, and changes in function and pain levels. For these analyses, we calculated the prevalence of CEN and DP in 2 different ways. Subjects were first categorized based on whether they demonstrated CEN, then compared with those who demonstrated non-CEN. Similarly, subjects were categorized and compared based on whether they demonstrated DP or no DP. Subjects were also categorized by combinations of CEN and DP, based on the patient response method. Because, by definition, subjects who demonstrated CEN also had a DP, the category representing combinations of CEN and DP consisted of all subjects who demonstrated CEN. Subjects who did not demonstrate CEN were categorized based on whether they demonstrated a DP: non-CEN/DP or non-CEN/no DP (FIGURE). When comparing across these 3 categories, the reference group consisted of subjects who demonstrated CEN. An improvement in FHS-36 scores of at least 5 points [15] and an improvement in pain scores of at least 4.1 [38] were considered clinically relevant.
In relation to these analyses, we evaluated for the following potential confounders, which have been shown in prior studies to be associated with outcomes in subjects with neck pain:age [1, 4, 12];
sex [3, 31];
fear-avoidance beliefs about physical activities [18, 19, 24];
number of comorbid conditions, [12] such as cardiac disease, cancer, diabetes mellitus, and obesity;
and symptom duration. [1, 4]These variables were added to the linear regression models in which the exposure was CEN and/ or DP and the outcomes were functional status and pain, respectively. Age and comorbidity were entered as continuous variables, whereas FABQ-PA score (dichotomized as elevated or not elevated) and symptom duration (0–21 days, 22–90 days, greater than 90 days) were collapsed, so as to more closely simulate the manner in which this information is used to make clinical decisions. Adding age and symptom duration produced a meaningful change (greater than 10%) in the effect estimate, [27] and these 2 variables were therefore retained in the final multivariate model.
Results
Data were collected from a total of 328 subjects, of whom 24 did not contribute CEN data and 26 did not contribute DP data. Those who contributed CEN data (n = 304) and DP data (n = 302) did not differ significantly from those who did not in relation to age, FABQ-PA score, number of comorbidities, sex, symptom duration, and pain and function intake scores. Of the subjects who contributed CEN and DP data, 264 also contributed data on function and 191 on pain at intake and discharge. When comparing subjects who contributed complete data on pain (the outcome measure with the most missing data) to those who did not, no significant differences in age, FABQ-PA score, number of comorbidities, symptom duration, or pain or functional level intake scores were found. There was, however, a significant difference in sex, with males significantly more likely to have missing pain data than females (P<.01).

Table 1

Table 2 The prevalence of CEN and DP, both separately and together, is provided in Table 1. The prevalence of CEN and DP was 0.4 and 0.7, respectively. Among subjects with a DP, 84% exhibited a DP into extension. Because all subjects who demonstrated CEN also had a DP, when combining categorizations of CEN and DP, the largest group consisted of those who demonstrated both CEN and DP (prevalence, 0.4).
Descriptive statistics on subjects who contributed data on CEN and DP are provided in Table 2. Sex was not associated with CEN (P = .50; odds ratio [OR] = 1.18; 95% confidence interval [CI]: 0.73, 1.89) or DP (P = .53; OR = 0.85; 95% CI: 0.50, 1.43). Younger subjects (global P = .01; OR = 1.93; 95% CI: 0.92, 4.05 or OR = 2.91; 95% CI: 1.36, 6.21, depending on comparison) and subjects with fewer comorbidities (global P = .03; OR = 1.13; 95% CI: 0.58, 2.19 to OR = 2.47; 95% CI: 1.25, 4.85, depending on comparison) were significantly more likely to demonstrate CEN than older subjects and subjects with more comorbidities; however, age (global P = .32; OR = 1.08; 95% CI: 0.52, 2.25 or OR = 1.60; 95% CI: 0.74, 3.45, depending on comparison) and comorbidity (global P = .11; OR = 0.71; 95% CI: 0.36, 1.42 to OR = 2.49; 95% CI: 0.83, 7.44, depending on comparison) were not associated with DP. Conversely, symptom duration was not associated with CEN (P = .07; OR = 1.15; 95% CI: 0.67, 1.99 to OR = 1.99; 95% CI: 1.11, 3.56, depending on comparison); however, subjects who were more acute were more likely to demonstrate a DP (P<.01; OR = 1.93; 95% CI: 1.04, 3.58 or OR = 3.55; 95% CI: 1.63, 7.70, depending on comparison). Low FABQ-PA scores were more common among subjects who demonstrated CEN (P = .01; OR = 1.96; 95% CI: 1.18, 3.34) and those with a DP (P<.01; OR = 2.50; 95% CI: 1.47, 4.35).

Table 3

Table 4 Results from regression models analyzing the association between CEN and DP and changes in function and pain are presented in Tables 3 and 4, respectively. In the multivariate model examining change in functional status (Table 3), subjects who demonstrated CEN experienced, on average, a 3.6–point (95% CI: –0.3, 7.4) improvement in function scores, whereas subjects with a DP had an average improvement of 5.4 points (95% CI: 0.8, 10.0), thereby exceeding the minimal detectable change of 5 points.15 Compared with subjects classified as non-CEN/DP and non-CEN/no DP, subjects classified as CEN and DP reported a 1.8–point (95% CI: -2.5, 6.2) and a 6.2–point (95% CI: 1.3, 11.1) improvement in function, respectively. Irrespective of CEN or DP, most subjects (83%) demonstrated improvements in function that exceeded the minimal detectable change for the FHS-36 of 5 points. [15] Among subjects who demonstrated CEN, 86% exceeded this threshold, compared with 80% of subjects who did not centralize. In relation to DP, differences in functional outcomes were similar: 84% of those with a DP and 78% of those with no DP exceeded the minimal detectable change. In the multivariate models examining pain intensity (Table 4), among subjects who demonstrated CEN, DP, or any of the combinations of CEN and DP, there were no statistically significant differences, based on a P value of .05 or less, or clinically relevant changes, based on the minimal detectable improvement of 4.1 points. [38]
Discussion
The prevalence of centralization (CEN) among subjects with neck pain in the present study and that reported in 3 prior studies [6, 34, 37] ranges from 0.2 to 0.4. In our study, the prevalence of CEN was slightly higher (0.4), despite similar definitions of CEN. This variability in prevalence rates across studies is likely attributable to differences in the populations studied and the assessment methods used to measure CEN, as well as the exclusion from our analyses of those subjects who could not be classified. Ours is the first study to describe the prevalence of directional preference (DP) among subjects with neck pain. The difference in prevalence rates between CEN and DP was expected because of the additional criteria used to determine DP. At 0.7, determining DP has the potential to inform interventions for a substantial number of patients with neck pain. When pain responses were classified using the patient response method, the largest group was CEN and DP; however, a substantial percentage of patients (30%) were identified as having DP in the absence of CEN.
We hypothesized that when comparing CEN with non-CEN, and DP with no DP, there would be differences in age and symptom duration. In our study, age was associated with CEN but not with DP, whereas symptom duration was associated with DP but not with CEN. One other study has addressed the association between CEN and age and symptom duration in subjects with neck pain, [37] the findings of which, in relation to age, are consistent with ours. However, in that study, [37] subjects who demonstrated CEN were more likely to have acute symptoms than those with non-CEN. We also found that subjects with CEN had fewer comorbid conditions, but there were no differences in the number of comorbid conditions among subjects with a DP. Differences in age, number of comorbid conditions, and symptom duration between categories of CEN and DP provide additional support for the assertion that CEN and DP represent different clinical entities.
We also hypothesized that CEN and DP would predict changes in functional outcomes and pain levels. When combined with treatments consisting of matched exercises and manual techniques, in our study, DP compared with no DP and CEN compared with non-CEN/no DP predicted changes in function but not pain. None of the categories of CEN or DP, including the patient response method, predicted pain outcomes.
In 3 other studies, [33, 34, 37] investigators reported on the association between CEN and function and pain outcomes in patients with cervical impairments, using similar operational definitions for categorizing CEN. In 2 of these studies, [33, 34] results for subjects with low back pain were combined with those for subjects with neck pain. CEN was associated with a greater reduction in disability and pain in both studies. In the third study, [37] CEN was associated with a greater reduction in pain but not with functional levels for subjects with cervical impairments. These studies differ from ours, in which CEN was not associated with changes in function or pain, except in relation to functional changes, and only when CEN was compared with non-CEN/no DP.
This is the first study to address characteristics of CEN and DP in subjects with neck pain in the same study. In relation to achieving a minimal detectable improvement in function of at least 5 points, [15] our study results suggest that DP compared with no DP and CEN/DP compared with non-CEN/no DP predict functional outcomes. The association between functional outcomes and CEN/DP and non-CEN/ DP categories was not significant, suggesting that dividing DP into these 2 subcategories at intake may not be clinically useful. If a patient demonstrates a DP during the initial evaluation, further delineation for a CEN pain response does not appear useful to predict outcomes from physical therapy interventions. Therefore, evaluating patients with neck pain solely for DP as operationally defined in our study appears to be the best strategy of those addressed in this study to improve the interpretation of functional outcomes. Future studies are required to replicate our findings using larger sample sizes and long-term outcome assessments.
We excluded patients who had no pain or relevant referred symptoms immediately before repeated-movement testing. These subjects, although small in number (n = 22) compared to our original sample, might represent an important category of patients to identify for effective treatment strategies.
Because all subjects who demonstrated CEN or DP received matched treatments based on DP, our study results show that the categorizations of CEN and DP were associated with improvements in function when subjects with neck pain also received treatment based on DP. It is therefore possible that CEN and DP predict better functional outcomes irrespective of treatment. If research findings in the lumbar spine are generalizable to the cervical spine, this alternative explanation is unlikely, because studies have shown that matched treatments for patients who demonstrate DP in the lumbar spine are more effective than unmatched treatments. [2, 20–23]
The present study has several limitations, some pertaining to data acquisition. Despite the fact that therapists participating in data collection were instructed to collect and record data on all subjects with neck pain, 24 subjects with data on neck pain had missing CEN data, and 26 had missing DP data. Therefore, the subjects in the present study constitute a sample of convenience. Additionally, we were unable to control for all potential confounding variables, as they were not measured during data collection. Finally, we made a determination regarding the presence of DP by the end of the initial visit. This protocol was implemented despite recommendations [25] that subjects who describe a subjective movement preference but have no objective findings indicative of a DP should be classified as having a DP if the subjective findings are confirmed during subsequent visits. Identifying the specific criteria for classifying DP to identify treatment strategies and to optimize outcomes is a clinically relevant question, and is planned for future study.
Study limitations also included those related to study design. The FHS-36 questionnaire, which we used to measure function, is not a commonly recognized tool to measure function in patients with neck pain, and was not designed to measure the functional levels of specific body parts. Also, the generalizability of our study results might be impacted by the utilization of therapists with advanced training in Mechanical Diagnosis and Therapy methods to collect data and treat subjects. We believe, however, that therapists can be trained easily to perform the components of Mechanical Diagnosis and Therapy methods that were incorporated in this study, specifically the examination techniques that used standardized operational definitions of repeated-motion testing and treatment strategies involving repeated and progressive movements in a specific direction based on DP.
Despite these limitations, our study provides support for including DP in any treatment-based classification system for patients with neck pain, as it informs interventions that result in improved functional outcomes.
Conclusions
Directional preference (DP) is a prevalent evaluation category that, when combined with treatments consisting of matched exercises and manual techniques, can be used to predict changes in function, but not pain, in patients with neck pain.
Key Points
FINDINGS: DP is a prevalent examination finding that predicts improvement
in function when combined with treatments matched to the direction of the DP.IMPLICATIONS: The evaluation of DP should be a component of the physical
therapy examination of patients with neck pain and, when present, should
inform intervention strategies.CAUTION: Criteria for identifying and categorizing DP in patients with
neck pain need further refinement.
ACKNOWLEDGEMENTS:
A special acknowledgement is dedicated to our coauthor Dr Dennis Hart, who recently passed, for his guidance and expertise in the study’s design. Dennis, you will be greatly missed, and your contributions to our research group and research initiatives as well as to the physical therapy profession will be long lasting
References:
Boissonnault WG, Badke MB.
Influence of acuity on physical therapy outcomes for patients with cervical disorders.
Arch Phys Med Rehabil. 2008;89:81-86Browder DA, Childs JD, Cleland JA, Fritz JM.
Effectiveness of an extension-oriented treatment approach in a subgroup of subjects with low back pain: a randomized clinical trial.
Phys Ther. 2007;87:1608-1618Carstensen TB, Frostholm L, Oernboel E, et al.
Are there gender differences in coping with neck pain following acute whiplash trauma? A 12-month follow-up study.
Eur J Pain. 2012;16:49-60Childs JD, Cleland JA, Elliott JM, et al.
Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association.
J Orthop Sports Phys Ther. 2008;38:A1-A34Childs JD, Fritz JM, Piva SR, Whitman JM.
Proposal of a classification system for patients with neck pain.
J Orthop Sports Phys Ther. 2004;34:686-696; discussion 697-700Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL.
Development of a Clinical Prediction Rule for Guiding Treatment of a Subgroup of Patients With Neck Pain:
Use of Thoracic Spine Manipulation, Exercise, and Patient Education
Phys Ther. 2007 (Jan); 87 (1): 9–23Cleland JA, Childs JD, Whitman JM.
Psychometric properties of the Neck Disability Index and numeric pain rating scale in patients with mechanical neck pain.
Arch Phys Med Rehabil. 2008;89:69-74Delitto A, George SZ, Van Dillen LR, et al.
Low back pain.
J Orthop Sports Phys Ther. 2012;42:A1-A57Donelson R, Silva G, Murphy K.
Centralization phenomenon. Its usefulness in evaluating and treating referred pain.
Spine (Phila Pa 1976). 1990;15:211-213Fritz JM, Brennan GP.
Preliminary examination of a proposed treatment-based classification system for patients receiving physical therapy interventions for neck pain.
Phys Ther. 2007;87:513-524George SZ, Fritz JM, Childs JD.
Investigation of elevated fear-avoidance beliefs for patients with low back pain: a secondary analysis involving patients enrolled in physical therapy clinical trials.
J Orthop Sports Phys Ther. 2008;38:50-58Guzman J, Haldeman S, Carroll LJ, et al.
Clinical Practice Implications of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders:
From Concepts and Findings to Recommendations
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S199–S212Hart DL.
Assessment of unidimensionality of physical functioning in patients receiving therapy in acute, orthopedic outpatient centers.
J Outcome Meas. 2000;4:413-430.Hart DL, Connolly JB.
Pay-for-Performance for Physical Therapy and Occupational Therapy:
Medicare Part B Services.
Knoxville, TN: Focus On Therapeutic Outcomes, Inc; June 1, 2006.Hart DL, Wright BD.
Development of an index of physical functional health status in rehabilitation.
Arch Phys Med Rehabil. 2002;83:655-665.Hurwitz, EL, Carragee, EJ, van der Velde, G et al.
Treatment of Neck Pain: Noninvasive Interventions: Results of the Bone and Joint Decade
2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123–152Karas R, McIntosh G, Hall H, Wilson L, Melles T.
The relationship between nonorganic signs and centralization of symptoms in the prediction of return to work for patients with low back pain.
Phys Ther. 1997;77:354-360; discussion 361-369.Landers MR, Creger RV, Baker CV, Stutelberg KS.
The use of fear-avoidance beliefs and nonorganic signs in predicting prolonged disability in patients with neck pain.
Man Ther. 2008;13:239-248Lee KC, Chiu TT, Lam TH.
The role of fear-avoidance beliefs in patients with neck pain: relationships with current and future disability and work capacity.
Clin Rehabil. 2007;21:812-821Long A, Donelson R, Fung T.
Does it matter which exercise? A randomized control trial of exercise for low back pain.
Spine (Phila Pa 1976). 2004;29:2593-2602.Long A, May S, Fung T.
The comparative prognostic value of directional preference and centralization: a useful tool for front-line clinicians?
J Man Manip Ther. 2008;16:248-254.Long A, May S, Fung T.
Specific directional exercises for patients with low back pain: a case series.
Physiother Can. 2008;60:307-Long AL.
The centralization phenomenon. Its usefulness as a predictor or outcome in conservative treatment of chronic low back pain (a pilot study).
Spine (Phila Pa 1976). 1995;20:2513-2520; discussion 2521.May S, Aina A.
Centralization and directional preference: a systematic review.
Man Ther. 2012;17:497-506McKenzie R, May S.
The Cervical and Thoracic Spine: Mechanical Diagnosis and Therapy. 2nd ed.
Waikanae, New Zealand: Spinal Publications; 2006.McKenzie R, May S.
The Lumbar Spine: Mechanical Diagnosis and Therapy. 2nd ed.
Waikanae, New Zealand: Spinal Publications; 2003.Rothman KJ, Greenland S.
Modern Epidemiology. 2nd ed.
Philadelphia, PA: Lippincott-Raven; 1998.Sufka A, Hauger B, Trenary M, et al.
Centralization of low back pain and perceived functional outcome.
J Orthop Sports Phys Ther. 1998;27:205-212Swinkels IC, Hart DL, Deutscher D, et al.
Comparing patient characteristics and treatment processes in patients receiving physical therapy in the United States, Israel and the Netherlands: cross sectional analyses of data from three clinical databases.
BMC Health Serv Res. 2008;8:163Swinkels IC, van den Ende CH, de Bakker D, et al.
Clinical databases in physical therapy.
Physiother Theory Pract. 2007;23:153-Wang YC, Hart DL, Stratford PW, Mioduski JE.
Clinical interpretation of a lower-extremity functional scale-derived computerized adaptive test.
Phys Ther. 2009;89:957-968Werneke M, Hart DL.
Centralization phenomenon as a prognostic factor for chronic low back pain and disability.
Spine (Phila Pa 1976). 2001;26:758-764; discussion 765.Werneke M, Hart DL.
Discriminant validity and relative precision for classifying patients with nonspecific neck and back pain by anatomic pain patterns.
Spine (Phila Pa 1976). 2003;28:161-166Werneke M, Hart DL, Cook D.
A descriptive study of the centralization phenomenon. A prospective analysis.
Spine (Phila Pa 1976). 1999;24:676-683.Werneke MW, Hart DL.
Categorizing patients with occupational low back pain by use of the Quebec Task Force Classification system versus pain pattern classification procedures: discriminant and predictive validity.
Phys Ther. 2004;84:243-254.Werneke MW, Hart DL, Cutrone G, et al.
Association between directional preference and centralization in patients with low back pain.
J Orthop Sports Phys Ther. 2011;41:22-31Werneke MW, Hart DL, Resnik L, Stratford PW, Reyes A.
Centralization: prevalence and effect on treatment outcomes using a standardized operational definition and measurement method.
J Orthop Sports Phys Ther. 2008;38:116-125Young IA, Cleland JA, Michener LA, Brown C.
Reliability, construct validity, and responsiveness of the Neck Disability Index, Patient-Specific Functional Scale, and Numeric Pain Rating Scale in patients with cervical radiculopathy.
Am J Phys Med Rehabil. 2010;89:831-839.
Return to McKENZIE METHOD
Return to CHRONIC NECK PAIN
Since 6-02-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |