

Manual and Instrument Applied Cervical Manipulation
for Mechanical Neck Pain: A Randomized
Controlled TrialThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther. 2016 (Jun); 35 (5): 319–329 ~ FULL TEXT
OPEN ACCESS Lindsay M Gorrell, MChiro, MRes, PhD, Kenneth Beath,
Roger M Engel, DO, DC, PhD
Sessional Academic,
Department of Chiropractic,
Macquarie University,
Sydney, NSW, Australia.
Thanks to JMPT for permission to reproduce this Open Access article! OBJECTIVE: The purpose of this study was to compare the effects of 2 different cervical manipulation techniques for mechanical neck pain (MNP).
METHODS: Participants with mechanical neck pain (MNP) of at least 1 month's duration (n = 65) were randomly allocated to 3 groups:(1) stretching (control)
(2) stretching plus manually applied manipulation (MAM), and
(3) stretching plus instrument-applied manipulation (IAM).MAM consisted of a single high-velocity, low-amplitude cervical chiropractic manipulation, whereas IAM involved the application of a single cervical manipulation using an (Activator IV) adjusting instrument. Preintervention and postintervention measurements were taken of all outcomes measures. Pain was the primary outcome and was measured using visual analogue scale and pressure pain thresholds. Secondary outcomes included cervical range of motion, hand grip-strength, and wrist blood pressure. Follow-up subjective pain scores were obtained via telephone text message 7 days postintervention.
RESULTS: Subjective pain scores decreased at 7–day follow-up in the manually applied manipulation (MAM) group compared with control (P = .015). Cervical rotation bilaterally (ipsilateral: P = .002; contralateral: P = .015) and lateral flexion on the contralateral side to manipulation (P = .001) increased following MAM. Hand grip-strength on the contralateral side to manipulation (P = .013) increased following IAM. No moderate or severe adverse events were reported. Mild adverse events were reported on 6 occasions (control, 4; MAM, 1; IAM, 1).
CONCLUSION: This study demonstrates that a single cervical manipulation is capable of producing immediate and short-term benefits for mechanical neck pain (MNP). The study also demonstrates that not all manipulative techniques have the same effect and that the differences may be mediated by neurological or biomechanical factors inherent to each technique.
KEYWORDS: Cervical Vertebrae; Chiropractic; Manipulation; Neck Pain; Randomized Controlled Trial; Spinal
From the Full-Text Article:
Introduction
The annual prevalence of neck pain is estimated to range from 30% to 50%, with reports of lifetime and point prevalence values approaching those of low back pain. [1–6] Mechanical neck pain (MNP) is defined as nonspecific pain of nonpathological origin occurring in the cervical spine. [7, 8] A common approach to managing MNP includes cervical spine manipulation. [8, 9] Although high-velocity, low-amplitude (HVLA) cervical manipulation has been shown to be effective for treating MNP [9, 10] and is included in several clinical practice guidelines, [11–13] the optimal manipulative technique for treating this condition remains ambiguous. [14] HVLA manipulation can be delivered manually (manually applied manipulation [MAM]) or by instrument (instrument-applied manipulation [IAM]). However, there is no clear evidence to support one approach over the other. [9, 15–23] MAM is commonly used and involves the manual application of a force aimed at moving a joint beyond its physiological range of motion (ROM) without exceeding the anatomical limit. [16, 24] By contrast, the delivery of a manipulative force in an IAM does not rely on moving a joint beyond its physiological ROM to achieve an effect. [25]
This difference in approach has not been adequately reflected in reports of change following spinal manipulation. [26–30] Three studies comparing the effectiveness of MAM and IAM for the treatment of MNP reported both approaches to be equally effective. [31–33] However, the quality of these studies was poor with inadequate sample sizes, lack of a control group, and heterogeneous methodologies, detracting from the validity and generalizability of the results. [34] This is in contrast to the findings of the largest study to date comparing MAM, IAM, and usual care for the treatment of low back pain which reported that, in a population of 107 participants, MAM provided greater short-term reductions in self-reported disability compared with IAM and usual care. [35]
Remote effects following HVLA spinal manipulation, that is, effects which occur in tissues not directly related to the area where the intervention was applied, have also been reported in the literature. [36, 37] The hypothesis that there is a connection between the response of the autonomic nervous system and pain perception following spinal manipulation has been investigated by a number of researchers. [36, 38, 39] Reports of changes in skin conductance, respiratory rate, blood pressure, and heart rate in healthy populations following mobilization or manipulation of specific areas of the spine support this hypothesis. [39, 40]
In addition to responses generated by the autonomic nervous system, cervical spine manipulation has also been associated with changes in the somatic nervous system. [41, 42] Studies investigating the effect of cervical manipulation on lateral epicondylalgia have described an increase in hand grip-strength, [43–45] whereas other studies have reported excitatory effects on motor activity. [46–48]
The aim of this study was to determine whether a single application of HVLA cervical manipulation (MAM or IAM) affected MNP and, if so, whether the effect was the same for both types of manipulation.
Methods
The study was designed as a randomized controlled trial with 1 control and 2 intervention groups. Volunteers aged 18 to 35 years with a history of MNP of greater than 1 month were screened for contraindications to cervical spinal manipulation. Contraindications included history of a connective tissue disorder, cervical pain which was not due to mechanical dysfunction or did not originate from the lower cervical spine, current use of anticoagulant therapy, history of recent surgery and/or neck trauma, facial or intraoral anesthesia or paresthesia, visual disturbances, dizziness, and/or vertigo. In addition to this, a person was excluded if they were pregnant or had received cervical mobilization or manipulation within the preceding 1 month. A volunteer who met the inclusion criteria, passed the screening stage, and provided written consent to participate was enrolled in the trial and randomly allocated to 1 of 3 groups.
Allocation was achieved using a computer-generated random number sequence created by an administrative officer not otherwise associated with the trial. Group 1 (control) received a standardized active muscle stretching routine (S); group 2 (MAM) received the same active muscle stretching routine (S) plus a single MAM; and group 3 (IAM) received the same active muscle stretching routine (S) plus a single IAM. The trial was conducted at Macquarie University’s Chiropractic Outpatient and Research Clinic in Sydney, Australia, between August and September 2014. The trial was approved by Macquarie University’s Human Research Ethics Committee (approval no.: 5201400281) and registered with the Australian and New Zealand Clinical Trials Registry (ACTRN: 12614000804684).
All outcome assessments were performed by a single assessor. The primary outcome assessment was neck pain evaluated using subjective measures: visual analogue scale (VAS), numerical pain rating scale (NPRS), and pressure point threshold (PPT). Secondary outcome measures included cervical ROM, hand grip-strength, and wrist blood pressure. Subjective pain levels (VAS) were recorded first, followed by wrist blood pressure, hand grip-strength, PPT, and finally cervical ROM. This order was selected to minimize the effect of one measurement on any other. All outcome measurements were taken immediately preintervention and postintervention. Subjective pain levels (NPRS) were also measured 7 days postintervention by telephone text message. The NPRS used 7 days postintervention was similar to the VAS used preintervention and immediately postintervention.
All MAMs were administered by a single practitioner with 30 years clinical experience in manual manipulation, whereas all IAMs were administered by a different practitioner with 29 years of clinical experience in instrument manipulation.
All participants performed the same stretching routine (S) which involved flexion, extension, bilateral lateral flexion, and rotation of the cervical spine to end-range, with each position maintained for 30 seconds and repeated 3 times. The use of stretching as a standardized active control ensured that each participant had the potential for improvement, as the benefit of exercise for MNP has been previously reported in the literature. [8, 14, 49] Each participant in the MAM and IAM groups received a single application of the relevant manipulation. The choice of which level of the cervical spine to address was at the discretion of the clinician following static palpation. To maintain consistency in blinding, all participants were informed that each intervention was a recommended treatment for MNP. [9, 14]
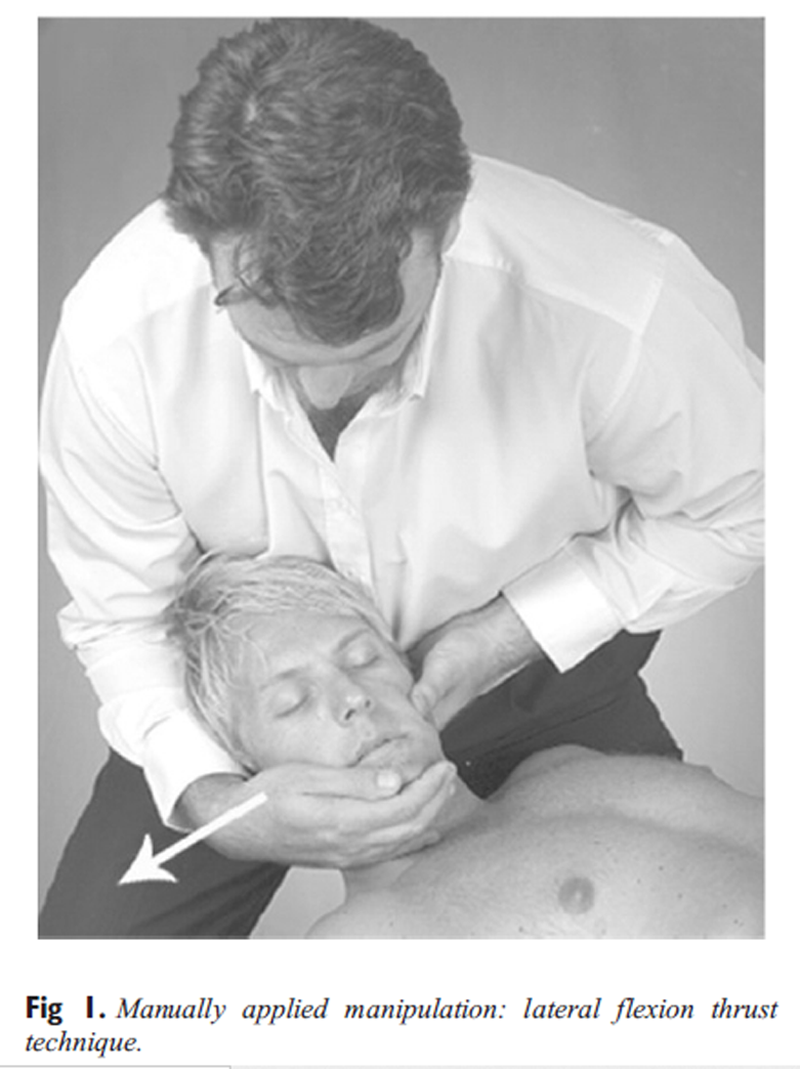
Figure 1
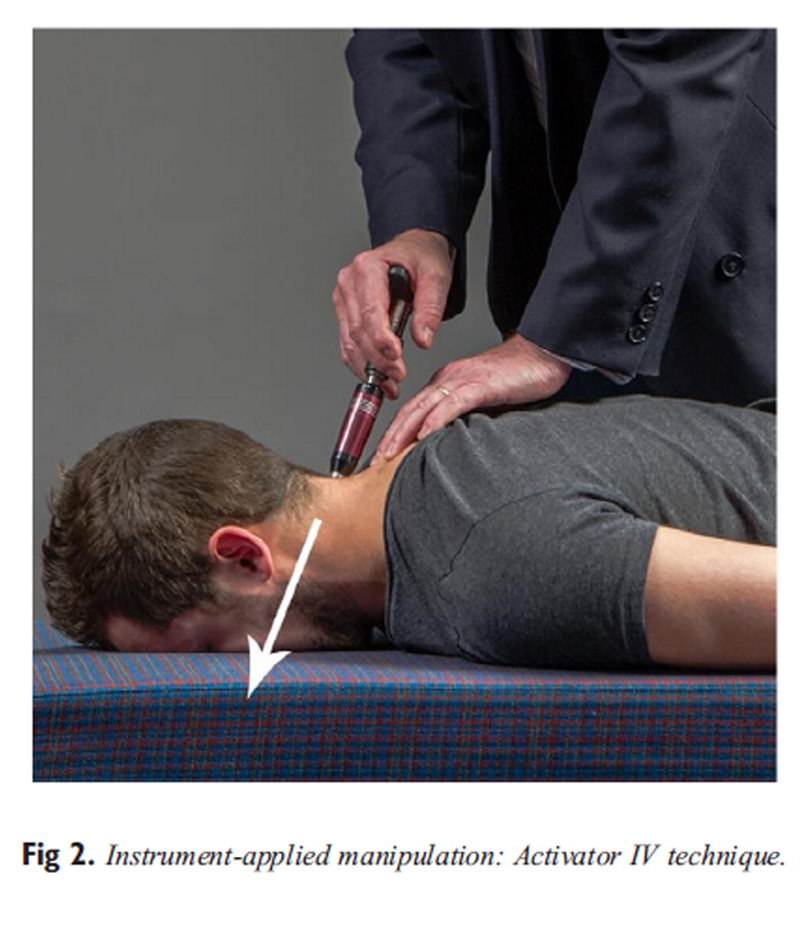
Figure 2 All MAMs were administered using the same technique — a lateral flexion thrust manipulation (Figure 1). In this technique, the side contacted by the hand delivering the thrust will be referred to as the ipsilateral side, whereas the opposite side is referred to as the contralateral side. [50, 51] All IAMs were administered using an Activator IV instrument on a setting of “2” with the manipulative force delivered to the pedicle-lamina junction of the involved segment in an anterior, superior, and slightly medial line of drive (Figure 2). In this trial, the instrument was used only as a biomechanical device, and no Activator Methods protocols were used. [52]
Subjective Pain Levels
Participants were asked to record their neck pain using an 11–point VAS immediately preintervention and postintervention. In addition to this, a follow-up telephone text message was sent 7 days postintervention asking the participant to report their neck pain on that day. This measure used the NPRS to rate the pain following the standard question, “Out of 10, how is your neck pain today?” The minimum clinically importance difference (MCID) is 1.7cm [53] for VAS and 1.3 points54 for NRPS.
Pressure Pain Threshold
Pressure pain threshold was measured using a JTech Medical Commander Algometer (Salt Lake City, UT). The instrument was placed over the spinous process of the involved segment using a 0.5–cm2 tip, and participants were instructed to notify the examiner the moment the sensation of pressure changed to discomfort or pain. The test was then stopped and the results recorded. [55] This procedure was performed 3 times and included a 10–second rest between tests, with the recorded score being the average of the 3 scores. The MCID for PPT is 1.77 kg/cm2. [56]
Cervical ROM
Cervical ROM was measured using a JTech Medical Dualer IQ Pro Digital Dual Inclinometer (Salt Lake City, UT). All measurements were taken in the “dynamic dual mode” [57] which involved a participant moving their neck to end-range. [58] Each of the 6 movement directions (flexion, extension, left and right lateral flexion, left and right rotation) were performed 3 times, with the average of these scores recorded as the final measurement for that movement. The clinically detectable change for each of these cervical movements has been reported in the literature previously. [58, 59]
Hand Grip-Strength
Hand grip-strength was measured using a JTech Medical Commander Grip (Salt Lake City, UT) dynamometer. Maximum isometric grip contraction was performed 3 times on each hand, alternating between hands to minimize performance fatigue. The average of the 3 measurements was recorded as the final grip-strength score for each hand. The clinically detectable change for hand grip-strength is 6 kg. [60]
Wrist Blood Pressure
Wrist blood pressure was measured using a digital Sigma Medical Heine Memotronic PC2 electronic sphygmomanometer (Herrsching, Germany). Blood pressure was taken 3 times, with the average of these scores recorded as the final measurement. The MCID for change in blood pressure is yet to be established in the literature because it can differ significantly between patients. [61]
Adverse Events
Adverse events were recorded immediately postintervention and as part of the 7–day follow-up telephone text message.
Statistical Analysis
Calculation of the minimum sample size was based on detecting a difference of 0.4 units in PPT levels, a standard deviation of 0.4, comparison of 2 means, an α of .05, and power (β) of 80%.62 These assumptions generated a minimum sample size of 21 participants per group and a total cohort size of 63. A significance level of .05 was used to assess the primary outcome measures, with a Bonferroni correction applied to correct for multiple tests for the 3 primary outcomes giving an individual significance level of .0167. No correction was applied for secondary outcomes. Data were checked for normality before statistical analysis. Baseline variables were compared between groups using one-way analysis of variance for continuous data except for VAS, Kruskal-Wallis for VAS and Pearson χ2 test for categorical data. An analysis of covariance with a factor for group and preintervention values as a covariate was performed to determine the effect of intervention on each outcome measure. For outcome measures with a significant between-group difference, Tukey honestly significantly difference test was performed to correct for multiple comparisons between groups. These statistical analyses were performed using Minitab17 software.
Results
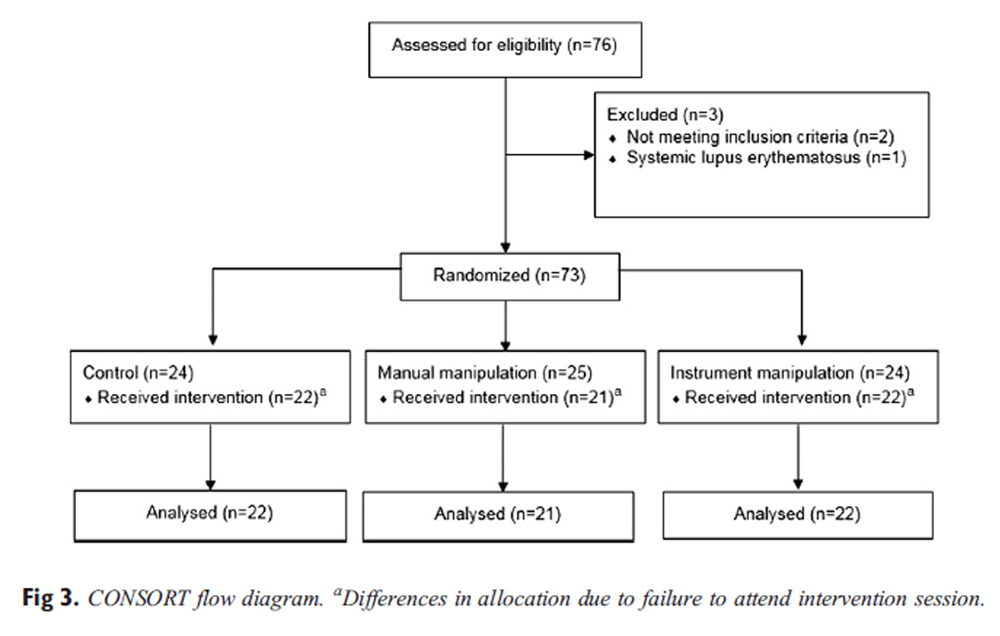
Figure 3

Table 1

Table 2 Seventy-six volunteers were assessed for eligibility in the trial, with 3 failing to meet the screening criteria and subsequently being excluded (Figure 3). Eight participants did not attend the initial assessment session, leaving baseline data from 65 participants (Table 1). Table 2 describes change scores for the trial at each time point.
Subjective Pain Levels (VAS and NPRS)
There was no immediate change in subjective pain levels for any of the 3 groups (F2,62 = 3.13, P = .051). However, there was a between-group difference in subjective pain levels at 7–day follow-up (F2,62 = 4.47, P = .015) for the MAM group which reported a decrease in pain compared with control of –1.40 points (P = .015; 95% confidence interval [CI], –2.52 to –0.27). There were no other between-group differences for subjective pain levels at 7–day follow-up: IAM to control (P = .235), and MAM to IAM (P = .367).
Pressure Pain Threshold
There were no between-group differences for PPT (F2,62 = 1.68, P = .195).
Cervical ROM
There was an immediate change in rotation bilaterally (ipsilateral: F1,41 = 11.17, P = .002; contralateral: F1,41 = 6.44, P = .015). This change was an increase for the MAM group of 10.35° on the ipsilateral side (P = .002; 95% CI, –16.60 to –4.09) and 6.32° on the contralateral side to manipulation (P = .015; 95% CI, –11.36 to –1.29) compared with the IAM group.
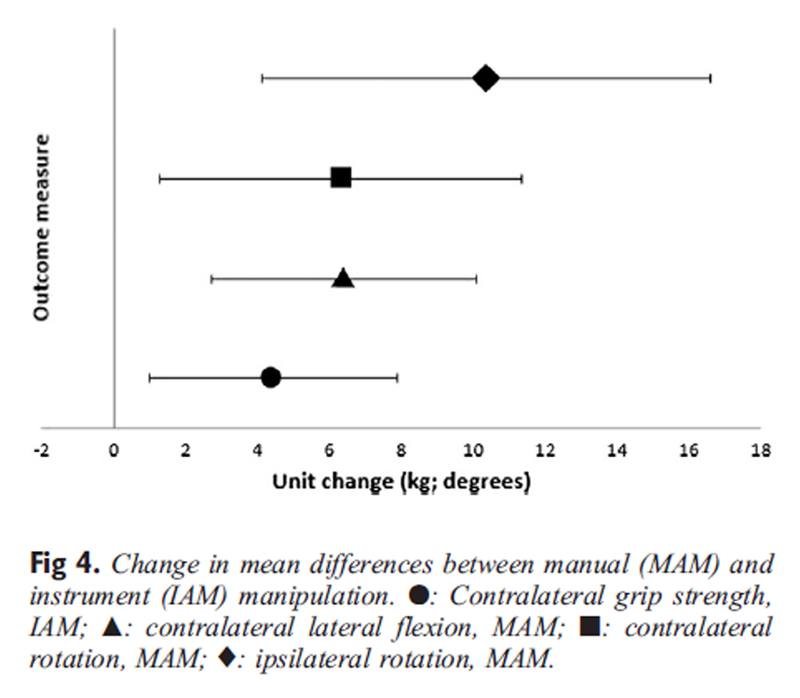
Figure 4 There was a between-group difference for lateral flexion on the contralateral side to manipulation (F1,41 = 12.44, P = .001) for the MAM group of 6.40° (P = .001; 95% CI, –10.06 to –2.73) compared with the IAM group (Figure 4). There was no difference in lateral flexion between the MAM and IAM groups on the ipsilateral side to manipulation (F1,41 = 3.73, P = .060). There were no between-group differences reported for flexion (F2,62 = 0.37, P = .691) or extension (F2,62 = 1.85, P = .166).
Hand Grip-Strength
There was a between-group difference reported in hand grip-strength on the contralateral side to manipulation (F1,41 = 6.77, P = .013). This difference was an increase of 4.43 kg (P = .013; 95% CI, 0.99–7.86) in the IAM group compared with MAM (Fig 4). There was no between-group difference on the ipsilateral side to manipulation (F1,41 = 0.87, P = .357).
Wrist Blood Pressure
There were no changes in wrist blood pressure reported in this trial: systole (F2,62 = 2.44, P = .096) or diastole (F2,62 = 2.53, P = .088).
Adverse Events
There were no moderate or severe adverse events following any of the interventions. There were 6 mild adverse events reported at 7–day follow-up: 4 in the control group and 1 each in the MAM and IAM groups. These reports included stiffness, mild soreness, and pain during neck movement. Two participants in the IAM group reported reactions which, although not classified as adverse events, have been included here for completeness. These reactions were “feeling unbalanced due to manipulation of only one side of the neck” and “increased clicking in the cervical spine following manipulation.”
Discussion
The findings reported in this study show that a single application of cervical manipulation increases cervical ROM and decreases subjective pain levels in people with MNP. The study also shows that cervical manipulation produces remote effects. However, these effects are noticeably different for each type of manipulation. MAM produced immediate increases in rotation bilaterally and lateral flexion on the contralateral side to manipulation compared with IAM and a decrease in subjective pain levels 7 days postintervention when compared with control. IAM did not produce equivalent changes. Our results support the findings of a recent large study comparing MAM, IAM, and usual care in a cohort with low back pain which reported greater reductions in short-term self-reported disability and pain scores following MAM. [35] However, our results contradict the findings from other smaller studies which reported that MAM and IAM were equally effective in the treatment of MNP. [31–33] In the absence of a control group, it is possible that performance bias may have affected the results from these smaller studies. [36, 63–66] In addition, given that these studies reported on small sample sizes (14–47 participants), it is possible that a series of type II errors may have occurred, resulting in incorrect acceptance of the hypothesis that there is no difference between MAM and IAM. [67, 68] Given the quality of previous studies investigating manipulation for MNP, we will compare our results with studies of higher quality that investigated the effects of spinal mobilization because the forces used in those studies are similar to those used in our study. [69, 70]
Subjective Pain Levels (VAS and NPRS)
Our results are consistent with previous reports that MAM is more effective than mobilization in reducing subjective pain levels for MNP. [10, 30, 71, 72] As in our study, time appears to be a factor, with these studies reporting improvements at 2,72 4,10 and 771 days postintervention. In contrast, Martinez-Segura et al [30] reported an immediate decrease in subjective pain levels following a single cervical HVLA manipulation compared with mobilization in participants with MNP.
Our results contradict the findings of 2 studies comparing the effectiveness of cervical MAM with mobilization in patients with neck pain. [15, 73] However, this contradiction may be explained by the heterogeneous nature of their designs compared with our study. In the first trial, patients with radiculopathy were included as well as treatment to the thoracic spine, [15] whereas in the second trial, treatment to the thoracic and lumbar regions was included, randomization only occurred after several treatments, and the type of MAM and mobilization procedures was not reported. [73]
As none of the groups in the current study reported changes that were above the MCID for either VAS or NPRS, the results should not strictly be interpreted as clinically significant. As our cohort displayed relatively low pain levels at baseline, it is possible that a “floor effect” may have contributed to this lack of clinical significance. [74, 75] This floor effect may have been avoided by excluding participants who reported a baseline pain level less than 3 of 10. [28] Furthermore, interpretation of subjective pain scores can vary between individuals. For example, some patients interpret the minimum end point on the scale (labeled “0”) as indicative of “normal” or “manageable” pain. These patients often exclude the lower half of the rating scale, considering such levels of pain as outside their experience. Interpretation of subjective pain scales in this way can result in distorted scores because these patients only use part of the range, that is, 6–10, leading some authors to question the validity of subjective pain scales. [76–80]
In addition, based on the change scores reported immediately postintervention, it is hypothesized that the MCID may have been achieved at 7–day follow-up had a second manipulation been applied such as would usually occur in clinical practice.
Pressure Pain Threshold
Our finding of no between-group differences in PPT immediately postintervention is consistent with results from other studies that found no differences in PPT following high -and low-force mobilization in people with chronic, nonspecific neck pain [10] or whiplash. [81] Furthermore, none of the reported changes in the current trial were above the MCID for PPT. This finding is also consistent with Martinez-Segura et al [30] who reported nonsignificant increases in PPT following both cervical and thoracic manipulation for MNP. As PPT is a self-reported measure of pain, it is possible that our results may have been influenced by participants who had varying pain thresholds, specifically where a sensitive participant may have reported pain earlier than a more stoic participant. In addition, the control group was not blinded, and it is possible that participants in this group may have had a falsely lowered pain threshold.
Cervical ROM
The immediate increase in cervical rotation and lateral flexion following MAM reported in this study contradicts findings from other studies where no change to cervical ROM was reported following cervical mobilization or manipulation in populations with MNP. [10, 30] Furthermore, 2 recent systematic reviews concluded that there was uncertainty as to whether spinal manipulation improved cervical ROM. [82, 83]
In explaining our findings, consideration must be given to the fact that we used an MAM technique which facilitated distraction and displacement of the cervical spine. As preload manipulative forces are capable of eliciting changes in paraspinal muscle activation, [23, 84–86] it is suggested that the chosen technique exerted a preload force that achieved this activation, thereby facilitating a change in cervical ROM. This may explain the lack of change to cervical ROM seen subsequent to IAM, as different preload forces are generated using this technique.
Hand Grip-Strength
This is the first study to report immediate increases in hand grip-strength following IAM and contradicts other reports of changes following manipulation. [41, 42, 44, 45] Notwithstanding this, the finding of increased hand grip-strength on the contralateral side to manipulation is supported by Humphries et al [42] who reported increases in a population of asymptomatic basketball players. Furthermore, other authors have reported an immediate increase in hand grip-strength on both the affected side (ipsilateral) [44, 45] as well as bilaterally [41] following cervical MAM. The current findings are congruent with previous studies reporting excitatory effects on motor activity subsequent to spinal manipulation. [46–48, 87] More specifically, Dunning and Rushton [88] demonstrated that a single cervical manipulation can elicit an immediate increase in resting electromyographic activity in an area distal and not directly connected to the cervical spine. Other studies investigating the effects of cervical manipulation on lateral epicondylalgia have described both sensory and motor changes including an increased hand grip-strength following manipulation. [44, 45, 89] It has also been reported that multiple sessions of cervical manipulation may produce a cumulative effect on hand grip-strength, supporting the concept of a dose-response mechanism. [41, 44] As the increases in hand grip-strength reported in this trial were not above the MCID, any interpretation of their clinical significance should be restrained.
Wrist Blood Pressure
Previous studies have reported mixed results when measuring changes in blood pressure following spinal manipulation. [36, 90–92] Two systematic reviews reflect this observation, with one reporting that spinal manipulation produced a nonsignificant, minimal clinical effect on blood pressure, [93] whereas the other reported strong evidence for a positive change in blood pressure in healthy populations following manipulation. [40] To the authors’ best knowledge, this is the first study to investigate the effect of cervical manipulation on blood pressure in a population with MNP.
Adverse Events
Although the absence of any moderate or severe adverse events following 21 MAMs and 22 IAMs in a young population with MNP is welcomed, it should not be interpreted as an unequivocal endorsement of the safety of cervical manipulation. Reports of this kind are evidence of the “relative” safety of cervical manipulation and add to the body of evidence in the field. Furthermore, reporting the rate of minor adverse events (4.7% in the current study) promotes evidence-based discussion on the risks associated with this type of intervention.
Limitations
There are a number of limitations which should be considered when interpreting the results of this study. Firstly, the trial was designed as a “proof of concept” with the choice to use a single manipulation as the intervention driven by the desire to directly measure dose-response, an approach previously recommended by several authors. [84–86, 94] The results should therefore not be interpreted as indicative of clinical practice. Secondly, as participants in the trial were young with low baseline levels of pain, the results may not be generalizable to older patients or those with other cervical complaints such as neck trauma or radiculopathy. Thirdly, we attempted to reduce interoperator inconsistencies by using a single clinician for each type of manipulation; therefore, it is possible that similar studies using multiple practitioners may have difficulty replicating our results. Fourthly, the reliability and validity of VAS [53, 75] and NPRS [95] have been reported separately; however, this does not extend to inclusion in the same analysis. To maintain consistency across measures, the average of a multiple-question NPRS could have been used at all time points to report subjective pain levels. In addition, it is possible that as numerous multiple comparisons were performed, a type I error may have occurred. [96] Furthermore, as there was no interexaminer validation of the diagnosis, it is also possible that the initial diagnosis may have been incorrect and therefore influenced the results. Notwithstanding, a recent study supports the use of a targeted physical examination involving pain provocation with manual palpation for accurate diagnosis of MNP. [97]
Conclusion
This study demonstrates that a single cervical manipulation is capable of producing both immediate and short-term benefits for MNP. The study also demonstrates that not all manipulative techniques have the same effect. The results reported in this study are consistent with the hypothesis that the biomechanical characteristics of different spinal manipulation techniques may be responsible for varying clinical effects. However, the results are not definitive, and further research investigating the nature of these changes is warranted.
Practical Applications
A single application of MAM increased rotation and lateral flexion movements
and decreased pain levels in people with mechanical neck pain.A single application of IAM increased hand grip-strength on the contralateral
side to manipulation.There was no change in PPT following either type of manipulation.
Following 21 MAMs and 22 IAMs, there were no moderate or severe adverse events
and 2 mild adverse events reported in this trial.
Funding Sources and Potential Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): L.G., R.E.
Design (planned the methods to generate the results): L.G., R.E.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): R.E.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): L.G.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): L.G., K.B., R.E.
Literature search (performed the literature search): L.G.
Writing (responsible for writing a substantive part of the manuscript): L.G., R.E.
Critical review (revised manuscript for intellectual content; this does not relate to spelling and grammar checking): L.G., K.B., R.E.
Other (list other specific novel contributions): R.E.—provided all MAM in trial.
Acknowledgements
The authors thank Mr Tim Wade-Ferrell and Mr Aron Downie for their assistance during the project.
References:
Fejer R Kyvik KO Hartvigsen J
The prevalence of neck pain in the world population:
a systematic critical review of the literature.
Eur Spine J. 2006; 15: 834-848Hogg-JohnsonS, van derVelde G, Carroll LJ, HolmLW, Cassidy JD,GuzmanJ, et al.
The Burden and Determinants of Neck Pain in the General Population:
Results of the Bone and Joint Decade 2000–2010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S39–51Martin, BI, Deyo, RA, Mirza, SK et al.
Expenditures and Health Status Among Adults With Back and Neck Problems
JAMA 2008 (Feb 13); 299 (6): 656–664Murray CJ, Vos T, Lozano R, et al.
Disability-adjusted life years (DALYs) for 291 diseases and injuries in
21 regions, 1990-2010: a systematic analysis for the
Global Burden of Disease Study 2010
Lancet 2013 (Dec 15); 380 (9859): 2197–223Vos T, Flaxman AD, Naghavi M, et al.
Years Lived with Disability (YLDs) for 1160 Sequelae of 289 Diseases
and Injuries 1990-2010: A Systematic Analysis for the
Global Burden of Disease Study 2010
Lancet. 2012 (Dec 15); 380 (9859): 2163–2196Vincent K Maigne JY Fischhoff C Lanlo O Dagenais S
Systematic review of manual therapies for nonspecific neck pain.
Joint Bone Spine. 2013; 80: 508-515Guzman J, Hurwitz EL, Carroll LJ, Haldeman S, Cote P, Carragee EJ, et al.
A New Conceptual Model Of Neck Pain: Linking Onset, Course, And Care
Results of the Bone and Joint Decade 2000–2010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S14–23Hurwitz, EL, Carragee, EJ, van der Velde, G et al.
Treatment of Neck Pain: Noninvasive Interventions:
Results of the Bone and Joint Decade 2000–2010
Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976) 2008 (Feb 15); 33 (4 Suppl): S123–152R. Bryans, P. Decina, M. Descarreaux, et al.,
Evidence-Based Guidelines for the Chiropractic Treatment
of Adults With Neck Pain
J Manipulative Physiol Ther 2014 (Jan); 37 (1): 42–63Lisa C Carlesso, Joy C MacDermid, Anita R Gross, David M Walton, et al.
Treatment Preferences Amongst Physical Therapists and
Chiropractors for the Management of Neck Pain:
Results of an International Survey
Chiropractic & Manual Therapies 2014 (Mar 24); 22 (1): 11Gross AR Kay TM Kennedy C et al.
Clinical practice guideline on the use of manipulation or mobilization
in the treatment of adults with mechanical neck disorders.
Man Ther. 2002; 7: 193-205Anderson-Peacock, E, Blouin, JS, Bryans, R et al.
Chiropractic Clinical Practice Guideline: Evidence-based
Treatment of Adult Neck Pain Not Due to Whiplash
J Canadian Chiro Assoc 2005 (Sep); 49 (3): 158–209Childs JD Cleland JA Elliott JM et al.
Neck pain: clinical practice guidelines linked to the
International Classification of Functioning, Disability,
and Health from the Orthopedic Section of
the American Physical Therapy Association.
J Orthop Sports Phys Ther. 2008; 38: 1-34Snodgrass SJ Rivett DA Sterling M Vicenzino B
Dose optimization for spinal treatment effectiveness:
a randomized controlled trial investigating the effects
of high and low mobilization forces in
patients with neck pain.
J Orthop Sports Phys Ther. 2014; 44: 141-152Hurwitz EL, Morgenstern H, Harber P, Kominski GF, Yu F, Adams AH.
A Randomized Trial of Chiropractic Manipulation and Mobilization
for Patients With Neck Pain: Clinical Outcomes From
the UCLA Neck-Pain Study
Am J Public Health 2002 (Oct); 92 (10): 1634–1641Bergmann T Peterson D
Chiropractic technique principles and procedures.
3rd ed. Elselvier Mosby, St Louis, Missouri 2011Clar C, Tsertsvadze A, Court R, Hundt G, Clarke A, Sutcliffe P.
Clinical Effectiveness of Manual Therapy for the Management of
Musculoskeletal and Non-Musculoskeletal Conditions:
Systematic Review and Update of UK Evidence Report
Chiropractic & Manual Therapies 2014 (Mar 28); 22 (1): 12Gert Bronfort DC, PhD; Roni Evans DC; Brian Nelson MD; Peter D. Aker DC, MSc; et al.
A Randomized Clinical Trial of Exercise and Spinal Manipulation
for Patients with Chronic Neck Pain
Spine (Phila Pa 1976). 2001 (Apr 1); 26 (7): 788–797Evans R, Bronfort G, Nelson B, Goldsmith CH.
Two-year Follow-up of a Randomized Clinical Trial of Spinal Manipulation
and Two Types of Exercise Patients With Chronic Neck Pain
Spine (Phila Pa 1976) 2002 (Nov 1); 27 (21): 2383–2389Shane H Taylor, Nicole D Arnold, Lesley Biggs, Christopher J Colloca et al.
A Review of the Literature Pertaining to the Efficacy,
Safety, Educational Requirements, Uses and Usage of
Mechanical Adjusting Devices: Part 2
J Canadian Chiropractic Assoc 2004 (Mar); 8 (1–2): 74–88, 152–161Read D Wilson F Gemmell H
Activator as a therapeutic instrument: survey of usage
and opinions amongst members of the British Chiropractic Association.
Clin Chiropr. 2006; 9: 70-75Herzog W
The Biomechanics of Spinal Manipulation
J Bodyw Mov Ther. 2010 (Jul); 14 (3): 280–286Huggins T Boras AL Gleberzon BJ Popescu M Bahry LA
Clinical effectiveness of the activator adjusting instrument in the
management of musculoskeletal disorders: a systematic review of the literature.
J Can Chiropr Assoc. 2012; 56: 49-57Pickar JG.
Neurophysiological Effects of Spinal Manipulation
Spine J (N American Spine Society) 2002 (Sep); 2 (5): 357–371Osterbauer PJ Fuhr AW Hildebrandt RW
Mechanical force, manually assisted short lever chiropractic adjustment.
J Manipulative Physiol Ther. 1992; 15: 309-317Srbely J, Vernon H, Lee D, et al.
Immediate Effects of Spinal Manipulative Therapy on Regional
Antinociceptive Effects in Myofascial Tissues
in Healthy Young Adults
J Manipulative and Physiological Therapeutics 2013 (Jul); 36 (6): 333-341Vernon H, Humphreys K, Hagino C.
Chronic Mechanical Neck Pain in Adults Treated by Manual Therapy:
A Systematic Review of Change Scores in Randomized Clinical Trials
J Manipulative Physiol Ther 2007 (Mar); 30 (3): 215–227Hegedus EJ Goode A Butler RJ Slaven E
The neurophysiological effects of a single session of
spinal joint mobilization: does the effect last?
J Man Manip Ther. 2011; 19: 143-151Slaven EJ Goode AP Coronado RA Poole C Hegedus EJ
The relative effectiveness of segment specific level and non-specific
level spinal joint mobilization on pain and range of motion:
results of a systematic review and meta-analysis.
J Man Manip Ther. 2013; 21: 7-17Martinez-Segura R de-la-Llave-Rincon AI Ortega-Santiago R Cleland JA Fernandez-de-las-Penas C
Immediate changes in widespread pressure pain sensitivity, neck pain,
and cervical range of motion after cervical or thoracic thrust
manipulation in patients with bilateral chronic
mechanical neck pain: a randomized clinical trial.
J Orthop Sports Phys Ther. 2012; 42: 806-814Yurkiw D Mior S
Comparison of two chiropractic techniques on pain and
lateral flexion in neck pain patients: a pilot study.
Chiropr Tech. 1996; 8: 155-162Gemmell H Miller P
Relative effectiveness and adverse effects of cervical manipulation,
mobilisation and the activator instrument in patients with sub-acute
non-specific neck pain: results from a stopped randomised trial.
Chiropr Osteopat. 2010; 18Wood TG, Colloca CJ, Mathews R.
A Pilot Randomized Clinical Trial on the Relative Effect of Instrumental
(MFMA) Versus Manual (HVLA) Manipulation in the Treatment
of Cervical Spine Dysfunction
J Manipulative Physiol Ther 2001 (May); 24 (4): 260–271Gemmell H Miller P
Comparative effectiveness of manipulation, mobilisation and the Activator instrument in treatment of non-specific neck pain: a systematic review.
Chiropr Osteopat. 2006; 14: 7
https://doi.org/10.1186/1746-1340-14-7Schneider, M, Haas, M, Glick, R, Stevans, J, and Landsittel, D.
Comparison of Spinal Manipulation Methods and Usual Medical Care
for Acute and Subacute Low Back Pain:
A Randomized Clinical Trial
Spine (Phila Pa 1976). 2015 (Feb 15); 40 (4): 209–217Budgell BS.
Reflex Effects of Subluxation: The Autonomic Nervous System
J Manipulative Physiol Ther 2000 (Feb); 23 (2): 104–106Driscoll MD Hall MJ
Effects of spinal manipulative therapy on autonomic activity and the
cardiovascular system: a case study using
the electrocardiogram and arterial tonometry.
J Manipulative Physiol Ther. 2000; 23: 545-550Dishman JD, Bulbulian R.
Spinal reflex attenuation associated with spinal manipulation
Spine 2000;25:2519–25Welch A., Boone R.
Sympathetic and Parasympathetic Responses to Specific Diversified
Adjustments to Chiropractic Vertebral Subluxations of
the Cervical and Thoracic Spine
J Chiropractic Medicine 2008 (Sep); 7 (3): 86–93Kingston L Claydon L Tumilty S
The effects of spinal mobilizations on the sympathetic nervous system: a systematic review.
Man Ther. 2014; 19: 281-287Botelho MB Andrade BB
Effect of cervical spine manipulative therapy on judo athletes' grip strength.
J Manipulative Physiol Ther. 2012; 35: 38-44Humphries KM Ward J Coats J Nobert J Amonette W Dyess S
Immediate effects of lower cervical spine manipulation on
handgrip strength and free-throw accuracy of
asymptomatic basketball players: a pilot study.
J Chiropr Med. 2013; 12: 153-159Vicenzino B Collins D Wright A
The initial effects of a cervical spine manipulative physiotherapy
treatment on the pain and dysfunction of lateral epicondylalgia.
Pain. 1996; 68: 69-74Fernandez-Carnero J Fernandez-de-las-Penas C Cleland JA
Immediate hypoalgesic and motor effects after a single cervical
spine manipulation in subjects with lateral epicondylalgia. J Manipulative Physiol Ther. 2008; 31: 675-681Fernandez-Carnero J Cleland JA Arbizu RL
Examination of motor and hypoalgesic effects of cervical vs thoracic
spine manipulation in patients with lateral epicondylalgia: a clinical trial.
J Manipulative Physiol Ther. 2011; 34: 432-440Keller TS, Colloca CJ:
Mechanical Force Spinal Manipulation Increases Trunk Muscle Strength
Assessed By Electromyography: A Comparative Clinical Trial
J Manipulative Physiol Ther. 2000 (Nov); 23 (9): 585–595Colloca CJ Keller TS
Electromyographic reflex responses to mechanical force,
manually assisted spinal manipulative therapy.
Spine. 2001; 26: 1117-1124Dishman JD Cunningham BM Burke J
Comparison of tibial nerve H-reflex excitability after
cervical and lumbar spine manipulation.
J Manipulative Physiol Ther. 2002; 25: 318-325Kay TM Gross A Goldsmith CH et al.
Exercises for mechanical neck disorders.
Cochrane Database Syst Rev. 2012; 8
https://doi.org/10.1002/14651858Esposito SPS
Spinal adjustment technique: the chiropractic art.
Craft Printing P/L, Alexandria 2005Gibbons P Tehan P
Manipulation of the spine, thorax and pelvis: an osteopathic perspective.
2 ed. Churchill- Livingstone, London, England 2009Fuhr AW
The Activator method. 2 ed.
Mosby Elselvier, St Louis, Missouri, USA 2009Gallagher EJ Liebman M Bijur PE
Prospective validation of clinically important changes in
pain severity measured on a visual analog scale.
Ann Emerg Med. 2001; 38: 633-638Cleland JA Childs JD Whitman JM
Psychometric properties of the Neck Disability Index and
Numeric Pain Rating Scale in patients with mechanical neck pain.
Arch Phys Med Rehabil. 2008; 89: 69-74Livingston T Bernardi D Carroll M
Commander Algometer [user manual].
J TECH Medical, Midvale, Utah 2015Chesterton LS Sim J Wright CC Foster NE
Interrater reliability of algometry in measuring pressure pain thresholds
in healthy humans, using multiple raters.
Clin J Pain. 2007; 23: 760-766J TECH Medical
Dualer IQ Inclinometer [user manual].
J TECH Medical, Midvale, Utah 2015Fletcher JP Bandy WD
Intrarater reliability of CROM measurement of cervical spine
active range of motion in persons with and without neck pain.
J Orthop Sports Phys Ther. 2008; 38: 640-645Audette I Dumas JP Cote JN De Serres SJ
Validity and between-day reliability of the cervical range of motion (CROM) device.
J Orthop Sports Phys Ther. 2010; 40: 318-323Nitschke JE McMeeken JM Burry HC Matyas TA
When is a change a genuine change? A clinically meaningful interpretation
of grip strength measurements in healthy and disabled women.
J Hand Ther. 1999; 12: 25-30McAlister FA
When should hypertension be treated?
The different perspectives of Canadian family physicians and patients.
Can Med Assoc J. 2000; 163: 403-408de Camargo VM Alburquerque-Sendin F Berzin F Stefanelli VC de Souza DP Fernandez-de-las-Penas C
Immediate effects on electromyographic activity and pressure pain thresholds
after a cervical manipulation in mechanical neck pain:
a randomized controlled trial.
J Manipulative Physiol Ther. 2011; 34: 211-220Furlan AD Pennick V Bombardier C van Tulder M
2009 Updated method guidelines for systematic reviews in the Cochrane Back Review Group.
Spine. 2009; 34: 1929-1941Jüni P Altman DG Egger M
Assessing the quality of controlled clinical trials.
BMJ. 2001; 323: 42-46Rubinstein SM van Eekelen R Oosterhuis T de Boer MR Ostelo RWJG van Tulder MW
The risk of bias and sample size of trials of spinal manipulative
therapy for low back and neck pain: analysis and recommendations.
J Manipulative Physiol Ther. 2014; 37: 523-541Vernon H Puhl A Reinhart C
Systematic review of clinical trials of cervical manipulation:
control group procedures and pain outcomes.
Chiropr Man Ther. 2011; 19: 3Jones SR Carley S Harrison M
An introduction to power and sample size estimation.
Emerg Med J. 2003; 20: 453-458Ioannidis JPA
Why most published research findings are false.
PLoS Med. 2005; 2e124Downie AS Vemulpad S Bull PW
Quantifying the high-velocity, low-amplitude spinal
manipulative thrust: a systematic review.
J Manipulative Physiol Ther. 2010; 33: 542-553Snodgrass SJ Rivett DA Robertson VJ
Manual forces applied during posterior-to- anterior
spinal mobilization: a review of the evidence.
J Manipulative Physiol Ther. 2006; 29: 316-329Saavedra-Hernandez M Arroyo-Morales M Cantarero-Villanueva I et al.
Short-term effects of spinal thrust joint manipulation in patients
with chronic neck pain: a randomized clinical trial.
Clin Rehabil. 2013; 27: 504-512Dunning JR Cleland JA Waldrop MA et al.
Upper cervical and upper thoracic thrust manipulation versus nonthrust
mobilization in patients with mechanical neck pain:
a multicenter randomized clinical trial.
J Orthop Sports Phys Ther. 2012; 42: 5-18Leaver AM Maher CG Herbert RD et al.
A randomized controlled trial comparing manipulation
with mobilization for recent onset neck pain.
Arch Phys Med Rehabil. 2010; 91: 1313-1318Langley GB Sheppeard H
The visual analogue scale: its use in pain measurement.
Rheumatol Int. 1985; 5: 145-148Paul-Dauphin A Guillemin F Virion JM Briancon S
Bias and precision in visual analogue scales: a randomized controlled trial.
Am J Epidemiol. 1999; 15: 1117-1127Myles PS Urquhart N
The linearity of the visual analogue scale in patients with severe acute pain.
Anaesth Intensive Care. 2005; 33: 54-58Ferreira-Valente MA Pais-Ribeiro JL Jensen MP
Validity of four pain intensity rating scales.
Pain. 2011; 152: 2399-2404Brent D. Leininger, Roni Evans, Gert Bronfort
Exploring Patient Satisfaction: A Secondary Analysis of a
Randomized Clinical Trial of Spinal Manipulation, Home
Exercise, and Medication for Acute and Subacute Neck Pain
J Manipulative Physiol Ther 2014 (Sep 5); 37 (8): 593–601Hjermstad MJ Fayers PM Haugen DF et al.
Studies comparing Numerical Rating Scales, Verbal Rating Scales,
and Visual Analogue Scales for assessment of pain intensity
in adults: a systematic literature review.
J Pain Symptom Manage. 2011; 41: 1073-1093Williams ACdC Davies HTO Chadury Y
Simple pain rating scales hide complex idiosyncratic meanings.
Pain. 2000; 85: 457-463Sterling M Pedler A Chan C Puglisi M Vuvan V Vicenzino B
Cervical lateral glide increases nociceptive flexion reflex
threshold but not pressure or thermal pain thresholds in
chronic whiplash associated disorders:
a pilot randomised controlled trial.
Man Ther. 2010; 15: 149-153Snodgrass SJ Cleland JA Haskins R Rivett DA
The clinical utility of cervical range of motion in diagnosis, prognosis,
and evaluating the effects of manipulation: a systematic review.
J Physiother. 2014; 100: 290-304Millan M Leboeuf-Yde C Budgell B Descarreaux M Amorim MA
The effect of spinal manipulative therapy on spinal range
of motion: a systematic literature review.
Chiropr Man Ther. 2012; 20: 23Descarreaux M Nougarou F Dugas C
Standardization of spinal manipulation therapy in humans:
development of a novel device designed to measure dose-response.
J Manipulative Physiol Ther. 2013; 36: 78-83Nougarou F Dugas C Deslauriers C Page I Descarreaux M
Physiological responses to spinal manipulation therapy:
investigation of the relationship between electromyographic responses and peak force.
J Manipulative Physiol Ther. 2013; 36: 557-563Nougarou F Dugas C Deslauriers C Page I Descarreaux M
The role of preload forces in spinal manipulation: experimental investigation
of kinematic and electromyographic responses in healthy adults.
J Manipulative Physiol Ther. 2014; 37: 287-293Dishman JD Burke J
Spinal reflex excitability changes after cervical and
lumbar spinal manipulation: a comparative study.
Spine J. 2003; 3: 204-212Dunning J Rushton A
The effects of cervical high-velocity low-amplitude thrust manipulation
on resting electromyographic activity of the biceps brachii muscle.
Man Ther. 2009; 14: 508-513Vicenzino B Paungmali A Buratowski S Wright A
Specific manipulative therapy treatment for chronic lateral
epicondylalgia produces uniquely characteristic hypoalgesia.
Man Ther. 2001; 6: 205-212Carrick FR
Changes in brain function after manipulation of the cervical spine.
J Manipulative Physiol Ther. 1997; 20: 529-545Eingorn AM Muhs GJ
Rationale for assessing the effects of manipulative therapy
on autonomic tone by analysis of heart rate variability.
J Manipulative Physiol Ther. 1999; 22: 161-165Bolton PS Kerman IA Woodring SF Yates BJ
Influences of neck afferents on sympathetic and respiratory nerve activity.
Brain Res Bull. 1998; 15: 413-419Mangum K Partna L Vavrek D
Spinal manipulation for the treatment of hypertension:
a systematic qualitative literature review.
J Manipulative Physiol Ther. 2012; 35: 235-243Kawchuk GN Prasad NG McLeod RC Liddle T Li T Zhu Q
Variability of force magnitude and force duration in manual
and instrument-based manipulation techniques.
J Manipulative Physiol Ther. 2006; 29: 611-618Bijur PE Latimer CT Gallagher EJ
Validation of a verbally administered numerical rating scale
of acute pain for use in the emergency department.
Acad Emerg Med. 2003; 10: 390-392Feise R
Do multiple outcome measures require p-value adjustment?
BMC Med Res Methodol. 2002; 2: 1-4Triano J, Budgell B, Bagnulo A, Roffey B, Bergmann T, Cooperstein R.
Review of Methods Used by Chiropractors to Determine
the Site for Applying Manipulation
Chiropractic & Manual Therapies 2013 (Oct 21); 21 (1): 36
Return to CHRONIC NECK PAIN
Return INSTRUMENT ADJUSTING
Since 6–02–2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |