

Psychosocial Factors and their Role in Chronic Pain:
A Brief Review of Development and Current StatusThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Chiropractic & Osteopathy 2005 (Apr 27); 13 (1): 6 ~ FULL TEXT
OPEN ACCESS Stanley I Innes
Private Practice
35 Maroondah Highway,
Lilydale, 3140, Australia.
sinn0235@bigpond.net.au
The belief that pain is a direct result of tissue damage has dominated medical thinking since the mid 20th Century. Several schools of psychological thought proffered linear causal models to explain non-physical pain observations such as phantom limb pain and the effects of placebo interventions. Psychological research has focused on identifying those people with acute pain who are at risk of transitioning into chronic and disabling pain, in the hope of producing better outcomes.
Several multicausal Cognitive Behavioural models dominate the research landscape in this area. They are gaining wider acceptance and some aspects are being integrated and implemented into a number of health care systems. The most notable of these is the concept of Yellow Flags. The research to validate the veracity of such programs has not yet been established.
In this paper I seek to briefly summarize the development of psychological thought, both past and present, then review current cognitive-behavioural models and the available supporting evidence. I conclude by discussing these factors and identifying those that have been shown to be reliable predictors of chronicity and those that may hold promise for the future.
Introduction
There is an increasing interest and acceptance in psychosocial factors and their correlations to the onset and outcomes of acute pain episodes. This review will briefly review its evolution and summarize the past and present theoretical models in relation to low back pain (LBP). Psychlit, MEDLINE and medindex searches were conducted to identify relevant articles with the search words 'psychological factors, chronic/persistent pain'.
Historical development
The psychological and psychiatric aspects of pain had been infrequently noted by modern writers as early as 1768. For a comprehensive historical review see Merksy & Spear [1]. By the second half of the 19th Century, however, pain was considered sensorial and organic causes were offered to explain all pains, even those without an obvious basis in tissue damage or organic disease. The belief that all pain was a direct result of tissue damage was firmly entrenched by the early 20th Century [2].
By the late 1950's it became increasingly evident that sensory explanations failed to account for certain puzzling pain phenomena (e.g., relief from pain with placebo interventions, phantom limb pain). Around the mid-20th Century several different theories were developed from differing theoretical backgrounds to explain the observation that sensory input did not always correlate with pain. I have summarized these differing schools of thought by prιcising a comprehensive review by Gamsa [3, 4].
Psycholanalytic Formulations
Here intractable pain, which defies organic explanations, was seen as a defence against unconscious conflict. Emotional pain is displaced onto the body where it is more bearable. For example, conscious or unconscious guilt with pain serving as a form of atonement, or the development of pain to replace feelings of loss. Critics have raised serious methodological and conceptual concerns [5, 6]. For example; the ability to quantify and research the constructs of Id, ego and superego. Psychoanalytic thinking no longer forms a significant basis for research or source of current interventions.
Behaviourist Models
Following the work of Skinner [7], behaviourists tried to show that all behaviour could be shaped, altered, weakened or strengthened as a direct of environmental manipulations. Fordyce et al. [8] were the first to apply the behaviour model to pain. It was thought that there was a simple causal connection between pain and its reinforcers. Respondent (acute) pain was seen as a reflexive response to antecedent stimulus (tissue damage). The respondent pain may eventually evolve into operant and persisting pain if the environment offers pain contingent reinforcement. Pain behaviour may also be learned by observing "pain models" i.e., individuals who exhibit such behaviour. More complex factors such as personal dynamics, emotional state, physical vulnerability, and numerous psychosocial variables were not addressed. It proposed that operant pain persists because the behaviour of others (family, friends and health care providers) during the acute pain stage reinforced that pain returned secondary gains, such as permission to avoid chores, or obtain otherwise unobtainable attention and care. Behaviour models have however contributed to the study of pain by the introduction of carefully designed control procedures and laboratory methods [4].
Cognitive Approaches
Cognitive approaches were inspired in part by Melzack and Wall's [9] gate control theory, which established a role for the cognitive-evaluative process in the modulation of pain. Since the mid 1970's proponents of cognitive theory studied the influence of the meaning of pain to patients, and examined the effect of coping styles on pain, for further review see Weisenberg [10]. Cognitive theory examines intervening variables such as attributions, expectations, beliefs, self-efficacy, personal control, attention to pain stimuli, problem solving, coping self-statements and imagery. Pain studies investigated the effects of these thought processes on the experience of pain and related problems. Cognitive theory has added an important dimension to psychological research into pain, but cognitive theorists themselves emphasise that they do not provide the solution, in isolation from other aspects of the multidimensional problem of pain [4, 19]. The combination of cognitive and behavioural approaches has been employed extensively in pain programmes during the last 1520 years with some reported success [11].
Psychophysiological Approaches
Examines the influence of mental events (thoughts memories and emotions) on physical changes which produce pain, for a comprehensive review see Flor and Turk [12]. For example, general arousal models propose that frequent or prolonged arousal of the Autonomic Nervous System (ANS) including prolonged muscular contractions, generate and perpetuate pain. Treatment, such as EMG, biofeedback, and relaxation techniques are designed to decrease the levels of muscular tension and ANS arousal and thereby decrease the pain. Studies have shown positive results from these interventions, but not necessarily more than other psychological techniques [3, 4].
In sum, psychological thought during the past half century has shifted from linear to multicausal models of pain. Methods of investigation have also improved.
Current theoretical models
A substantial number of acute painful musculoskeletal injuries do not resolve quickly and account for the majority of the associated costs [13]. Early intervention appears to result in improved outcomes [14]. Consequently, it is not surprising that the on-going evolution of the understanding of the non-physical aspects of pain has been applied to the areas of screening for, intervening in and predicting those at risk of developing into a chronic and disabling situation [15, 16, 33].
The recent New Zealand Government review into LBP, its subsequent published guidelines, and resultant growing acceptance of the "Yellow Flags" concept is a pertinent example [1719]. Variables such as attitudes, beliefs, mood state, social factors and work appear to interact with pain behaviour, and are cumulatively referred to as psychosocial factors. However, to date there has not been developed a comprehensive, multivariate and empirically supported Integrated Biopsychosocial Risk-for-Disability Model. During a plenary session at the Forth International Forum on LBP Research in 2000 [20] Pincus et al amalgamated the Cognitive and behavioural thinking and proffered the closest structure yet to such a model. It has sought to incorporate many of these factors, and as such offers a structure from which to review these psychosocial factors.
The cognitive-behavioural researchers in the late 20th century noted that acute pain was associated with a pattern of physiologic responses seen in anxiety attacks, whilst chronic back pain was characterized more effectively by habitation of autonomic responses and by a pattern of vegetative signs similar to those seen in depressive disorders. One of the prominent researchers, Waddell, noted that one of the striking findings was that "fear of pain was more disabling than the pain itself" [21]. As a result the notion that reduced ability to carry out daily tasks was merely a consequence of pain severity had to be reconsidered. Several studies have indicated that pain-related fear is one of the most potent predictors of observable performance and is highly correlated to self-reported disability levels in subacute and chronic pain [2223].
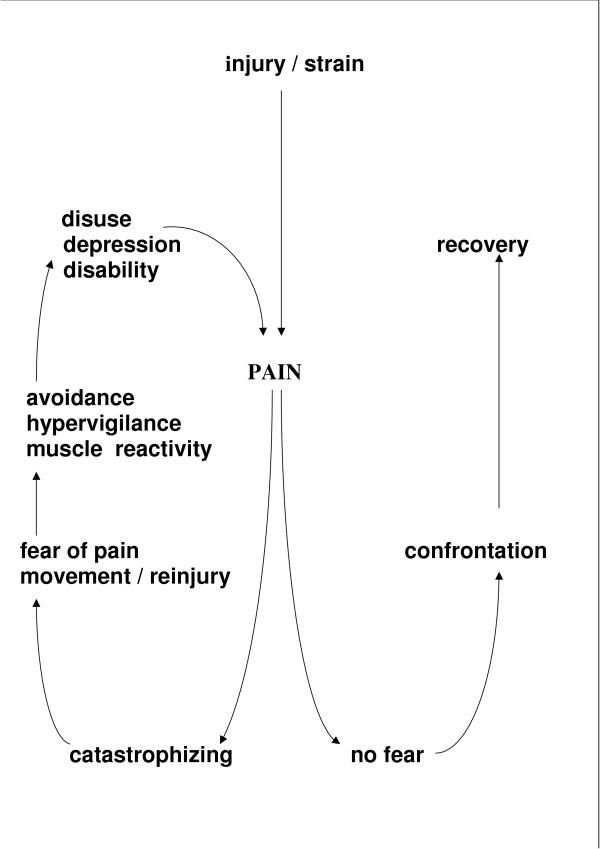
In the acute pain situation, "avoidance" behaviours, such as resting, are effective in allowing the healing process to occur [24]. In chronic pain patients, the pain and disability appear to persist beyond the expected healing time for such a complaint. The danger is that a protracted period of inactivity, as a strategy for coping with the persistent pain may lead to a disuse syndrome (see Figure 1). This is a detrimental condition. It is associated with physical deconditioning such as loss of mobility, muscle strength and lowered pain thresholds (allodynia). Consequently, the performance of daily physical activities may lead more easily to pain and physical discomfort. As a result, the avoidance of activity becomes increasing likely, as does the risk of chronicity. Cognitive-behavioural theorists have variously described this process that leads to chronicity stemming from pathological levels of fear / anxiety as "Fear of pain" [25], fear of physical activity and work [2627], avoiders and confronters [28], kinesiophobia [29] and anxiety sensitivity [30].
Figure 1. A cognitive-behavioural model of pain related fear. [43]
When a person experiences pain they experience varying degrees of psychological distress. A recent study suggests that as many as one third of people seeking care at physical therapists may have significant levels of distress [31]. Many dimensions of this process have been identified and their role posited in the development of chronicity.
One such example is catastrophic thinking processes and is broadly described as an exaggerated orientation towards pain stimuli and pain experience [32]. Negative appraisals about pain and its consequences have been postulated to be a potential precursor to persistent pain. People who consider pain as a serious threat to their health are more likely to become fearful as compared with those who approach pain as a trivial annoyance [33].
Pain-related fear can also contribute to disability through interference with cognitive functions. Fearful patients will tend more to possible signals of threat (hyper-vigilance) and will be less able to shift attention away from pain related information at the expense of other tasks, including actively coping with problems of daily life [34].
Although these and other factors such as coping strategies [35], sense of control [36], personality type [37], faith and religious beliefs [38], have been reported in literature (for a comprehensive review see Keefe et al. [44], the most significant and reproducible factors have been mood / depression and to a lesser extent somatization / anxiety [16, 39]. Depression has been associated with decreased pain thresholds and tolerance levels, reduced ability, general withdrawal and mood disturbance such as irritability, anhedonia (loss of enjoyment of good things in life), frustration and reduced cognitive capacity.
Somatization disorder is a chronic condition in which there are numerous physical complaints. It is perceived as very similar in nature to, and difficult to differentiate from an anxiety disorder [40]. The most common characteristic of a somatoform disorder is the appearance of physical symptoms or complaints for which there is no organic basis. Such dysfunctional symptoms tend to range from sensory or motor disability, and hypersensitivity to pain. This is a difficult and complex syndrome and is more fully dealt with elsewhere [41].
A mention should be made of occupational factors. Job dissatisfaction has repeatedly demonstrated itself to be a significant factor in disability / persistent pain studies. The most recent literature has implicated such factors as support from supervisors at work and low job control (i.e., inadequate power to make decisions and utilize one's skills) which can create distress, and, when perpetual, may result in ill health [42].
Conclusion
In sum, while this cognitive-behavioural model focused on fear / avoidance shows much promise; it has yet not been validated by the research to date [15]. There are studies in progress that may further our knowledge of identifying those at risk of progressing from acute to chronic [13]. Until the veracity of this model becomes further elucidated, depression and somatization / anxiety should be regarded as the central and dominant influencing psychological factors in the assessment for identification and intervention strategies.
Competing interests
The author(s) declare that they have no competing interests.
References:
Mesky H, Spear FG. Pain: Psychological and psychiatric aspects. Bailliere, Tindall and Cassell: London; 1967.
Bonica JJ. Pain research and therapy, achievements of the past and challenges of the future (IASP Presidential Address) In: Bonica JJ, editor. Advances in Pain Research and Therapy. Raven Press, New York; 1983. pp. 136.
Gamsa A. The role of psychological factors in chronic pain. 1 A half century of study. Pain. 1994;57:515
Gamsa A. The role of psychological factors in chronic pain. 2 A critical appraisal. Pain. 1994;57:1729
Roy R. Pain prone patient: A revisit. Psychotherapy. 1982;37:202213
Roy R. Engel's pain-prone disorder patient: 25 years after, Psychotherapy. Psychosomatic. 1985;43:126135
Skinner BF. Science and Human Behaviour. MacMillan: New York; 1953.
Fordyce WE, Fowler RS, Lehmann JF, De Lateur BJ. Some implications of learning in problems of chronic pain. J Chronic Disability. 1968;21:179190
Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971979
Weisenberg J. Cognitive aspects of pain. In: Wall PD, Melzack R, editor. Textbook of pain. 2. Churchill Livingston: Edinburgh; 1989. pp. 231241.
Patrick LE, Altmaier EM, Found EM. Long-term outcomes in multidisciplinary treatment of chronic low back pain: Results of a 13-year follow-up. Spine. 2004;29:850855
Flor H, Turk DC. Psychophysiology of chronic pain: do chronic pain patients exhibit symptom-specific psychophysiological responses? Psychol Bull. 1989;105:215259
Turner JA, Franklin G, Fulton-Kehoe D, Egan K, Wickizer TM, Lymp JF, Sheppard L, Laufman JD. Prediction of chronic disability in work-related muscolskeletal disorders: a prospective, population-based study. BMC Musculoskeletal Disorders. 2004;5:1421
Feldman JB. The prevention of occupational low back pain disability: Evidence-based reviews point in a new direction. Journal of Surgical Orthopaedics. 2004;13:114
Pincus T, Vlaeyen JWS, Kendall NAS, Von Korff MR, Kalaukalani DA, Reiss S. Cognitive-Behavioural therapy and psychosocial factors and low back pain. Spine. 2002;27:133138
Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts in low back pain. Spine. 2002;27:109120
Kendall NAS, Linton SJ, Main CJ. Guide to assessing psychosocial factors Yellow Flags in Acute Low Back Pain: Risk Factors for Long Term disability and Work Loss. Wellington: New Zealand, Accident Rehabilitation & Compensation Insurance Corporation of New Zealand, and the National Health Committee, Ministry of Health; 1997
ACC, the National Health Committee . Acute Low Back Pain Management Guide-Patient Guide. Wellington: New Zealand: Accident Rehabilitation & Compensation Insurance Corporation of New Zealand, and the National Health Committee, Ministry of Health; 1997
Royal College of General Practitioners.
Clinical Guidelines for the Management of Acute Low Back Pain
London: Royal College of General Practitioners; (1999). [UK]Pincus T, Vlaeyen JW, Kendall NA, Von Korff MR, Kalauokalani DA, Reis S. Cognitive-behavioural therapy and psychosocial factors in low back pain: directions for the future. Spine. 2002;5:133138
Waddell G, Newton M, Henderson I, Somerville , Main C. The Fear Avoidance Beliefs Questionairre and the role of Fear Avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157168
Asmundson GJ, Norton PJ, Norton GR. Beyond pain, the role of fear and avoidance in chronicity. Clinical Psych Rev. 1999;19:97119
Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculto-skeletal pain, a state of the art. Pain. 2000;85:317332
Wall PD. On the relation of pain to injury. Pain. 1979;6:253264
Crombez G. Pain modulation through anticipation. Doctoral Dissertation, University of Leuven, Belgium; 1994
McCracken LM, Sorg PJ, Edmands TA, Gross RT. Prediction of pain in persistent pain suffers with CLBP: effects of inaccurate predictions and pain related anxiety. Behavioural Research Therapy. 1993;31:647652
Vlaeyen JW, Kole-Snijders AM, Boeren RG. Fear of Movement/(re) injury in chronic low back pain and its relation to behavioural performance. Pain. 1995;62:363372
Miller RP, Kori SH, Todd DD. Kinesiophobia: A new review of chronic pain behaviour. Pain Management. 1990;3:3543
McCracken LM, Gross RT. Does anxiety affect the coping with chronic pain? Clinical Journal of pain. 1993;9:253259
Asmundson GIG, Norton GR. Anxiety sensitivity in patients with physically unexplained low back pain. Behaviour Research and Therapy. 1999;33:771777
Cairns MC, Forster NE, Wright CC, Pennington D. Level of distress in a recurrent pain population referred for physical therapy. Spine. 2003;28:953959
Turner JA, Jensen MP, Romano JM. Do beliefs, coping, catastrophizing independently predict functioning in patients with chronic pain? Pain. 2000;85:115126
Linton SJ, Hallden K. Can we screen for problematic back pain ? Clinical Journal of Pain. 1998;14:209215
Eccleston C, Crombez G. Pain demands attention: A cognitive-affective model of the interruptive function of pain. Psychological Bulletin. 1999;125:356366
Ax S, Gregg VH, Jones D. Coping and illness cognitions, chronic fatigue syndrome. Clinical Psychology Review. 2001;21:161182
Woby SR, Watson PJ, Roach NK, Urmston M. Adjustment to chronic low back pain the relative influence of fear-avoidance beliefs, catastrophizing, and appraisals of control. Behavioural Research and Therapy. 2004;42:76174
Radnitz CL, Bockian N, Moran A. Assessment of psychopathology and personality in people with physical disabilities. In: Frank RG, Elliot TR, editor. Handbook of rehabilitation psychology. American Psychological Association: Washington DC; 2000. pp. 287309
Koenig HG. Is religion good for your health? Haworth Pastoral Press, Binghampton: NY; 1997
Fayad F, Lefevre-Colau MM, Poiraudeau S, Fermanian J, Rannou F, Wlodyka Demaille S, Benyahya R, Revel M. Chronicity, recurrence, and return to work in low back pain: common prognostic factors. Ann Readapt Med Phys. 2004;47:179189
DSM IV. Diagnostic and statistic manual of mental disorders. American Psychiatric Association: Washington, DC; 1994. p. 446
Moss-Morris R, Wrapson W. Functional Somatic Syndromes. In: Kolt GS, Andersen MB, editor. Psychology in the physical and manual therapies. Churchill Livingstone: London; 2000. pp. 293319
Kaila-Kangas L, Kivirnaki M, Riihimaki H, Luukkonen R, Kironen J, LeinoArjas P. Psychosocial factors at work as predictors of hospitalisation for back disorders. Spine. 2004;30:18231830
Vlaeyen JW, Kole-Snijders AM, Boeren RG. Fear of Movement/[re] injury in chronic low back pain and its relation to behavioural performance. Pain. 1995;62;:363372
Keefe FJ, Rumble ME, Scipio CD, Giordano LA, Caitlin L, Perri M. Psychological Aspects of persistent Pain: Current state of the science. Journal of Pain. 2004;4:195211

Return to CHRONIC NECK PAIN
Return to SPINAL PAIN MANAGEMENT
Return to BIOPSYCHOSOCIAL MODEL
Return to REHABILITATION DIPLOMATE
Since 6-23-2005


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |