

Vertical Posture and Head Stability
in Patients With Chronic Neck PainThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Rehabil Med. 2003 (Sep); 35 (5): 229–235 ~ FULL TEXT
P. Michaelson, M. Michaelson, S. Jaric, M .L. Latash,
P. Sjölander, M. Djupsjöbacka
Southern Lapland Research Department,
Vilhelmina, Sweden.
OBJECTIVE: To evaluate postural performance and head stabilization of patients with chronic neck pain.
DESIGN: A single-blind comparative group study.
SUBJECTS: Patients with work-related chronic neck pain (n = 9), with chronic whiplash associated disorders (n = 9) and healthy subjects (n = 16).
METHODS: During quiet standing in different conditions (e.g. 1 and 2 feet standing, tandem standing, and open and closed eyes) the sway areas and the ability to maintain the postures were measured. The maximal peak-to-peak displacement of the centre of pressure and the head translation were analysed during predictable and unpredictable postural perturbations.
RESULTS: Patients with chronic neck pain, in particular those with whiplash-associated disorders, showed larger sway areas and reduced ability to successfully execute more challenging balance tasks. They also displayed larger sway areas and reduced head stability during perturbations.
CONCLUSION: The results show that disturbances of postural control in chronic neck pain are dependent on the aetiology, and that it is possible to quantify characteristic postural disturbances in different neck pain conditions. It is suggested that the dissimilarities in postural performance are a reflection of different degrees of disturbances of the proprioceptive input to the central nervous system and/or of the central processing of such input.
From the FULL TEXT Article:
INTRODUCTION
Several studies have reported significant disturbances of vertical posture during various standing and walking conditions in patients with chronic neck pain. [1–4] There are however conflicting reports on the characteristics of postural sway during quiet standing in patients with chronic neck pain. McPartland et al. [5] reported similar body sway in patients suffering from chronic neck pain to that seen in healthy subjects. In contrast, poor balance and increased sway have been reported in several studies of patients with chronic musculoskeletal pain of various aetiologies including patients with whiplash injuries. [1–4, 6] In studies of the migration of the centre of pressure (CoP), increased sway has been indicated for patients with cervical dizziness and vertigo. [7, 8] Patients with chronic neck pain have been reported to develop significantly larger mean torque during simple balance test, compared with healthy control subjects, but not during more challenging tests such as one-foot and tandem standing. [5] However, it has also been shown that the ability to execute different postural tasks is reduced with increasing task complexity in patients with whiplash associated disorders (WAD). [4]
One purpose of the current study was to resolve the controversy about the effects of chronic neck pain on postural sway during quiet standing in various conditions.
Two hypotheses were suggested.Hypothesis–1: patients with chronic neck pain, compared with healthy controls, are expected to show increased postural sway and reduced ability to successfully complete various balance tests.
Hypothesis–2: the differences in the sway and in the inability to complete tests are expected to become more pronounced in more challenging postural tasks.The maintenance of balance during quiet standing is only one component of everyday tasks faced by the system for postural stabilization. Equally, or even more, important is the system’s ability to generate appropriate corrective signals in the presence of expected and unexpected postural perturbations (for reviews, see [9, 10]). A disturbed control of back muscles that stabilize the trunk has been demonstrated in patients with low back pain during rapid arm movements. [11] In patients with chronic neck pain, postural perturbations that cause perturbation of the head posture with respect to the trunk appear to be particularly important since they directly influence the painful region. Thus, an additional hypothesis was suggested. Patients with chronic neck pain are expected to show increased sway and poor head stabilization in the presence of postural perturbations (Hypothesis–3).
Cervical muscles in patients with chronic neck pain have been shown to be morphologically different from non-painful neck muscles (for references, see [12]). It has also been reported that vibration of neck muscles in patients with chronic neck pain induces exaggerated perturbing effects of the vertical posture [1], indicating that their balance disorders might be related to altered sensitivity of proprioceptors within the neck muscles. [2, 13] This is supported by animal studies showing that the output from muscle spindles in neck muscles is significantly changed during activation of nociceptors in neck muscles and cervical facet joints. [14, 15] Studies of patients with WAD indicate that they have more severe balance disturbances compared with patients with work-related chronic neck pain [4, 6], suggesting that a whiplash trauma imposes disturbances of the proprioceptive output from the neck region, and/or causes motor control dysfunction that is not present in chronic neck pain without a traumatic origin. To test possible effects of aetiology on sway characteristics and on the ability successfully execute various balance tests, we investigated 2 groups of patients, those who suffered from work-related chronic neck pain and those who had developed chronic neck pain following a whiplash injury.
DISCUSSION
Despite the fact that a rather small number of patients and subjects were included in the present study, a number of significant differences in balance and head stabilization were observed between patients with chronic neck pain and healthy subjects. These differences indicated a strong dependence on the aetiology of the neck pain, i.e. larger differences between the patients with whiplash associated disorder (WAD) and the control subjects than between the patients with work-related pain (WRP) and the control group. The design of the study allow us to address the hypotheses on postural sway and head stabilization in chronic neck pain (see Introduction), and the results indicate that it is possible to quantify characteristic postural disturbances in neck pain of various origin.
Changes in postural stability with task complexity

Table II Making the task of vertical standing more challenging, by closing the eyes and by moving from standing in Romberg position to Tandem standing and one foot standing, resulted in increased sway and decreased ability to complete the task across all subjects. The differences between the WAD group and the other 2 groups increased with increasing difficulty of the postural task (Table II). The WAD patients were particularly likely to fail in the more challenging tasks. It seems conceivable that the rate of success in a particular postural task is related to the ability to keep the postural sway below a given threshold. These observations support both Hypothesis–1 and 2, and are in line with earlier reports (4, 6). Similar effects have also been described on patients with chronic low back pain (24).
Postural adjustments to perturbations

Table III The most pronounced differences between the WAD and the WRP group were observed when external perturbations were added to a quite standing task. We used 2 tests to assess how well the subjects maintained vertical posture and head stability during self-imposed mechanical perturbations. Voluntary bilateral arm movements have been used in many studies of postural adjustments to perturbations. [25, 26] Arm movement imposes torque on the trunk and other body segments, and is accompanied by postural corrections leading to shifts of the centre of mass. [10] The impact of such perturbations seems to be related to the speed of arm movement. In our study, the control subjects moved their arms faster than both the WAD and WRP patients, although the differences were significant only in comparison to the WRP group (Table III). Hence, one would expect transient mechanical perturbations associated with the movement to be larger in the control subjects. However, the amplitude of the anterioposterior CoP-displacement immediately following the perturbation was larger in patients with WAD, in spite of the smaller perturbations (Table III).
The load-release tests, which were independent of the subjects’ ability to perform fast movements [27], also showed a significant difference between the groups. In both the self-triggered and experimenter-triggered load release tests, the patients with WAD demonstrated increased displacement of the CoP immediately following the perturbation, as compared to the control subjects and the patients with WRP. Taken together, these findings suggest a major impairment of the ability to maintain body posture during perturbations in patients with WAD, which is in support of Hypothesis–3.
Chronic neck pain and head stabilization
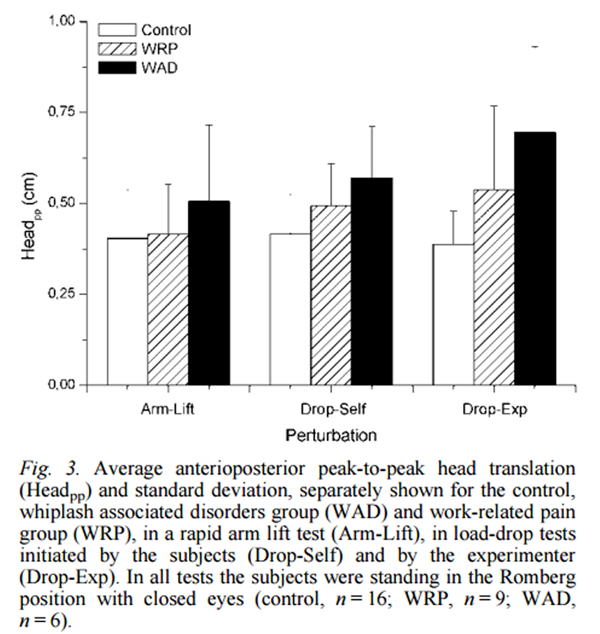
Figure 3 Fast arm movements and load releases unavoidably induce perturbations on both the vertical posture and the head stability, because of the mechanical coupling of different body segments. Our observations of head translation occurring immediately after a perturbation revealed that the patients with WAD demonstrated larger neck motion as a result of both selftriggered and experimenter-triggered perturbations (Figure 3), which is in agreement with Hypothesis–3. The larger neck motion could be a result of an inadequate ability to co-ordinate the neck muscles, potentially leading to larger perturbing torques acting on the head. The latter is supported by Jull [28], who showed increased activity in superficial neck muscles in patients with in combination with a decreased ability to perform controlled neck flexion, implying a disturbed control of the neck muscles involved in neck stabilization.
Possible explanations for the observed differences between WAD and WRP
There is a risk that the differences found between WAD and WRP to some extent could have been due to a selection bias inferred by the small number of patients included in the study. Although a multifactorial inclusion/exclusion procedure was applied, it can not be ruled out that partly different results would have occurred if other criteria had been used. Yet, since all patients showed typical characteristics of chronic neck pain syndromes, and outliers were identified through stringent criteria, it seems more likely that the observed differences had other causes.
Motor control disturbances found in patients with chronic neck pain are thought to be due largely to changed proprioceptive signals from neck muscles (e.g. [2, 13]). It has been shown that activation of nociceptors in muscles and joints excite fusimotor neurones, which alter the sensitivity of the muscle spindle afferents. [14, 15, 29–30] A disturbed sensitivity of the fusimotor system could be triggered by long-lasting exposure to awkward postures or static/repetitive work, such as in WRP, or by a massive, transient afferent input onto the fusimotor neurones from nociceptors and mechanoreceptors in muscles, tendons, ligaments and joint capsules [15, 29], which is likely to occur during a whiplash trauma. Thus, the differences in postural performance found between the 2 patient groups might reflect different degrees of disturbance of the fusimotor system, causing differences in the proprioceptive precision [29, 30], perhaps in combination with permanent damage to cervical soft tissue, the spinal cord and/or the brain stem in some patients with WAD. [31–33]
Another possibility, which does not exclude effects of changed proprioception, is that the observed differences to some extent may be related to adaptive adjustments of postural control strategies developed by patients with chronic neck pain. Adaptive changes of posture and movement have been reported in subjects with atypical movement patterns (for review, see [34]). The slower arm movements of the patients with neck pain, together with their increased head motion and sway area during perturbations, could be a reflection of control strategies adopted to minimize the risk of repeated neck injuries. However, it remains to be elucidated whether or not motor control strategies with a protective purpose are developed in chronic neck pain.
Concluding remarks
Our experiments have confirmed earlier reports on increased postural sway and decreased ability to maintain more demanding standing posture in patients with chronic neck pain, and, in addition, showed major differences in vertical postural and head stability to perturbations. The differences between the patients with WAD and those suffering from WRP suggest that deficits in proprioception and motor control, rather than the chronic pain itself, may be the main factors defining the clinical picture in different chronic neck pain conditions. Consequently, qualitative and quantitative measures of postural performance and head stabilization could be used to increase the precision and efficiency of diagnosis and rehabilitation of chronic neck pain of different aetiology.

Return to CHRONIC NECK PAIN
Return to FORWARD HEAD POSTURE
Since 5–17–2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |