

Blood Pressure Changes in African American Patients
Receiving Chiropractic Care in a Teaching Clinic:
A Preliminary StudyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Chiropractic Medicine 2013 (Jun); 12 (2): 55–59 ~ FULL TEXT
OPEN ACCESS Kim L. McMasters, Joe Wang, Jennifer York, John Hart,
Cheneir Neely, and Rochelle J. Delain
Chiropractor, Private Practice,
McMasters Chiropractic Center,
Asheboro, NC.OBJECTIVE: The purpose of this preliminary study was to determine if a course of chiropractic care would change blood pressure measurements in African American patients and to determine if a study was feasible in a chiropractic teaching clinic.
METHODS: Twenty-four African American patients received chiropractic care in a chiropractic teaching clinic over a study period that spanned 23 visits for each patient. Inclusion criteria consisted of patients having a diagnosis of prehypertension (120-139/80-89) or hypertension stage 1 (140-159/90-99). The mean values of 3 baseline blood pressure readings were compared with the mean values of blood pressure readings taken on visits 21, 22, and 23.
RESULTS: For the entire sample, reductions for both systolic and diastolic blood pressures were not statistically significant (P > .07). When 4 patients having body mass index values that were considered as outliers were excluded, a statistically significant decrease in diastolic blood pressure was observed (P = .004). By group, a statistically significant reduction occurred in the hypertension stage 1 group for systolic and diastolic blood pressures.
CONCLUSION: This study showed that research of this nature may be feasible in chiropractic teaching clinics. The preliminary findings of this study showed that, for a subgroup of African American patients receiving chiropractic care, blood pressure decreased for (a) hypertension stage 1 patients and (b) the sample when those with excessive body mass index were excluded.
KEYWORDS: Blood pressure; Chiropractic; Health occupations students
From the FULL TEXT Article:
Introduction
Hypertension is found in nearly one-third of Americans. [1] For those younger than 65 years, blacks (74.1%) have a greater prevalence compared with whites (57.4%). [1] One study [2] revealed that 90% of study participants reported a high normal blood pressure (BP) measurement within the past 2 years. Of this percentage, 87% were currently using medication for hypertension. The study concluded that improvements in hypertension control among African Americans are likely to depend on changes in diagnosis and management practices by health care providers. Potential issues of reducing hypertension in African Americans include trust in medical care. In one study on African American men, as trust decreased, adherence to medication decreased. [3] Therefore, there is an interest in investigating alternate forms of hypertension management, such as through alternative health care methods. Studies pertaining to chiropractic care and BP indicate that there may be a potential reduction in BP following chiropractic care. [4–7] Although the underlying mechanism for these reductions is unknown, [7] theories include spinal segment reflexes that may affect visceral function. [6]
Studies pertaining to a single race appear to be sparse. This may be a factor in various studies that may not account for differences in BP among different races. The present study focuses on African Americans, as this group tends to experience a greater prevalence of hypertension compared with other racial groups. [1, 2] The purpose of this preliminary study was to determine if a course of chiropractic care would change BP measurements in African American patients and to determine if a study was feasible in a chiropractic teaching clinic.
Methods
The study was approved by the institutional review board at Sherman College of Chiropractic. All patients signed consent before entering this study. The patients were recruited by or referred to the college interns who also provided the chiropractic care for these patients under the guidance of licensed doctors of chiropractic. Consequently, the sample is considered convenient rather than random. Fifty-eight African American patients (28 men, 30 women) older than 40 years from the chiropractic college health center were initially included in this observational study. Fifteen interns provided the care. In addition to race, inclusion criteria consisted of patients having a diagnosis of prehypertension (120–139/80–89) or hypertension stage 1 (140–159/90–99), [8] with or without medication. Each visit consisted of a BP reading followed by a full spine examination (thermography, palpation, and leg length inequality assessment) [9] along with a BP reading (digital automatic: ReliOn, Model HEM-741CREL; Omron Healthcare Inc, Vernon Hills, IL). As this is a pragmatic study, each of the patients received chiropractic adjustments (manipulation) based upon the spinal examination findings for each treatment visit.
Five of the 58 patients completed 45 visits over an approximate 1–year period, although most patients completed approximately half this number of visits during the study period. The median number of visits was 22.5 (45/2). In an effort to obtain the largest number of visits along with the largest number of patients, the end point centered around the median number of visits, that is, visits 21, 22, and 23 (referred to here as postadjustment readings or POST), resulting in a sample of 24 patients. The average of the initial 3 readings (PRE) for systolic and diastolic pressures on the first 3 visits was compared with the average of the readings for visits 21 to 23 (POST).
Data analysis
Mean values for visits 1 to 3 (PRE) were compared with mean values for visits 21 to 23 (POST) for differences in systolic and diastolic BPs. The mean values were assessed for normal distribution by assessing their skew values. Skew values between – 1.96 and + 1.96 were considered not to be significantly different from normal. The 2 data sets of mean values (PRE and POST) fell within this range. Consequently, a 2–tailed t test for paired data was considered appropriate. Data were analyzed in Excel 2003 (Microsoft Corp, Redmond, WA) and Stata IC 12 (StataCorp, College Station, TX) to determine statistical differences between PRE and POST systolic and diastolic readings. Body mass index (BMI) was also calculated [11] to determine if there was a relationship between BMI and whether there were BP reductions between PRE and POST.
Results

Table 1 Among the initial sample of 58 patients, 19 (32.8%) dropped out of the study by the 21st visit. For the initial visit as a group, there were no statistically significant differences in BP readings between the left arm (132.5 ± 15.9 for systolic, 79.6 ± 8.7 for diastolic; P > .8) and the right arm (131.7 ± 14.3 for systolic, 79.7 ± 10.3 for diastolic; P > .8). Summary BP findings by visit can be found in Table 1. The mean BP increased on some visits while decreasing on other visits for both the PRE average and POST average readings (Table 1). No statistically significant differences were observed between the 3 PRE readings for systolic and diastolic (P > .05). Similarly, no statistically significant differences were observed between the 3 POST readings for systolic and diastolic (P > .05).

Figure 1
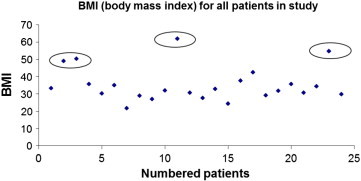
Figure 2 For systolic BPs, the mean PRE was 135.5 ± 12.7 (95% confidence interval [CI], 130.1-140.8), whereas the mean POST was 132.3 ± 12.7 (95% CI, 126.9-137.6), a difference that was not statistically significant (P = .207). For diastolic BP, the PRE average was 81.0 ± 8.4 (95% CI, 77.4-84.5), whereas the POST average was 78.1 ± 10.8 (95% CI, 73.6-82.7), a difference that approached statistical significance (P = .079; Figure 1).
Box plot of BMI scores revealed 4 possible outliers (Figure 2). Quartile analysis (lower fence = Q1 – [1.5 * interquartile range]; upper fence = Q3 + [1.5 * interquartile range]) indicated that these 4 were indeed outliers, that is, outside the fences (of 19.76 and 46.06). Upon exclusion of these 4 outliers, a second comparison of PRE and POST systolic and diastolic BPs was performed.
Because multiple tests for statistical significance were performed in this study (n = 4 tests; systolic and diastolic with vs without outliers), a Bonferroni-adjusted ? was used, resulting in an adjusted ? of .0125 (.05/4). Consequently, P values ≤ .0125 were considered statistically significant. A similar strategy was applied to analysis by group, that is, systolic and diastolic in prehypertensive patients and stage 1 hypertensive patients.

Figure 3 For combined groups minus the BMI outliers, mean PRE systolic pressure was 136.3 ± 13.6 (95% CI, 129.9-142.7) compared with mean POST systolic that was 130.2 ± 11.7 (124.7-135.7), a difference that nearly reached statistical significance (P = .013). For diastolic BP without the 4 BMI outliers, mean PRE diastolic pressure was 81.5 ± 8.5 (95% CI, 77.5-85.5) compared with mean POST diastolic that was 77.1 ± 9.1 (95% CI, 72.9-81.4), a difference that was statistically significant (P = .004; Figure 3).
By groups, there were no statistically significant pre-post differences for either systolic or diastolic BPs for prehypertensive patients (P > .05). For stage 1 hypertensive patients (n = 7), mean PRE systolic BP was 152.7 ± 6.7 (95% CI, 146.6-158.9) vs mean POST systolic BP that was 139.9 ± 11.6 (95% CI, 129.2-150.6), a difference that was statistically significant (P = .0089). Similarly, for stage 1 hypertensive patients, mean PRE diastolic pressure was 87.2 ± 9.4 (95% CI, 78.5-95.8) vs POST mean diastolic pressure of 79.6 ± 11.5 (95% CI, 69.0-90.2), a difference that was also statistically significant (P = .0012).
Discussion
There was no statistically significant difference in BP following chiropractic care for this group of African American patients. However, when 4 patients who had large BMIs (outliers) were excluded from the group, a statistically significant decrease in diastolic BP was observed. It is possible that patients with higher BMI may be more resistant to BP reductions in the context of chiropractic care. Unfortunately, the mechanism between BMI and BP is not well understood. [12]
The findings in this study are similar to those in the study by Bakris et al [7] to the extent that there was a statistically significant reduction in BP in one of the subgroups (diastolic, without BMI outliers). There are a number of differences though between our study and the study of Bakris et al; for example, patients in our study who were already taking BP medication were not “washed out” before the study. Our findings are consistent with other studies that found BP reductions following chiropractic care. [4-7]
Limitations
Limitations of the study include the following: The sample of patients was not randomized, and there was no control group. There was a high dropout rate. There was a lack of accounting of confounding determinants of hypertension, such as diet and exercise. Blood pressure may have reduced on their own, following a waning of a possible “white coat” effect; but that does not appear to be the case in the present study as evidenced by the lack of statistically significant differences among the PRE readings as well as among the POST readings.
Chiropractic interns, rather than doctors of chiropractic, provided the chiropractic care. We suggest that, in future research, student chiropractors could be compared with doctors of chiropractic. In this study, the side of arm on which the BP was taken was not recorded except for the initial visit, which is a limitation to the study. It is well known that some patients have a difference between BPs in their left vs right arm. [10] It is unknown whether the same arm for the same patient was used for the BP readings from visit to visit. It seems unlikely that the side of arm used in this group of patients matters given the lack of statistically significant differences between the left and right arm for this group of patients in their initial BP reading;
The exclusion of BMI outliers is a limitation to this study. When these patients are most likely to exhibit hypertension may be questionable. It may be that patients with higher BMI values may not respond as readily as those with lower BMIs. Future studies could have inclusion criteria for patients with specific BMIs. Although the diastolic reduction (minus the BMI outliers) was statistically significant, it is unknown whether this reduction or the other reductions were clinically significant. In the analysis by groups where statistically significant differences were observed for stage 1 hypertensive patients, the sample size was substantially reduced (to n = 7); so these results should be interpreted with caution. There are other potential factors that may be associated with lowering BP that may be or may not be related to the chiropractic care rendered for these patients. These may include psychosocial factors, reduction in pain, sense of well-being, and other mind-body factors. Because the patients were not randomized and no control group was included, generalization of these findings is not possible. Future study should address the limitations listed above, such as the addition of a control group and randomization of patients.
Conclusion
In this preliminary study of African American patients with prehypertension or stage 1 hypertension, reductions in BP were not statistically significant following chiropractic care delivered in a teaching clinic. However, when patients with outlier BMIs were excluded, a statistically significant reduction in diastolic BP was observed. This study showed that research of this nature may be feasible in chiropractic teaching clinics.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Acknowledgment
The authors thank the following doctors of chiropractic for providing quality care of the patients in this study: Dr Priscilla Bamberg, Dr Melissa Barnett, Dr Morris Clarington, Dr Kiofa Clark, Dr Steve Dotson, Dr Matthew Lewis, Dr Kim McMasters, Dr Qunna Morrow, Dr Cheneir Neely, Dr Michael Pickens, Dr Samuel Ralls, Dr Donna Rouse, Dr Joe Wang, Dr Anthony Witherspoon, and Dr Jennifer York.
References:
Centers for Disease Control and Prevention (CDC)
Racial/ethnic disparities in the awareness, treatment, and control of hypertension—
United States, 2003-2010. MMWR Morb Mortal Wkly Rep. 2013;62(18):351–355
http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6218a2.htmHyman D.J., Pavlik V.N., Vallbona C.
Blood pressure measurement and antihypertensive treatment in a low-income African-American population.
Am J Public Health. 1998;88(2):292–294Elder K., Ramamonjiarivelo Z., Wiltshire J.
Trust, medication adherence, and hypertension control in Southern African American men.
Am J Public Health. 2012;102(12):2242–2245Yates R.G., Lamping D.L., Abram N.L., Wright C.
Effects of Chiropractic Treatment on Blood Pressure and Anxiety: A Randomized, Controlled Trial
J Manipulative Physiol Ther 1988 (Dec); 11 (6): 484–488McKnight M.E., DeBoer K.F.
Preliminary Study of Blood Pressure Changes in Normotensive Subjects Undergoing Chiropractic Care
J Manipulative Physiol Ther 1988 (Aug); 11 (4): 261–266Knutson G.A.
Significant Changes in Systolic Blood Pressure Post Vectored Upper Cervical Adjustment vs Resting
Control Groups: A Possible Effect of the Cervicosympathetic and/or Pressor Reflex
J Manipulative Physiol Ther 2001 (Feb); 24 (2): 101–109Bakris G., Dickholtz M., Meyer P.
Atlas Vertebra Realignment and Achievement of Arterial Pressure Goal in Hypertensive Patients:
A Pilot Study
Journal of Human Hypertension 2007 (May); 21 (5): 347–352Understanding blood pressure readings.
American Heart Association. [Cited 2013 Mar 27].
Available from: http://www.heart.org/HEARTORG/Owen E.F.
Chiropractic Subluxation Assessment: What the Research Tells Us
J Can Chiropr Assoc. 2002;46(4):215–220Right or left arm?
American Heart Association. [Cited 2013 Mar 27].
Available from: www.americanheart.orgU.S. Department of Health and Human Services
Calculate your body mass index.
http://www.nhlbisupport.com/bmi/ [Cited 2010 Mar 10]Kaufman J.S., Asuzu M.C., Mufunda J.
Relationship between blood pressure and body mass index in lean populations.
Hypertension. 1997;30:1511–1516
Return to BLOOD PRESSURE
Since 1-14-2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |