

Effectiveness of Multimodal Chiropractic Care
Featuring Spinal Manipulation for Persistent
Spinal Pain Syndrome Following Lumbar Spine
Surgery: Retrospective Chart Review of
31 Adults in Hong KongThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Medical Science Monitor 2022 (Aug 2); 28: e937640 ~ FULL TEXT
OPEN ACCESS Eric Chun-Pu Chu, Robert J. Trager
New York Chiropractic and Physiotherapy Centre,
EC Healthcare,
Kowloon, Hong Kong.

BACKGROUND The term "persistent spinal pain syndrome type 2" (PSPS-2) has been proposed by the International Association for the Study of Pain to replace the term "failed back surgery syndrome". This retrospective study aimed to evaluate effectiveness of multimodal care featuring chiropractic spinal manipulation (CSMT) in 31 adults in Hong Kong with PSPS-2.
MATERIAL AND METHODS We identified new adult patients with PSPS-2 receiving CSMT from 2016 to 2018. Demographic and clinical data and baseline/follow-up numeric pain rating scale (NPRS) and Oswestry Disability Index (ODI) scores were extracted. Multiple linear regression was used to examine posttreatment NPRS and ODI reduction, with clinical variables as covariates.
RESULTS Of 6,589 patients with low back pain, 31 met criteria (mean age 52.2 ± 13.7 years). Surgeries included laminectomy (81%), discectomy (13%), and fusion (6%). Mean baseline NRPS was 6.6 ± 1.9; ODI was 43.8 ± 15.1%. Patients received CSMT (100%), drop technique (81%), passive modalities (65%), soft tissue manipulation (13%), flexion-distraction (13%), and mechanical traction (13%). Mean posttreatment NPRS was 0.6 ± 1.0; ODI was 2.4 ± 3.3%. All patients had a minimum clinically important difference for NPRS (≥2/10) and ODI (≥30%). One year after treatment, 48% maintained improvement, 42% experienced recurrence; in 10%, follow-up was unavailable. Regression analysis identified younger age, shorter symptom duration, and greater baseline NPRS as predictors of NPRS reduction; and greater baseline ODI as a predictor of ODI reduction (all P<0.05).
CONCLUSIONS Patients with PSPS-2 improved with multimodal care featuring CSMT, which was more effective in patients with younger age, shorter symptom duration, and higher baseline pain or disability levels.
KEYWORDS: Chiropractic, Failed Back Surgery Syndrome, Low Back Pain, Manipulation, Spinal, Musculoskeletal Manipulations
From the FULL TEXT Article:
Background
Persistent spinal pain syndrome (PSPS) is a new term proposed by the International Association for the Study of Pain to define chronic or recurrent pain of spinal origin and replaces older, potentially pejorative terms such as “failed back surgery”. [1–3] PSPS is divided into type 1 (no previous surgery) and type 2 (relevant previous surgery; PSPS-2), which affects 20% to 40% of patients who have had spine surgery. [1] Despite the growing, aging population with PSPS-2, there is no consensus regarding the optimal treatment for this condition. [4] While conservative therapies such as physical therapy, medication, and injections are often recommended instead of revision surgery [4, 5], little research has examined the utility of chiropractic spinal manipulative therapy (CSMT) for PSPS-2. [6, 7]
Chiropractors are portal-of-entry providers that most often treat low back pain (LBP). [8] The most common treatment that chiropractors utilize is spinal manipulation [8], a form of manual therapy directed at the spinal joints. [9] Spinal manipulation is an evidence-based therapy and is recommended by several practice guidelines for LBP. [10–12] However, few large-scale studies have explored the effectiveness of CSMT for PSPS-2, with the majority of evidence derived from case reports and series. [6, 7, 13]
Patients may seek chiropractic care for PSPS-2 because they are often advised to exhaust all conservative options before resorting to a revision spinal surgery, which has a low likelihood of providing relief in many cases. [4, 5] Further, one study found that patients may seek chiropractic care because they prefer to avoid taking prescription medications. [14] Patients also seek chiropractic care because they have a high trust or confidence in the chiropractor’s ability to manage back pain. [14]
Several mechanisms of action for CSMT have been proposed. [15] Historically, chiropractors provided CSMT with the intention of correcting vertebral misalignment. [16] While investigations have not demonstrated significant changes in bony position after CSMT, newer research suggests that pain relief instead relates to biomechanical and neurological changes. [16, 17] Specifically, CSMT may improve intervertebral mobility in areas where mobility is reduced, or inhibit nociceptive (pain) signaling. [15, 16]
CSMT has several contraindications, including manipulation of the spine in the presence of spinal infection or malignancy. [18, 19] Currently, less is known about precautions to CSMT in patients with previous spinal surgery. [7] However, limited evidence suggests that CSMT can be safely administered in this patient population. [6] In addition, while there is limited understanding of the types of CSMT approaches used in PSPS- 2 [7], there is some evidence that chiropractors modify their approach for patients with more complex surgeries, such as fusions. [20] In one survey, chiropractors reported often avoiding CSMT in the region of previous lumbar fusion. [20]
The chiropractic examination for patients with PSPS-2 includes taking a medical history and performing a physical examination. [20] This includes conducting orthopedic and neurologic assessments and reviewing available previous imaging. [6, 21] Chiropractors typically examine patients’ range of motion, sensory and motor function, and muscle stretch reflexes. [6, 22] Positional or neurodynamic maneuvers, such as the straight leg raise, are also tested. [6, 22] Further, chiropractors typically palpate the spine to assess for intervertebral mobility and/ or tenderness. [23] In the present study, the above procedures were conducted for included patients.
Of the prior research examining the effectiveness of CSMT for PSPS-2, we are aware of 2 studies similar to our present study. These included 54 and 32 patients, respectively. [24, 25] Both studies were limited to patients receiving lumbar flexion-distraction (a type of CSMT) alongside other conservative modalities, such as exercise. [24, 25] While these studies each reported improvements in patients’ pain severity, changes in low-back related disability were not examined. [24, 25] Accordingly, the present study aims to add to this research by including a more diverse array of CSMT techniques, as well as examining measures of disability in addition to pain.
Therefore, this retrospective study aimed to investigate the effectiveness of CSMT for PSPS-2 in adult patients in Hong Kong, with the hypothesis that those receiving multimodal chiropractic care featuring CSMT would have clinically important reductions in pain and disability.
Material and Methods
Study Design
The Ethics Committee of the Chiropractic Doctors Association of Hong Kong approved this study and granted a waiver of informed patient consent (Causeway Bay, Hong Kong; IRB ID: CDA20220611). The study is a retrospective chart review of routinely collected clinical data, and the data query and abstraction occurred in June 2022.
Convenience sampling was used, which is a strategy that involves selecting all available cases within a given time period. [26] This method of sampling was most appropriate for this study, considering it is most applicable in instances of rare conditions and smaller expected sample sizes. [27]
Setting
Patients were evaluated and treated in any of 20 affiliated multidisciplinary chiropractic clinics (New York Chiropractic & Physiotherapy Center, EC Healthcare, Hong Kong) by licensed, formally trained chiropractic providers from 2016 through 2018. These clinics are part of a larger healthcare organization (EC Healthcare) that also has neurosurgery and orthopedic departments, which can act as a referral source to the chiropractic clinics. However, patients can also present to chiropractors without an internal or external referral. Chiropractors at these clinics accept insurance, yet many patients ultimately pay out of pocket for treatment.
Although the treating chiropractors in the current study obtained their professional degrees from various institutions, the affiliated clinics (New York Chiropractic & Physiotherapy Center) require an intensive 3–month training and adherence to a clinical handbook for newly hired chiropractors. As part of this onboarding process, each of the chiropractors underwent one-on-one supervised training with the lead investigator of the present study. This fostered some degree of standardization of treatments and clinical protocols among the treating chiropractors.
Data Source
Data was sourced from a customized electronic health records system that encompasses these clinics (CSP, EC Healthcare, Hong Kong) and is searchable by free text query. Data abstraction was conducted by information technology personnel who were blinded to the study hypothesis. Queries of the medical records data was conducted by searching for instances of “spine surgery”, “back surgery”, “fusion”, “laminectomy”, “discectomy”, “lumbar surgery”, and grammatical variants of these terms (eg, discectomies, spinal surgery). Data were abstracted into a Microsoft Excel spreadsheet with pre-defined columns for each data item. Abstracted data were subsequently verified by EC. Free text data extraction was further checked for errors and missing data and was harmonized by RT to a common terminology to enable statistical analysis.
Data regarding potential adverse events was taken from multiple sources, including long-term follow-up data, the larger health records system, which encompasses other medical departments’ documentation, including that of neurosurgery, as well as a feedback/questionnaire sent to patients after their visits, which asks about any symptoms they may have had. Recurrence of symptoms was not considered an adverse event.
Participants
All patients were required to be at least 18 years old and to meet the definition for PSPS-2, having recurrent or persistent chronic LBP and a history of previous lumbar spine surgery. [1] For the purposes of this study, and as defined elsewhere, a minimum symptom duration of 3 months was required for symptoms following lumbar spine surgery. [28]
Patients were required to have treatment with CSMT of any type, including high-velocity, low-amplitude (HVLA), or mobilization techniques, such as flexion-distraction. Patients were also required to have initial and follow-up outcome assessment forms (Oswestry disability index; ODI).
For the purposes of this study, spinal cord stimulator implantation, sacroiliac joint fusion, and ablative procedures, such as radiofrequency ablation, were not considered lumbar spine surgeries. In addition, patients having only a surgery of the cervical or thoracic spine were excluded. Patients with unavailable surgical details were also excluded. In addition, patients with signs and symptoms of cauda equina syndrome (eg, bowel, bladder dysfunction), spinal metastasis, or acute spinal fracture were excluded, as these patients would not be candidates for CSMT and would be referred elsewhere for care.
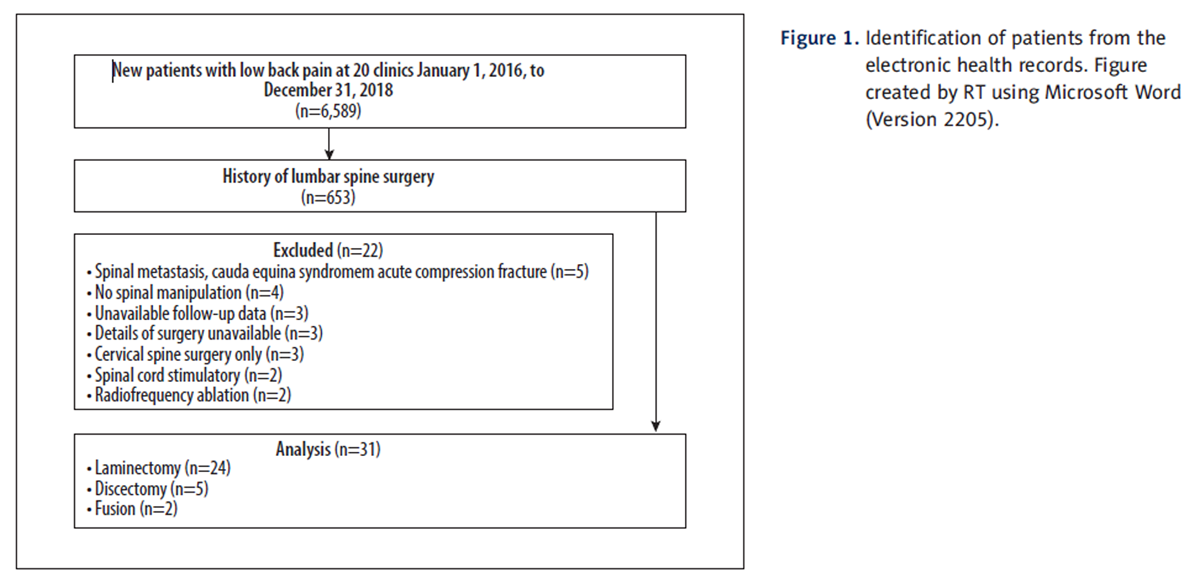
Figure 1 The electronic health records system was searched during June 2022, and a total of 6,589 patients who presented with LBP at the affiliated clinics during the study time window (January 1, 2016, to December 31, 2018) were identified. Among these patients, 53 reported a history of spine surgery. Thirty-one patients met the inclusion criteria and 22 were excluded (Figure 1).
Variables
Basic patient information was recorded in a de-identified manner. The patient’s sex and age in years, upon presentation to the chiropractor, was recorded. The patient’s chief concerns in addition to LBP were written in free text. In this system, sciatica was used to denote pain radiating from the low back into the leg, distal to the knee. Comorbidities that met the criteria for the Centers for Medicare and Medicaid definition for Chronic Conditions were extracted from the electronic health record. [29]
The primary outcome variable of pain severity was recorded at the initial and final presentation to the chiropractor on an 11–point numeric pain rating scale from 0 to 10, in which 10 is the most severe pain. [30] This value was obtained from a written questionnaire rather than from a verbal assessment of pain. Pain severity was used as a continuous variable in the regression models. A 30% reduction in pain severity, or difference of 2 points, was considered the minimal clinically important difference (MCID), when comparing to follow-up baseline data, according to a previous standard. [31]
The primary outcome variable of the ODI has been validated for use in patients with back pain and is widely used in research. [32] The ODI was used as a primary outcome in the current study and was obtained at the initial and final chiropractic visit. [32] ODI is based on the patient’s response to a 10–item written questionnaire, with each question scored from 0 to 5, and is reported as a percentage. [32] In this index a score of 0% to 20% indicates minimal disability; 21% to 40%, moderate disability; 41% to 60%, severe disability; 61% to 80%, crippled; and 81% to 100% is bed-bound or exaggerating symptoms (range, 0% to 100%). A 30% reduction in ODI was considered the MCID when comparing with baseline data. [31] The ODI raw score was used as a continuous variable within the regression models rather than the percentage.

Figures
2–6The year of the patient’s surgery was rounded to the nearest year to obfuscate exact dates, which can be a patient identifier. If the patient had 2 surgeries, the most recent surgery year was utilized for this variable. Surgeries were categorized as a laminectomy (Figure 2), discectomy, fusion, or other descriptor, which was extracted from the medical record.
The patient’s duration of LBP was rounded to the nearest year to obfuscate patient identifiers. This variable did not equal the time since surgery, as certain patients had a pain-free interval for years following their surgery. This was used as a continuous variable in the regression models.
Chiropractic treatment sessions were typically rendered 2 times per week. While all treatments included CSMT, patients also variously received passive modalities (ultrasound thermotherapy, electrotherapy, and cryotherapy/thermotherapy), mechanical spinal traction, or lumbosacral orthotics. Treatment was continued either until the maximum improvement was reached or the patient’s improvement plateaued.
According to a clinic protocol, side posture rotational spinal manipulation for the lumbopelvic region was avoided in patients with PSPS-2 with signs of potential lumbar disc herniation, such as radicular symptoms or imaging evidence of disc displacement. This was a precaution against aggravating discogenic radicular symptoms. In these cases, HVLA CSMT was performed via the aid of a prone drop table technique at the lumbar spine or sacroiliac joint. The drop tables used (various brands) involve a release mechanism that allows part of the cushioned table to release to a lower position during manipulation and have been suggested to reduce the necessary force used in manipulations (Figure 3). [33] HVLA manipulation was avoided altogether in the lumbar region in patients with previous fusion. However, patients with PSPS-2 did have HVLA manipulations in the thoracic and/or cervical spine, away from the site of surgery.
Flexion-distraction is a non-thrust rhythmic mobilization/traction CSMT technique [34], which was applied to the lumbar spine using an automatic table that flexes and extends according to parameters set by the supervising chiropractor (Chirobot®, Chirotech Innovation Co., Ltd, Taiwan; Figure 4). Mechanical traction is a passive technique, not considered CSMT in the present study, that involves an axial distractive force applied to the spine. [35] In the present study, intermittent mechanical traction was performed with the same equipment for each patient (MID Spine Decompression Device, WIZ Medical, Korea), using a traction force ranging from 30% to 60% of the patient’s body weight according to the patient’s tolerance level and clinician’s judgement (Figure 5). [36] Instrument-assisted soft tissue manipulation was applied with a thin layer of emollient on the patient’s lower back and gentle repeated strokes of a massage tool (Strig, Korea; Figure 6).
The duration of CSMT was rounded to the nearest whole number of months. According to a standard clinic procedure, long-term follow-up was assessed when a patient was contacted by a personal health manager employed by the clinic system (EC Healthcare, Hong Kong) at 1 year after the final chiropractic visit. The health manager determined if the patient had maintained their level of improvement or if their symptoms had returned. An adverse event was defined as a serious undesirable outcome beyond transient soreness related to treatment, including exacerbation of neurologic deficits or need for urgent surgery following CSMT.
All patients were recommended a set of home exercises; however, the treating chiropractor may have adapted these to each patient’s specific condition. Further, compliance with home exercises was not tracked during care, and therefore, this variable was not included as a covariate in the regression models. Typical exercises that were recommended to patients included the quadruped cat-camel, bird-dog exercises, and supine dying bug. [37] These are all considered safe, low-load exercises that focus on spine stability and motor control. [37]
Statistical Analysis
All statistical analyses were conducted using GNU PSPP Statistical Analysis Software (V.1.0.1). A P value of less than 0.05 was considered statistically significant. Multiple linear regression was utilized, as it allows examination of the relationship between multiple independent variables and a continuous treatment outcome. [38] This method was ideal for the current study as NPRS and ODI were continuous variables, and treatment response could depend on several clinical factors.
According to recent research, the minimum required sample size for a multiple linear regression is at least 2 subjects per variable. [39, 40] In designing the regression model, a select number of key covariates were chosen from the available dataset. This process was guided by previous research on this topic. [7] Our present study included 7 covariates in each regression model, which accordingly required at least 14 subjects for this method of analysis.
Prior to linear regression, bivariate correlation testing was performed using a 2–tailed Pearson correlation matrix to test for multicollinearity between patient age, sex, surgery type, symptom duration, baseline NPRS, baseline ODI, and duration of visits. Two pairs of variables had a statistically significant correlation coefficient >0.7, with 1 being the baseline NPRS and baseline ODI raw score (coefficient 0.95, P<0.001). Because the ODI incorporates other questions about activity of daily living in addition to pain as measured in NPRS, it was not considered to represent unnecessary redundancy and was kept in the regression model. [41] For treatment duration measured in months and number of visits (coefficient 1.00, P<0.001), the months of treatment was excluded from the regression model as this represented unnecessary redundancy. This high correlation was explained as being due to rounding to the nearest month and a relatively uniform treatment frequency among included patients.
Results
Participants

Table 1 Thirty-one patients, (age 52.2 ± 13.7 years, 17/31 male [55%]), were included in the retrospective analysis (Table 1). All patients had surgery at least 3 months previously, and therefore, no patients were excluded based on this criterion. Although lumbar spine imaging was not a selection criterion, all included patients either presented having previous post-surgery imaging or obtained new lumbar spine imaging, including radiographs and/or magnetic resonance imaging after presentation.
Four patients did not receive CSMT and were accordingly excluded (mean age 41.0 ± 4.6, 50% male). In each of these 4 cases, patients presented to the chiropractor only once, and 1 patient was referred for imaging tests which were not obtained, and 3 patients were referred to a medical specialist for consultation for possible epidural spinal injection. Surgeries included laminectomy (n = 3) and facetectomy (n = 1). These patients had a mean baseline NPRS rating of 9.5 ± 0.5, and mean ODI of 62.5 ± 3.0.
Three patients initially received CSMT but did not have available follow-up NPRS and ODI data and were therefore excluded (mean age 47.7 ± 2.1, 67% male). In 1 case, the chiropractor ordered imaging, which was not obtained, and the patient discontinued care after 2 visits. In the other 2 cases, the reason for lack of follow-up was less clear and the patients had only 1 visit each. The surgeries in these 3 excluded patients who initially received CSMT were laminectomy (n = 2) and discectomy (n = 1). The mean NPRS rating was 8.0 ± 0.0, and the mean ODI was 50.7 ± 1.9.
Among the 31 included patients, in addition to LBP, patients often had a chief concern of lower extremity symptoms, including pain, numbness, weakness, and cramping (28/31, 90%). A minority of patients had LBP as the only symptom (3/31, 10%). The mean duration of symptoms was 3.3 ± 4.4 years. Patients had a mean baseline NRPS of 6.6 ± 1.9, and mean baseline ODI of 43.8 ± 15.1%. The mean interval between lumbar spine surgery to chiropractic evaluation was 3.3 ± 4.4 years. The mean symptom duration was 2.6 ± 2.0 years. The most common surgery was laminectomy (25/31, 81%; Figure 2), followed by discectomy (4/31, 13%) and fusion (2/31, 6%). Most patients had only 1 surgery (29/31, 94%), while 2 patients had 2 surgeries each, which in each case was a second laminectomy (2/31, 6%). Twelve patients (38.7%) had comorbid conditions including diabetes, cardiovascular disease, hyperlipidemia, thyroid disease, and depression.
While all patients received CSMT per the selection criteria, the type of CSMT was further characterized among the other forms of therapy. All patients received HVLA CSMT (31/31, 100%) and home exercise recommendations (31/31, 100%), followed by drop technique CSMT (25/31, 81%), and passive modalities, including ultrasound thermotherapy, electrotherapy, cryotherapy, and thermotherapy (20/31, 65%), instrument-assisted soft tissue manipulation (4/31, 13%), flexion-distraction CSMT (4/31, 13%), and mechanical traction (4/31, 13%). The mean number of chiropractic visits was 21.5 ± 8.7, which occurred over a mean duration of 2.5 ± 1.5 months.
Outcome Data
All patients experienced improvements in the NPRS and ODI from baseline to the final CSMT visit, and no patients reported any serious adverse events. The mean posttreatment NPRS was 0.6 ± 1.0, and ODI was 2.4 ± 3.3%. All patients had a MCID for NPRS (≥2 points) and ODI (≥30%). Seventeen patients (55%) reported posttreatment NPRS and ODI scores of 0, indicating no pain or low back-related disability.
Long-term follow-up analysis at 1 year after treatment identified that 15 of 31 (48%) patients maintained the improvements that they attained during care, while 13 of 31 (42%) experienced recurrence symptoms, with a return of their original symptoms. In 3 of 31 (10%) of patients, 1–year follow-up data was unavailable. Eight of the 17 patients (26% of total patients) who reported complete symptom resolution with CSMT reported continued relief at the 1–year follow-up.

Tables
2 + 3Multiple linear regression with NPRS as the dependent variable identified that younger age, shorter symptom duration, and greater baseline NPRS were significant predictors of posttreatment NPRS reduction with CSMT (Table 2). For every 1 year decrease in age, the posttreatment NPRS was reduced by b (0.20) with CSMT, so a 10–year reduction in age would correspond with an expected reduction in NPRS of 2 points. For every 1–year decrease in symptom duration, the follow-up NPRS was reduced by b (0.34) with CSMT (eg, a 10–year reduction in age would correspond with 3.4 points reduction in NPRS). Last, for every 1–point increase in baseline NPRS, the posttreatment NPRS was reduced by b (0.67) with CSMT (eg, a 10–point increase or maximum NPRS would correspond with a 6.7–point reduction in NPRS).
Our regression model with ODI raw score as the dependent variable showed that a higher baseline ODI raw score predicted a greater improvement in posttreatment ODI after CSMT (Table 3). For every 1–point increase in baseline ODI raw score (which translates to 2% in ODI interpretation), the posttreatment ODI raw score was found to be reduced by b (1.12) with CSMT. Effectively, a 10–point increase in baseline ODI would correspond with an 11.2–point reduction in posttreatment ODI. The other predictors did not reach significance in this model.
The adjusted R2value can be used to determine how well the regression models fit the study observations and can range from 0 to 1 (or 0% to 100%). [40] In both of our regression models, the adjusted R2values were high (0.85 for the NPRS outcome, 0.96 for the ODI outcome). This suggests that the regression models were adequately designed and sufficient to examine the main outcomes in our study.
Discussion
In this retrospective chart review, 31 adult patients were identified from chiropractic clinics in Hong Kong who had PSPS-2 and LBP and received multimodal chiropractic care featuring CSMT. These patients were typically middle- to older-aged adults and most often had lumbar laminectomy. Patients typically presented with moderate to severe low back and lower extremity symptoms and had a moderate to severe low back-related disability measured by ODI. With several sessions of CSMT, all patients showed improvements in pain and ODI, exceeding MCID for each. At the 1–year follow-up, nearly half maintained their improvement, while the others had recurrent symptoms or no available follow-up data. Further analysis showed that younger patients and those with a shorter duration of symptoms and higher baseline pain or ODI were more likely to respond positively to CSMT.
The present study represents one of the largest series of patients with PSPS-2 treated with CSMT. From a recent systematic review and search of PubMed for other studies on June 16, 2022, we found 2 studies of a similar size which were also retrospective in design and examined patients receiving multimodal care featuring flexion-distraction CSMT for PSPS-2. One of these studies, including 54 patients, found similar results to our chart review, as the majority of patients (81%) experienced MCID for pain relief. [24] The other similar study, including 32 patients, also found an MCID in pain relief, yet also noted that patients with combined types of surgery, such as discectomy-laminectomy, had greater improvements in pain. [25]
There are several differences between the present study and these 2 previously published large studies on CSMT and PSPS-2. [24, 25] One major difference is the high prevalence of laminectomy in the present study, whereas the previous studies reported that discectomy was the most common type of surgery. [24, 25] Another difference is that the previous studies mostly or exclusively used flexion-distraction CSMT [24, 25], whereas in the present study, patients typically received drop table lumbopelvic manipulation and HVLA manipulation elsewhere in the spine, and flexion-distraction was used less frequently. However, it is possible that the difference in surgery types accounted for the different CSMT approaches. Another difference is that the present study identified a mean MCID for both pain and low back-related disability, whereas previous studies examined the main outcome of pain only. [24, 25]
The results of the present study add to the understanding that patients are more likely to improve with multimodal conservative care featuring CSMT. Two previous studies that included patients without previous surgery found that a shorter duration of LBP increased the odds of recovery with CSMT. [42, 43] However, in 1 of the studies, baseline NPRS and ODI were not significantly associated with odds of improvement with CSMT. [42] Although this differs from the results of the present study, this may be explained by differences in patient population, since our study included only patients with PSPS-2.
Future research should expand on the present study. A randomized controlled trial is needed to account for many of the confounding sources in the present retrospective study. Several designs could be used in which other therapies, such as physical therapy or medication, could be used in a control group. In addition, health services research designs could enable an examination of the long-term associations of CSMT for PSPS-2, with regards to the likelihood of revision surgery, utilization of pain medications, and cost-effectiveness of CSMT compared with that other treatment pathways.
Limitations
The present study had several limitations. First, as it was retrospective in nature, data identified from the medical record could be inaccurate, missing, or subject to patients’ recall bias. Second, without a control group to account for the natural history and progression of PSPS-2, we cannot conclude that the positive treatment response was caused by CSMT. Third, we did not examine several other important outcomes, such as cost effectiveness, medication utilization, and quality of life, which could provide broader measures of effectiveness. Fourth, the results may not be generalizable as our study population had a high rate of laminectomy, differing from the study populations of other studies of CSMT for PSPS-2 [24, 25], which could be explained by a difference in preferences among surgeons in Asia versus those in other regions. [44] Laminectomies are less complex surgeries than fusions [45]; therefore, this difference could account for some of the observed positive treatment response. Fifth, there were 2 patients that dropped out of care for unknown reasons after a single visit. It is possible that these patients dropped out of care because of financial or other reasons; however, had they not responded to CSMT, their results could have slightly influenced our overall results. Sixth, the sample size of this study was sufficient to conduct a basic descriptive analysis and utilize regression models with a select number of key covariates. However, a larger sample would allow us to explore the effect of additional variables on treatment outcome. These might include comorbidities, pain distribution, time interval since lumbar surgery, imaging findings, and the specific treatments patients received. [7] Further, additional predictor variables could reach statistical significance with a larger population.
Seventh, given patients received a variety of treatments in addition to CSMT, it is unclear if the observed results were related to CSMT alone or to other added therapies. A larger sample and/or prospective design would allow us to either control for these additional therapies or standardize the treatment approach. Finally, although the chiropractors in this study had similar training and similar equipment and adhered to the same clinic protocols, there was likely some variation between the CSMT and other care administered by each chiropractor. Previous studies have shown that forces delivered with manipulation can vary according to practitioner body mass or patient positioning. [46] Therefore, it is unclear if provider or treatment-related differences played a role in the observed outcomes. The treatment protocols could be more standardized in a prospective trial on this topic to reduce this confounding source.
Conclusions
We found that adult patients with PSPS-2 showed improvement with multimodal chiropractic care featuring CSMT, which was more effective in patients who were younger, had a shorter duration of symptoms, and/or had a higher level of pain or disability before treatment.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References
Christelis N, Simpson B, Russo M, et al.
Persistent spinal pain syndrome: A proposal for failed back surgery syndrome and ICD-11.
Pain Med. 2021;22:807-18Lucas AJ.
Failed back surgery syndrome: Whose failure? Time to discard a redundant term.
Br J Pain. 2012;6:162-65Al Kaisy A, Pang D, Desai MJ, et al.
Failed back surgery syndrome: Who has failed?
Neurochirurgie. 2015;61(Suppl. 1):S6-14Daniell JR, Osti OL.
Failed back surgery syndrome: A review article.
Asian Spine J. 2018;12:372-79Baber Z, Erdek MA.
Failed back surgery syndrome: Current perspectives.
J Pain Res. 2016;9:979-87Daniels CJ, Cupler ZA, Gliedt JA, et al.
Manipulative and manual therapies in the management of patients with prior lumbar surgery: A systematic review.
Complement Ther Clin Pract. 2021;42:101261Trager RJ, Daniels CJ, Meyer KW, et al.
Clinical decision-making for spinal manipulation for persistent spinal pain following lumbar surgery: A protocol for a systematic review and meta-analysis of individual participant data.
BMJ Open. 2021;11:e054070Beliveau PJH, Wong JJ, Sutton DA, Simon NB, Bussieres AE, Mior SA, et al.
The Chiropractic Profession: A Scoping Review of Utilization Rates,
Reasons for Seeking Care, Patient Profiles, and Care Provided
Chiropractic & Manual Therapies 2017 (Nov 22); 25: 35Hurwitz, EL.
Epidemiology: Spinal Manipulation Utilization
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 648–654Oliveira CB, Maher CG, Pinto RZ, et al.
Clinical practice guidelines for the management of non-specific low back pain in primary care: An updated overview.
Eur Spine J. 2018;27:2791-803Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Stochkendahl MJ, Kjaer P, Hartvigsen J et al.
National Clinical Guidelines for Non-surgical Treatment of Patients with
Recent Onset Low Back Pain or Lumbar Radiculopathy
European Spine Journal 2018 (Jan); 27 (1): 60–75O’Shaughnessy J, Drolet M, Roy JF, Descarreaux M.
Chiropractic management of patients post-disc arthroplasty: Eight case reports.
Chiropr Osteopat. 2010;18:7Sharma R, Haas M, Stano M.
Patient attitudes, insurance, and other determinants of self-referral to medical and chiropractic physicians.
Am J Public Health. 2003;93(12):2111-17Hinkeldey N, Okamoto C, Khan J.
Spinal manipulation and select manual therapies: Current perspectives.
Phys Med Rehabil Clin N Am. 2020;31(4):593-608Henderson, C. N.
The Basis for Spinal Manipulation:
Chiropractic Perspective of Indications and Theory
J Electromyography and Kinesiology 2012 (Oct); 22 (5): 632–642Hennenhoefer K, Schmidt D.
Toward a theory of the mechanism of high-velocity, low-amplitude technique: A literature review.
J Am Osteopath Assoc. 2019;119(10):688-95World Health Organization (WHO)
WHO Guidelines on Basic Training and Safety in Chiropractic
Geneva, Switzerland: (November 2005)Peterson CK, Gatterman MI.
The nonmanipulable subluxation.
Foundations of chiropractic: subluxation 2nd ed St
Louis: Mosby Yearbook Inc. 2005;168-90Daniels CJ, Gliedt JA, Suri P, et al.
Management of patients with prior lumbar fusion: A cross-sectional survey of Veterans Affairs chiropractors’ attitudes, beliefs, and practices.
Chiropr Man Ther. 2020;28:1-10Daniels CJ, Wakefield PJ, Bub GA, Toombs JD.
A narrative review of lumbar fusion surgery with relevance to chiropractic practice.
J Chiropr Med. Elsevier; 2016;15:259-71Evans RC.
Illustrated orthopedic physical assessment.
Elsevier Health Sciences; 2008Triano J, Budgell B, Bagnulo A, Roffey B, Bergmann T, Cooperstein R.
Review of Methods Used by Chiropractors to Determine
the Site for Applying Manipulation
Chiropractic & Manual Therapies 2013 (Oct 21); 21 (1): 36Gudavalli MR, Olding K, Joachim G, Cox JM.
Chiropractic distraction spinal manipulation on postsurgical continued low back and radicular pain patients: A retrospective case series.
J Chiropr Med. 2016;15:121-28Kruse RA, Cambron J.
Chiropractic Management of Postsurgical Lumbar Spine Pain:
A Retrospective Study of 32 Cases
J Manipulative Physiol Ther 2011 (Jul); 34 (6): 408–412Worster A, Haines T.
Advanced statistics: Understanding medical record review (MRR) studies.
Acad Emerg Med. 2004;11(2):187-92Vassar M, Holzmann M.
The retrospective chart review: Important methodological considerations.
J Educ Eval Health Prof. 2013;10:12Schug SA, Lavand’homme P, Barke A, et al.
The IASP classification of chronic pain for ICD-11: Chronic postsurgical or posttraumatic pain.
PAIN. 2019;160:45-52Centers for Medicare & Medicaid Services:
Chronic Conditions Overview [Internet]. [cited 2022 Jun 16]. Available from:
https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-ConditionsKrebs EE, Carey TS, Weinberger M.
Accuracy of the pain numeric rating scale as a screening test in primary care.
J Gen Intern Med. 2007;22:1453-58Ostelo RWJG, Deyo RA, Stratford P, et al.
Interpreting change scores for pain and functional status in low back pain: Towards international consensus regarding minimal important change.
Spine. 2008;33:90-94Fairbank JC, Pynsent PB.
The Oswestry Disability Index
Spine (Phila Pa 1976) 2000 (Nov 15); 25 (22): 2940–2952Bergmann TF, Peterson DH.
Principles of adjustive technique.
Chiropractic technique: Principles and procedures. 3rd edition.
St. Louis, Mo: Mosby; 2010;84-142Cox JM, Gudavalli M.
Traction and distraction techniques.
Principles and practice of chiropractic 3rd edn
McGraw-Hill, New York. 2005;821-40Tadano S, Tanabe H, Arai S, et al.
Lumbar mechanical traction: A biomechanical assessment of change at the lumbar spine.
BMC Musculoskelet Disord. 2019;20:155Meszaros TF, Olson R, Kulig K, et al.
Effect of 10%, 30%, and 60% body weight traction on the straight leg raise test of symptomatic patients with low back pain.
J Orthop Sports Phys Ther. 2000;30(10):595-601Liebenson C.
A modern approach to abdominal training – part III: Putting it together.
J Bodyw Mov Ther. 2008;12(1):31-36Jiang J.
Multiple linear regression. Applied Medical Statistics. 1st edition.
Hoboken, NJ: Wiley; 2022;345-52Hanley JA.
Simple and multiple linear regression: Sample size considerations.
J Clin Epidemiol. 2016;79:112-19Austin PC, Steyerberg EW.
The number of subjects per variable required in linear regression analyses.
J Clin Epidemiol. 2015;68(6):627-36Kraha A, Turner H, Nimon K, et al.
Tools to support interpreting multiple regression in the face of multicollinearity.
Front Psychol. 2012;3:44Peterson CK, Bolton J, Humphreys BK.
Predictors of Improvement in Patients With Acute and
Chronic Low Back Pain Undergoing Chiropractic Treatment
J Manipulative Physiol Ther. 2012 (Sep); 35 (7): 525-533Newell D, Field J.
Who will get better? Predicting clinical outcomes in a chiropractic practice.
Clin Chiropr. 2007;10:179-86Kim J-S, Yeung A, Lokanath YK, Lewandrowski K-U.
Is Asia truly a hotspot of contemporary minimally invasive and endoscopic spinal surgery?
J Spine Surg. 2020;6:S224-36Azizkhanian I, Alcantara R, Ballinger Z, et al.
Spine surgery complexity score predicts outcomes in 671 consecutive spine surgery patients.
Surg Neurol Int. 2021;12:206Downie AS, Vemulpad S, Bull PW:
Quantifying the High-velocity, Low-amplitude Spinal
Manipulative Thrust: A Systematic Review
J Manipulative Physiol Ther. 2010 (Sep); 33 (7): 542-53
Return LOW BACK PAIN
Return to SPINAL PAIN MANAGEMENT
Since 8-21-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |