

Cost-Effectiveness of Non-Invasive and
Non-Pharmacological Interventions for Low Back Pain:
A Systematic Literature ReviewThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Applied Health Econ and Health Policy 2017 (Apr); 15 (2): 173–201 ~ FULL TEXT
OPEN ACCESS Lazaros Andronis, Philip Kinghorn, Suyin Qiao, David G. T. Whitehurst,
Susie Durrell, Hugh McLeod
Health Economics Unit,
Public Health Building,
University of Birmingham,
Birmingham, B15 2TT, UK.
FROM: Weeks ~ JMPT 2016 (Feb) Hurwitz ~ JMPT 2016 (May)BACKGROUND: Low back pain (LBP) is a major health problem, having a substantial effect on peoples' quality of life and placing a significant economic burden on healthcare systems and, more broadly, societies. Many interventions to alleviate LBP are available but their cost effectiveness is unclear.
OBJECTIVES: To identify, document and appraise studies reporting on the cost effectiveness of non-invasive and non-pharmacological treatment options for LBP.
METHODS: Relevant studies were identified through systematic searches in bibliographic databases (EMBASE, MEDLINE, PsycINFO, Cochrane Library, CINAHL and the National Health Service Economic Evaluation Database), 'similar article' searches and reference list scanning. Study selection was carried out by three assessors, independently. Study quality was assessed using the Consensus on Health Economic Criteria checklist. Data were extracted using customized extraction forms.
RESULTS: Thirty-three studies were identified. Study interventions were categorised as:(1) combined physical exercise and psychological therapy,
(2) physical exercise therapy only,
(3) information and education, and
(4) manual therapy.Interventions assessed within each category varied in terms of their components and delivery. In general, combined physical and psychological treatments, information and education interventions, and manual therapies appeared to be cost effective when compared with the study-specific comparators. There is inconsistent evidence around the cost effectiveness of physical exercise programmes as a whole, with yoga, but not group exercise, being cost effective.
There are more articles like this @ our: Cost-Effectiveness of Chiropractic Page CONCLUSIONS: The identified evidence suggests that combined physical and psychological treatments, medical yoga, information and education programmes, spinal manipulation and acupuncture are likely to be cost-effective options for LBP.
Key points for decision makers
Differences across studies due to diversity in comparators and methods employed limit the comparability of studies and hinder drawing conclusions.
Identified studies reported a variety of outcomes, most often incremental cost per quality-adjusted life year, but also additional cost per improvement in pain, quality of life or reduction in work absenteeism.
Evidence suggests that combined physical and psychological treatments, medical yoga, information and education programmes, spinal manipulation and acupuncture are likely to be cost-effective options for LBP. Active exercise programmes are more equivocal in terms of cost-effectiveness.
From the FULL TEXT Article:
Introduction
Low back pain (LBP) is one of the commonest health problems, with a lifetime prevalence of 80–85%. [1] In 2010, LBP ranked first in causes of global years lived with disability (defined as ‘life lived in less than ideal health’), and third for global disability-adjusted life years (defined as ‘the sum of years of life lost due to premature mortality and years lived with disability’) for non-communicable diseases. [2, 3]
The economic burden of LBP is equally substantial. Estimating this burden has been the focus of a number of studies over the past 15 years, most of which have a particular emphasis on North America and Europe. [4–8] A UK study published in 2000 (using 1998 prices) reported an upper estimate for the societal impact of LBP-related health service resource use and periods of work absence to be in excess of £12 billion. This estimate comprised £1.6 billion incurred through the provision of direct health care resources, £1.6 billion related to informal care and £9.1 billion associated with production losses (sometimes referred to as ‘indirect’ costs) due to morbidity. In the US, of the $90.7 billion of total (i.e. both back pain related and unrelated) health care expenditures incurred by individuals with LBP in 1998, Luo and colleagues [6] estimated that $26.3 billion were attributable to LBP. International evidence has provided some consistent findings; indirect costs represent the majority of overall costs, the provision of care by primary care practitioners and physiotherapists contributes 25–30% of direct healthcare costs, and chronic LBP patients account for a large proportion of total health care costs. [4, 5, 8]
It is evident that significant savings—to both the health care system and society as a whole—are possible through improved management of LBP. However, there is a paucity of evidence on the cost-effectiveness of different LBP treatments. This is evident in the fact that primary care LBP researchers have explicitly identified the absence of such evidence, with consideration of ‘cost-effectiveness’ having recently been named as a leading research priority. [9]
Many therapies are available for treatment of LBP. [10] Clinicians’ recommendations for appropriate therapies can vary substantially, [11, 12] and there is considerable uncertainty regarding the respective value of such treatments and interventions. [13] The aim of this systematic review was to identify, document and appraise studies reporting on the cost-effectiveness of non-invasive and non-pharmacological interventions for LBP.
Methods
Study identification
We searched for economic evaluations of non-invasive and non-pharmacological interventions in six major electronic bibliographic databases (EMBASE, MEDLINE, PsycINFO, Cochrane Library, CINAHL and NHS Economic Evaluation Database). The review’s protocol was not published. Searches covered the period from January 2000 to July 2015, and were informed by a list of safe and potentially beneficial non-invasive and non-pharmacological interventions included in guidelines published by the National Institute for Health and Care Excellence (NICE) in the UK [13] and the American Pain Society/American College of Physicians (APS/ACP) in the US. [10]These included various combined physical exercise and psychological treatments, physical exercise interventions, manual therapy programmes, and information and education programmes (see Online Resource 1). Acupuncture was included as a non-invasive intervention in line with the draft LBP guidance published by NICE in 2016. [14] Employed search strategies comprised combinations of key words, synonyms, term variants, expressions and Medical Subject Heading (MeSH) terms. A sample search strategy can be found in the electronic supplementary material (Online Resource 1). Supplementary searches were carried out through a review of reference lists of key articles and previous systematic reviews known to the research team, through screening reference lists of articles included in the study and through carrying out ‘similar article’ searches in MEDLINE (via the PubMed interface).
Study selection
All identified articles were considered against a list of predetermined inclusion and exclusion criteria (Online Resource 1). Selection of articles was carried out by three reviewers (SQ, LA, and PK) independently. Disagreement in inclusion or exclusion was discussed between the reviewers. Selection was carried out in two stages. The first stage aimed to filter out clearly irrelevant publications and involved applying the inclusion criteria on each article’s title and abstract. Publications which met the inclusion criteria at the first stage, as well as articles for which an exclusion or inclusion decision could not be made on the basis of their title and abstract alone, were forwarded to the second stage, where they were judged on the basis of their full text.
To identify and assess the available cost-effectiveness evidence, we targeted different types of economic evaluation studies. Economic evaluations are defined as comparative analyses of alternative technologies, interventions or programmes in terms of both their costs and consequences. [15] Three forms of economic evaluation are typically identified: cost-effectiveness analyses (CEA), cost-utility analyses (CUA), and cost-benefit analyses (CBA). In all three forms of economic analysis, costs are measured in monetary terms. In CEA, consequences are captured as a simplistic, single, natural unit of outcome. In CUA, consequences are expressed in terms of quality adjusted life years (QALYs). QALYs are calculated by adjusting the time spent in a particular health state by the utility or disutility associated with that specific health state. One QALY is equivalent to one year of full health. Finally, in CBA the utility or disutility associated with a treatment or intervention is expressed as a monetary value.
Extraction, quality assessment and synthesis of relevant information
A customised data extraction form was created to record information on relevant aspects, such as bibliographic information (author(s), journal and year of publication), general information (country, population, interventions and comparators), methodological characteristics (type of economic evaluation, type of analysis, perspective, included costs and reported outcomes). Data were extracted by one reviewer (SQ) and were checked and verified by four of the reviewers (LA, DW, PK, and HM). Quality assessment of the identified studies was carried out by two reviewers (LA and SQ) using the Consensus on Health Economic Criteria (CHEC-list) checklist. [16] The CHEC-list was developed to provide a means of obtaining insights into the methodological quality of economic evaluation studies summarised in systematic reviews. The list has been used widely and is recommended in Cochrane reviews as a means of informing appraisal of the methodological quality of economic evaluations. [17] The list comprises 19 questions which were developed and agreed by 23 international experts over three rounds of a Delphi consensus building exercise. Each item of the CHEC-list was formulated as a question that can be answered by yes or no. The checklist does not make provisions for the calculation of numerical scores that summarise a study’s quality, thus no such scores were calculated.
Negative answers to checklist items do not necessarily concede poor practice or result in bias. While no identified studies were discarded on the grounds of poor methodology, relevant limitations are explicitly discussed in the following section. Studies were grouped thematically, according to the type of the intervention they assess. Narrative synthesis was used to analyse, summarise and present the information provided in each of the selected articles.
Results
A total of 891 unique records identified through searches in bibliographic databases and other sources were considered for inclusion. Scanning these records on the basis of their title and abstract led to exclusion of 802 irrelevant records (stage 1). Full text assessment of the 89 potentially relevant studies resulted in the exclusion of a further 56 records. The remaining 33 studies [18–50] comprised the final set of studies that formed the basis for this review. The PRISMA flowchart summarising the selection process is given in Figure 1.
Figure 1. Preferred Reporting Items
for Systematic Reviews and Meta-Analyses
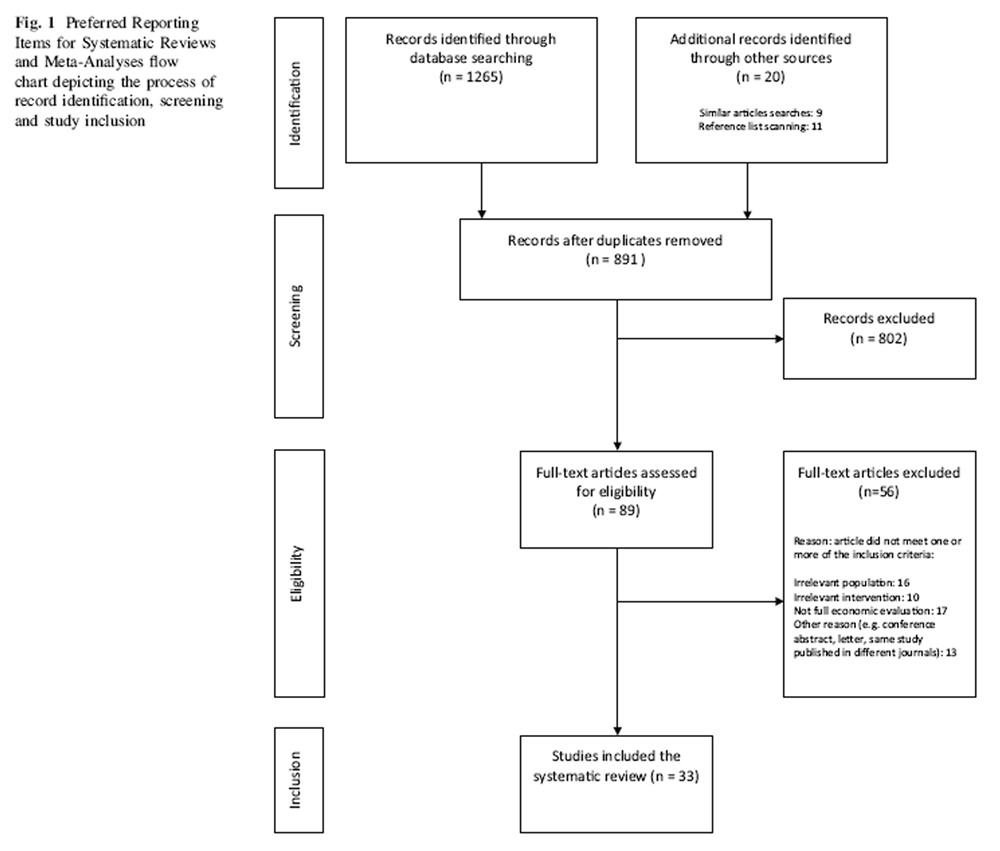
Overview
All of the identified studies were carried out in developed countries and were published between 2002 and 2015. Of these studies, 26 were conducted in Europe (United Kingdom: 14, Norway: 3, Germany: 2, The Netherlands: 2, Finland: 2, Sweden: 1; Denmark: 1, Switzerland: 1), while the remaining seven studies were carried out in North America (United States: 4, Canada: 2) and Asia (South Korea: 1). Interventions assessed in the identified studies were categorised into the following groups: (i) combined physical exercise and psychological treatment (n=12), ii) physical exercise therapy (n=6), iii) manual therapy (n=10), and iv) information and education (n=5).
Characteristics of the identified studies, including the compared interventions, employed methodology and economic evaluation outcomes, are given in Table 2. Twenty-two studies undertook and reported CUA, in all of which outcomes were measured in terms of QALYs. Four studies were CEA [21, 24, 25, 29], typically looking into outcomes such as reduction in disability or pain. Two studies were CBA [19, 20], three reported both a CUA and a CEA [34, 37, 38] and two reported a CEA and a CBA. [18, 46]

Table 1

Table 2 Indications on the methodological quality of the identified studies were obtained through assessment against the 19 items (questions) of the CHEC-list quality assessment checklist. [16] Answers to CHEC-list questions are presented in Table 1. Positive answers to these questions are considered to be indicative of good practice in undertaking and reporting economic evaluations. In all of the identified studies, the number of positive (‘yes’) answers exceeded those of negative or not applicable responses. Many of the negative responses were given to questions related to i) subjecting uncertain variables to sensitivity analysis, ii) discussing the generalisability of the obtained results, and iii) identifying and measuring all appropriate and relevant costs. While sensitivity analyses were present in the majority of the studies, these would often not target variables that the authors identify to be uncertain. An extensive discussion of findings’ generalisability was often not present in cases where the authors conducted an evaluation of a particular, tailored programme provided by a specific payer. Last, questions related to identification and measurement of all appropriate and relevant costs received negative responses when costs relevant to the chosen perspective (e.g. productivity loss when a societal perspective was adopted) were not included.
In the majority of the studies, economic evaluation was carried out alongside clinical studies, most often randomised clinical trials (RCTs) (n=29). One study was based on both a randomised and a non-randomised trial [24] and two studies drew data from a prospective, sequential comparison of separate patient cohorts. [47, 50] Two studies synthesised information from different sources through decision analytic models. [40, 49]
Typically, the time horizon for the analysis was 12 months and was dictated by the maximum follow up in clinical studies which provided data for the economic evaluations. Five studies reported results over a 6 month time horizon [23, 28, 30, 35, 50] and five studies looked at costs and benefits accruing between 12 and 24 months post intervention. [19, 25, 26, 31, 38] Only four studies reported results over time horizons longer than 24 months. Of these, two studies used data from clinical studies with long follow-up [18, 20] and two studies estimated cost-utility results by extrapolating over long time horizons using decision analytic models. [40, 49] In line with recommendations, discounting was carried out to account for the effect of preferential timing in six of the 10 [19, 20, 26, 31, 40, 49] studies which had a follow-up time greater than 12 months. Discounting was not explicitly mentioned in the remaining four studies. [18, 21, 24, 33]
Findings of identified studies
Findings of each study, grouped according to the nature of the compared interventions, are given in the text below.
Combined physical exercise and psychological treatment interventions Twelve studies looking into the cost-effectiveness of combined physical and psychological interventions were identified. Rogerson et al. [42] (USA, societal perspective) focused on a patient group with comparatively severe LPB symptoms, targeting patients screened to identify those at high risk of chronic disability with an intervention combining cognitive behavioural therapy (CBT) and physical therapy. From a societal perspective, the intervention dominated as a treatment strategy, with greater QALY gain and lower total costs. Similarly, Lamb et al. [41] (UK, health care system perspective) found that although the addition of CBT was associated with higher costs (compared to usual care and from a healthcare provider perspective), the favourable QALY gain associated with CBT resulted in a low incremental cost-effectiveness ratio (ICER) of £1,786 per QALY (valuation year: 2008) and a high probability of CBT being cost-effective.
Norton et al. [49] (USA, commercial payer perspective) constructed a decision analytic model to explore the short and long term cost and QALYs of CBT. Key inputs in this analysis, including the likelihood of improvement and quality of life (QoL) values, were obtained from the RCT reported in Lamb et al. [41], as well as from the existing literature. Using a US healthcare payer perspective, Norton et al. [49] estimated the ICER for CBT versus usual care to be $7,197 per QALY in the first year, and $5,855 per QALY over a 10 year time horizon (valuation year 2008).
Four studies evaluated the use of the Keele risk stratification tool, a prognostic screening method which was developed to categorise patients by LBP prognosis to different targeted physiotherapy treatment regimes. The initial StarT Back RCT aimed to assess the effectiveness and cost-effectiveness of the tool [43, 45] (UK, health care system and societal perspectives). This was followed by the IMPaCT Back Study, which sought to determine the effect of implementing the tool on physicians’ choices and patient outcomes [47, 50] (UK, health care system and societal perspectives). In addition to evidence on health outcomes, these studies offered patient level data on use of NHS health care resources, private patient payment and productivity losses. The initial study [43, 45] found the intervention to be cost-effective compared to current practice across all three risk defined sub-groups, with results ranging from dominance for the medium-risk group to a low ICER of £463 per QALY (valuation year: 2008) for the high-risk group. [45] The implementation study [47, 50] found the Keele stratification tool was cost-effective (resulting in cost savings and QALY gains of £124 and 0.023, respectively) only for the high-risk patients [50] (valuation year: 2008).
Four of the studies of CBT or interventions containing some psychosocial element report results which are ambiguous or open to debate. Whitehurst et al. [34] (UK, health care perspective) report a slightly greater clinical benefit from physical therapy than from a brief pain management programme (BPM) targeting psychosocial factors, but lower mean healthcare costs for the latter. In this study, the most cost-effective option is physical therapy (with a cost per QALY of £2,362 (valuation year: 2001)), though the authors suggest that BPM may be acceptable as an additional treatment option, if provided in fewer sessions. [34]
Schweikert et al. [28] (Germany, societal perspective) set out to assess the cost-effectiveness of providing CBT in addition to usual care in patients with chronic LBP in Germany. This study, which had a follow-up period of just six months, showed no statistically significant difference in treatment costs between CBT and standard therapy, and no significant differences in health outcomes, expressed in QALYs. However, due to differences in indirect costs described as being of borderline significance, the authors indicated that the intervention would be cost saving from a societal perspective.
Similarly, Johnson et al. [33] (UK, health care system perspective) conducted a trial-based economic evaluation to determine the impact of a CBT-based exercise and education programme on resource use, costs and patient outcomes. While the intervention led to a small, non-significant reduction in pain and disability, use of resources and costs were low, resulting in an ICER of £5000 per additional QALY (valuation year: 2003). However, the authors suggest that changes detected in QALYs may have been due to bias associated with those patients who had consciously opted into CBT.
Skouen et al. [19] (Norway, societal perspective) carried out a CBA where the benefits of treatment were expressed in terms of productivity gains. The authors found that a light multidisciplinary treatment programme resulted in net benefit for men, but that there was no significant treatment effect for women. No significant differences in costs and benefits were found for a more substantial and extensive multidisciplinary treatment programme.
In the last study in this group, Critchley et al. [31] (UK, health care system perspective) sought to compare the effectiveness and cost-effectiveness of different types of physiotherapy for patients with chronic LBP. Three interventions were compared against each other: usual outpatient physiotherapy, spinal stabilisation classes and physiotherapist-led pain management classes which were informed by a cognitive-behavioural approach. The authors found all three physiotherapy programmes to result in reduced disability (measured by the Roland Disability Questionnaire), improved health-related QoL (measured by EQ-5D), and fewer days off work. In relation to cost-effectiveness, physiotherapist-led pain management appeared to be less costly and marginally more effective than the other interventions.
Physical exercise therapy interventions Six studies assessed the health and economic benefits of exercise and physical activity programmes. All these studies conducted and reported CUAs, with Smeets et al. [38] also reporting a CEA (cost per reduction in disability).
Two studies assessed the costs and benefits of yoga, both of which were carried out on the basis of data collected from randomised controlled trials. In the first of them, Aboagye et al. [48] (Sweden, employer and societal perspectives) found yoga to be cost-effective from the employer’s perspective compared to exercise therapy and self-care advice. From the employer’s perspective, the authors estimated the ICER for yoga to be as low as EUR 4,984 per QALY (valuation year: 2011) when compared to self-care advice, and found that yoga is less costly and of equivalent effectiveness when compared to exercise. When considering productivity costs as part of a societal perspective, Aboagye et al. [48] found that yoga would be a cost-effective option if decision makers deem that a QALY is worth EUR 11,500.
In the second study, Chuang et al. [44] (UK, health care system and societal perspectives) compared yoga in addition to usual care against usual care alone. From the health care perspective, the authors found yoga to be cost effective if decision makers were willing to pay up to £20,000 for an additional QALY (ICER of £13,606 per QALY, valuation year: 2008), while from a societal perspective yoga is associated with cost savings and a greater number of QALYs. Both studies were conducted in Europe (Sweden and the UK respectively), and as with the exercise studies, both adopted a 12 month follow-up.
Two studies looked at the cost-effectiveness of group exercise therapy. Henchoz et al. [39] (Switzerland, societal perspective) compared a 12 week long exercise programme supervised by a sports therapist against usual care comprising advice to exercise regularly, both of which were offered as a follow-up to an outpatient multidisciplinary rehabilitation programme. While the exercise programme resulted in improved disability and trunk muscle endurance, these improvements did not lead to economic benefits. The authors estimated that the addition of exercise as a follow up to a multidisciplinary programme resulted in an ICER of EUR 79,270 (valuation year: 2005) and concluded that group exercise is not cost-effective given commonly cited values of decision makers’ willingness-to-pay (WTP) for a QALY. In a study comparing intensive group training against usual physiotherapy care, van der Roer et al. [37] (Netherlands, societal perspective) found that group exercise resulted in higher costs and no significant differences in QALYs as compared to standard physiotherapy. A main driver of the higher cost was the increased use of secondary and alternative care services in the exercise group.
Smeets et al. [38] (Netherlands, societal perspective) assessed the cost per one-point improvement in disability and cost per QALY for the comparison between: (i) 10 weeks of physical training (including aerobic training and muscle strengthening), (ii) 10 weeks of gradual assumption of patient relevant activities and problem solving training, and (iii) a combination of the two programmes. Findings suggested that whilst combined treatment was not cost-effective, graded activity plus problem solving training delivered as a single intervention was marginally more effective (in terms of QALYs and reduction in disability) than the active physical treatment programme and the combination programme, as it was associated with lower direct and indirect costs.
Rivero-Arias et al. [27] (UK, health care and societal perspectives) sought to evaluate the potential costs and benefits of physiotherapy treatment compared to usual advice given by a physiotherapist for patients with subacute and chronic LBP. The analysis, which makes use of data from a randomised controlled trial, reported no significant differences QoL between the physiotherapy and advice groups, though they found physiotherapy treatment to be associated with significantly higher out-of-pocket expenditures for patients. Despite the relatively low ICER of physiotherapy treatment of £3,890 per QALY (valuation year: 2004), the higher out-of-pocket expenditures were a main influence in the authors’ conclusion that physiotherapist advice should be the treatment of choice in patients with the particular level of LBP severity.
Information and education interventions Five studies looked at the costs and benefits of interventions involving education and provision of information. Loisel et al. [18] (Canada, insurance provider perspective) compared clinical rehabilitation, an occupational intervention comprising visits to an occupational therapist and participatory work with ergonomists, and a combination of the above (Sherbrooke model) against standard care. Two analyses were undertaken: a CEA and a CBA. For the former, the authors compared the additional costs per number of days on full benefits (full compensation) due of absence from work, and found that the greatest savings were associated with the occupational intervention. For their CBA analysis, Loisel et al. [18] subtracted the additional gains from avoided work absence between each intervention and standard care, from the additional cost of the intervention as compared to standard care. The authors found that the Sherbrook model results in mean savings of $18,585 per worker over 6.4 years (valuation year: 1998), although they acknowledge that there were no statistically significant differences in absenteeism avoided between the four interventions.
A similar outcome—the net monetary value due to avoided absenteeism—was explored in the study by Molde Hagen et al. [20] (Norway, societal perspective). This study compared a spine clinic examination and provision of advice and information against usual treatment in primary care. The authors used a CBA framework to explore the long term economic returns of the intervention, in terms of productivity gains due to reduced absenteeism. Findings suggest that spinal clinic care and advice led to significantly fewer days of sick leave at 1 and 3 year follow-up points, which translated to economic returns of approximately $3,500 per person (valuation year: 1995) (though a net benefit value of $2,822 per person is given in the abstract).
Strong and colleagues [29] (USA, insurer perspective) set out to evaluate the effectiveness and cost-effectiveness of psychologist-led and lay person-led back pain educational sessions. Information on resource use and effectiveness was obtained from two cohorts of primary care patients participating in two RCTs. Costs included in the study related to expenditures for delivering the interventions and resource use within primary care. Effectiveness was measured in terms of the number of low impact days, i.e. days during which patients were satisfied with the level of back pain they experienced. Both the psychologist and lay person led interventions resulted in additional low-impact days. The additional cost per low-impact day was found to be $9.70 and $6.13 (valuation year not stated) for the lay and psychologist-led interventions.
In a more recent study, Jensen et al. [46] (Denmark, health care system, taxpayer and societal perspectives) looked at the cost-effectiveness of interventions aimed to enabling LBP patients who have been on sick leave to return to work. The authors compared a brief intervention comprising initial clinical examination followed by advice to increase physical activity against a multidisciplinary intervention, which, in addition to these components, included a tailored plan to facilitate return to work, co-ordinated by a case manager. Two analyses were conducted: a CEA from the perspective of the health care system in Denmark to determine the additional cost per a one-week reduction in sick leave, and a CBA, which adopted a societal perspective and included costs borne by the health care system and productivity losses. The authors [46] reported that the multidisciplinary intervention was more costly that the brief intervention, and, in general, did not result in fewer days of sick leave.
On the premise that psychosocial factors may play a part in preventing LBP from becoming chronic, Jellema et al. [32] (Netherlands, societal perspective) assessed the costs and effectiveness of a minimal intervention strategy aimed at psychosocial factors compared to usual care in patients with sub-acute LBP. The authors found no statistically significant differences in either costs or QALYs in their analysis based on complete trial data, which gave a relatively high ICER of EUR 47,348 (valuation year: 2002) for the minimal intervention strategy. These findings prompted the authors to suggest that usual care should not be replaced by the minimal intervention.
Manual therapy Ten studies evaluating some form of manual therapy were identified. Four of these studies were CUA and were conducted in the UK. [22, 23, 36] The study by Williams et al. [23] (UK, health care system) investigated the cost-utility of osteopathy clinic services within general practices in the UK, as compared to standard care. The authors found the osteopathy clinic intervention to result in higher health care system costs for an increase in health functioning, and estimated an ICER for osteopathy of £3,560 per QALY (valuation year: 1999). However, the authors caution that the conclusion “was subject to considerable random error” and highlight a need for further research to substantiate these results and assess the generalisability of the approach.
The UK BEAM Trial Team [22] (UK, health care system and patient perspective) compared a 12 week exercise programme and a spinal manipulation package, along with combined treatment, to a comparator of best care. Findings of the study suggested that the cost-effectiveness of each programme would depend on decision makers’ WTP for a QALY: if this value is much less than £3,800 (valuation year: 2000), ‘best care’ is likely to be the best strategy. If WTP lies between £3,800 and £8,700, the optimal treatment would be spinal manipulation followed by exercise (i.e. the ‘combined’ treatment). For WTP values well above £8,700, manipulation alone would be the most cost-effective treatment.
Hollinghurst et al. [36] (UK, health care system, patient and societal perspectives) consider three single interventions (massage, Alexander technique and exercise), as well as five iterations of combined treatments, with normal care as the comparator. In terms of the single intervention, exercise performed best in terms of incremental cost-effectiveness (£2,847 per QALY, valuation year: 2005). However, this was due to its low cost and it is noted that exercise performs badly in terms of pain free days. Among two-stage therapies, exercise combined with the Alexander technique was the optimal strategy (£5,332 per QALY).
Haas et al. [24] (USA, perspective not explicitly stated) calculated the total healthcare costs in relation to Medicare expenditure for chiropractic care and found that this option was associated with only moderately higher total costs than usual care, mainly due to fewer onward/external referrals. The cost per reduction in pain and disability score for chiropractic care was lower for chronic than for acute patients. The intervention becomes more cost effective for chronic patients at 12 months than at three months, though the opposite results are observed for acute patients.
Niemisto et al. [21, 25] (Finland, societal perspective conducted a randomised controlled trial to compare physician consultation care combined with manipulative treatment and stabilising exercise against physician consultation. Findings were reported in two studies. The earlier of them [21] was based on 12 month follow up data and had a focus on the effectiveness of the treatments. The authors found no statistically significant differences in costs or health outcomes between the interventions, and calculated an additional cost of $23 per one-point change in a pain visual analogue scale associated with the combined intervention (valuation year: 2002). In the more recent study [25], the finding that a combination of manipulative treatment with exercises and physician consultation is cost-effective appears to reverse. Although there were still statistically significant differences in QoL between the combined intervention and physician consultation, these were deemed to be clinically minor and total annual cost savings were higher in the control.
Four studies investigated the effectiveness of acupuncture, three of which were cost-utility analyses measuring QALYs derived from the SF-6D tariff set. Ratcliffe et al. [26] (UK, health care system perspective) used data from a RCT to estimate the cost and QALYs associated with a programme of individualised acupuncture treatments delivered by acupuncturists trained in traditional Chinese medicine. The intervention was compared with usual care in the UK. The analysis showed acupuncture to be associated with increased costs (largely due to the initial cost of delivering acupuncture treatment), improved QoL and QALYs (mean incremental gain of 0.027 QALYs over 2 years), and an ICER of £4241 per additional QALY gained (valuation year: 2002). Given the low additional cost for a modest improvement in QALYs, Ratcliffe and colleagues [26] suggest that, in the longer term, acupuncture care appears to be a cost-effective treatment for LBP.
The most complex intervention involving acupuncture was evaluated by Herman et al. [35] (Canada, employer, participant and societal perspectives), who label as ‘naturopathic care’ a combination of acupuncture, exercise, dietary advice, relaxation training and education. Cost-effectiveness was calculated from three perspectives: societal, employer and participant. Findings suggested that naturopathic care was cost effective from all perspectives and was dominant from the societal perspective, compared to standardized physiotherapy education.
In a study carried out in Germany, Witt et al. [30] (societal perspective) compared the provision of immediate acupuncture against delayed acupuncture, provided three months later. Two analyses were undertaken, the first on the basis of patients randomised to immediate or delayed acupuncture, and the second on the basis of patients who declined to be randomised and received immediate acupuncture. Data collected over a relatively short period of time (six months) showed immediate acupuncture to be cost-effective from a health service and societal perspective respectively.
Kim et al. [40] (South Korea, societal perspective) sought to assess the cost-effectiveness of acupuncture as a complement to routine care in the treatment of chronic LBP in South Korea. To this end, the authors [40] developed a decision analytic model and populated it with cost and effectiveness information from the literature. Kim and colleagues [40] found acupuncture to result in improved QoL compared to usual care, for a modest increase in costs, a finding similar to Ratcliffe et al. [26] The ICER for this comparison was calculated to be $2,759 per QALY gained (valuation year: 2009).
Discussion
This review identified 33 studies seeking to assess the costs and benefits of a wide range of non-invasive and non-pharmacological interventions for LBP. Studies were grouped into four categories, according to the type of intervention they evaluated. The diversity of the interventions and the setting in which the assessment took place, and the often marked differences in the inputs and evaluation methods employed makes comparisons between studies, even within the same category, difficult. Nevertheless, the review offers insights into the cost-effectiveness of a wealth of interventions.
Summary of findings
Combined physical exercise and psychological treatments comprised the largest and the most diverse group of interventions. The group included studies which evaluated the use of the Keele risk stratification tool to target physiotherapy treatments [43, 45, 47, 50], as well as studies on group exercise and education sessions [33], pain-management programmes [31, 34], stabilisation physiotherapy [31]), multidisciplinary programmes with input from different health care professionals [19, 41, 42, 49] as well as a psychologist-led intervention [28]. With one exception [34], the interventions were compared to usual care and were found to be cost-effective. [28, 31, 33, 41–43, 45, 49] In general, interventions were characterised by non-significant improvements in QALYs and modest increases in costs compared to comparators [31, 33, 34, 42, 43, 45, 47, 50], or the significance of these differences is not reported. [41, 49]
Findings of studies evaluating physical exercise therapy interventions are inconclusive, which may be partially explained by differences in the assessed programmes and employed methods. Studies assessing medical yoga showed this type of activity to be cost-effective from a payer’s perspective and suggest that it may result in averted loss of productivity. [44, 48] On the other hand, studies looking into structured exercise programmes are more cautious: although such programmes appeared to lead to small improvements in QoL, authors do not recommend their widespread use. [27, 37–39] In comparison to combined psychological and physical exercise interventions, physical exercise only interventions appear to be less cost-effective, but it would be interesting to see how the use of yoga, such as that described in the study by Chuang et al. [44], would compare to the interventions reported by Lamb et al. [41] and Foster et al. [47]
Studies evaluating interventions comprising provision of information and education are an equally diverse group. Interventions under assessment are usually multidisciplinary and comprise of clinical examination followed by information and advice. Three out of the five studies in this group employ CBA to estimate the benefit due to days on sick absence averted, net of the cost of the interventions. [18, 20, 46] In general, interventions which have an ‘advice and information’ component appear to lead to reductions in absenteeism, which compensate for the modest increases in costs.
Studies assessing the costs and benefits of manual therapy typically compare spinal manipulation alone or in combination with other components—most often exercise—against usual care, or acupuncture. Bar the studies by Niemisto and colleagues [21, 25], the non-acupuncture studies in this category suggest that manual therapy is a cost-effective alternative to usual care. Interestingly, Niemisto et al. [21] found that manipulative treatment is cost-effective as compared to usual care at 12 months post intervention, but usual care becomes more cost-effective at the 2 year follow-up.
On the whole, the identified evidence on acupuncture interventions is supportive of the idea that provision of acupuncture—either on its own, or in combination with usual care or other active treatments—improves LBP and is a cost-effective option. Three [26, 30, 40] of the four studies reported ICERs below the commonly cited threshold value of £20,000 per QALY, while the study by Herman et al. [35] found a multidisciplinary intervention that combines acupuncture with exercise and dietary advice, relaxation training and the provision of an educational booklet to be both less costly and more effective than standardised physiotherapy.
The clinical recommendations for effective management of back pain advise an individualised multi-modal package of care. A detailed bio-psychosocial assessment, including prognostic risk stratification, should inform targeted interventions. All patients will benefit from reassurance and advice and information on self-management. Further common interventions include physical activity and exercise programmes, manual therapy, with or without acupuncture, as part of a package of care empowering self-management but taking patient preference into account. Those with high risk stratification identifying barriers to recovery may benefit from more intensive intervention with a cognitive behavioural approach. While the clinical guidance for LBP is currently under review, the objective of this review is to assess cost-effectiveness, which does not imply clinical effectiveness.
Methodological issues and comparability
As mentioned above, various factors affect the quality of the identified studies and limit the extent to which reported results are comparable across, or even within, categories of interventions. Prominent amongst such factors are differences in the employed methods.
A first factor that may limit the comparability between studies is the form of economic analysis employed. The choice between CEA, CUA, or CBA depends upon influences such as the requirements of local decision-making bodies, the funding and organisation of local health care services and to some extent the expertise and judgement of the research team. Thus, the use of different forms of analysis poses difficulties in making direct comparisons of the results between studies. However, even when the same form of analysis is adopted, there are many aspects of study design which could, and do, vary. For example, the results of any economic evaluation will differ if the primary measure of effect is changed. [51, 52] What has taken place in all of the studies reported, however, is a systematic comparison of alternative courses of action in terms of their costs and consequences. Hence, the headline findings of the different studies can be cautiously (with trends, patterns and contradictory findings highlighted) as a clear indication of the cost-effectiveness of the assessed interventions.
A further noteworthy issue relates to the adopted perspective. While good practice guidelines for conducting economic evaluations recommend adoption of a wide perspective which will reflect costs incurred to the health care system, patients, their family and their carers, and the economy as a whole, many of the identified studies adopted narrower perspectives. This is likely to have been a pragmatic choice, dictated by the nature of the health care system in place and by the interest of decision makers who are likely to use the reported results. For example, studies conducted in the USA, such as those by Haas et al. [24], Strong et al. [29] and Norton et al. [49] were carried out from the perspective of the organisation that bears the cost, typically the insurer. In contrast, studies which were conducted in countries with public health care coverage, such as those by Whitehurst et al. [45], Chuang et al. [44] and Aboagye et al. [48], typically adopt a health care system (NHS) and societal perspective.
Directly related to the chosen perspective is the inclusion of resource use and cost items in analyses. While good practice guidelines for conducting economic evaluations suggest that appraisal of interventions which are likely to affect absenteeism should include productivity costs [53, 54], there was considerable variation amongst studies in relation to the inclusion of such costs. The diversity in the resource use and costs included, as well as differences in sources of resource use and unit costs employed make comparisons of total costs between studies problematic. As private payments and productivity costs have been shown to constitute a significant share of the total cost of LBP [4, 55, 56], the inclusion or exclusion of such costs in the analysis is expected to have a sizeable impact on results. Similarly, if included, the impact of private healthcare costs can be more influential than payer costs. In general, a range of different interventions are associated with modest impact on QoL, such that additional intervention costs, if any, are not sufficiently large to prevent the interventions from being cost-effective compared to usual practice. However, differences in treatment costs and QALYs tend not to be statistically significant when interventions are compared to usual care. In this context decision-makers need to be aware of how local service activity and costs are likely to compare to those represented in the published studies.
In relation to benefits, the identified studies employ a variety of health care measures to capture outcomes. These include a variety of condition and symptom specific measures about pain and disability, as well as QALYs. QALYs offer a generic measure of QoL that can facilitate comparisons, and this certainly has advantages over arguably narrower measures of outcome associated with CEAs. The multidimensional impact of LBP on people’s usual activities suggests that, in the future, there is potential to use other QoL measures, such as wellbeing and capability measures [57], which offer an opportunity to compare QoL more holistically than the ‘health’ focus of QALYs.
Equally importantly, it must be noted that that evidence of cost-effectiveness does not necessarily imply clinical effectiveness. [58] Indeed there are many situations where intervention appear to result in clinical benefit, but economic analyses indicates that they are not cost-effective. Conversely, treatments which show little clinical benefit may result in cost savings that make them particularly appealing. [58] In addition, observing non-significant differences in QALYs (or costs) should not be interpreted as evidence of ‘no effect’, unless the study is specifically powered to detect such differences. Even if a study is suitably powered, it is widely agreed that, instead of focusing on hypothesis testing, conclusions about treatments’ cost-effectiveness should not be drawn from interpreting the key measure of interest and the uncertainty around it. [15] Another factor which limits the accuracy of the reported aggregate value of health and economic outcomes, relates to the employed time horizon. The greatest share of studies were based on relatively short (typically 12 month) time horizons, which are likely to be inadequate in capturing the full extent of the long-term costs (or cost-savings) and benefits (or disbenefits) associated with treatments for LBP. Interestingly, in cases where a longer time horizon is adopted, this does affect the magnitude of the findings—and in the case of Niemisto et al. [25] it reversed the overall conclusion.
Comparisons were also hindered by the way final results were presented across studies. While the majority of studies calculated and presented incremental cost-effectiveness ratios, not all of them explicated the uncertainty around these estimates. The likelihood of assessed interventions to be cost-effective at different WTP values was typically presented in later studies. It is clear that journals do not necessarily require researchers to adhere to publication guidelines for economic evaluations.
All studies identified in this review were conducted in developed countries, mostly in North America, Western and Central Europe and Scandinavia. While, from a clinical perspective, populations in these countries can be expected to be similar and the effectiveness of treatments can be assumed to be generalizable across countries, comparisons of cost-effectiveness results are likely to be unrealistic, given the considerable variability in the structure of health care systems, differences in the delivery and cost of health care services, and diversity in the bundle of services comprising usual care in different countries.
Strengths and limitations
The review poses particular strengths. In line with recommendations, we searched key electronic bibliographic databases and other sources, by constructing elaborate combinations of free text and indexing terms. Additional searches were carried out in reference lists of key known and identified references, including systematic reviews and official guidelines. Identified studies were independently assessed for inclusion against a set of predetermined criteria. No restrictions were applied on types of economic evaluation or analytic approach used: all types of full economic evaluations, as per the definition by Drummond et al. [15] were considered relevant, including both trial and model-based economic evaluation.
Nonetheless, our review presents specific limitations. In order to narrow the wide range of possible non-invasive and non-pharmacological interventions, we looked into those interventions for which there are indications that are safe and potentially beneficial in guidelines by NICE and APA/ASC. This, however, may have led to the exclusion of interventions which are not mentioned in these guidelines. In addition, given the evolving nature of the interventions, and in the light of changes in the methodology used to assess them, we limited the review to studies published in the last 15 years. This decision enabled us to reduce the chances of compromising comparability due to dissimilarities in the method of economic evaluations used, especially if such dissimilarities were introduced by studies assessing interventions which are now obsolete. While we have endeavoured to give authors’ conclusions around cost-effectiveness of interventions, in cases where judgements were needed on what may be perceived to be cost-effective, we based such judgements on indicative values of WTP for an additional QALY suggested by NICE in the UK. However, it is likely that WTP values may vary across countries.
Comparison with other studies and future research
Given the diverse nature of the interventions (exacerbated by the complex combinations of elements making up a single intervention) and the differences in the aims and scope of the included studies, the scope for comparison between our review and other studies is limited. The study that is deemed to be closest to our review in terms of its aims and focus is that of Lin et al. [59] The authors [59] concluded that the cost-effectiveness of advice as an intervention for LBP is unclear, but other interventions, including interdisciplinary rehabilitation, exercise, acupuncture, spinal manipulation and cognitive-behavioural therapy were, in general, cost-effective for people with sub-acute or chronic LBP. Findings in Lin et al. [59] and our review are in broad agreement. No studies evaluating the cost-effectiveness of medical yoga were identified or reported in the review by Lin et al. [59], though, in our review, we identified evidence which is supportive of yoga.
Conclusions
In summary, the reviewed evidence suggests that combined physical exercise and psychological treatments (CBT and risk stratification), provision of information, manual therapy (chiefly spinal manipulation and acupuncture) are cost-effective options for LBP. The identified evidence around physical exercise therapy is inconclusive; while medical yoga appears to be cost-effective compared to usual care, the finding for some active exercise programmes are equivocal.
References and Tables:


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |
