The Global Spine Care Initiative: Applying Evidence-based
Guidelines on the Non-invasive Management of Back and
Neck Pain to Low- and Middle-income CommunitiesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: European Spine Journal 2018 (Sep); 27 (Suppl 6): 851–860 ~ FULL TEXT
Roger Chou, Pierre Côté, Kristi Randhawa, Paola Torres, Hainan Yu,
Margareta Nordin, Eric L. Hurwitz, Scott Haldeman, Christine Cedraschi
Department of Medical Informatics and Clinical Epidemiology,
Oregon Health and Science University,
Portland, OR, USA.
chour@ohsu.edu.
PURPOSE: The purpose of this review was to develop recommendations for the management of spinal disorders in low-income communities, with a focus on non-invasive pharmacological and non-pharmacological therapies for non-specific low back and neck pain.
METHODS: We synthesized two evidence-based clinical practice guidelines for the management of low back and neck pain. Our recommendations considered benefits, harms, quality of evidence, and costs, with attention to feasibility in medically underserved areas and low- and middle-income countries.
RESULTS: Clinicians should provide education and reassurance, advise patients to remain active, and provide information about self-care options. For acute low back and neck pain without serious pathology, primary conservative treatment options are exercise, manual therapy, superficial heat, and nonsteroidal anti-inflammatory drugs (NSAIDs). For patients with chronic low back and neck pain without serious pathology, primary treatment options are exercise, yoga, cognitive behavioral therapies, acupuncture, biofeedback, progressive relaxation, massage, manual therapy, interdisciplinary rehabilitation, NSAIDs, acetaminophen, and antidepressants. For patients with spinal pain with radiculopathy, clinicians may consider exercise, spinal manipulation, or NSAIDs; use of other interventions requires extrapolation from evidence regarding effectiveness for non-radicular spinal pain. Clinicians should not offer treatments that are not effective, including benzodiazepines, botulinum toxin injection, systemic corticosteroids, cervical collar, electrical muscle stimulation, short-wave diathermy, transcutaneous electrical nerve stimulation, and traction.
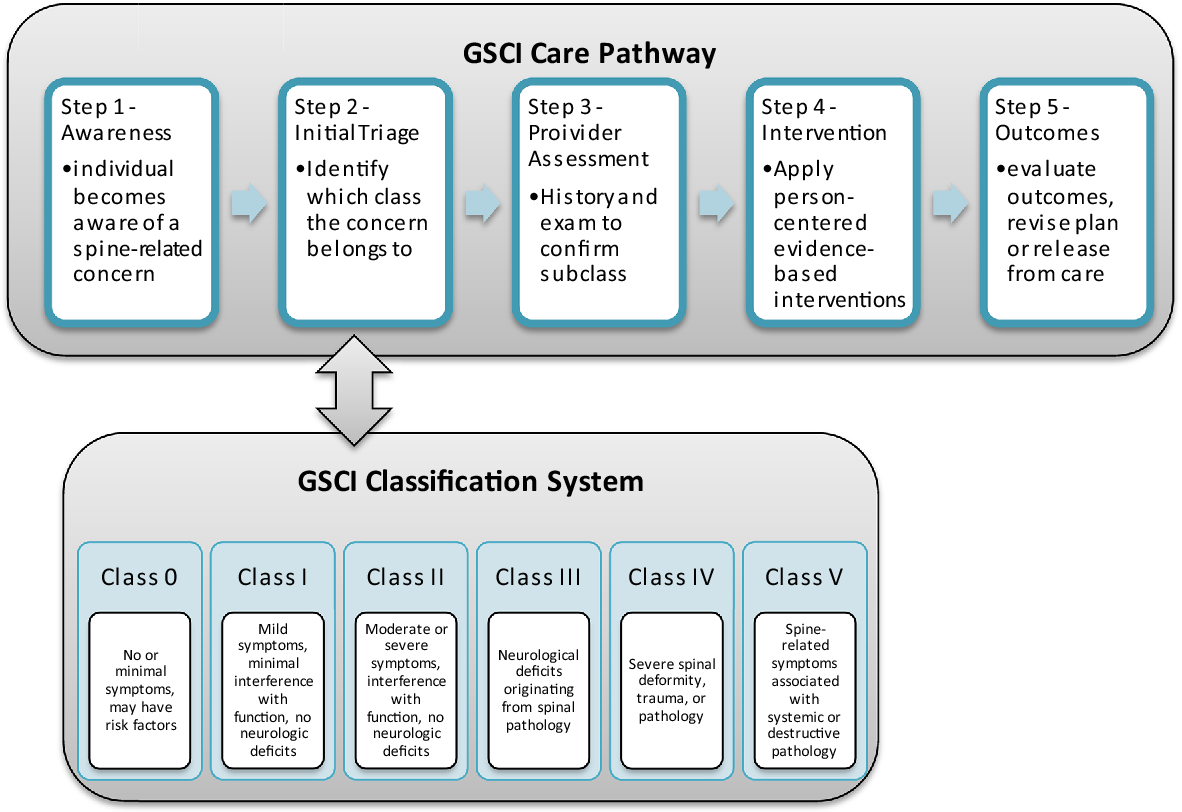
CONCLUSION: Guidelines developed for high-income settings were adapted to inform a care pathway and model of care for medically underserved areas and low- and middle-income countries by considering factors such as costs and feasibility, in addition to benefits, harms, and the quality of underlying evidence. The selection of recommended conservative treatments must be finalized through discussion with the involved community and based on a biopsychosocial approach. Decision determinants for selecting recommended treatments include costs, availability of interventions, and cultural and patient preferences. These slides can be retrieved under Electronic Supplementary Material.
KEYWORDS: Conservative treatment; Low back pain; Medically underserved area; Neck pain; Spine; Therapeutics
From the FULL TEXT Article:
Introduction
Spinal disorders are common worldwide. [1] They are a major contributor to the global disability burden and result in significant costs to health care and social security systems. [1. 2] The most common spinal disorders are nonspecific back and neck pain, which affect approximately one billion adults worldwide. [1] It is estimated that 8.9 and 4.8% of the world’s population, respectively, experienced low back pain (LBP) and neck pain, for longer than 3 months in 2013. [1] More importantly, low back and neck pain are the first and fourth most common disabling conditions worldwide. [1] Most spinal disorders are non-specific in that they cannot be reliably attributed to a specific underlying condition such as cancer, infection, ankylosing spondylitis, or other inflammatory or infectious diseases. [3] Although degenerative changes may be seen in patients with non-specific spinal disorders, such findings are common and age-related and their presence only weakly correlates with the presence and severity of symptoms. Only 1–2% of individuals with spinal pain have a serious pathology (e.g., cancer, infection, cauda equina syndrome). [4, 5] The prevalence of radicular LBP is about 12% or less, most commonly caused by disc herniation. [6, 7]
Evidence-based clinical practice guidelines are available to assist clinicians with the management of neck and LBP. These guidelines recommend that clinicians reassure patients that the prognosis of non-specific back and neck pain is favorable and advise patients to remain active. [8–10] First line pharmacologic options include nonsteroidal antiinflammatory drugs (NSAIDs) and acetaminophen, and recommended non-pharmacologic options include education, psychological interventions, exercise, spinal manipulation, and other complementary and alternative therapies. [11–14] The purpose of these interventions is to reduce pain, improve function, and address psychological contributors to pain. Prior guidelines have generally been developed based on literature conducted in high-income countries and for use in such settings. Feasibility and implementation in low- and middle income communities were not considered in prior guideline development efforts. [15]
The purpose of this article was to develop recommendations to the Global Spine Care Initiative care pathway and model of care for the management of non-specific low back and neck pain with a focus on non-invasive pharmacological and non-pharmacological therapies in medically underserved areas and low- and middle-income countries.
Methods
Development of recommendations
We selected two evidence-based clinical practice guidelines for the management of low back and neck pain without serious pathology. [13, 16] The LBP guideline was developed by the American College of Physicians and the American Pain Society (ACP/APS) and has been adopted by other groups including the US Department of Veterans Affairs and Department of Defense; an updated evidence review funded by the US Agency for Healthcare Research and Quality (AHRQ) was recently commissioned by the American College of Physicians to inform an update of this guideline. The neck pain guideline was commissioned by the Ontario Ministry of Finance to inform a reform of the automobile insurance system and was developed by the UOIT-CMCC Centre for Disability Prevention and Rehabilitation.
We focused on these two guidelines because they adhered to standards for developing high-quality guidelines; in addition two authors of this article led these guideline efforts. The LBP guideline was critically appraised by two systematic reviews of LBP clinical practice guidelines [9, 17] using the AGREE instrument. [18] The total quality score of the LBP guideline ranked 2nd among 14 guidelines published since 2004. Specifically, the domain of rigor of development scored 95% of the maximum possible score in the LBP guideline. Both guidelines meet criteria for development of high-quality guidelines including a clear scope and purpose, a comprehensive expert panel and sufficient stakeholder involvement, used systematic methods to search for evidence, clear description of strengths and limitations of the literature, explicit link between recommendations and supporting evidence, specific and clear recommendations, editorial independence, and reporting of competing interests.
The LBP guideline provides evidence-based recommendations for the management of LBP with or without radiculopathy of any duration. [16, 19] Specifically, LBP is classified into three categories: (1) nonspecific LBP; (2) back pain potentially associated with radiculopathy or spinal stenosis; and (3) back pain potentially associated with another specific spinal cause. The neck pain guideline provides evidencebased recommendations for the management of neck pain and associated disorders (NAD) grades I–III (see Online Resource Table 1) [20, 21] of less than 6 months duration. [13] Both guidelines aim to: (1) accelerate recovery; (2) reduce the intensity of symptoms; (3) promote early restoration of function; (4) prevent chronic pain and disability; (5) improve health related quality of life; (6) reduce recurrences; and (7) promote active participation of patients in their care. [13, 16]
Synthesis of recommendations
Two investigators (RC and PC) independently classified recommendations for each intervention addressed in the guidelines into four categories:(1) recommended for LBP alone;
(2) recommended for neck pain alone;
(3) recommended for both low back and neck pain; and
(4) recommended for LBP but not neck pain, or vice versa. We assessed recommendations for acute back or neck pain separately from chronic back or neck pain.We further classified each recommendation using the system proposed by the National Institute for Health and Care Excellence (see Online Resource Table 2). [22] Recommendations in the ACP/APS were adapted to conform to the NICE wording. Based on this methodology, recommendations start with the word "offer (recommended)" (for interventions that are of superior effectiveness compared to other interventions, placebo/sham interventions, or no intervention), "consider (recommended for consideration)" (for interventions providing similar effectiveness to other interventions), or "do not offer (recommended against)" (for interventions providing no benefit beyond placebo/sham or are harmful). Disagreements in how recommendations were classified were resolved through consensus of the primary authors (PC, RC).
For each intervention, one reviewer (PT, RC) extracted the available information regarding clinical benefits, harms, resources, and feasibility from the guidelines and accompanying systematic reviews, as well as the LBP evidence review update (see Online Resource Tables 3 and 4). A second reviewer (PT, RC) checked the data for accuracy and completeness by comparing the synthesized data with the data reported by the guidelines. We categorized the magnitude of benefits and harms as uncertain, low/small, moderate, or high/large based on the categories used in the recent AHRQ review on LBP interventions (see Online Resource Tables 2 and 3). We also rated costs and feasibility of each intervention for application in low-income communities. We categorized costs as low, moderate, or high based on the cost of the intervention (e.g., medication cost), cost of the personnel required to administer the intervention, and any facility or other costs required to deliver the intervention (e.g., spinal manipulation table, acupuncture needles, equipment for certain types of exercise therapy, EMG biofeedback). Given the lack of data on costs in low- and middle-income countries and variability in costs across countries, we used US and Canadian costs as a benchmark, unless information on differential costs in low- and middle-income settings was available. Feasibility was based on the availability of the intervention, the need for and availability of specially trained personnel to administer the intervention, regulatory or administrative constraints on the interventions, and the degree to which the intervention is sustainable (e.g., does it require ongoing training or new equipment).
For each intervention, we assigned final recommendations using the NICE categories, based on estimated benefits and harms, costs, and feasibility. For some interventions (e.g., muscle relaxants), evidence was available for LBP but not neck pain, or vice versa. In these situations, to generate final recommendations, the authors determined whether evidence from one condition could reasonably be extrapolated to the other. To the extent possible, the authors sought to have consistent recommendations on interventions for low back and neck pain, to promote a consistent approach to spinal disorders, and facilitate implementation in low-income community settings, including those in which health care is provided by persons with limited training.
Results
Recommendation 1: management of low back and neck pain without serious pathology: education and self-care
Clinicians should educate and reassure patients about benign and self-limited nature of the typical course of spinal disorders without serious pathology, advise patients to remain active, and provide information about effective selfcare options. Patients should be counseled on the need for re-evaluation if they develop worsening symptoms or fail to improve.
Education and self-care require few resources, can be implemented in all clinical settings, and are considered a core spinal pain intervention. Education should take into account the general favorable natural history of acute spinal pain, with most patients experiencing substantial improvements in the first 4–6 weeks. In addition, the approach to education and self-care should emphasize interventions that focus on maintenance of function, reducing maladaptive coping strategies that may contribute to the development of persistent disabling spinal pain, and actively engaging patients in their care. Clinicians should provide care in partnership with the patient and involve the patient in care planning and decision-making. Maladaptive coping strategies include beliefs that activity is unsafe and should be avoided (fear avoidance) or that low back pain will never improve (catastrophizing). Instruments that have been validated in high-income countries for assessing fear avoidance and catastrophizing are available; alternatively, for a simple screen clinicians could use items 5 through 7 of the STarT Back Screening Tool. [23] However, these tools need to be cross-culturally validated for use in low- and middle-income countries. To address maladaptive coping strategies, clinicians should reassure patients that, in the majority of cases, spinal pain is benign and has a self-limited course. Patients should be educated about the benefits of remaining active. For symptom relief, patients can be counseled on use of superficial heat. Patients should also be counseled on the need for re-evaluation if they fail to improve or develop worsening or new symptoms.
Recommendation 2: management of acute low back and neck pain without serious pathology (Tables 1, 2)

Table 1

Table 2 For patients with acute spinal disorders without serious pathology, exercise, cognitive behavioral therapies, manual therapy, and multimodal approaches can be considered as non-pharmacological interventions. Clinicians may consider the use of NSAIDs as a first-line medication option. A short course of skeletal muscle relaxants may also be considered but should not be prescribed routinely.
For patients with acute low back and neck pain without serious pathology, clinicians may offer non-pharmacological therapies and medications in conjunction with education and self-care, for patients who do not improve with self-care alone. Selection of non-pharmacological therapies should be based on a biopsychosocial approach that emphasizes treatments that focus on improvement in function and that more actively address psychological and social contributors to pain. These include exercise, cognitive behavioral, or manual therapies. Manual therapy (e.g., manipulation and/ or mobilization) can be used in conjunction with exercise. Medication options for symptomatic relief are NSAIDs, based on small benefits, small risk of harms in appropriately selected patients, and low costs. Skeletal muscle relaxants can also be considered for short-term symptom relief but are not considered a first-line medication option due to a high risk of central nervous system (CNS) harms (e.g., sedation). [11] Decisions regarding selection of therapies for acute LBP should be informed by the natural history, which indicates marked improvement in the majority of patients over the first 4 weeks. Factors that influence the selection of therapies for acute LBP include costs, patient preferences, and whether the intervention is readily available and can be delivered in a timely manner. For interventions that are more costly or that have limited availability, a reasonable strategy would be to prioritize their use for patients who do not improve with alternative options, are at higher risk for chronic disabling LBP, or have strong preferences for their use.
Although prior guidelines recommended acetaminophen as an option for acute pain, a recent well-conducted trial found acetaminophen ineffective to promote recovery in patients with acute LBP [24]; more trials are needed to confirm this finding. In addition, the trial focused on outcomes at set time points (e.g., 1 week, 2 weeks, 4 weeks, 3 months), rather than on short-duration relief of symptoms in the few hours after taking the acetaminophen. [24] Therefore, the role of acetaminophen for temporary relief of acute spine pain is uncertain. Given its low costs and small harms in appropriately selected, including consideration of genetic differences in and otherwise healthy patients, it may be a reasonable option for short-term relief when used as needed. It may also provide an alternative to NSAIDs, particularly in patients at higher risk for NSAID-related adverse events.
Recommendation 3: management of chronic low back and neck pain without serious pathology (Tables 3, 4)

Table 3

Table 4 For patients with chronic spinal disorders without serious pathology, recommended non-pharmacological options are exercise and yoga; clinicians may also consider non-pharmacological options such as psychotherapy, (e.g., cognitive behavioral therapies), acupuncture, biofeedback, low-level laser, clinical massage, manual therapy, multidisciplinary/ multimodal rehabilitation, progressive relaxation, or psychological therapies. Pharmacologic options include NSAIDs (first-line therapy), acetaminophen, or antidepressants. Opioids may also be considered in carefully selected patients, but they should be used with caution.
The natural history of spinal pain that lasts > 3 months is for ongoing, persistent symptoms and is often accompanied by significant functional limitations. Similar to acute low back and neck pain, clinicians may offer pharmacological and non-pharmacological therapies in conjunction with self-care and education. Although pharmacological therapies may provide some symptomatic relief in patients with chronic low back and neck pain, they are “passive” and do not address the psychological or social factors that often contribute to persistent disabling spinal disorders. Therefore, non-pharmacological therapies that actively address such psychological and social factors and target improvement in function are a core component of management. First-line non-pharmacological therapy options that are effective for chronic low back and neck pain include exercise, massage, mindfulness-based interventions (e.g., yoga, mindfulnessbased relaxation), and psychological therapies (e.g., cognitive behavioral therapies, progressive relaxation, biofeedback); provision of all of these therapies requires health care personnel with the requisite training, and in some cases (e.g., biofeedback) may require specialized equipment. For individuals who do not receive manual therapy and exercise during the acute phase, a course of manual therapy combined with exercise may be considered. Although multidisciplinary/ multimodal rehabilitation that includes exercise-based and psychological therapies may be more effective than single modality interventions, it should generally be reserved for high-risk patients or those who do not improve using other therapies, due to high costs; in addition this intervention is unlikely to be available in many low resource settings. In conjunction with non-pharmacologic therapies, first-line pharmacological therapy options are NSAIDs and acetaminophen, given low costs, some benefits, and small harms in appropriately selected patients. Antidepressants such as tricyclic antidepressants (TCAs) and serotonin–norepinephrine reuptake inhibitor (SNRIs) are a second-line option. Although they are associated with some benefits, TCAs are associated with frequent side effects and SNRIs are generally more costly, without clearly being more effective than acetaminophen or NSAIDs. [11] However, in patients with concomitant depression or anxiety, antidepressants may be considered a preferred option for their analgesic effects as well as effects on psychiatric co-morbidities. Opioids should be used with caution in patients with chronic low back and neck pain, given the risk of serious harms, modest shortterm benefits, and lack of evidence on long-term benefits. Opioids may result in physical dependence, addiction, and rare non-fatal unintentional overdose and death. [25] They should only be prescribed in appropriately selected patients and require diligent monitoring and follow-up of response to determine if ongoing treatment is warranted. [25] Individuals with active substance use disorder should not be prescribed opioids except in the context of treatment for opioid use disorder.
Recommendation 4: management of low back and neck pain with radiculopathy (Tables 5, 6)

Table 5

Table 6 For patients with spinal pain with radiculopathy, clinicians may consider the use of NSAIDs as first-line medication and exercise or spinal manipulation as non-pharmacologic therapy.
Evidence on the effectiveness of interventions for low back and neck pain associated with radiculopathy is limited. Some evidence suggests that NSAIDs, exercise, and manipulation may be effective in persons with radicular LBP. [9, 16, 19] Although gabapentin, pregabalin, and duloxetine are approved to treat other neuropathic pain conditions, their effectiveness for radicular spinal pain has not been clearly demonstrated. [19] Recent analyses of these medications are associated with adverse events, including CNS adverse events. Therefore, there is insufficient evidence to determine the appropriate use of these medications for radicular spinal pain. For non-pharmacological therapies other than exercise and manipulation, there was insufficient evidence to make evidence-based recommendations regarding use for radicular spinal pain. Decisions about the use of such interventions may be informed by extrapolation from evidence regarding benefits and harms for non-radicular spinal pain.
Recommendation 5: Interventions that should not be offered for the management of
low back and neck pain without serious pathology
Clinicians should not offer benzodiazepines, systemic corticosteroids, botulinum toxin injection, cervical collar, electrical muscle stimulation, short-wave diathermy, TENS and traction (Tables 1, 2, 3, 4, 5, 6).
The above interventions are recommended against due to evidence showing harms outweighing benefits or evidence indicating ineffectiveness. Among recommended non-pharmacological interventions, such as acupuncture, massage, superficial heat, and progressive relaxation, evidence for certain specific or related techniques (e.g., electroacupuncture, relaxation massage, strain–counterstrain, moist heat, standalone relaxation training) have not shown effectiveness, or have limited evidence to support them. However, trials directly comparing different techniques within an intervention have generally been unable to show clear differences in effectiveness. More research is needed to understand the optimal methods for delivering these non-pharmacological interventions, as well as the optimal intensity and duration of treatment.
Discussion
We used two evidence-based clinical practice guidelines to determine options for interventions that can be considered for the the management of non-specific spinal pain without serious pathology and radiculopathy. The two guidelines did not provide recommendations specific to low- and middleincome countries; however, based on an assessment of benefits and harms as well as resources and feasibility of the interventions recommended in the guidelines, we developed recommendations that may be appropriate for these settings and populations. However, clinicians should be aware of local circumstances that may inform selection of recommended therapies (e.g., genetic polymorphisms or presence of cultural or social factors potentially impacting acceptability or effectiveness). After our recommendations had been developed, ACP issued an updated guideline on management of low back pain. [26] Differences between the updated guideline and the previous ACP/APS guideline include a greater emphasis on use of non-pharmacological over pharmacological therapies, particularly for chronic low back pain, removed acetaminophen as a recommended treatment, emphasized cautious and limited use of opioids, and recommended mindfulness-based stress reduction as an additional treatment option for chronic low back pain. Although we were unable to formally include the updated ACP guideline, the recommendations in this article are consistent with it.
The recommended approach to use of non-invasive interventions for low back and neck pain is predicated on evidence showing benefits outweighing harms. The approach emphasizes self-care and education and non-pharmacological therapies, particular those that “actively” focus on movement and addressing psychological and social contributors to pain, in order to more effectively engage patients in care and improve function as well as pain. Importantly, recommended interventions for the management of low back and neck pain in medically underserved areas and low- and middle-income countries must be affordable and accessible. [27] However, there is a knowledge gap regarding the management of spinal pain in these communities. Therefore, evidence-based treatment recommendations must be relevant and their implementation feasible within these communities. The available literature from the developing world is of limited use to inform the management of spinal pain in small communities because most studies were conducted in high-resource settings. [28] Recommendations suitable in medically underserved areas and low- and middle-income countries should take into consideration resources requirements and the feasibility of interventions. Implementing evidence-based recommendations could improve quality of care and reduce costs in health care systems. Given the resource limitations in low-income settings, it is especially important to implement evidence-based care that is both effective and efficient, while avoiding unnecessary and ineffective treatments.
Limitations
Two evidence-based clinical practice guidelines were used for the recommendations. The recommendations are for the management of spinal pain, specifically for neck and back pain. These recommendations may not be appropriate for the management of thoracic pain. However, the most commonly reported spinal disorders are back and neck pain, and evidence on interventions for thoracic back pain are extremely limited. A reasonable approach may be to extrapolate recommendations on management of low back and neck pain to thoracic back pain. We recommend that clinicians, insurers, and policy-makers use the ADAPTE framework to adapt this guideline to their needs and environment. [29] Research is needed to understand effects of implementing these recommendations in low- and middle-income settings, understand optimal sequencing and prioritization of therapies, and clarify effective treatments for management of radiculopathy and thoracic back pain.
Conclusion
Guidelines developed for high-income settings were adapted to inform a care pathway and model of care for medically underserved areas and low- and middle-income countries by considering factors such as costs and feasibility, in addition to benefits, harms, and the quality of underlying evidence. The selection of recommended conservative treatments must be finalized through discussion with the involved community and based on a biopsychosocial approach. Decision determinants for selecting recommended treatments include costs, availability of interventions, and cultural and patient preferences. This information can be used to inform the GSCI care pathway and model of care in medically underserved areas and low- and middle-income countries.
Acknowledgements
We thank Leslie Verville for her contributions to this paper.
Funding
The Global Spine Care Initiative and this study were funded by grants from the Skoll Foundation and NCMIC Foundation. World Spine Care provided financial management for this project. The funders had no role in study design, analysis, or preparation of this paper.
References:
Global Burden of Disease 2013 Collaborators (2013)
Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 301 Acute
and Chronic Diseases and Injuries in 188 Countries, 1990-2013: A Systematic Analysis
for the Global Burden of Disease Study 2013
Lancet. 2015 (Aug 22); 386 (9995): 743–800Hogg-Johnson, S, van der Velde, G, Carroll, LJ et al.
The Burden and Determinants of Neck Pain in the General Population: Results of the
Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S39–51Savigny P, Kuntze S, Watson P, Underwood M, Ritchie G, Cotterell M, Hill D, Browne N (2009)
Low Back Pain: Early Management of Persistent Non-specific Low Back Pain
London, UK: National Collaborating Centre for Primary Care and
The Royal College of General Practitioners; 2009.Gozna E (2001)
Guidelines for the Diagnosis and Treatment of Low Back Pain
Workplace Health, Safety and Compensation Commission of New Brunswick, New BrunswickLærum E, Dullerud R, Kirkesola G, Mengshoel A, Nygaard Ø, Kouen J (2002)
Acute Low Back Pain: Interdisciplinary Clinical Guidelines
Oslo, UK: The Norwegian Back Pain Network; 2002Deyo RA, Tsui-Wu YJ (1987)
Descriptive epidemiology of lowback pain and its related medical care in the United States.
Spine 12(3):264–268Bogduk N (2005)
Clinical anatomy of the lumbar spine and sacrum.
Elsevier Health Sciences, LondonKoes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C.
An Updated Overview of Clinical Guidelines for the Management of Non-specific Low Back Pain
in Primary Care
European Spine Journal 2010 (Dec); 19 (12): 2075–2094Wong JJ, Cote P, Sutton DA, et al.
Clinical Practice Guidelines for the Noninvasive Management of Low Back Pain: A Systematic Review
by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration
European J Pain 2017 (Feb); 21 (2): 201–216Wong JJ, Côté P, Shearer HM, Carroll LJ, Yu H, Varatharajan S, Southerst D (2015)
Clinical practice guidelines for the management of conditions related to traffic collisions:
a systematic review by the OPTIMa Collaboration.
Disabil Rehabil 37(6):471–489Chou R, Huffman LH;
Medications for Acute and Chronic Low Back Pain: A Review of the Evidence for an
American Pain Society/American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 505–514Chou R, Huffman LH; American Pain Society.
Nonpharmacologic Therapies for Acute and Chronic Low Back Pain:
A Review of the Evidence for an American Pain Society/
American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 492–504Côté P, Wong JJ, Sutton D, Shearer HM, Mior S, Randhawa K, Ameis A, Carroll LJ (2016)
Management of neck pain and associated disorders: a clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration.
Eur Spine J. https ://doi.org/10.1007/s0058 6-016-4467-7Hurwitz EL, Carragee EJ, van der Velde G, Carroll LJ, Nordin M, Guzman J, Peloso PM(2008)
Treatment of Neck Pain: Noninvasive Interventions: Results of the Bone and Joint Decade
2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123–152Mousavi SJ, Akbari ME, Mehdian H, Mobini B, Montazeri A, Akbarnia B (2011)
Low back pain in Iran: a growing need to adapt and implement evidence-based practice
in developing countries.
Spine 36(10):E638–E646. https ://doi.org/10.1097/BRS.0b013 e3181 fa1da 2Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr., Shekelle P, Owens DK:
Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline
from the American College of Physicians and the American Pain Society
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 478–491Bouwmeester W, van Enst A, van Tulder M (2009)
Quality of low back pain guidelines improved.
Spine 34(23):2562–2567. https ://doi.org/10.1097/BRS.0b013 e3181 b4d50 dAGREE (Appraisal of Guidelines R, and Evaluation in Europe) Collaborative Group (2000)
Guideline development in Europe. An international comparison.
Int J Technol Assess Health Care 16(4):1039–1049Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al.
Noninvasive Treatments for Low Back Pain
Comparative Effectiveness Review no. 169
(Prepared by the Pacific Northwest Evidence-based Practice Center under contract no. 290-2012-00014-I.)
AHRQ publication no. 16-EHC004-EF. Rockville:
Agency for Healthcare Research and Quality; February 2016Guzman J, Hurwitz EL, Carroll LJ, Haldeman S, Côté P, Carragee EJ, Peloso PM (2008)
A New Conceptual Model Of Neck Pain: Linking Onset, Course, And Care
Results of the Bone and Joint Decade 2000–2010 Task Force on
Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S14–23Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73National Institute for Health and Care Excellence (NICE) (2012)
The guidelines manual.
https://www.nice.org.uk/article/pmg6/chapter/introduction#ftn.footnote_1
Accessed 16 May 2016Hill JC, Whitehurts DG, Lewis M, Bryan S, Dunn KM, Foster NE, Konstantinou K, Main CJ (2011)
Comparison of Stratified Primary Care Management for Low Back Pain
with Current Best Practice (STarT Back): A Randomised Controlled Trial
Lancet. 2011 (Oct 29); 378 (9802): 1560–1571Williams CM, Maher CG, Latimer J, McLachlan AJ, Hancock MJ, Day RO, Lin CW (2014)
Efficacy of paracetamol for acute low-back pain: a double-blind, randomised controlled trial.
Lancet (London, England) 384(9954):1586–1596. https ://doi.org/10.1016/s0140 -6736(14)60805 -9The Centers for Disease Control and Prevention (2011)
Policy impact: prescription painkiller overdoses. https ://www.cdc.gov/drugo verdo se/pubs/index .html#tabs-76009 4-4
Accessed 28 Sept 2016Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530World Health Organization (2007)
WHO normative guidelines on pain management.
Report of a Delphi Study to determine the need for guidelines and to identify the number
and topics of guidelines that should be developed by WHO.
Geneva, SwitzerlandSize M, Soyannwo OA, Justins DM (2007)
Pain management in developing countries.
Anaesthesia 62(Suppl 1):38–43. https ://doi.org/10.1111/j.1365-2044.2007.05296 .xADAPTE Collaboration (2009)
Guideline adaptation: a resource toolkit.
http://www.g-i-n.net/docum ent-store /worki ng-groups-docum ents/adapt ation/adapt e-resou rce-
toolk it-guide line-adaptation -2-0.pdf
Accessed 2 June 2016
Return to LOW BACK PAIN
Return to LOW BACK GUIDELINES
Return to GLOBAL BURDEN OF DISEASE
Since 8-10-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |