FROM:
European Spine Journal 2018 (Jul); 27 (7): 1526–1537 ~ FULL TEXT
Martha Funabashi, Gregory N. Kawchuk, Albert H. Vette, Peter Goldsmith, and Narasimha Prasad
Department of Physical Therapy,
University of Alberta,
Edmonton, AB, Canada.
Spinal manipulative therapy (SMT) creates health benefits for some while for others, no benefit or even adverse events. Understanding these differential responses is important to optimize patient care and safety. Toward this, characterizing how loads created by SMT relate to those created by typical motions is fundamental. Using robotic testing, it is now possible to make these comparisons to determine if SMT generates unique loading scenarios. In 12 porcine cadavers, SMT and passive motions were applied to the L3/L4 segment and the resulting kinematics tracked. The L3/L4 segment was removed, mounted in a parallel robot and kinematics of SMT and passive movements replayed robotically. The resulting forces experienced by L3/L4 were collected. Overall, SMT created both significantly greater and smaller loads compared to passive motions, with SMT generating greater anterioposterior peak force (the direction of force application) compared to all passive motions. In some comparisons, SMT did not create significantly different loads in the intact specimen, but did so in specific spinal tissues. Despite methodological differences between studies, SMT forces and loading rates fell below published injury values. Future studies are warranted to understand if loading scenarios unique to SMT confer its differential therapeutic effects.
From the FULL TEXT Article:
Introduction
Low back pain — the leading cause of global disability [1] —
is recognized as an important public health concern, because
it is associated with considerable burden to individuals,
industry, and society. [2–5] It affects about 70% of all people
in their lifetime, and between 15 and 30% on any given day,
with varying types of clinical presentations. [6–8] Symptomatic
lumbar disc herniation (LDH) can be one of the most
recognizable presentations of low back pain. The diagnosis
is typically based on a combination of symptoms and signs
suggesting lumbar spinal nerve root compression or irritation
including: lumbosacral radiculopathy (i.e., radicular
leg pain or “sciatica”), nerve root tension signs, neurologic
deficits (i.e., muscle weakness and reflex changes), and
advanced imaging (i.e., MRI or CT) findings that correlate
with the clinical syndrome. [9–11] However, many patients
present with a less clear clinical picture involving low back
pain in the early (prodromal) phase that then progresses to
radicular leg pain with or without neurologic signs. [12, 13]
In addition, diagnostic imaging may only be indicated in the
prodromal phase if there is suspicion of serious underlying
pathology (e.g., infection or malignancy). [14] These factors
contribute in making diagnosis during the early course of
symptomatic LDH especially difficult.
In North America, back pain is managed primarily by
physicians, chiropractors, and physical therapists. [15]
Approximately 12% of American and Canadian adults seek
chiropractic care annually, and about 95% of chiropractic
visits involve spinal manipulation treatment. [16–19] Several
systematic reviews suggest that chiropractic spinal manipulation
can benefit low back pain, but the summarized studies
are of varying quality and too small to evaluate the risk
for rare serious adverse events. [20–25] In addition, there
is evidence from randomized clinical trials showing benefit
of spinal manipulation for the management of LDH with
radiculopathy [26–28], yet little is known about the safety of
this treatment. To date, no valid epidemiologic assessment
of the risk for acute disc herniation following chiropractic
treatment is available in the scientific literature. [29, 30] The
current literature presents case reports and small case series
linking lumbar spine manipulation to disc herniation and
cauda equina syndrome. [31] However, case reports offer the
lowest level of scientific evidence with regard to the determination
of risk and cannot be used to make valid inferences
about the lack of safety of a treatment. They have, however,
raised a hypothesis of potential harm.
Individuals in the early prodromal phase of a symptomatic
LDH often complain of back pain. [12, 13] As the
condition progresses, most develop sciatica. At different
points in time along this course, they may seek healthcare
for assessment and intervention. If chiropractic treatment
occurs before an LDH progresses to radiculopathy or neurologic
deficit and is thus diagnosed, then the treatment
itself can be erroneously blamed for causing the LDH. This
systematic error — known as protopathic bias — is a type of
reverse-causality bias due to processes that occur before a
diagnosed or measured outcome event. [32, 33] Given that
LDH can initially present as low back pain, it is possible that
these patients seek chiropractic care in the prodromal phase
of LDH [34], implying that an observed association between
chiropractic care and acute LDH may not be causal. Since
patients also commonly see primary care physicians (PCPs)
for back pain and this healthcare encounter is unlikely to
cause disc herniation, an observed association between PCP
visits and acute LDH could be attributed to care seeking for
the initial symptoms of LDH (protopathic bias).
Rigorous epidemiological studies are needed to assess
the possibility of increased risk for acute LDH following
chiropractic care. Our objective was to investigate and compare
the associations between both chiropractic and PCP
care, and acute LDH with incident early surgery using the
self-controlled case series method and population-based
healthcare data from Ontario, Canada. We hypothesized that
evidence that chiropractic care increases the risk for acute
LDH would be present if the measured association between
chiropractic visits and acute LDH exceeds the association
between PCP visits and acute LDH.
Methods
Data sources
We combined data from four population-based healthcare
databases, totaling over 100 million person-years of observation:
(1) the Ontario Registered Persons Database;
(2) the Discharge Abstract Database (DAD);
(3) the National Ambulatory Care Reporting System (NACRS); and
(4) the Ontario Health Insurance Plan Billings Database (OHIP).
These administrative health data include information on
patients’ hospitalizations and surgeries, emergency department
(ED) visits, and practitioner (chiropractor and physician)
and other healthcare utilization as documented by
fee-for-service billings. Linkage between data sets used
encrypted health card numbers as unique identifiers, and all
health information obtained was anonymous. We requested
and received these data from the Health Data Branch of the
Ontario Ministry of Health and Long-Term Care. Research
ethics board approval was received at the University Health
Network (REB #09-0668-AE).
Study design
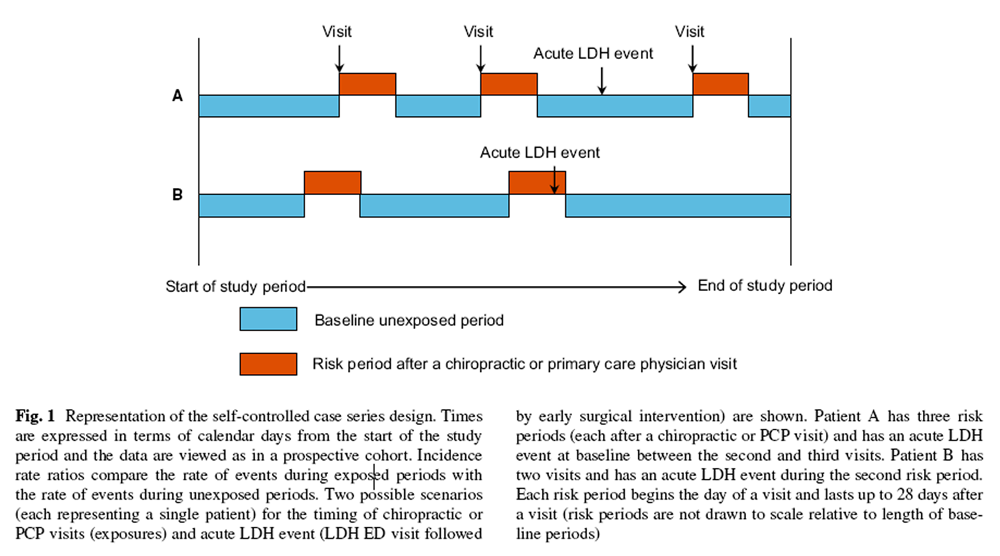 Figure 1
Figure 1
|
The self-controlled case series method is a cohort study in
which the relative risk is based on within-person comparisons
rather than between-person comparisons, with each
person contributing to both the exposed and unexposed
observation time (i.e., a case-only design). [35, 36] Using
patients as their own controls, the design produces estimates
that are controlled for variables, such as sex and genetics,
that are fixed (time-invariant) over the observation period.
This design is most appropriate when a brief, well-defined
exposure (e.g., a chiropractic or PCP visit) is associated with
a transient change in risk for a rare-onset disease or event
(e.g., acute LDH with early surgery). The main advantage
of this design is that inference is within a person, so that
the confounding effects of both known and unknown confounders
that do not vary with time during the observation
period are eliminated by design.
Figure 1 illustrates the self-controlled
case series design.
Source population
All Ontario residents, aged 18 years or older, who were covered
by the provincial universal healthcare system between
April 1, 1992 and November 30, 2004, were the source population.
We had to limit the study period to November 30,
2004, because this was the last date that chiropractic care
was covered by the universal healthcare plan in Ontario, limiting
our ability to identify chiropractic visits after this date.
Members of the armed forces, federal inmates, the Royal
Canadian Mounted Police, and First Nation individuals living
on reserves were ineligible for the study, as they have
federal rather then provincial healthcare coverage.
Outcome and case definition
We used the following four-step approach to define cases
of acute LDH with incident early surgery (codes detailed in
Online Resource 1):
Cases of incident LDH surgery between April 1, 1994
and November 30, 2004, with at least 2 years of healthcare
coverage prior to their surgery (so that exposure
visits to chiropractors and PCPs could be extracted),
were identified using at least one disc surgery intervention
code and one LDH diagnosis code from DAD or
NACRS data. Hospital discharge codes for LDH have
been shown to have a high positive predictive value
(93%) when compared to chart review. [37]
Candidate cases of acute LDH with incident early surgery
were then identified using OHIP and NACRS data
by including persons from Step 1 who presented to
a hospital ED for LDH within 8 weeks prior to their
LDH surgery. The 8–week ED visit window (ED window)
prior to LDH surgery was chosen in consultation
with a spine surgery expert and evidence, suggesting
that early surgery for severe or intractable radiculopathy
due to disc herniation can occur 6–12 weeks following
the onset of symptoms. [38, 39] We hypothesized that
this outcome event scenario (ED visit for LDH followed
by early surgical intervention) would most reliably represent
a clinically relevant acute LDH event (i.e., acute
LDH conceptualized as a rare serious adverse event
following chiropractic treatment) that could be reproducibly
identified using administrative health data. The
event index date was defined as this date of service for
LDH at the ED within 8 weeks prior to the LDH surgery
date.
Using DAD and NACRS data, we excluded persons who
had a diagnosis of LDH or other conditions potentially
associated with LDH, 21 months prior to their event
index date (the maximum time window for which we
could consistently apply exclusions prior to the index
date given access to up to 2 years of healthcare utilization
data prior to patients’ surgery date). Excluded also
were those with other spine surgery interventions on or
prior to their date of incident LDH surgery.
Using OHIP data, we excluded persons who had, within
21 months prior to their event index date, a diagnosis
of LDH or other conditions potentially associated with
LDH, specialist visits to neurosurgeons, orthopaedic
surgeons, neurologists, physiatrists and rheumatologists,
or advanced spine imaging or diagnostic testing related
to LDH. Long-term care patients in the 2 years prior to
LDH surgery were also excluded.
Exposures
Healthcare visits to chiropractors and PCPs were the
exposures of interest. In the 1–year period before the
event index date, we identified all ambulatory care billing
records for chiropractic and PCP visits in the OHIP
data (codes detailed in Online Resource 2). Multiple billings
of the same type on the same date were counted as
one visit. Lumbar spine-related chiropractic visits were
defined using chiropractic diagnosis codes: C07–C09,
lumbar, lumbosacral, sacroiliac, and coccyx subluxation;
C13–15, multiple site subluxation; C20–24, acquired,
postural or congenital spine curvature; C31–C32, lumbosacral
sprain/strain. For PCP visits, we included community
medicine physicians if they submitted ambulatory
fee codes to OHIP. PCP visits for natal care, ophthalmology
care, genetic screening, and group counselling were
excluded. Lumbar spine-related PCP visits were identified
using diagnosis codes: 724, lumbar strain, lumbago,
coccydynia, sciatica; and 847, low back, coccyx sprain/
strain.
Statistical analysis
For descriptive purposes, we identified cases with a diagnosis
of diabetes, hypertension, coronary heart disease,
high cholesterol, osteoarthritis, and rheumatoid arthritis
using OHIP billing diagnosis codes during the 2 years
prior to their LDH surgery. We defined each condition
according to the following OHIP diagnosis codes: diabetes
(code 250), hypertension (codes 401–403), coronary
heart disease (codes 410–415 and 426–429), high cholesterol
(code 272), osteoarthritis (code 715), and rheumatoid
arthritis (code 714).
An important assumption underpinning the standard
self-controlled case series method is that the occurrence of
an event must not alter the probability of subsequent exposure.
However, this assumption does not hold for healthcare
exposures such as chiropractic or PCP visits, because
the occurrence of acute LDH requiring early surgery likely
influences the probability of post-event visits to a chiropractor
or PCP. Therefore, we used a validated approach
to estimate the relative incidence that was designed to
address this curtailment of exposures and that uses only
exposures experienced prior to the event. [35, 40, 41]
The observation time in the year prior to the index acute
LDH ED visit was divided into risk periods and baseline
(unexposed) time. We ran analyses with risk periods
of four different lengths:
(1) 0–2 days after a visit,
(2) 0–7 days after a visit,
(3) 0–14 days after a visit, and
(4) 0–28 days after a visit; the baseline period comprised remaining unexposed time.
To estimate the associations
between acute LDH and chiropractic care, and acute LDH
and PCP care, we used conditional Poisson regression to
calculate incidence rate ratios (IRRs) and 95% confidence
intervals for events occurring within each risk period compared
to baseline. [35, 39–42] In the case of overlapping
risk periods, we adopted a convention used in the selfcontrolled
case series method: later exposure visits take
precedence over earlier ones. [36] Separate analyses were
conducted for exposure to any chiropractic and PCP visits,
and lumbar spine-related chiropractic and PCP visits. All
analyses were performed using R, version 2.15.1. [46]
We examined the annual number of events by fiscal year
of data (1–April to 31–March) and observed an unequal
distribution of events corresponding to the implementation
of the NACRS database in the Ontario healthcare
system beginning in 2002. The implementation of the
NACRS introduced a new administrative health database
for ED and day surgery services along with ICD–10 codes
for diagnoses and interventions within these settings. To
assess the impact of event misclassification that may have
been related to the initiation of the NACRS on April 1,
2002, we also calculated “NACRS-adjusted” risk estimates
for all analyses.
We ran several sensitivity analyses:
(1) To investigate the
effect of different time intervals defining “early” surgery
after an acute LDH ED visit, we also examined time intervals
of 4 and 12 weeks between an ED LDH visit and LDH
surgery date.
(2) To examine the impact of potential misclassification
of the event diagnosis, we repeated analyses using
a broader (more sensitive) set of codes for LDH diagnosis
on the index date (Online Resource 1).
(3) To assess the
effect of visits to chiropractors and PCPs that occurred on
the event index date (event-day exposures leading to possible
reverse-causality associations), we ran analyses with a 1–day
lag on exposure dates to estimate incidence ratios excluding
event-day exposure visits.
(4) Where possible, we also
performed analyses in subgroups of patients whom only had
chiropractic care and those whom only had PCP care during
their observation period.
Finally, we used the nonparametric bootstrap for two
additional analyses:
(1) To check the model-based confidence
intervals for our primary model IRR estimates, we
took 2000 bootstrap resamples from the cases of acute LDH
with early surgery and refitted the models for both DC visits
and PCP visits to each sample. The 2.5th and 97.5th percentiles
of the 2000 estimates of the IRRs were used to estimate
the 95% confidence interval for the IRR;
(2) for each of the
bootstrap samples, we divided the IRR for a DC visit by the
IRR for a PCP visit, thereby estimating the specific effect
on the risk for acute LDH with early surgery of seeing a
chiropractor relative to seeing a PCP.
Role of the funding source
The sponsors of the study had no role in study design, data
collection, data analysis, data interpretation, the writing
of the report, or in the decision to submit the report for
publication.
Results
Identification of acute LDH cases
A total of 36,745 persons were identified with incident disc
surgery during the study period. Of these, we excluded 423
that were under 18 years of age at the time of their surgery,
180 with a history of long-term care service in the 2 years
prior to their surgery, 9,576 with no LDH diagnosis linked
to their disc surgery, 25,323 with no ED LDH visit within
8 weeks prior to their LDH surgery date, and 1,048 with
prevalent LDH or associated diagnoses and interventions
within 21 months prior to the acute LDH event index date.
Figure 2 shows the case selection and exclusions process. For our primary analysis, 195 cases of acute LDH requiring
ED visit and early surgery met our case definition criteria,
and are described in Table 1. The mean age of cases was
43 years at the LDH surgery date, and 60% were male. Of
the 195 cases, 72 (37%) had visited a chiropractor during the
observation period starting 12 months prior to their event
index date, while 186 (95%) had visited a PCP within that
time. Comorbidities were as common in patients with chiropractic
visits as in patients with PCP visits.
Description of visits
Overall, 22% of cases had a chiropractic visit within 14 days
prior to the event index date, while 59% of cases had a PCP
visit within that same time interval (Table 2). A total of 57
cases were identified during the first 8 years of the study
period (April 1, 1994–March 31, 2002). 138 cases were
identified during the balance of the study period (April 1,
2002–November 30, 2004), which corresponded with the
initiation of the NACRS database for ED services in Ontario,
on April 1, 2002. Table 2 shows that visits were just as common
prior to the 2002 fiscal year (pre-NACRS) as they were
after the start of the NACRS database. For instance, among
cases whose event occurred prior to the 2002 fiscal year,
16% had consulted a chiropractor within 7 days of their
index date, and 47% had consulted a PCP within the same
interval. Among cases whose event occurred after the start
of the NACRS database (event fiscal year ≥ 2002), 21% had
consulted a chiropractor within 7 days of their index date,
and 44% had consulted a PCP within the same interval.
Self-controlled case series results
We found evidence of positive associations between chiropractic
visits and acute LDH with early surgery regardless
of the length of the risk period (Table 3). For the risk period
0–7 days after a chiropractor visit, there was a total of 9
patient-years of exposed time and 38 patients experienced
an acute LDH with early surgery event. The adjusted IRR for
this exposed period was 12.9 (95% CI 7.2–23.3).
There was similar evidence of strong positive associations
between PCP visits and acute LDH with early surgery for all
risk periods up to 28 days after a visit (Table 3). In a total of
28 patient-years of exposed time 0–7 days after a PCP visit,
87 persons experienced an acute LDH event, resulting in an
IRR of 14.5 (95% CI 9.9–21.2).
When restricting the analyses to visits related to lumbar
spine complaints, we observed increases in associations
for PCP visits, but not for associations for chiropractic visits
(Table 3). Adjustment for the initiation of the NACRS
database (April 1, 2002) reduced the observed associations;
however, the estimates remained consistently high for all risk
period lengths, for both chiropractic and PCP visits, with
substantial overlap of confidence intervals.
Results of sensitivity and secondary analyses
 Table 3
Table 3
 Table 4
Table 4
|
The sensitivity analyses gave qualitatively similar results to
the primary analysis (Table 4), showing consistently strong
positive associations between acute LDH with early surgical
intervention and both chiropractic and PCP visits. As
in the primary analyses, restricting to lumbar spine visits
resulted in substantially increased IRRs for PCPs visits but
not chiropractic visits.
Sensitivity analyses that used a broader (more sensitive)
set of codes for the event index of acute LDH presenting
to the ED prior to LDH surgery resulted in more precise
confidence interval estimates and less overlap of the confidence
intervals for chiropractic and PCP care (Table 4). In
particular, the largest analytical sample involving up to a
12–week window of time between acute LDH presenting to
the ED and LDH surgery, more sensitive codes for the ED
LDH visit, and exposure to any chiropractic and PCP visit
(n = 961) gave results with no overlap of the confidence
intervals (DC care IRR 10.0; 95% CI 7.4–13.5 vs. PCP care
IRR 18.6, 95% CI 15.0–23.0).
The bootstrap estimates of the CIs for IRRs in the primary
analysis of any visit exposure with a risk period of 0–7 days
were in line with our model estimates: adjusted IRR for
acute LDH with early surgery, 9.5 (95% CI 3.0–35.5) for
chiropractic care, compared with 14.4 (95% CI 7.6–29.3)
for PCP care. Finally, the bootstrap analysis of the ratio of
chiropractic care to PCP care IRRs suggested a positive
safety profile for chiropractic care relative to the baseline
risk represented by PCP care, with a median ratio of the
chiropractic care to PCP care IRRs of 0.6 (95% CI 0.2–2.4).
The majority (72%) of the 2000 bootstrapped values had a
smaller incidence ratio for a DC visit than for a PCP visit.
Discussion
Our study is the first population-based epidemiologic investigation
of the association between chiropractic care and
acute LDH conceptualized as a serious adverse event, that
is, acute LDH presenting to an ED with incident early surgical
intervention. We found a positive association between
chiropractic care and the incidence of acute LDH with early
surgery. We also found a strong positive association between
PCP visits and subsequent acute LDH with early surgery. We
believe that protopathic bias explains our findings—some
patients with low back pain, a common early symptom of
LDH, may have sought healthcare due to this prodromal
symptom prior to LDH being diagnosed. Since PCPs would
not plausibly cause LDH through their typical care for these
patients, we posit that that the observed association between
recent PCP visits and acute LDH with early surgical management
represents the background risk associated with
patients seeking healthcare for early prodromal symptoms
of LDH. Our findings should be interpreted cautiously and
considered within clinical context. Chiropractic care is not
likely to be a major cause of these rare events. Nevertheless,
we cannot exclude the possibility that spinal manipulation,
or even simple physical examination by any healthcare
practitioner, could cause an exacerbation of a developing or
underlying disc herniation leading to full clinical expression
of the pre-existing condition.
In studies examining the risk for acute LDH following
a healthcare visit, the potential for confounding is great,
because persons who seek healthcare may differ from those
who do not in ways that may be difficult to measure and
control for. A major strength of our study is that we used the
self-controlled case series method, in which within-person
comparisons are made, thereby controlling for both known
and unknown confounding factors that do not change over
time and which could affect the risk for acute LDH. This is
important, because smoking, obesity, average occupational
lumbar spine load, and other important risk factors for symptomatic
LDH [44] are not commonly recorded in administrative
health data. Confounding could have occurred only if
patients had risk factors for surgically managed acute LDH
that changed over time, and if these factors were also associated
with the timing of visits to chiropractors and PCPs, and
if these time-dependent effects existed for a high proportion
of study participants.
Our study population included the entire population registered
in Ontario’s provincial healthcare system over an
11–year period, representing over 100 million person-years
of observation. This allowed us to identify all incident early
surgically managed cases of acute LDH, as well as OHIPinsured
visits to chiropractors and PCPs. Yet, we identified
only 195 acute LDH cases for our primary analysis, limiting
the precision of our estimates. In particular, further stratification
by lumbar spine visit diagnosis codes yielded wider
confidence intervals. Nonetheless, there are few other jurisdictions
in the world where it would be possible to carry out
a population-based study linking incident surgically managed
acute LDH with chiropractic and PCP visits.
Key limitations of our study should be considered.
Misclassification bias is an important limitation of using
administrative healthcare data. Our case conceptualization
is an algorithm of surgical intervention codes, hospital
diagnosis codes, and health services diagnosis and
fee codes, from multiple databases over an 11–year study
period. The reliability and validity of our case definition is
unknown. It is possible that our case definition algorithm
resulted in an overinclusive or underinclusive cohort of
cases, and our definition does not capture events that were
managed without early surgery. To investigate the potential
impact of misclassification bias, we carried out sensitivity
analyses varying the time interval between the LDH
surgery and the preceding ED visit for disc herniation,
and repeated analyses using a broader (more sensitive) set
of codes for ED LDH diagnosis on the index date. These
sensitivity analyses yielded results similar to our primary
analysis and did not change our conclusions (Table 4). It
is possible that some chiropractic visits did not involve
spinal manipulation treatment—some empirical evidence
suggests this may be about 5% of visits. [18, 19] It is
also not known what other modalities, if any, were prescribed
and received by patients following both PCP and
chiropractic visits. It seems reasonable to assume that a
PCP visit could have resulted in exposure to a number of
potential treatments such as medication, bed rest, physical
therapy, and exercise. It is also possible that chiropractic
visits may have also involved other therapeutic modalities
besides spinal manipulation, including exercise, modified
activities, and nonprescription medication. This type of
potential misclassification bias may have resulted in some
attenuation of the estimates, but is not expected to alter our
conclusions assuming nondifferential misclassification of
chiropractic and PCP visits.
In our study, the risk period starts on the same day as a
visit to a chiropractor or PCP; therefore, the day of a health
encounter contributes to the exposed period. This leads to
the challenge of dealing with events that occurred on the
same day as an exposure visit and the possibility that the
exposure visit may have taken place after the ED LDH visit,
which could have been possible for both chiropractic and
PCP event-day visits. This potential reverse-causality bias
would lead to our estimates overestimating the associations
between acute LDH and both chiropractic and PCP care.
To assess the effect of event-day visits to chiropractors and
PCPs, we conducted a sensitivity analysis with a 1–day lag
on exposure visit dates to estimate incidence ratios excluding
event-day exposure visits. This, in effect, re-specified the
risk period intervals as: 1–3, 1–8, 1–15, and 1–29 days after
a visit, thereby removing the effect of event-day exposure
visits on our estimates. Our analysis showed some attenuation
of the PCP estimates, but made no material difference
to our findings (Table 4).
Although our study period could only extend up until
December 2004 due to the limitation of OHIP coverage
for chiropractic care in Ontario, our findings are likely still
relevant today as the practice of chiropractic and primary
medical care for acute low back pain and the indications for
early LDH surgery (i.e., severe intractable pain or neurologic
deficit) have not changed materially over the ensuing time
period.
Our findings are similar to a previous study examining the
association between chiropractic care and vertebrobasilar
stroke, in which similar associations were found between
both chiropractic care and PCP care, and the outcome of
vertebrobasilar stroke. [45] Cassidy and colleagues reported
no evidence of excess risk for vertebrobasilar stroke associated
with chiropractic care compared to primary medical
care. They attributed their observed associations to the effect
of patients seeking healthcare, from both chiropractors and
PCPs, for prodromal neck pain and headache before receiving
a diagnosis of vertebrobasilar stroke. [45]
Clinical and research challenges remain. There are no
clinical screening tests to identify patients with back pain
that may be at increased risk of developing acute disc herniation [46], and the current evidence indicates poor diagnostic
performance of most physical tests used to identify LDH. [10, 47] Future studies would need to be multi-centred and undertake prospective, unbiased, and detailed ascertainment
of patients’ reasons for seeking healthcare. With respect to
clinical practice in light of our current state of knowledge,
decisions on how to treat patients with low back pain should
continue to be guided primarily by clinical effectiveness and
current best practice for patient-centred care. [48, 49]
Conclusion
Our population-based self-controlled case series study found
positive associations between acute LDH requiring ED visit
and early surgical intervention, and health care visits to both
chiropractors and PCPs. This suggests that patients with prodromal
back pain related to a developing disc herniation
seek healthcare from both chiropractors and PCPs before
full clinical expression of acute LDH that is subsequently
managed with early surgery.
Acknowledgements
We thank Dr. Heather Whitaker and Dr. Ronny
Kuhnert for their advice about the self-controlled case series design and
analysis of this study. We acknowledge the Ontario Ministry of Health
and Long-Term Care for support with data acquisition.
Author contributions
CAH conceived and designed the study,
acquired, processed, and analysed the data, interpreted the results, and
drafted and revised the paper. GT designed the study, analysed the data,
interpreted the results, and revised the paper. PC and JDC conceived
and designed the study, interpreted the results, and revised the paper.
YRR and ARJ designed the study, interpreted the results, and revised
the paper. CAH acts as guarantor.
Funding sources
Canadian Institutes of Health Research (Grant ID:
200902KPD-205299-111612), Canadian Chiropractic Research Foundation,
and Canadian Chiropractic Protective Association.
Conflict of interest
All authors have completed the ICMJE uniform
disclosure form at http://www.icmje.org/coi_disclosure.pdf (available
from the corresponding author) and declare: CAH was funded
by a Fellowship Award in the Area of Knowledge Translation from
Canadian Institutes of Health Research (Grant ID: 200902KPD-
205299-111612), and Canadian Chiropractic Research Foundation,
PC is funded by a Canada Research Chair in Disability Prevention and
Rehabilitation at the University of Ontario Institute of Technology,
the study received additional support from the Canadian Chiropractic
Protective Association; PC consults for European Spine Society,
National Judicial Institute of Canada, Canadian Memorial Chiropractic
College, Canadian Chiropractic Protective Association, Society of
Musculoskeletal Manual Practitioners of Saskatchewan, Société des
experts en évaluation médico-légale du Québec, YRR consults for
Medtronic, outside the submitted work; no other relationships or activities
that could appear to have influenced the submitted work. The
funders played no role in the design and conduct of the study; collection,
management, analysis, and interpretation of the data; and preparation,
review, or approval of the manuscript.
References:
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, et al.:
Years Lived with Disability (YLDs) for 1160 Sequelae of 289 Diseases and Injuries 1990-2010:
A Systematic Analysis for the Global Burden of Disease Study 2010
Lancet. 2012 (Dec 15); 380 (9859): 2163–2196
Hoy D, Brooks P, Blyth F, Buchbinder R (2010)
The epidemiology of low back pain.
Best Pract Res Clin Rheumatol 24:769–781
Hoy, D., L. March, P. Brooks, F. Blyth, A. Woolf, et al.
The Global Burden of Low Back Pain: Estimates from the Global Burden of Disease 2010 study
Ann Rheum Dis. 2014 (Jun); 73 (6): 968–974
Cassidy JD, Cote P, Carroll LJ, Kristman V (2005)
Incidence and course of low back pain episodes in the general population.
Spine 30:2817–2823
Hincapié CA, Cassidy JD, Côté P (2008)
Is a history of work-related low back injury associated with prevalent low back pain and depression in the general population?
BMC Musculoskelet Disord 9:22
Kent PM, Keating JL (2005)
The epidemiology of low back pain in primary care.
Chiropr Osteopat 13:13
Walker BF (2000)
The prevalence of low back pain: a systematic review of the literature from 1966 to 1998.
J Spinal Disord 13:205–217
Andersson GB (1998)
Epidemiology of low back pain.
Acta Orthop Scand Suppl 281:28–31
Genevay S, Atlas SJ, Katz JN (2010)
Variation in eligibility criteria from studies of radiculopathy due to a herniated disc and of neurogenic claudication due to lumbar spinal stenosis: a structured literature review.
Spine 35:803–811
van der Windt DA, Simons E, Riphagen, II, Ammendolia C, Verhagen
AP et al (2010)
Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain.
Cochrane Database Syst Rev 17:CD007431
Vroomen PC, de Krom MC, Wilmink JT, Kester AD, Knottnerus
JA (2002)
Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression.
J Neurol Neurosurg Psychiatry 72:630–634
Deyo RA, Loeser JD, Bigos SJ (1990)
Herniated lumbar intervertebral disk.
Ann Intern Med 112:598–603
Weber H (1994)
The natural history of disc herniation and the influence of intervention.
Spine 19:2234–2238
Koes BW, van Tulder M, Peul WC.
Diagnosis and Treatment of Sciatica
British Medical Journal 2019 (Nov 19); 367: l6273
Cote P, Cassidy JD, Carroll L.
The Treatment of Neck and Low Back Pain:
Seeks Care? Who Goes Where?
Med Care. 2001 (Sep); 39 (9): 956–967
Hurwitz EL, Chiang LM.
A Comparative Analysis of Chiropractic and General Practitioner
Patients in Noth America: Findings From the Joint Canada/
United States Survey of Health, 2002-03
BMC Health Serv Res 2006 (Apr 6); 6: 49
Hurwitz EL, Coulter ID, Adams AH, Genovese BJ, Shekelle PG
(1998)
Use of chiropractic services from 1985 through 1991 in the United States and Canada.
Am J Public Health 88:771–776
Senstad O, Leboeuf-Yde C, Borchgrevink C (1997)
Frequency and characteristics of side effects of spinal manipulative therapy.
Spine 22:435–440
Leboeuf-Yde C, Hennius B, Rudberg E, Leufvenmark P, Thunman
M (1997)
Side effects of chiropractic treatment: a prospective study.
J Manipulative Physiol Ther 20:511–515
Ferreira ML, Ferreira PH, Latimer J, Herbert R, Maher CG
(2003)
Efficacy of spinal manipulative therapy for low back pain of less than three months’ duration.
J Manipulative Physiol Ther 26:593–601
Bronfort, G, Haas, M, Evans, RL, and Bouter, LM.
Efficacy of Spinal Manipulation and Mobilization
for Low Back Pain and Neck Pain:
A Systematic Review and Best Evidence Synthesis
Spine J (N American Spine Soc) 2004 (May); 4 (3): 335–356
Chou R, Huffman LH; American Pain Society.
Nonpharmacologic Therapies for Acute and Chronic Low Back Pain:
A Review of the Evidence for an American Pain Society/
American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 492–504
Furlan AD, Yazdi F, Tsertsvadze A, Gross A, Van Tulder M, Santaguida L, et. al. (2012)
A Systematic Review and Meta-analysis of Efficacy, Cost-effectiveness, and Safety
of Selected Complementary and Alternative Medicine for Neck and Low-back Pain
Evidence-Based Complementary and Alternative Medicine. 2012 (Nov 24); 2012: 953139
Paige NM, Myiake-Lye IM, Booth MS, et al.
Association of Spinal Manipulative Therapy with Clinical Benefit and Harm
for Acute Low Back Pain: Systematic Review and Meta-analysis
JAMA. 2017 (Apr 11); 317 (14): 1451–1460
Gorrell LM, Engel RM, Brown B, Lystad RP (2016)
The reporting of adverse events following spinal manipulation in randomized clinical trials-a systematic review.
Spine J 16:1143–1151
Santilli V, Beghi E, Finucci S.
Chiropractic Manipulation in the Treatment of Acute Back Pain and Sciatica
with Disc Protrusion: A Randomized Double-blind Clinical Trial
of Active and Simulated Spinal Manipulations
Spine J. 2006 (Mar); 6 (2): 131—137
McMorland G, Suter E, Casha S, du Plessis SJ, Hurlbert RJ.
Manipulation or Microdiskectomy for Sciatica?
A Prospective Randomized Clinical Study
J Manipulative Physiol Ther. 2010 (Oct); 33 (8): 576–584
Bronfort G, Hondras MA, Schulz CA, Evans RL, Long CR et al (2014)
Spinal Manipulation and Home Exercise With Advice for Subacute
and Chronic Back-related Leg Pain: A Trial With Adaptive Allocation
Annals of Internal Medicine 2014 (Sep 16); 161 (6): 381—391
Boucher P, Robidoux S (2014)
Lumbar disc herniation and cauda equina syndrome following spinal manipulative therapy: a review of six court decisions in Canada.
J Forensic Leg Med 22:159–169
Hincapié CA, Cassidy JD, Côté P, Rampersaud YR, Jadad AR et al (2017)
Chiropractic Spinal Manipulation and the Risk for Acute Lumbar Disc Herniation:
A Belief Elicitation Study
European Spine Journal 2018 (Jul); 27 (7): 1517–1525
Hebert JJ, Stomski NJ, French SD, Rubinstein SM (2013)
Serious Adverse Events and Spinal Manipulative Therapy
of the Low Back Region: A Systematic Review of Cases
J Manipulative Physiol Ther 2015 (Nov); 38 (9): 677–691
Maclure M, Fireman B, Nelson JC, Hua W, Shoaibi A et al (2012)
When should case-only designs be used for safety monitoring of medical products?
Pharmacoepidemiol Drug Saf 21(Suppl 1):50–61
Salas M, Hofman A, Stricker BH (1999)
Confounding by indication: an example of variation in the use of epidemiologic terminology.
Am J Epidemiol 149:981–983
Crawford CM, Hannan RF (1999)
Management of acute lumbar disk herniation initially presenting as mechanical low back pain.
J Manipulative Physiol Ther 22:235–244
Whitaker HJ, Hocine MN, Farrington CP (2009)
The methodology of self-controlled case series studies.
Stat Methods Med Res 18:7–26
Whitaker HJ, Farrington CP, Spiessens B, Musonda P (2006)
Tutorial in biostatistics: the self-controlled case series method.
Stat Med 25:1768–1797
Faciszewski T, Broste SK, Fardon D (1997)
Quality of data regarding diagnoses of spinal disorders in administrative databases. A multicenter study.
J Bone Jt Surg Am 79:1481–1488
Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW et al (2008)
Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial.
BMJ 336:1355–1358
Peul WC, van Houwelingen HC, van der Hout WB, Brand R, et al (2005)
Prolonged conservative treatment or ‘early’ surgery in sciatica caused by a lumbar disc herniation: rationale
and design of a randomized trial [ISRCT 26872154].
BMC Musculoskelet Disord 6:8
Farrington CP, Whitaker HJ, Hocine MN (2009)
Case series analysis for censored, perturbed, or curtailed post-event exposures.
Biostatistics 10:3–16
Hua W, Sun G, Dodd CN, Romio SA, Whitaker HJ et al (2013)
A simulation study to compare three self-controlled case series approaches: correction for violation of assumption and evaluation of bias.
Pharmacoepidemiol Drug Saf 22:819–825
Kunhert R, Whitaker HJ (2012)
adSCCS: Case series analysis for censored, perturbed or curtailed post-event exposures [computer program].
R package version 1.5
R Development Core Team (2012)
R: a language and environment for statistical computing.
In. R Foundation for Statistical Computing, Vienna, Austria
Hincapié CA (2015)
Chiropractic care and risk for acute lumbar disc herniation: a mixed methods approach [Doctoral Thesis].
University of Toronto, Toronto. Available from:
http://hdl.handle.net/1807/75685
Accessed 20 Sept 2016
Cassidy JD, Boyle E, Cote P, et al.
Risk of Vertebrobasilar Stroke and Chiropractic Care: Results of a Population-based
Case-control and Case-crossover Study
Spine (Phila Pa 1976) 2008 (Feb 15); 33 (4 Suppl): S176–183
Hartvigsen L, Kongsted A, Hestbaek L.
Clinical Examination Findings as Prognostic Factors in Low Back Pain:
A Systematic Review of the Literature
Chiropractic & Manual Therapies 2015 (Mar 23); 23: 13
Al Nezari NH, Schneiders AG, Hendrick PA (2013)
Neurological examination of the peripheral nervous system to diagnose lumbar spinal disc herniation with suspected radiculopathy: a systematic review and meta-analysis.
Spine J 13:657–674
Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C.
An Updated Overview of Clinical Guidelines for the Management of
Non-specific Low Back Pain in Primary Care
European Spine Journal 2010 (Dec); 19 (12): 2075–2094
Dagenais S, Tricco AC, Haldeman S.
Synthesis of Recommendations for the Assessment and Management
of Low Back Pain From Recent Clinical Practice Guidelines
Spine J. 2010 (Jun); 10 (6): 514–529

Return to LOW BACK PAIN
Return to DISC HERNIATION
Since 10-17-2017
|











