

Clinical Practice Guideline:
Chiropractic Care for Low Back PainThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2016 (Jan); 39 (1): 1–22 ~ FULL TEXT
OPEN ACCESS Gary Globe, PhD, MBA, DC, Ronald J. Farabaugh, DC, Cheryl Hawk, DC, PhD,
Craig E. Morris, DC, Greg Baker, DC, Wayne M. Whalen, DC, Sheryl Walters, MLS,
Martha Kaeser, DC, MA, Mark Dehen, DC, Thomas Augat, DC
Senior Manager,
Global Health Economics,
Amgen, Inc., Thousand Oaks, CA.
gglobe@amgen.com.

OBJECTIVE: The purpose of this article is to provide an update of a previously published evidence-based practice guideline on chiropractic management of low back pain.
METHODS: This project updated and combined 3 previous guidelines. A systematic review of articles published between October 2009 through February 2014 was conducted to update the literature published since the previous Council on Chiropractic Guidelines and Practice Parameters (CCGPP) guideline was developed. Articles with new relevant information were summarized and provided to the Delphi panel as background information along with the previous CCGPP guidelines. Delphi panelists who served on previous consensus projects and represented a broad sampling of jurisdictions and practice experience related to low back pain management were invited to participate. Thirty-seven panelists participated; 33 were doctors of chiropractic (DCs). In addition, public comment was sought by posting the consensus statements on the CCGPP Web site. The RAND-UCLA methodology was used to reach formal consensus.
RESULTS: Consensus was reached after 1 round of revisions, with an additional round conducted to reach consensus on the changes that resulted from the public comment period. Most recommendations made in the original guidelines were unchanged after going through the consensus process.
CONCLUSIONS: The evidence supports that doctors of chiropractic are well suited to diagnose, treat, co-manage, and manage the treatment of patients with low back pain disorders.
KEYWORDS: Chiropractic; Guidelines; Low Back Pain; Manipulation; Spinal
From the FULL TEXT Article:
Introduction
Early development of the chiropractic profession in the 1900s represented the application of accumulated wisdom and traditional practices. [1, 2] As was the practice of medicine, philosophy and practice of chiropractic were informed to a large extent by an apprenticeship and clinical experiential model in a time predominantly absent of clinical trials and observational research.
The traditional chiropractic approach, in which a trial of natural and less invasive methods precedes aggressive therapies, has gained credibility. However, the chiropractic profession can gain wider acceptance in the role as the first point of contact health care provider to patients with low back disorders, particularly within integrated health care delivery systems, by embracing the scientific approach integral to evidence-based health care. [3–7] It is in this context that these guidelines were developed and are updated and revised. [8–12]
By today’s standards, it is the responsibility of a health profession to use scientific methods to conduct research and critically evaluate the evidence base for clinical methods used. [13, 14] This scientific approach helps to ensure that best practices are emphasized. [15] With respect to low back disorders, clinical experience suggests that some patients respond to different treatments. The availability of other clinical methods for conditions that are unresponsive to more evidence-informed approaches (primary nonresponders) introduces the opportunity for patients to achieve improved outcomes by alternative and personalized approaches that may be more attuned to individual differences that cannot be informed by typical clinical trials. [16–18] To a large degree, variability in the selection of treatment methods among doctors of chiropractic (DCs) continues to exist, even though the large body of research on low back pain (LBP) has focused on the most commonly used manipulative methods. [17, 19, 20]
Although the weight of the evidence may favor the evidence referenced in a guideline for particular clinical methods, an individual patient may be best served in subsequent trials of care by treatment that is highly personalized to their own mechanical disorder, experience of pain and disability, as well as preference for a specific treatment approach.
This is consistent with the 3 components of evidence-based practice:clinician experience and judgment,
patient preferences and values, and
the best available scientific evidence. [3, 13]Doctors of chiropractic use methods that assist patients in self-management such as exercise, diet, and lifestyle modification to improve outcomes and their stabilization to avoid dependency on health care system resources. [19, 21] They also recognize that a variety of health care providers play a critical role in the treatment and recovery process of patients at various stages, and that DCs should consult, refer patients, and co-manage patients with them when in the patient’s best interest. [19]
To facilitate best practices specific to the chiropractic management of patients with common, primarily musculoskeletal disorders, the profession established the Council on Chiropractic Guidelines and Practice Parameters (CCGPP) in 1995. [6] The organization sponsored and/or participated in the development of a number of “best practices” recommendations on various conditions. [21–32] With respect to chiropractic management of LBP, a CCGPP team produced a literature synthesis [8] which formed the basis of the first iteration of this guideline in 2008. [9] In 2010, a new guideline focused on chronic spine-related pain was published, [12] with a companion publication to both the 2008 and 2010 guidelines published in 2012, providing algorithms for chiropractic management of both acute and chronic pain. [10] Guidelines should be updated regularly. [33, 34] Therefore, this article provides the clinical practice guideline (CPG) based on an updated systematic literature review and extensive and robust consensus process. [9–12]
Methods
This project was a guideline update based on current evidence and consensus of a multidisciplinary panel of experts in the conservative management of LBP. It has been recommended that, although periodic updates of guidelines are necessary, “partial updating often makes more sense than updating the whole CPG because topics and recommendations differ in terms of the need for updating.” [33] Logan University Institutional Review Board determined that the project was exempt. We used Appraisal of Guidelines for Research & Evaluation (AGREE) in developing the guideline methodology.
Systematic Review
Between March 2014 through July 2014, we conducted a systematic review to update the literature published since the previous CCGPP guideline was developed. The search included articles that were published between October 2009 through February 2014.
Our question was,“What is the effectiveness of chiropractic care including spinal manipulation
for nonspecific low back pain?”Table 1 summarizes the eligibility criteria for the search.
Search Strategy

Table 1
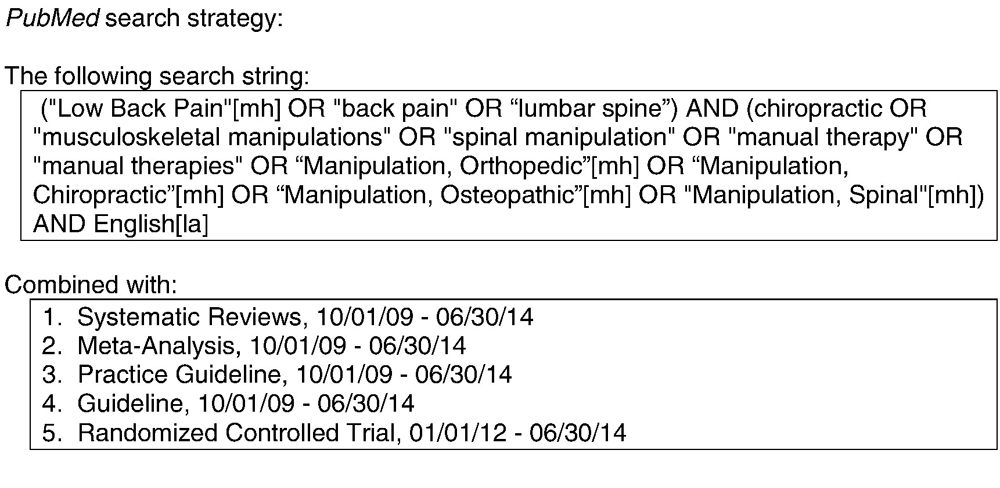
Figure 1 The following databases were included in the search: PubMed, Index to Chiropractic Literature, CINAHL, and MANTIS. Details of the strategy for each database are provided in Figure 1. Articles and abstracts were screened independently by 2 reviewers. Data were not further extracted.
Evaluation of Articles
We evaluated articles using the Scottish Intercollegiate Guideline Network checklists
(http://www.sign.ac.uk/methodology/checklists.html) for randomized controlled trials (RCTs) and systematic reviews/meta-analyses. For guidelines, the AGREE 2013 instrument [35] was used. At least 2 of the 3 investigators conducting the review (CH, SW, MK) reviewed each article. If both reviewers rated the study as either high quality or acceptable, it was included for consideration; if both reviewers rated it as unacceptable, it was removed. For AGREE, we considered “unacceptable” to be a sum of <4. If there was disagreement between reviewers, a third also reviewed the article, and the majority rating was used.
Results of Literature Review
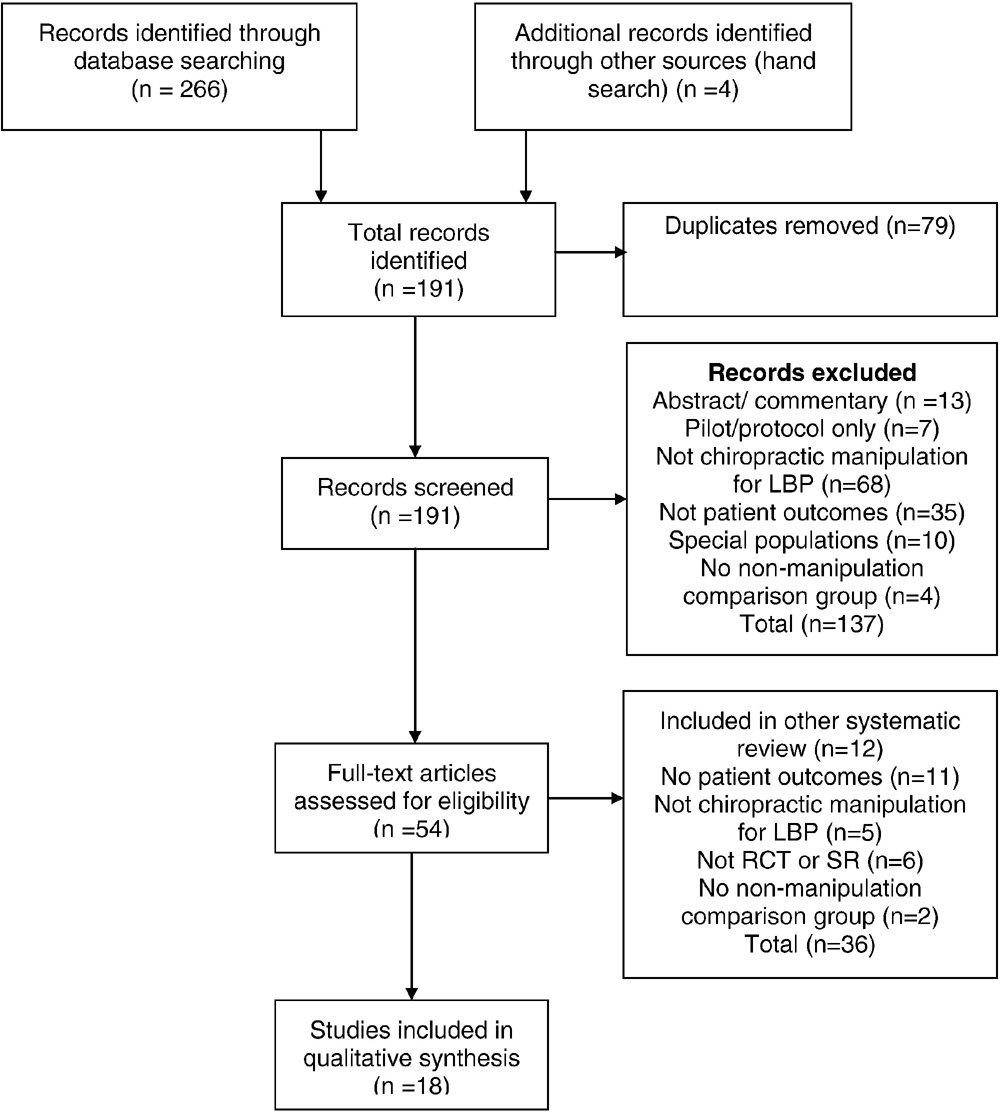
Figure 2

Table 2 Part A

Table 2 Part B This search yielded 270 articles. Screening the articles for eligibility resulted in 18 articles included for evaluation, as detailed in Figure 2, using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart. [36]
Of the 18 articles included after screening, 16 were retained as acceptable/high quality [12, 17, 37–52] (both systematic reviews) were excluded as being of unacceptable quality according to the Scottish Intercollegiate Guideline Network checklist. Those with new relevant information were summarized and provided to the Delphi panel as background information. Table 2 lists the articles by lead author and date, and the topic addressed, if new findings were present.
Seed Documents and Seed Statements
Along with the literature summary, seed documents were comprised of the 3 previous CCGPP guidelines [9, 10, 12]; links were provided to full text versions. The original guidelines had been developed based on the evidence, including guidelines and research available at the time. [16, 53–63] The steering committee, composed of authors on these previous guidelines, developed 51 seed statements based on the background documents, revising the previous statements if it seemed advisable based on the literature. The steering committee did not conduct a formal consensus process; however, the seed statement development was a team effort, with changes only made if all members of the steering committee were in agreement.
Before conducting this project, these seed statements had gone through a local Delphi process among clinical and academic faculty at Logan University as part of their development of care pathways for their clinical faculty. This was done to assess the readability of the seed statements to a group of practicing clinicians. In the Delphi process, 7 statements were slightly modified from the original, and none of those changes were substantive, but rather for purposes of clarification. Consensus was reached for the seed document, which was then adopted by that institution for use in its teaching clinics. That document formed the seed document for the current project. For the Delphi rounds, the 51 statements were divided into 3 sections to be less onerous for the panelists to rate in a timely manner.
Delphi Panel
Panelists who served on the 3 previous consensus projects [10–12] related to LBP management were invited to participate. Steering committee members made additional recommendations for experts in management of LBP who were not DCs to increase multidisciplinary input. There were 37 panelists; 33 were DCs, one of whom had dual licensure — DC and massage therapist. The 4 non-DC panelists consisted of an acupuncturist who is also a medical doctor, a medical doctor (orthopedic surgeon), a massage therapist, and a physical therapist. Thirty-three of the 37 panelists were in practice (89%); the mean number of years in practice was 27. Seventeen were also affiliated with a chiropractic institution (46%), with 2 of these associated with Logan University; 3 were affiliated with a different health care professional institution (8%); and 1 was employed with a government agency.
Because this guideline focuses primarily on chiropractic practice in the United States, geographically, all panelists were from the United States, with 19 states represented. These were Arizona (1), California (4), Florida (3), Georgia (3), Hawaii (2), Iowa (2), Illinois (3), Kansas (1), Michigan (1), Minnesota (1), Missouri (3), North Carolina (1), New Jersey (2), New York (5), South Carolina (1), South Dakota (1), Texas (1), Virginia (1), and Vermont (1). Of the 33 DCs, 21 (64%) were members of the American Chiropractic Association, 2 (6%) were members of the International Chiropractors Association, and 10 (30%) did not belong to any national chiropractic professional organization.
Delphi Rounds and Rating System
The consensus process was conducted by e-mail. For purposes of analyzing the ratings and comments, panelists were identified by an ID number only. The Delphi panelists were not aware of other panelists’ identity during the duration of the study. As in our previous projects, we used the RAND-UCLA methodology for formal consensus. [64]
This methodology uses an ordinal scale of 1–9 (highly inappropriate to highly appropriate) to rate each seed statement. RAND/UCLA defines appropriateness to mean that expected patient health benefits are greater than expected negative effects by a large enough margin that the action is worthwhile, without considering costs. [64]
After scoring each Delphi round, the project coordinator provided the medians, percentages, and comments (as a Word table) to the steering committee. They reviewed all comments and revised any statements not reaching consensus as per these comments. The project coordinator circulated the revised statements, accompanied by the deidentified comments, to the Delphi panel for the next round.
We considered consensus on a statement’s appropriateness to have been reached if both the median rating was 7 or higher and at least 80% of panelists’ ratings for that statement were 7 or higher. Panelists were provided with space to make unlimited comments on each statement. If consensus could not be reached, it was planned that minority reports would be included.
Public Comments
As per recommendations for guideline development such as AGREE, we invited public comment on the draft CPG. This was accomplished by posting the consensus statement on the CCGPP Web site. Press releases and direct e-mail contacts announced a 2–week public comment period, with comments collected via an online Web survey application. Organizations and institutions who were contacted included the following: all US chiropractic colleges; members of all chiropractic state organizations; state boards of chiropractic examiners; chiropractic practice consultants; chiropractic attorneys; chiropractic media (including 1 publication sent to all US-licensed DCs); and chiropractic vendors, whose contacts also included interested laypersons. The steering committee then crafted additional or revised statements as per the comments collected through this method, and these statements were then recirculated through the Delphi panel until consensus was reached.
Data Analysis
For scoring purposes, ratings of 1–3 were collapsed as “inappropriate,” 4–6 as “uncertain,” and 7–9 as “appropriate.” If a panelist rated a statement as “inappropriate,” he or she was instructed to articulate a specific reason and provide a citation from the peer-reviewed literature to support it, if possible. The project coordinator entered ratings into a database (SPSS v. 22.0, Armonk, NY: IBM Corp, 2013).
Results
The verbatim evidence-informed consensus-based seed statements, as approved by the Delphi panel, are presented below. Consensus was reached after 1 round of revisions, with an additional round conducted to reach consensus on the changes that resulted from the public comment period. No minority reports are included because consensus was reached on all statements. There were 7 comments received, 6 from DCs and 1 from a layperson. Three did not require a response; statements were added or modified in response to the other 4 comments.
A. General Considerations

Table 3 Most acute pain, typically the result of injury (micro- or macrotrauma), responds to a short course of conservative treatment (Table 3). If effectively treated at this stage, patients often recover with full resolution of pain and function, although recurrences are common. Delayed or inadequate early clinical management may result in increased risk of chronicity and disability. Furthermore, those responding poorly in the acute stage and those with increased risk factors for chronicity must also be identified as early as possible.
Clinicians must continually be vigilant for the appearance of clinical red flags that may arise at any point during patient care. In addition, biopsychosocial factors (also known as clinical yellow flags) should be identified and addressed as early as possible as part of a comprehensive approach to clinical management.
Chiropractic doctors are skilled in multiple approaches of functional assessment and treatment. Depending on the clinical complexity, DCs can work independently or as part of a multidisciplinary team approach to functional restoration of patients with acute and chronic LBP.
It is the ultimate goal of chiropractic care to improve patients' functional capacity and educate them to accept independently the responsibility for their own health.
B. Informed Consent
Informed consent is the process of proactive communication between a patient and physician that results in the patient's authorization or agreement to undergo a specific medical intervention. Informed consent should be obtained from the patient and performed within the local and/or regional standards of practice. The DC should explain the diagnosis, examination, and proposed procedures clearly and simply and answer patients’ questions to ensure that they can make an informed decision about their health care choices. He or she should explain material risks* of care along with other reasonable treatment options, including the risks of no treatment. (*Note: The legal definition of material risk may vary state by state.)
C. Examination Procedures
Thorough history and evidence-informed examination procedures are critical components of chiropractic clinical management. These procedures provide the clinical rationale for appropriate diagnosis and subsequent treatment planning.
Assessment should include but is not limited to the following [38]:
Health history (eg, pain characteristics, red flags, review of systems, risk factors for chronicity)
Specific causes of LBP (eg, aortic aneurysm, inflammatory disorders)
Examination (eg, reflexes, dermatomes, myotomes, orthopedic tests)
Diagnostic testing (indications) for red flags (eg, imaging and laboratory tests)
Routine imaging or other diagnostic tests are not recommended for patients with nonspecific LBP. [55]
Imaging and other diagnostic tests are indicated in the presence of severe and/or progressive neurologic deficits or if the history and physical examination cause suspicion of serious underlying pathology. [55]
Patients with persistent LBP accompanied by signs or symptoms of radiculopathy or spinal stenosis should be evaluated, preferably, with magnetic resonance imaging or computed tomography. [55]
Imaging studies should be considered when patients fail to improve following a reasonable course of conservative care or when there is suspicion of an underlying anatomical anomaly, such as spondylolisthesis, moderate to severe spondylosis, posttrauma with worsening symptomatogy (consider imaging, referral, or co-management) with evidence of persistent or increasing neurological (ie, reflex, motor, and/or sensory) compromise, or other factors which might alter the treatment approach. Lateral view flexion/extension studies may be warranted to assess for mechanical instability due to excessive intervertebral translation and/or wedging. Imaging studies should be considered only after careful review and correlation of the history and examination. [65]
D. Severity and Duration of Conditions
Conditions of illness and injury are typically classified by severity and/or duration. Common descriptions of the stages of illness and injuries are acute, subacute, chronic, and recurrent, and further subdivided into mild, moderate, and severe.
Acute — symptoms persisting for less than 6 weeks.
Subacute — symptoms persisting between 6 and 12 weeks.
Chronic — symptoms persisting for at least 12 weeks' duration.
Recurrent/flare-up — return of symptoms perceived to be similar to those of the original injury
at sporadic intervals or as a result of exacerbating factors.E. Treatment Frequency and Duration
Although most patients respond within anticipated time frames, frequency and duration of treatment may be influenced by individual patient factors or characteristics that present as barriers to recovery (eg, comorbidities, clinical yellow flags). Depending on these individualized factors, additional time and treatment may be required to observe a therapeutic response. The therapeutic effects of chiropractic care/treatment should be evaluated by subjective and/or objective assessments after each course of treatment (see “Outcome Measurement”).
Recommended therapeutic trial ranges are representative of typical care parameters. A typical initial therapeutic trial of chiropractic care consists of 6 to 12 visits over a 2– to 4–week period, with the doctor monitoring the patient's progress with each visit to ensure that acceptable clinical gains are realized (Table 3).
For acute conditions, fewer treatments may be necessary to observe a therapeutic effect and to obtain complete recovery. Chiropractic management is also recommended for various chronic low back conditions where repeated episodes (or acute exacerbations) are experienced by the patient, particularly when a previous course of care has demonstrated clinical effectiveness and reduced the long-term use of medications.
F. Initial Course of Treatments for Low Back Disorders
To be consistent with an evidence-based approach, DCs should use clinical methods that generally reflect the best available evidence, combined with clinical judgment, experience, and patient preference. For example, currently, the most robust literature regarding manual therapy for LBP is based primarily on high-velocity, low-amplitude (HVLA) techniques, and mobilization (such as flexion-distraction). [17, 20, 66] Therefore, in the absence of contraindications, these methods are generally recommended. However, best practices for individualized patient care, based on clinical judgment and patient preference, may require alternative clinical strategies for which the evidence of effectiveness may be less robust.
The treatment recommendations that follow, based on clinical experience combined with the best available evidence, are posited for the “typical” patient and do not include risk stratification for complicating factors. Complicating factors are discussed elsewhere in this document.
An initial course of chiropractic treatment typically includes 1 or more “passive” (ie, nonexercise) manual therapeutic procedures (ie, spinal manipulation or mobilization) and physiotherapeutic modalities for pain reduction, in addition to patient education designed to reassure and instill optimal strategies for independent management.
Although the evidence reviewed does not generally support the use of therapeutic modalities (ie, ultrasonography, electrical stimulation, etc) in isolation, [67] their use as part of a passive-to-active care multimodal approach to LBP management may be warranted based on clinician judgment and patient preferences. Because of the scarcity of definitive evidence, [68] lumbar supports (bracing/taping/orthoses) are not recommended for routine use, but there may be some utility in both acute and chronic conditions based upon clinician judgment, patient presentation, and preferences. Caution should be exercised as these orthopedic devices may interfere with conditioning and return to regular activities of daily living (ADLs).
The initial visits allow the doctor to explain that the clinician and the patient must work as a proactive team and to outline the patient's responsibilities. Although passive care methods for pain or discomfort may be initially emphasized, “active” (ie, exercise) care should be increasingly integrated to increase function and return the patient to regular activities. Table 3 lists appropriate frequency and duration ranges for trials of chiropractic treatment for different stages of LBP.
G. Reevaluation and Reexamination
After an initial course of treatment has been concluded, a detailed or focused reevaluation should be performed. The purpose of this reevaluation is to determine whether the patient has made clinically meaningful improvement. A determination of the necessity for additional treatment should be based on the response to the initial trial of care and the likelihood that additional gains can be achieved.
As patients begin to plateau in their response to treatment, further care should be tapered or discontinued depending on the presentation. A reevaluation is recommended to confirm that the condition has reached a clinical plateau or has resolved. When a patient reaches complete or partial resolution of their condition and all reasonable treatment and diagnostic studies have been provided, then this should be considered a final plateau (maximum therapeutic benefit, MTB). The DC should perform a final examination, typically following a trial of therapeutic withdrawal, to verify that MTB has been achieved and provide any necessary patient education and instructions in effective future self-management and/or the possible need for future chiropractic care to retain the benefits achieved.
H. Continuing Course of Treatment
If the criteria to support continuing chiropractic care (substantive, measurable functional gains with remaining functional deficits) have been achieved, a follow-up course of treatment may be indicated. However, one of the goals of any treatment plan should be to reduce the frequency of treatments to the point where MTB continues to be achieved while encouraging more active self-therapy, such as independent strengthening and range of motion exercises and rehabilitative exercises. Patients also need to be encouraged to return to usual activity levels as well as to avoid catastrophizing and overdependence on physicians, including DCs. The frequency of continued treatment generally depends on the severity and duration of the condition. Patients who are interested in wellness care (formerly called maintenance care [11]) should be given those options as well. (Wellness or maintenance care was defined by Dehen et al [11] as “care to reduce the incidence or prevalence of illness, impairment, and risk factors and to promote optimal function.”)
When the patient's condition reaches a plateau or no longer shows ongoing improvement from the therapy, a decision must be made on whether the patient will need to continue treatment. Generally, progressively longer trials of therapeutic withdrawal may be useful in ascertaining whether therapeutic gains can be maintained without treatment.
In a case where a patient reaches a clinical plateau in their recovery (MTB) and has been provided reasonable trials of interdisciplinary treatments, additional chiropractic care may be indicated in cases of exacerbation/flare-up or when withdrawal of care results in substantial, measurable decline in functional or work status. Additional chiropractic care may be indicated in cases of exacerbation/flare-up in patients who have previously reached MTB if criteria to support such care (substantive, measurable prior functional gains with recurrence of functional deficits) have been established.
I. Outcome Measurement
For a trial of care to be considered beneficial, it must be substantive, meaning that a definite improvement in the patient's functional capacity has occurred. Examples of measurable outcomes and activities of daily living and employment include the following:
Pain scales such as the visual analog scale and the numeric rating scale.
Pain diagrams that allow the patient to demonstrate the location and character of their symptoms.
Validated ADL measures, such as the Revised Oswestry Back Disability Index,
Roland Morris Back Disability Index, RAND 36, and Bournemouth Disability Questionnaire.Increases in home and leisure activities, in addition to increases in exercise capacity.
Increases in work capacity or decreases in prior work restrictions.
Improvement in validated functional capacity testing, such as lifting capacity, strength,
flexibility, and endurance.J. Spinal Range of Motion Assessment
Range of motion testing may be used as a part of the physical examination to assess for regional mobility, although evidence does not support its reliability in determining functional status. [69]
K. Benefit vs Risk
Care rendered by DCs has been documented to be quite safe and effective compared with other common medical treatments and procedures. A 2010 systematic review concluded that serious adverse events were no more than 1 per million patient visits for lumbar spine manipulation.20 Another systematic review found that the risk of major adverse events with manual therapy is low, but many patients experience minor to moderate short-lived (<48 hours) adverse events after treatment. [70]
These are usually brief episodes of muscle stiffness or soreness. [20] The relative risk (RR) of adverse events appears greater with drug therapy but less with usual medical care. [70] Comparatively, an earlier study from 1995 related to cervical manipulation found that the RR for high-velocity manipulation causing minor/moderate adverse events was significantly less than the RR of the comparison medication (usually nonsteroidal anti-inflammatory drugs [NSAIDs]). [71] The risk of death from NSAIDs for osteoarthritis was estimated to be 100–400 times the risk of death from cervical manipulation. [71] Because lumbar spine manipulation is considered lower risk than cervical manipulation, it is reasonable to extrapolate that NSAIDs pose at least the same comparative risk when prescribed for the treatment of LBP. Special attention must be given to each patient’s individual history and presentation. In that context, it should be noted that for patients who are not good candidates for HVLA manipulation, DCs should modify their manual approach accordingly.
L. Cautions and Contraindications
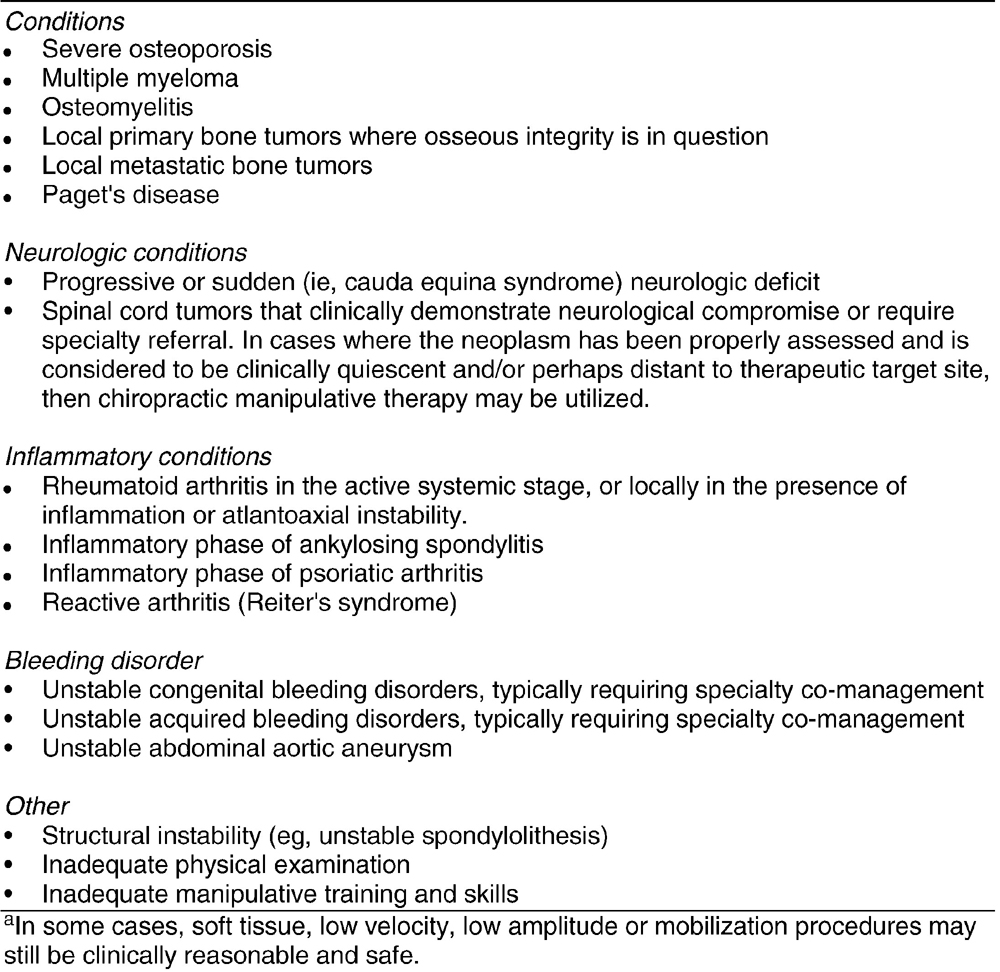
Figure 3 Chiropractic-directed care, including patient education, and passive and active care therapy, is a safe and effective form of health care for low back disorders. As stated in the previous section, there are certain clinical situations where HVLA manipulation or other manual therapies may be contraindicated. It is incumbent upon the treating DC to evaluate the need for care and the risks associated with any treatment to be applied. Many contraindications are considered relative to the location and stage of severity of the morbidity, whether there is co-management with one or more specialists, and the therapeutic methods being used by the chiropractic physician. Figure 3 lists contraindications for high-velocity manipulation to the lumbar spine (red flags); however, these do not necessarily prohibit soft-tissue, low-velocity, low-amplitude procedures and mobilization.
M. Conditions Contraindicating Certain Chiropractic-Directed
Treatments Such as Spinal Manipulation and Passive Therapy
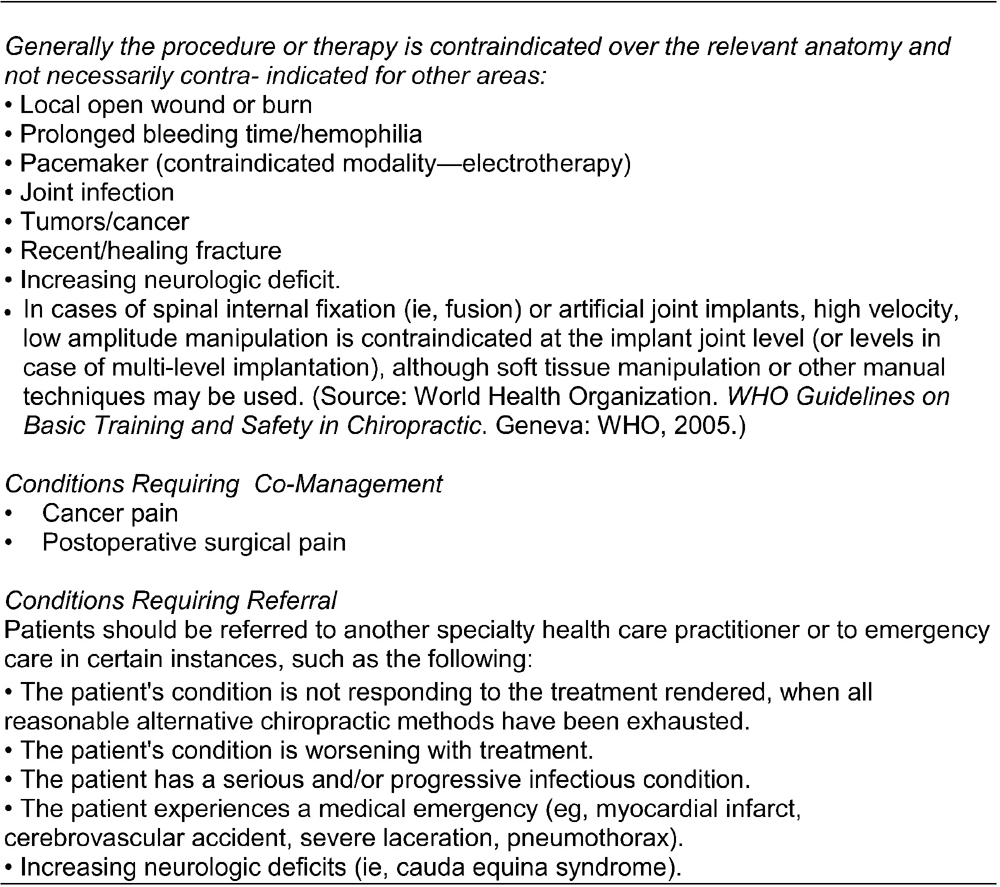
Figure 4

Figure 5 In some complex cases where biomechanical, neurological, or vascular structure or integrity is compromised, the clinician may need to modify or omit the delivery of manipulative procedures. Chiropractic co-management may still be appropriate using a variety of treatments and therapies commonly used by DCs. It is prudent to document the steps taken to minimize the additional risk that these conditions may present. Figure 4 lists conditions which present contraindications to spinal manipulation and passive therapy, along with conditions requiring co-management and/or referral.
During the course of ongoing chronic pain management of spine-related conditions, the provider must remain alert to the emergence of well-known and established “red flags” that could indicate the presence of serious pathology. Patients presenting with “red flag” signs and/or symptoms require prompt diagnostic workup which can include imaging, laboratory studies, and/or referral to another provider. Ignoring these “red flag” indicators increases the likelihood of patient harm. Figure 5 summarizes red flags that present contraindications to ongoing HVLA spinal manipulation.
N. Management of Chronic LBP
Definition of chronic pain patients. Note: MTB is defined as the point at which a patient's condition has plateaued and is unlikely to improve further. Chronic pain patients are those for whom ongoing supervised treatment/care has demonstrated clinically meaningful improvement with a course of management and who have reached MTB, but in whom substantial residual deficits in activity performance remain or recur upon withdrawal of treatment. The management for chronic pain patients ranges from home-directed self-care to episodic care to scheduled ongoing care. Patients who require provider-assisted ongoing care are those for whom self-care measures, although necessary, are not sufficient to sustain previously achieved therapeutic gains; these patients may be expected to progressively deteriorate as demonstrated by previous treatment withdrawals.
O. Chronic Care Goals
Minimize lost time on the job
Support patient's current level of function/ADL
Pain control/relief to tolerance
Minimize further disability
Minimize exacerbation frequency and severity
Maximize patient satisfaction
Reduce and/or minimize reliance on medication
P. Application of Chronic Pain Management
Chronic pain management occurs after the appropriate application of active and passive care including lifestyle modifications. It may be appropriate when rehabilitative and/or functional restorative and other care options, such as psychosocial issues, home-based self-care, and lifestyle modifications, have been considered and/or attempted, yet treatment fails to sustain prior therapeutic gains and withdrawal/reduction results in the exacerbation of the patient's condition and/or adversely affects their ADLs.
Ongoing care may be inappropriate when it interferes with other appropriate care or when the risk of supportive care outweighs its benefits, that is, physician dependence, somatization, illness behavior, or secondary gain. However, when the benefits outweigh the risks, ongoing care may be both medically necessary and appropriate.
Appropriate chronic pain management of spine-related conditions includes addressing the issues of physician dependence, somatization, illness behavior, and secondary gain. Those conditions that require ongoing supervised treatment after having first achieved MTB should have appropriate documentation that clearly describes them as persistent or recurrent conditions. Once documented as persistent or recurrent, these chronic presentations should not be categorized as “acute” or uncomplicated.
Q. Factors Affecting the Necessity for Chronic Pain Management of LBP
Prognostic factors that may provide a partial basis for the necessity for chronic pain management
of LBP after MTB has been achieved include the following:
Older age (pain and disability)
History of prior episodes (pain, activity limitation, disability)
Duration of current episode >1 month (activity limitation, disability)
Leg pain (for patients having LBP) (pain, activity limitation, disability)
Psychosocial factors (depression [pain]; high fear-avoidance beliefs, poor coping skills
[activity limitation]; expectations of recovery)High pain intensity (activity limitation; disability)
Occupational factors (higher job physical or psychological demands [disability])
The list above is not all-inclusive and is provided to represent prognostic factors most commonly seen in the literature. Other factors or comorbidities not listed above may adversely affect a given patient's prognosis and management. These should be documented in the clinical record and considered on a case-by-case basis.
Each of the following factors may complicate the patient's condition, extend recovery time,
and result in the necessity of ongoing care:
Nature of employment/work activities or ergonomics: The nature and psychosocial aspects
of a patient's employment must be considered when evaluating the need for ongoing care
(eg, prolonged standing posture, high loads, and extended muscle activity).Impairment/disability: The patient who has reached MTB but has failed to reach
preinjury status has an impairment/disability even if the injured patient has not
yet received a permanent impairment/disability award.Medical history: Concurrent condition(s) and/or use of certain medications may affect outcomes.
History of prior treatment: Initial and subsequent care (type and duration), as well as patient
compliance and response to care, can assist the physician in developing appropriate
treatment planning. Delays in the initiation of appropriate care may complicate the
patient's condition and extend recovery time.Lifestyle habits: Lifestyle habits may impact the magnitude of treatment response,
including outcomes at MTB.Psychological factors: A history of depression, anxiety, somatoform disorder, or other
psychopathology may complicate treatment and/or recovery.R. Treatment Withdrawal Fails to Sustain MTBG
Documented flare-ups/exacerbations (ie, increased pain and/or associated symptoms, which may or may not be related to specific incidents), superimposed on a recurrent or chronic course, may be an indication of chronicity and/or need for ongoing care.
S. Complicating/Risk Factors for Failure to Sustain MTB
Figure 5 lists complicating factors that may document the necessity of ongoing care for chronic spine-related conditions. Such lists of complicating/risk factors are not all-inclusive. Individual factors from this list may adequately explain the condition chronicity, complexity, and instability in some cases. However, most chronic cases that require ongoing care are characterized by multiple complicating factors. These factors should be carefully identified and documented in the patient's file to support the characterization of a condition as chronic.
T. Risk Factors for the Transition of Acute/Subacute
Spine-Related Conditions to Chronicity (Yellow Flags)
A number of prognostic variables have been identified as increasing the risk of transition from acute/subacute to chronic nonspecific spine-related pain. However, their independent prognostic value is low. A multidimensional model, that is, a number of clinical, demographic, psychological, and social factors are considered simultaneously, has been recommended. This model emphasizes the interaction among these factors, as well as the possible overlap between variables such as pain beliefs and pain behaviors.
Chronicity may be described in terms of pain and/or activity limitation (function) and/or work disability.
Risk factors for chronicity have been categorized by similar domains:
Symptoms
Psychosocial factors
Function
Occupational factors
Factors directly associated with the clinician/patient encounter may influence the transition to chronicity:
Treatment expectations: Patients with high expectations for a specific treatment may contribute
to better functional outcomes if they receive that treatment.Significant others' support: Patients’ risk of chronicity may be reduced when family members
encourage their participation in social and recreational activities.U. Diagnosis of Chronic LBP
The diagnosis should never be used exclusively to determine need for care (or lack thereof). The diagnosis must be considered with the remainder of case documentation to assist the physician or reviewer in developing a comprehensive clinical picture of the condition/patient under treatment.
V. Clinical Reevaluation Information
Clinical information obtained during reevaluation that may be used to document the necessity of chronic pain management for persistent or recurrent spine-related conditions includes, but is not limited to, the following:
Response to date of care management for the current and previous episodes.
Response to therapeutic withdrawal (either gradual or complete withdrawal) or absence of care.
MTB has been reached and documented.
Patient-centered outcome assessment instruments.
Analgesic use patterns.
Other health care services used.
W. Clinical Reevaluation Information to Document Necessity
for Ongoing Care of Chronic LBP
In addition to standard documentation elements (ie, date, history, physical evaluation, diagnosis, and treatment plan),
the clinical information typically relied upon to document the necessity of ongoing chronic pain management
includes the following:
Documentation of having achieved a clinically meaningful favorable response to
initial treatment or documentation that the plan of care is to be amended.Documentation that the patient has reached maximum therapeutic benefit (MTB).
Substantial residual deficits in activity limitations are present at MTB.
Documented attempts of transition to primary self-care.
Documented attempts and/or consideration of alternative treatment approaches.
Documentation of those factors influencing the likelihood that self-care alone
will be insufficient to sustain or restore MTB.
Once the need for additional care has been documented, findings of diagnostic/assessment procedures
that may influence treatment selection include the following:
Neurological/provocative testing (standard neurological testing, orthopedic tests, manual muscle testing);
Diagnostic imaging (radiography, computed tomography, magnetic resonance imaging);
Electrodiagnostics;
Functional movement/assessment (eg, ambulatory assessment/limp);
Chiropractic analysis procedures;
Biomechanical analysis (pain, asymmetry, range of motion, tissue tone changes);
Palpation (static, motion);
Nutritional/dietary assessment with respect to factors related to pain management (such as vitamin D intake).
This list is provided for guidance only and is not all-inclusive. All items are not required to justify the need for ongoing care. Each item of clinical information should be documented in the case file to describe the patient's clinical status, present and past.
In the absence of documented flare-up/exacerbation, the ongoing treatment of persistent or recurrent spine-related disorders is not expected to result in any clinically meaningful change. In the event of a flare-up or exacerbation, a patient may require additional supervised treatment to facilitate return to MTB status. Individual circumstances including patient preferences and previous response to specific interventions guide the appropriate services to be used in each case.
X. Chronic Pain Management Components in Physician-Directed Case Management
Case management of patients with chronic LBP should be based upon an individualized approach to care that combines the best evidence with clinician judgment and patient preferences. In addition to spinal manipulation and/or mobilization, an active care plan for chronic pain management may include, but is not restricted to, the following:Procedures
- Massage therapy
- Other manual therapeutic methods
- Physical modalities
- Acupuncture
- Bracing/orthoses
Behavioral and exercise recommendations
- Supervised rehabilitative/therapeutic exercise
- General and/or specific exercise programs
- Mind/body programs (eg, yoga, Tai Chi)
- Multidisciplinary rehabilitation
- Cognitive behavioral programs
Counseling recommendations
- ADL recommendations
- Co-management/coordination of care with other physicians/health care providers
- Ergonomic recommendations
- Exercise recommendations and instruction
- Home care recommendations
- Lifestyle modifications/counseling
- Pain management recommendations
- Psychosocial counseling/behavioral modification/risk avoidance counseling
- Monitoring patient compliance with self-care recommendations
Y. Chronic Pain Management Treatment Planning
A variety of functional and physiological changes may occur in chronic conditions. Therefore, a variety of treatment procedures, modalities, and recommendations may be applied to benefit the patient. The necessity for ongoing chronic pain management of spine-related conditions for individual patients is established when there is a return of pain and/or other symptoms and/or pain-related difficulty performing tasks and actions equivalent to the appropriate minimal clinically important change value for more than 24 hours, for example, change in numeric rating scale of more than 2 points for chronic LBP.
Although the visit frequency and duration of supervised treatment vary and are influenced by the rate of recovery toward MTB values and the individual's ability to self-manage the recurrence of complaints, a reasonable therapeutic trial for managing patients requiring ongoing care is up to 4 visits after a therapeutic withdrawal. If reevaluation indicates further care, this may be delivered at up to 4 visits per month. (Caution: The majority of chronic pain patients can self/home-manage, be managed in short episodic bursts of care, or require ongoing care at 1–2 visits per month, to be reevaluated at a minimum of every 12 visits. It is rare that a patient would require 4 visits per month to manage even advanced or complicated chronic pain.) Clinicians should routinely monitor a patient's change in pain/function to determine appropriateness of continued care. An appropriate reevaluation should be completed at minimum every 12 visits. Reevaluation may be indicated more frequently in the event a patient reports a substantial or unanticipated change in symptoms and/or there is a basis for determining the need for change in the treatment plan/goals.
Z. Scheduled Ongoing Chronic Pain Management Treatment Planning
When pain and/or ADL dysfunction exceeds the patient's ability to self-manage, the medical necessity of care should be documented and the chronic care treatment plan altered appropriately.
Patient recovery patterns vary depending on degrees of exacerbations. Mild exacerbation episodes may be manageable with 1–6 office visits within a chronic care treatment plan. There is not a linear effect between the intensity of exacerbation and time to recovery.
Moderate and severe exacerbation episodes within a chronic care treatment plan require acute care recommendations and case management. [12]
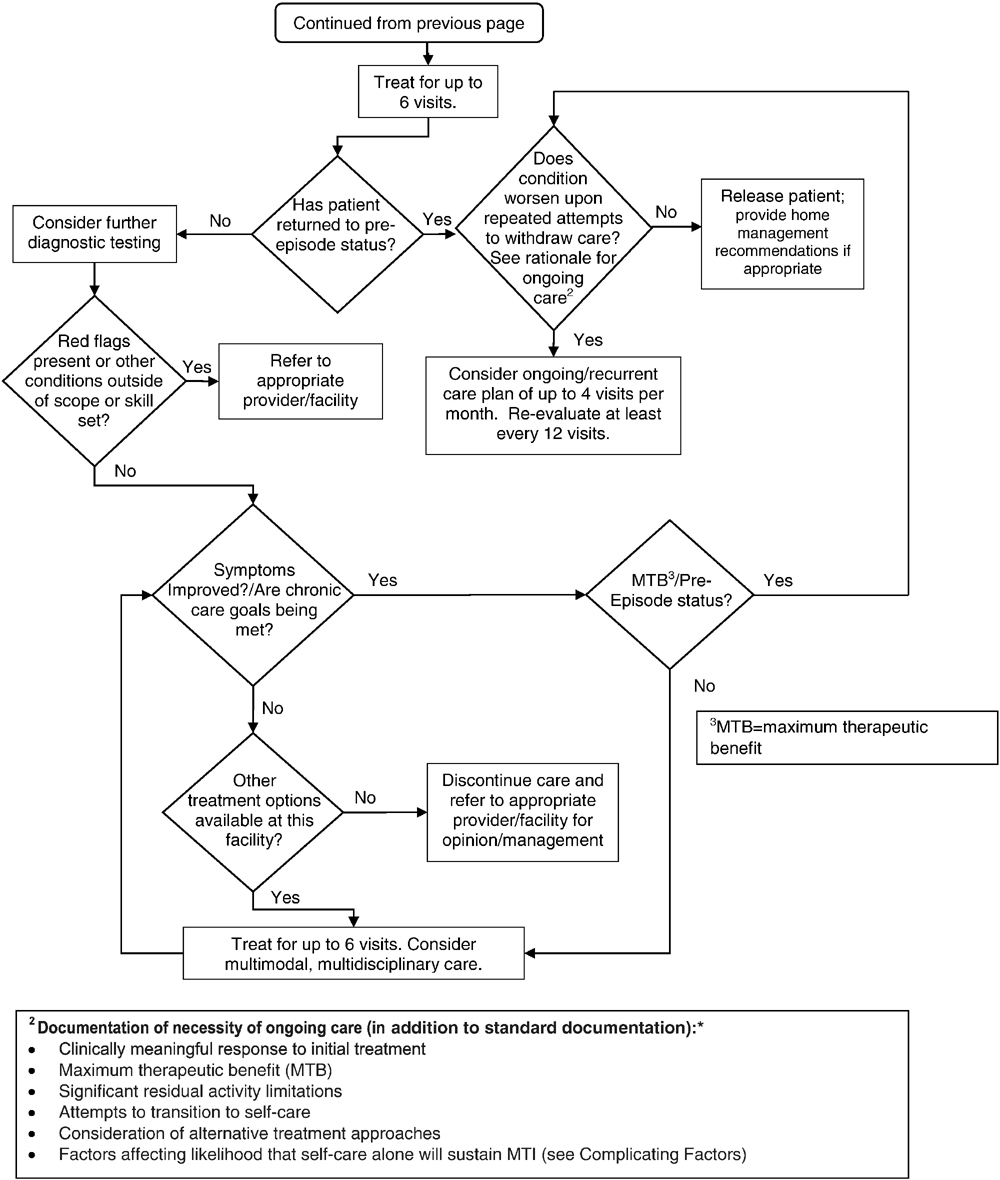
Algorithms
Figure 6A.
General Algorithm
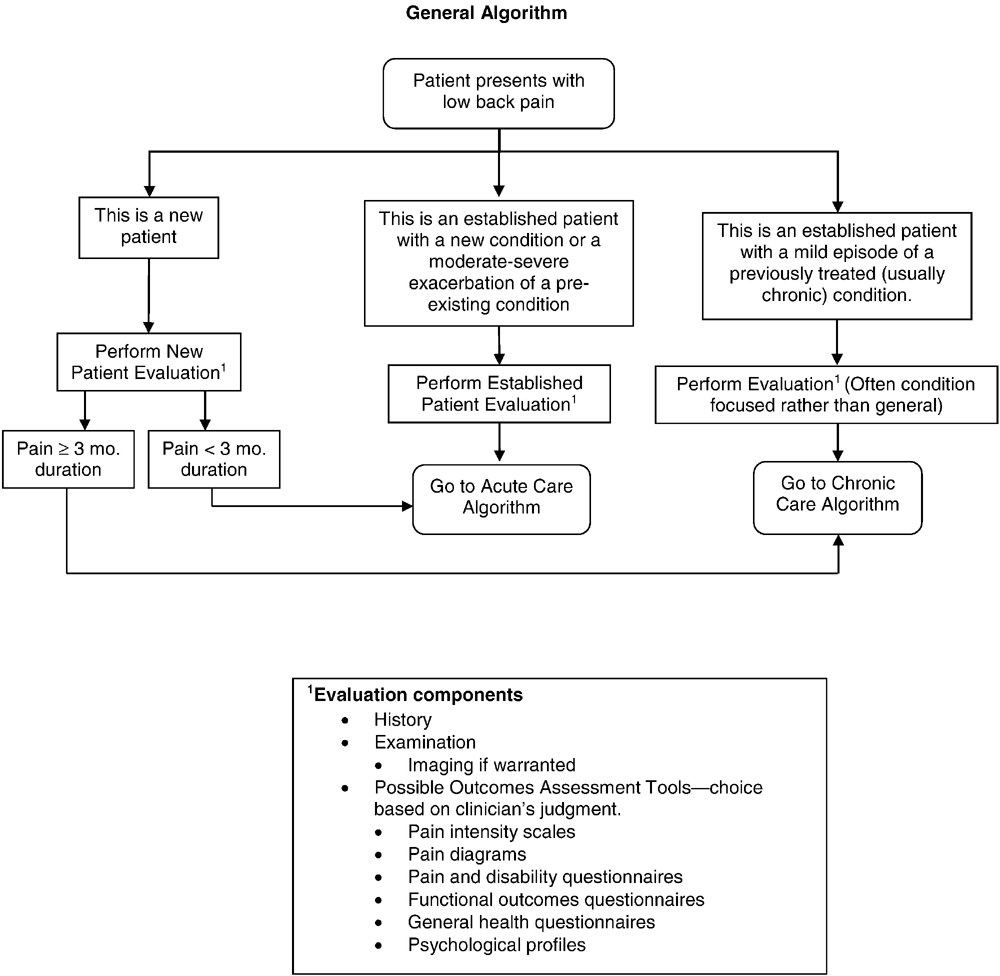
Figure 6B.
Acute Care Algorithm
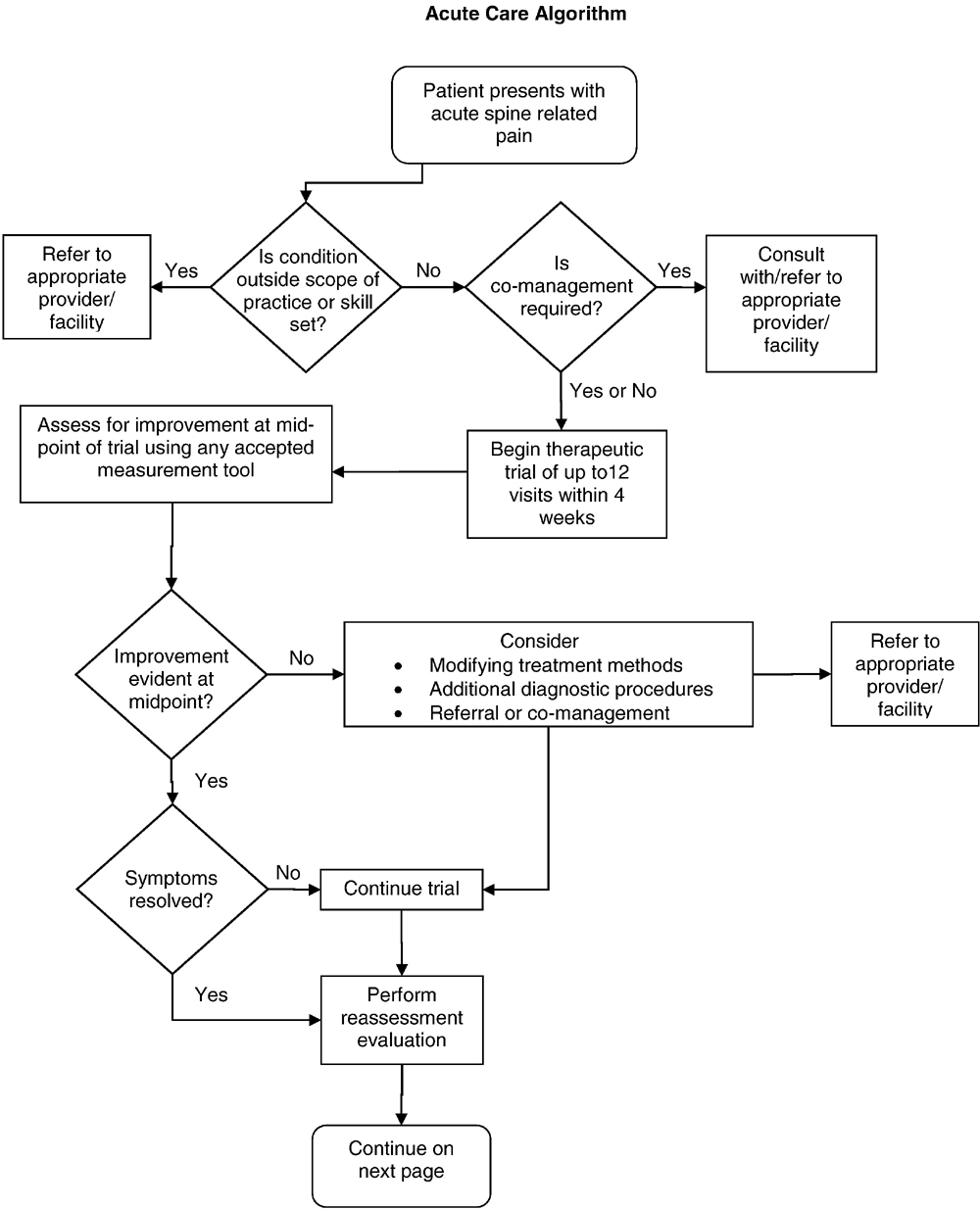
Figure 6C.
Acute Care Algorithm (cont.)

Figure 6D.
Chronic Pain Algorithm

Figure 6E.
Chronic Pain Algorithm (cont.)
Discussion
With the chiropractic profession’s establishment of the CCGPP to facilitate the development of best practices, 3 guidelines addressing the management of low back disorders were ultimately published. [9, 10, 12] This set in motion an effort to improve clinical methods by reducing variation in chiropractic treatment patterns that has long been unaddressed by any other evidence-informed and consensus-driven official guideline. [16, 54, 55, 62, 63, 72] The approach to the development of these recommendations has been evolutionary so as to guide the profession toward the utilization of more evidence-informed clinical methods intended to improve patient outcomes. Historically, this also explains why the initial low back guideline, published in 2008, required 2 subsequent additional guidelines to expand on acute and chronic conditions. This was practical to introduce additional guidance in a stepwise fashion.
The focus of these recommendations has been patient centered and not practitioner centered. Practices and techniques that have not demonstrated superior efficacy in published studies may be used as alternative approaches to those methods that have more robust evidence. No other guidelines have been specific to this purpose within the chiropractic profession and endorsed as broadly, making this guideline unique. It is also important to consider that guidelines specific to other professions may or may not include clinical approaches that do not best inform chiropractic management of low back disorders. Although evidence produced under the auspices of other professions is important to consider, it is also important to consider whether this evidence informs a conservative care approach. For example, from a chiropractic viewpoint, drug and surgical treatment approaches are generally regarded as more invasive and should be considered as second- and third-line approaches to the treatment of low back disorders. That is why we believe that professional guidelines specific to a profession’s scope and approach to intervening in the natural course of disease are important.
It is the responsibility of a profession to periodically update guidelines to ensure consistency with new research findings and subsequent clinical experience. As such, an updated literature review was conducted, and the previous best practice guidelines were revised. The evidence reviewed has informed several important new recommendations to this updated guideline. For example, the evidence informs us that the routine use of radiographic imaging studies is not in the best interest of most patients with nonspecific LBP. [53, 55] However, there may be exceptions to this based upon history and clinical examination characteristics. Doctors of chiropractic are advised that it is frequently in the best interest of patients to select manual method approaches that do not rely on radiographs to determine the method of manipulation or adjustment. [69] In addition, it is not in the patient’s best interest for the DC to use the least evidence-informed chiropractic techniques as their first-line approach over those where the evidence is more robust.
While adding important new recommendations, it is useful to note that the updated literature synthesis did not ultimately require many other changes from the original guideline recommendations. The changes reflected in this current update were as follows:(1) a brief description of key elements that should standardly be included during an informed consent discussion;
(2) the recommendation that routine radiographs, other imaging, and other diagnostic tests are not recommended for patients with nonspecific LBP (along with recommendations for when these studies should be considered);
(3) recommendation that the hierarchy of clinical methods used in patient care should generally correspond to the supporting level of existing evidence;
(4) additional clarification about the limited use of therapeutic modalities and lumbar supports that reflects patient preferences with the intention to best facilitate the shift from passive-to-active care and not dependency on passive modalities with limited evidence of efficacy;
(5) recognition that although range of motion testing may be clinically useful as a part of the physical examination to assess for regional mobility, the evidence does not support its reliability in determining functional status; and
(6) inclusion of a brief summary of the evidence informing manipulation risk vs benefit assessment.Although this revision contemplates new guidance on key practice areas, it is not expected that these new recommendations will necessarily apply to every patient seen by a DC.
Similarly, with respect to the dosage recommendations (ie, treatment frequency and duration) within this guideline, dosage should be modified to fit the individual patient’s needs. For example, the majority of chronic pain patients can self-manage, can be managed in short episodic bursts of care, or require ongoing care at 1–2 visits per month, to be reevaluated at a minimum of every 12 visits. It is rare that a patient would require 4 visits per month to manage advanced or complicated chronic pain. Thus, it is important to consider this guideline’s recommendations for visit frequency as ranges rather than specific numbers. In addition, with regard to continuing assessments to evaluate the effectiveness of treatment, after the initial round of up to 6 visits, a brief evaluation should be performed to evaluate the progress of care. Such reevaluations at a minimum should include assessment of subjective and/or objective factors. These might include using pain scales such as the visual analog scale, the numeric rating scale, pain diagrams, and/or validated ADL measures, such as the Revised Oswestry Back Disability Index, Roland Morris Back Disability Index, RAND 36, or the Bournemouth Disability Questionnaire. Additional orthopedic/neurological tests may be considered on a case-by-case basis.
Nothing in this guideline should be interpreted as saying that patients should never have imaging ordered based upon examination and clinical judgment. Similarly, the conclusion should not be that every patient should only receive treatment methods with the highest level of evidence. It is the recommendation of this guideline that imaging and clinical methods have evidence to inform their use. In addition, patients should be informed when their care appears to require a trial of an alternate, less evidence-informed strategy.
Regarding the evidence used to support these guidelines, most clinical trials are limited in duration and usually reflect a target patient population that is not necessarily representative of all patients encountered in standard practice. Patients possess characteristics that include risk factors (ie, age, history of previous episodes of LBP, etc) and other clinical characteristics that were not specifically assessed in clinical trials. Therefore, it is important to view practice guidelines in this context and that a 1–size-fits-all approach will not fit all patients. It is the collective judgment of CCGPP, the Delphi panelists, and the authors that unexplainable and unnecessary variation in treatment patterns for standard presentations of nonspecific LBP, without considering or using the best evidence, will not necessarily lead to improvements in clinical methods and improved patient outcomes.
Future Studies
The work of developing and improving guidelines is a never-ending and time-consuming task. Therefore, the authors have suggested areas of patient management that should be considered during future revisions. Three areas suggested during the manuscript review process were(1) guidance on the evidence of the value of limited rest at various phases of recovery across the range of low back disorders,
(2) more detailed guidance as to what history findings would/should lead to imaging, and
(3) review of the literature describing efforts to develop assessment methods and tools to characterize the predictors of outcomes and inform selection and greater standardization of clinical methods. [73, 74]Two areas of focus for future updates are also strongly recommended by the coauthors as well. The first concerns attempting to achieve a more detailed understanding of the hierarchy of chiropractic techniques that should be used based upon various archetypal patient presentations across the range of low back disorders. This would require reviewing head-to-head comparative research to determine relative efficacy of clinical methods using specific chiropractic techniques.
The authors recognize that some legacy outcome measures used in clinical practice and in clinical trials were not developed specifically with patients who may be interested in prioritizing conservative care approaches first. Also, because a measure’s ability to detect change and clinically minimal important difference (CMID) is linked directly to the target population and contextual characteristics, it is unlikely that there is a monolithic CMID value for a clinical outcomes assessment tool (including patient rated outcome measures) across all contexts of use and patient cohorts. More likely, there would be a range in CMID estimates that differs across varying patient cohorts and clinical trial contexts. [75] The chiropractic profession has relied upon instruments that are less sensitive to changes in the types of risks, adverse effects, symptoms, and impacts that chiropractic patients might consider most important. This includes the benefits of avoidance of risks and adverse events associated with medication use and surgical interventions. As such, a comprehensive review is recommended to determine the evidence for the use of these legacy instruments in practice as well as, most critically, clinical trials that include the evaluation of the outcomes of the treatment of low back disorders that include chiropractic subjects. This type of review should include members who have a background in outcomes measurement and the development of de novo patient-reported outcomes instruments. Finally, an ever-broadening horizon of new and ongoing areas of related research constantly needs to be scanned for updated and applicable learnings, such as improved understanding of the interplay between functional anatomy (eg, muscular and fascial) and the generation of LBP. [76, 77]
Limitations
This guideline did not address several important issues that future efforts should focus on, including the following: the important issues of appropriate recommendations on limited rest; guidance on how DCs should assess history findings that might require imaging; expanded review and assessment of comparative efficacy of chiropractic manipulative techniques; and a full-scale review of outcome measures used by chiropractors and chiropractic researchers to evaluate the suitability of legacy measures as well as the robustness of their reported CMID in the context of populations frequently treated by chiropractors. [78–80]
Our Delphi panel may not have represented the broadest spectrum of DCs in terms of philosophy and approach to practice. In addition, this guideline is most applicable to chiropractic practice in the United States. Input from other professions was present but also limited to 4 members from other professions (acupuncture, massage therapy, medicine, and physical therapy). However, the panel had geographic diversity and was clearly based upon practice expertise with 33 of 37 panelists being in practice an average 27 years.
Another limitation relates to the literature included in the systematic review, which extended through February 2014 to provide time for project implementation. It is possible that articles were inadvertently excluded. An important issue related to the literature is that issues of great practical importance, such as the determination of optimal procedures and protocols for specific patients, do not yet have enough high-quality evidence to make detailed recommendations. An example of this is the use of a wide variety of manipulative techniques by DCs, [19] even though most randomized trials use only HVLA manipulation, due to the requirements of the study design for uniformity of the intervention. As the evidence base for manipulative techniques grows and expands its scope, it is essential that CPGs continue to be updated in response to new evidence. Although the authors did not task themselves with the responsibility of developing a formal dissemination plan, CCGPP is currently developing one to coordinate with the timing of the publication of this guideline.
Finally, any guideline recommendations are limited by those who would use partial statements, out of context, to justify a treatment, utilization, and/or reimbursement decision. It is critical to the appropriate use of this CPG that recommendations are not misconstrued by being taken out of context by the use of partial statements. To avoid such practice, we strongly recommend that when a quote from this guideline is to be used, an entire paragraph be included to contextualize the recommendation being cited.
Conclusion
This publication is an update of the best practice recommendations for chiropractic management of LBP. [9, 10, 12] This guide summarizes recommendations throughout the continuum of care from acute to chronic and offers the chiropractic profession and other key stakeholders an up-to-date evidence- and clinical practice experience–informed resource outlining best practice approaches for the treatment of patients with LBP.
Funding Sources and Conflicts of Interest
All authors and panelists participated without compensation from any organization. Logan University made an in-kind contribution to the project by allowing Drs. Hawk and Kaeser and Ms. Anderson and Walters to devote a portion of their work time to this project. The University of Western States also provided in-kind support for a portion of Dr. Hawk’s time. Dr. Farabaugh currently holds the position of the National Physical Medicine Director of Advanced Medical Integration Group, LP. Dr. Morris is a post-graduate faculty member of the National University of Health Sciences and receives access to library resources. There were no conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): C.H., G.G., C.M., W.W., G.B.
Design (planned the methods to generate the results): C.H., G.G.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): C.H., G.G., C.M.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): C.H.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): C.H., G.G., C.M., G.B.
Literature search (performed the literature search): C.H., M.K., S.W., R.F., G.G., C.M.
Writing (responsible for writing a substantive part of the manuscript): C.H., R.F., G.G., C.M., W.W., G.B.
Critical review (revised manuscript for intellectual content; this does not relate to spelling and grammar checking): C.H., M.K., S.W., R.F., M.D., G.G., C.M., W.W., M.D., G.B., T.A.
Acknowledgment
The authors thank Michelle Anderson, project coordinator, who ensured that all communications were completed smoothly and in a timely manner. The experts, listed below, who served on the Delphi panel made this project possible by generously donating their expertise and clinical judgment.
Logan University panelists who developed the seed document that served as the basis for the consensus process: Robin McCauley Bozark, DC; Karen Dishauzi, DC, MEd; Krista Gerau, DC; Edward Johnnie, DC; Aimee Jokerst, DC; Jeffrey Kamper, DC; Norman Kettner, DC; Janine Ludwinski, DC; Donna Mannello, DC; Anthony Miller, DC; Patrick Montgomery, DC; Michael J. Wittmer, DC. Muriel Perillat, DC, MS, Logan Dean of Clinics, also provided an independent review of the document.
Delphi panelists for the consensus process: Charles Blum, DC; Bryan Bond, DC; Jeff Bonsell, DC; Jerrilyn Cambron, LMT, DC, MPH, PhD; Joseph Cipriano, DC; Mark Cotney, DC; Edward Cremata, DC; Don Cross, DC; Donald Dishman, DC; Gregory Doerr, DC; Paul Dougherty, DC; Joseph Ferstl, DC; Anthony Q. Hall, DC; Michael W. Hall, DC; Robert Hayden, DC, PhD; Kathryn Hoiriis, DC; Lawrence Humberstone, DC; Norman Kettner, DC; Robert Klein, DC; Kurt Kuhn, DC, PhD; William Lauretti, DC; Gene Lewis, DC, MPH; John Lockenour, DC; James McDaniel, DC; Martha Menard, PhD, LMT; Angela Nicholas, DC; Mariangela Penna, DC; Dan Spencer, DC; Albert Stabile, DC; John S. Stites, DC; Kasey Sudkamp, DPT; Leonard Suiter, DC; John Ventura, DC; Sivarama Vinjamury, MD, MAOM, MPH, LAc; Jeffrey Weber, MA, DC; Gregory Yoshida, MD.
References:
Meeker, W., & Haldeman, S. (2002).
Chiropractic: A Profession at the Crossroads
of Mainstream and Alternative Medicine
Annals of Internal Medicine 2002 (Feb 5); 136 (3): 216–227Coulter, I.
The roles of philosophy and belief systems in complementary and alternative health care.
in: Paper presented at: Conference on Philosophy of Chiropractic Education 2000; Toronto.LeFebvre R, Peterson D, Haas M:
Evidence-Based Practice and Chiropractic Care
J Evid Based Complementary Altern Med 2012 (Dec 28); 18 (1): 75–79Triano, J and Raley, B.
Chiropractic in the interdisciplinary team practice.
Top Clin Chiropr. 1994; 1: 58–66Triano, JJ.
Literature syntheses for the Council on Chiropractic Guidelines and Practice Parameters: methodology.
J Manipulative Physiol Ther. 2008; 31: 645–650Triano, JJ.
What Constitutes Evidence For Best Practice?
J Manipulative Physiol Ther. 2008 (Nov); 31 (9): 637–643Triano, JJ, Goertz, C, Weeks, J et al.
Chiropractic in North America: toward a strategic plan for professional renewal—outcomes from the 2006 Chiropractic Strategic Planning Conference.
J Manipulative Physiol Ther. 2010; 33: 395–405Lawrence DJ, Meeker W, Branson R, Bronfort G, Cates JR, Haas M, Haneline M et al.
Chiropractic Management of Low Back Pain and Low Back-Related
Leg Complaints: A Literature Synthesis
J Manipulative Physiol Ther 2008 (Nov); 31 (9): 659–674Globe GA, Morris CE, Whalen WM, et al.
Chiropractic Management of Low Back Disorders:
Report From a Consensus Process
J Manipulative Physiol Ther 2008 (Nov); 31 (9): 651–658Baker, G, Farabaugh, RJ, Augat, TJ, and Hawk, C.
Algorithms for the Chiropractic Management of Acute
and Chronic Spine-Related Pain
Topics in Integrative Health Care 2012 (Dec 31); 3 (4)Dehen, MD, Whalen, WM, Farabaugh, RJ, and Hawk, C.
Consensus Terminology for Stages of Care:
Acute, Chronic, Recurrent, and Wellness
J Manipulative Physiol Ther. 2010 (Jul); 33 (6): 458–463Farabaugh, RJ, Dehen, MD, and Hawk, C.
Management of Chronic Spine-Related Conditions:
Consensus Recommendations of a Multidisciplinary Panel
J Manipulative Physiol Ther 2010 (Sep); 33 (7): 484–492Sackett, DL, Rosenberg, WM, Gray, JA, Haynes, RB, and Richardson, WS.
Evidence-Based Medicine: What It Is and What It Isn't
British Medical Journal 1996 (Jan 13); 312 (7023): 71–72Sackett, DL, Straus, SE, Richardson, WS et al.
Evidence-based medicine: how to practice and teach EBM. 2nd ed.
Church Livingston, Edinburgh; 2000Slaughter, AL, Frith, K, O'Keefe, L, Alexander, S, and Stoll, R.
Promoting best practices for managing acute low back pain in an occupational environment.
Workplace Health Saf. 2015; 63: 408–414Haldeman S, Dagenais S.
What Have We Learned About the Evidence-informed
Management of Chronic Low Back Pain?
Spine J. 2008 (Jan); 8 (1): 266–277Clar C, Tsertsvadze A, Court R, Hundt G, Clarke A, Sutcliffe P.
Clinical Effectiveness of Manual Therapy for the Management of
Musculoskeletal and Non-Musculoskeletal Conditions:
Systematic Review and Update of UK Evidence Report
Chiropractic & Manual Therapies 2014 (Mar 28); 22 (1): 12Council on Chiropractic Education.
Accreditation standards, principles, processes & requirements for accreditation.
2013 (Scottsdale, AZ)Christensen, M, Kollasch, M, and Hyland, JK.
Practice analysis of chiropractic 2010
NBCE, Greeley, CO; 2010Bronfort G, Haas M, Evans R, Leiniger B, Triano J.
Effectiveness of Manual Therapies: The UK Evidence Report
Chiropractic & Osteopathy 2010 (Feb 25); 18 (1): 3Hawk, C, Schneider, M, Evans, MW, and Redwood, D.
Consensus Process to Develop a Best-Practice Document
on the Role of Chiropractic Care in Health Promotion,
Disease Prevention, and Wellness
J Manipulative Physiol Ther. 2012 (Sep); 35 (7): 556–567Hawk, C, Khorsan, R, Lisi, AJ, Ferrance, RJ, and Evans, MW.
Chiropractic Care for Nonmusculoskeletal Conditions:
A Systematic Review With Implications For
Whole Systems Research
J Altern Complement Med. 2007 (Jun); 13 (5): 491–512Hawk, C, Schneider, M, Dougherty, P, Gleberzon, BJ, and Killinger, LZ.
Best Practices Recommendations for Chiropractic Care for
Older Adults: Results of a Consensus Process
J Manipulative Physiol Ther 2010 (Jul); 33 (6): 464-473Hawk, C, Schneider, M, Ferrance, RJ, Hewitt, E, Van Loon, M, and Tanis, L.
Best Practices Recommendations for Chiropractic Care for Infants,
Children, and Adolescents: Results of a Consensus Process
J Manipulative Physiol Ther. 2009 (Oct); 32 (8): 639–647Schneider, M, Vernon, H, Ko, G, Lawson, G, and Perera, J.
Chiropractic management of fibromyalgia syndrome: a systematic review of the literature.
J Manipulative Physiol Ther. 2009; 32: 25–40Vernon, H and Schneider, M.
Chiropractic Management of Myofascial Trigger Points and Myofascial
Pain Syndrome: A Systematic Review of the Literature
J Manipulative Physiol Ther. 2009 (Jan); 32 (1): 14–24Pfefer, MT, Cooper, SR, and Uhl, NL.
Chiropractic management of tendinopathy: a literature synthesis.
J Manipulative Physiol Ther. 2009; 32: 41–52Brantingham, JW, Bonnefin, D, Perle, SM et al.
Manipulative therapy for lower extremity conditions: update of a literature review.
J Manipulative Physiol Ther. 2012; 35: 127–166Brantingham, JW, Cassa, TK, Bonnefin, D et al.
Manipulative therapy for shoulder pain and disorders: expansion of a systematic review.
J Manipulative Physiol Ther. 2011; 34: 314–346Brantingham, JW, Cassa, TK, Bonnefin, D et al.
Manipulative and multimodal therapy for upper extremity and temporomandibular disorders: a systematic review.
J Manipulative Physiol Ther. 2013; 36: 143–201Brantingham, JW, Globe, G, Pollard, H, Hicks, M, Korporaal, C, and Hoskins, W.
Manipulative therapy for lower extremity conditions: expansion of literature review.
J Manipulative Physiol Ther. 2009; 32: 53–71Brantingham, JW, Parkin-Smith, G, Cassa, TK et al.
Full kinetic chain manual and manipulative therapy plus exercise compared with targeted manual and manipulative therapy plus exercise for symptomatic osteoarthritis of the hip: a randomized controlled trial.
Arch Phys Med Rehabil. 2012; 93: 259–267Becker, M, Neugebauer, EA, and Eikermann, M.
Partial updating of clinical practice guidelines often makes more sense than full updating: a systematic review on methods and the development of an updating procedure.
J Clin Epidemiol. 2014; 67: 33–45Shekelle, P, Woolf, S, Grimshaw, JM, Schunemann, HJ, and Eccles, MP.
Developing Clinical Practice Guidelines: Reviewing, Reporting, and
Publishing Guidelines; Updating Guidelines; and the Emerging
Issues of Enhancing Guideline Implementability and Accounting
for Comorbid Conditions in Guideline Development
Implementation Science 2012 (Jul 4); 7: 62The AGREE Next Steps Consortium.
Appraisal of guidelines for research and evaluation II.
2013 ([Ontario, Canada])Moher D, Liberati A, Tetzlaff J, Altman DG.
Preferred Reporting Items for Systematic Reviews
and Meta-Analyses: The PRISMA Statement
PLoS Medicine 2009 (Jul 21); 6 (7): e1000100Dagenais, S., Gay, R. E., Tricco, A. C., Freeman, M. D., & Mayer, J. M.
NASS Contemporary Concepts in Spine Care:
Spinal Manipulation Therapy for Acute Low Back Pain
The Spine Journal 2010 (Oct); 10 (10): 918-940Dagenais S, Tricco AC, Haldeman S.
Synthesis of Recommendations for the Assessment and Management
of Low Back Pain From Recent Clinical Practice Guidelines
Spine J. 2010 (Jun); 10 (6): 514–529Furlan, AD, Yazdi, F, Tsertsvadze, A et al.
Complementary and Alternative Therapies for Back Pain II
Evidence/Technology Report Number 194
AHRQ Publication No. 10(11)-E007 (October 2010),
U.S. Department of Health and Human Services, Rockville, MDGoertz CM, Pohlman KA, Vining RV, Brantingham JW, Long CR.
Patient-centered Outcomes of High-velocity, Low-amplitude
Spinal Manipulation for Low Back Pain: A Systematic Review
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 670–691Hidalgo, B, Detrembleur, C, Hall, T, Mahaudens, P, and Nielens, H.
The Efficacy of Manual Therapy and Exercise for Different Stages of
Non-specific Low Back Pain: An Update of Systematic Reviews
J Man Manip Ther. 2014 (May); 22 (2): 59–74Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C.
An Updated Overview of Clinical Guidelines for the Management of
Non-specific Low Back Pain in Primary Care
European Spine Journal 2010 (Dec); 19 (12): 2075–2094McIntosh, G and Hall, H.
Low back pain (acute).
BMJ Clin Evid. 2011; 2011Posadzki, P and Ernst, E.
Spinal manipulations for cervicogenic headaches: a systematic review of randomized clinical trials.
Headache. 2011; 51: 1132–1139Rubinstein, SM, Terwee, CB, Assendelft, WJ, de Boer, MR, and van Tulder, MW.
Spinal manipulative therapy for acute low back pain: an update of the cochrane review.
Spine (Phila Pa 1976). 2013; 38: E158–E177Rubinstein, SM, van Middelkoop, M, Assendelft, WJ, de Boer, MR, and van Tulder, MW.
Spinal manipulative therapy for chronic low-back pain: an update of a Cochrane review.
Spine (Phila Pa 1976). 2011; 36: E825–E846Haas M, Vavrek D, Peterson D, Polissar N, Neradilek MB.
Dose-response and Efficacy of Spinal Manipulation for Care of
Chronic Low Back Pain: A Randomized Controlled Trial
Spine J. 2014 (Jul 1); 14 (7): 1106–1116Senna M.K., Machaly S.A.
Does Maintained Spinal Manipulation Therapy for Chronic Non-specific
Low Back Pain Result in Better Long Term Outcome?
Spine (Phila Pa 1976) 2011 (Aug 15); 36 (18): 1427–1437von HeymannWJ, Schloemer P, Timm J, Muehlbauer B.
Spinal High-velocity Low Amplitude Manipulation in Acute Nonspecific
Low Back Pain: A Double-blinded Randomized Controlled Trial
in Comparison With Diclofenac and Placebo
Spine (Phila Pa 1976) 2013 (Apr 1); 38 (7): 540–548Walker BF, Hebert JJ, Stomski NJ, Losco B, French SD.
Short-term Usual Chiropractic Care for Spinal Pain:
A Randomized Controlled Trial
Spine (Phila Pa 1976). 2013 (Nov 15); 38 (24): 2071–2078Ernst, E.
Chiropractic spinal manipulation: what does the 'best' evidence show?.
Focus Altern Complement Ther. 2012; 17: E463–E472Menke, JM.
Do manual therapies help low back pain? A comparative effectiveness meta-analysis.
Spine (Phila Pa 1976). 2014; 39: E463–E472Chou, R, Fu, R, Carrino, JA, and Deyo, RA.
Imaging strategies for low-back pain: systematic review and meta-analysis.
Lancet. 2009; 373: 463–472Chou R, Huffman LH; American Pain Society.
Nonpharmacologic Therapies for Acute and Chronic Low Back Pain:
A Review of the Evidence for an American Pain Society/
American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 492–504Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr., Shekelle P, Owens DK:
Diagnosis and Treatment of Low Back Pain: A Joint Clinical
Practice Guideline from the American College of Physicians
and the American Pain Society
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 478–491Chou, WC, Tinetti, ME, King, MB, Irwin, K, and Fortinsky, RH.
Perceptions of physicians on the barriers and facilitators to integrating fall risk evaluation and management into practice.
J Gen Intern Med. 2006; 21: 117–122Guzman J, Haldeman S, Carroll LJ, et al.
Clinical Practice Implications of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders:
From Concepts and Findings to Recommendations
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S199–S212Haas, M, Bronfort, G, and Evans, RL.
Chiropractic clinical research: progress and recommendations.
J Manipulative Physiol Ther. 2006; 29: 695–706Haas, M, Jacobs, GE, Raphael, R, and Petzing, K.
Low back pain outcome measurement assessment in chiropractic teaching clinics: responsiveness and applicability of two functional disability questionnaires.
J Manipulative Physiol Ther. 1995; 18: 79–87Haas M, Sharma R, Stano M.
Cost-effectiveness of Medical and Chiropractic Care for Acute
and Chronic Low Back Pain
J Manipulative Physiol Ther 2005 (Oct); 28 (8): 555–563Haldeman S, Carroll L, Cassidy JD, Schubert J, Nygren A.
The Bone and Joint Decade 2000–2010 Task Force on Neck Pain
and Its Associated Disorders: Executive Summary
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S5–7Haldeman S, Chapman-Smith D, Peterson, DM Jr.
Guidelines for Chiropractic Quality Assurance and Practice Parameters
Proceedings of a consensus conference commissioned by the Congress of
Chiropractic State Associations, held at the Mercy Conference Center,
Burlingame, CA, January 25-30, 1992.
Gaithersburg, MD: Aspen, 1993Haldeman S, Dagenais S.
A Supermarket Approach to the Evidence-informed Management
of Chronic Low Back Pain
Spine Journal 2008 (Jan); 8 (1): 1–7Fitch, K, Bernstein, SJ, Aquilar, MS et al.
The RAND UCLA Appropriateness Method user's manual.
RAND Corp., Santa Monica, CA; 2003American Medical Association.
Guide to the evaluation of permanent impairment. 6th ed.
American Medical Association, Chicago; 2008Schneider, M, Haas, M, Glick, R, Stevans, J, and Landsittel, D.
Comparison of Spinal Manipulation Methods and Usual Medical Care
for Acute and Subacute Low Back Pain:
A Randomized Clinical Trial
Spine (Phila Pa 1976). 2015 (Feb 15); 40 (4): 209–217National Institute for Health and Clinical Excellence (NICE).
Low Back Pain: Early Management of Persistent Nonspecific Low Back Pain
London: National Institute for Health and Care Excellence; 2009.
[Report No.: Clinical guideline 88].van Duijvenbode, I, Jellema, P, van Poppel, MN, and van Tulder, MW.
Lumbar supports for prevention and treatment of low back pain.
Cochrane Database Syst Rev. 2011; : CD001823Triano J, Budgell B, Bagnulo A, Roffey B, Bergmann T, Cooperstein R.
Review of Methods Used by Chiropractors to Determine
the Site for Applying Manipulation
Chiropractic & Manual Therapies 2013 (Oct 21); 21 (1): 36Carnes, D, Mars, TS, Mullinger, B, Froud, R, and Underwood, M.
Adverse events and manual therapy: a systematic review.
Man Ther. 2010; 15: 355–363Dabbs V Lauretti WJ
A Risk Assessment of Cervical Manipulation vs. NSAIDs
for the Treatment of Neck Pain
J Manipulative Physiol Ther 1995 (Oct); 18 (8): 530–536Boswell, MV, Trescot, AM, Datta, S et al.
Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain.
Pain Physician. 2007; 10: 7–111R.A. Deyo, S.F. Dworkin, D. Amtmann, G. Andersson, et al.,
Report of the NIH Task Force on Research Standards
for Chronic Low Back Pain
Journal of Pain 2014 (Jun); 15 (6): 569–585Russell, R.
The Rationale for Primary Spine Care Employing Biopsychosocial,
Stratified and Diagnosis-based Care-pathways at a
Chiropractic College Public Clinic:
A Literature Review
Chiropractic & Manual Therapies 2013 (Jun 9); 21 (1): 19Revicki, D, Hays, RD, Cella, D, and Sloan, J.
Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes.
J Clin Epidemiol. 2008; 61: 102–109Bush, HM, Pagorek, S, Kuperstein, J, Guo, J, Ballert, KN, and Crofford, LJ.
The association of chronic back pain and stress urinary incontinence: a cross-sectional study.
J Womens Health Phys Ther. 2013; 37: 11–18Bi, X, Zhao, J, Zhao, L et al.
Pelvic floor muscle exercise for chronic low back pain.
J Int Med Res. 2013; 41: 146–152Parkin-Smith GF, Norman IJ, Briggs E, Angier E, Wood TG, Brantingham JW.
A Structured Protocol of Evidence-based Conservative Care Compared
with Usual Care for Acute Nonspecific Low Back Pain:
A Randomized Clinical Trial
Arch Phys Med Rehabil. 2012 (Jan); 93 (1): 11–20Peterson C, Bolton J, Humphreys BK.
Predictors of Outcome in Neck Pain Patients Undergoing
Chiropractic Care: Comparison of Acute
and Chronic Patients
Chiropractic & Manual Therapies 2012 (Aug 24); 20 (1): 27Peterson CK, Bolton J, Humphreys BK.
Predictors of Improvement in Patients With Acute and Chronic
Low Back Pain Undergoing Chiropractic Treatment
J Manipulative Physiol Ther. 2012 (Sep); 35 (7): 525-533
Return to LOW BACK PAIN
Return to LOW BACK GUIDELINES
Return to EVIDENCE–BASED PRACTICE
Return to BEST PRACTICES IN CHIROPRACTIC
Since 7-28-2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |