

Deconstructing Chronic Low Back Pain in the Older Adult- Step by Step
Evidence and Expert-Based Recommendations for Evaluation and Treatment:
Part X: Sacroiliac Joint SyndromeThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Pain Medicine 2016 (Sep); 17 (9): 16381647 ~ FULL TEXT
OPEN ACCESS Patrick J. Polsunas, BS, Gwendolyn Sowa, MD, PhD, Julie M. Fritz, PT, PhD,
Angela Gentili, MD, Natalia E. Morone, MD, MS, Srinivasa Naga Raja, MD,
Eric Rodriguez, MD, Kenneth Schmader, MD, Joel D. Scholten, MD, Debra K. Weiner, MD
University of Pittsburgh School of Medicine,
Pittsburgh, PA
debra.weiner@va.govOBJECTIVE: To present an algorithm of sequential treatment options for managing sacroiliac joint (SIJ) pain in the setting of chronic low back pain (CLBP) in the older adult. This is the tenth part in a series, and includes an illustrative clinical case.
METHODS: The stepped care drug table and evaluation and treatment algorithm were created following a thorough literature review of approaches and subsequent analysis through a modified Delphi process. The principal investigator developed the initial draft, which was refined for content by an interdisciplinary panel of five experts. The refined materials were then assessed for the feasibility of implementation and validity of recommendations for older adults in a primary care setting by a panel of nine primary care providers. While not exclusive to Veteran's Health Administration (VHA) facilities, an emphasis was made to include resources and medications available to providers in the VHA.
RESULTS: The algorithm and drug table developed to systematically identify and address SIJ pain in the older adult is presented here. The process should begin with recognizing the presenting symptoms of CLBP stemming from the SI region, and supporting physical exam testing using the compression test and thigh thrust maneuver. Identification of the SIJ as a pain generator is followed by assessment and treatment of contributory factors. SIJ pain treatment should begin with education and self-management including exercise, and may escalate to include interventional procedures and/or referral to a pain rehabilitation program.
CONCLUSIONS: Pain originating from the SIJ is often under-recognized, but a structured and consistent approach can help identify older patients who would benefit from treatment of this contributor to CLBP.
KEYWORDS: Chronic Low Back Pain; Sacroiliac Joint Pain; Older Adults.
From the FULL TEXT Article:
Introduction
The understanding of the sacroiliac joints (SIJs) has a complex history stretching back centuries. [1] Debate over their form, function, specific contribution to CLBP, and how to effectively identify and treat pain originating from the SIJ continues today.
The first of a two-part study by Fortin et al. in 1994 [2] helped establish the fact that pain can arise from the SIJ itself through intra-articular injections of contrast in asymptomatic controls. The second part sought to develop a screening tool to aid in the clinical diagnosis of SIJ pain [3]; more than two decades later, the ideal evaluation methods have yet to be defined.
Complicating the effort to make a diagnosis is the well-established recognition that pain that appears in the region of the SIJ can originate from other sources, including herniated discs and facet joints. [4, 5] Conversely, pain originating from the SIJ can refer to the groin and adjacent areas such as the gluteal muscles and lower extremity, even as far as the foot. [6] Furthermore, as described by King et al., consistency within the literature on the precise usage of SIJ pain as intra- vs extra-articular in origin is lacking; the former, they describe as true SIJ pain, while the latter would more properly defined as sacroiliac complex pain, which would include pain originating from the supporting ligaments. [7]
Imaging, including computed tomography (CT) and magnetic resonance imaging (MRI), can be useful in the identification of sacroiliitis associated with trauma or ankylosing spondylitis (AS) [8]; the latter rarely presents symptomatically in patients beyond their fifth decade. [9] However, in the absence of these conditions, imaging findings are rarely helpful in identifying the sacroiliac joint as a pain generator. Further complicating radiographic diagnosis is the common co-existence of degenerative changes observed in lumbar spine imaging of older adults. As discussed earlier in this series [10, 11], Hicks et al. performed radiographic assessment of 320 subjects over 65, 162 with CLBP alongside 158 without pain, and discovered that 95% of subjects in both groups showed evidence of degenerative disc disease [12], while Jarvik et al. identified moderate or severe stenosis in the lumbar spine in 21% of a small group [13] of pain-free adults over 65 when examined by MRI. The near-ubiquity of degenerative findings on plain radiographic [12] or advanced imaging [13] suggest that these modalities have little if any value used as a screening test establishing a specific cause and guiding treatment of CLBP in the older adult.
This article aims to define an algorithm for treatment of patients with suspected or confirmed LBP that originates in the SI joints. We present a case adapted from a patient cared for by one of the contributors. We describe what may be a familiar patient presentation to a clinician managing the health and wellbeing of adults in the later stages of life, and how to systematically address the often complex problem of CLBP.
Methods

Figure 1

Table 1

Table 2 As part of the special series addressing CLBP in older adults, this work utilized the modified Delphi technique described in detail in the introduction to this series [ 10 ]. Through that process, an algorithm (Figure 1) and corresponding evidence table (Table 1) were developed, along with a stepped care drug management table (Table 2). The panel of five experts was comprised of two physiatrists, physical therapist, internal medicine physician, and a pain anesthesiologist. One member of the team had a primary appointment in the VA Healthcare System. The completed algorithm was reviewed by a panel of nine primary care physicians, followed by feedback and modification to result in the final algorithm.
Case Presentation
Relevant History
The patient was a 69-year-old female with a 2-year history of low back/buttock/hip pain radiating to the left lower extremity that began after surgical treatment for chronic left foot pain. Three years prior she was diagnosed with posterior tibial tendon dysfunction, and subsequently underwent triple arthrodesis at the subtalar, talonavicular, and calcaneocuboid joints of the left foot, with a revision due to nonunion 6 months prior to presentation. Her low back pain began 1 year after her initial arthrodesis, which she felt was due to her foot pain causing irregularities in her gait. Pain was reported as always present, with a baseline severity of 4/10 and frequent increases to 10/10. She states that the pain was worsened by transitions between sitting and standing, walking long distances, and lying for long periods on her back or side. She was no longer able to vacuum her home. The pain was mildly relieved by heat, rest, and forward flexion. She denied bladder or bowel incontinence, spinal trauma, weakness, numbness, tingling, or falls. Prior treatments included gabapentin, acetaminophen, topical lidocaine, several non-steroidal anti-inflammatory drugs (NSAIDs), L4-L5 epidural steroid injection, and physical therapy (PT) directed toward core strengthening. None of these interventions provided significant pain relief or functional improvement. She owned a cane and a walker, but felt steadier without them. She never used shoe orthoses. She was recently prescribed hydrocodone 10 mg/acetaminophen 325 mg to be taken every 4 hours as needed, which she typically took to get out of bed in the morning and to fall asleep at night.
Relevant Physical Examination
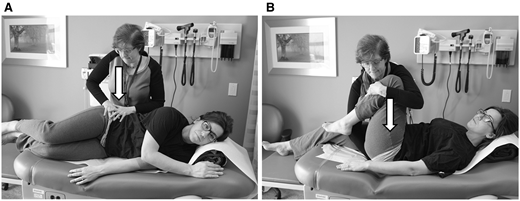
Figure 2 The patient was alert, oriented, pleasant, cooperative, and in no apparent distress. She had an antalgic gait that was slightly wide-based. Lumbar range of motion was pain limited, provocative in flexion, but not extension. There was no evidence of scoliosis or kyphosis. Significant tenderness was present on palpation of the left greater trochanter, no tenderness on the right greater trochanter. No leg length discrepancy was observed in the supine position. Anterior superior iliac spines were symmetric when standing. The left SIJ was tender to palpation but there was no tenderness on the right. Compression test (Figure 2 A) and thigh thrust ( Figure 2 B) maneuvers were provocative of low back pain symptoms on the left side and non-provocative on the right. Internal and external hip range of motion were normal and non-provocative of pain. The seated slump test, to evaluate for radiculopathy [14], was provocative of left posterior thigh pain, but demonstrated no change with release of dural tension (i.e., cervical extension), and non-provocative on the right. Straight leg raise was negative bilaterally. Bilateral strength, sensation, and reflexes in the lower extremities were symmetric and within normal limits. She had a pes planus deformity of the left foot, and impaired active and passive range of motion for left ankle plantarflexion and dorsiflexion.
Imaging
Lumbar x-rays from a previous provider obtained approximately 6 months prior to presentation showed grade 1 (mild) anterolisthesis of L4 on L5, preserved disc height and vertebral body height, and mild bilateral sclerosis of the sacroiliac joints, with left worse than right.
Clinical Course
The patient was started on a PT program with an emphasis on hip abductor strengthening and gait normalization, along with a home exercise program (HEP). Her hydrocodone/acetaminophen was discontinued, and tramadol was initiated. However, the tramadol precipitated migraine headaches, and was discontinued. She began using over-the-counter analgesics only as needed. Her back pain and functional status continued to decline over the following 4 months despite compliance with her HEP. She began having difficulty walking in the community. She was counseled on the risks and benefits of a fluoroscopically guided intra-articular SI joint injection, and decided to pursue this procedure. Following anesthetization of the skin, a 22-gauge, 3.5-inch spinal needle was advanced under continuous fluoroscopy into the left sacroiliac joint. Contrast agent was infused to ensure proper placement and a typical arthrographic joint pattern was produced. Depo-Medrol and 2% lidocaine were then infused. This injection reproduced her concordant back pain, and was therefore considered diagnostic. Following the procedure, the patient reported an immediate pain reduction from 10/10 to 4/10, with a 50% reduction in pain severity present at 6-week follow up. She was able to walk for considerably longer distances and sleep comfortably on her back and sides. With symptoms more effectively controlled, she was able to restart physical therapy along with her home exercise program, and continued to progress toward achieving her functional goals.
Approach to Management
This patient has CLBP that is likely multifactorial and has been aggravated by compensatory change in gait due to her chronic lower extremity pathology. Her foot pain had been present for nearly her entire adult life, but she experienced a significant increase in severity over the past decade, further exacerbated after a corrective surgical procedure. Her CLBP had previously been attributed to a variety of sources, including sciatica, lumbosacral degenerative disc disease, lumbar spinal stenosis, spondylolisthesis and lumbosacral neuritis before presenting to our clinic. Her initial exam provoked pain consistent with trochanteric bursitis [15], adding to the list of potential contributory sources. This complex history highlights the fact that CLBP is frequently multifactorial.

Figure 3
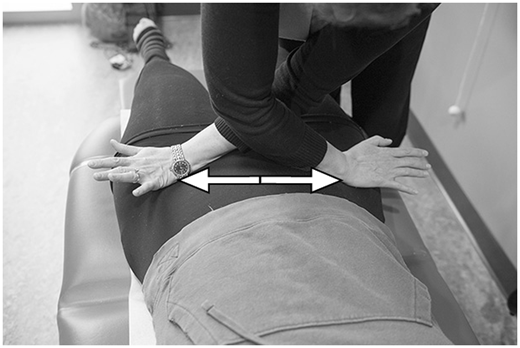
Figure 4
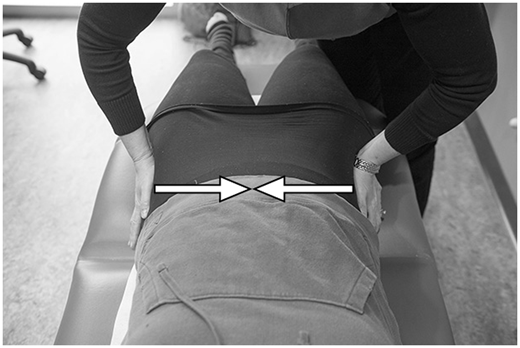
Figure 5

Figure 6 Van der Wurff et al. examined the diagnostic accuracy of a multi-test regimen for the sacroiliac joint, compared to fluoroscopically controlled double SIJ blocks. [16] This study of 27 patients suggested that a test regimen with three or more positive physical exam tests is indicative of SIJ pain and may be used to reduce diagnostic SIJ injections, corroborating previous studies. [17] Similarly, Szadek et al. described positive results on two pain provocation tests, the compression test (Figure 2 A) and thigh thrust (Figure 2 B) [18], as helpful in diagnosing SIJ pain. They also reported that three or more positive pain provocation tests is preferred to achieve a high diagnostic odds ratio (DOR), calculated as 17.2. However, they stressed that even this testing should be regarded cautiously, based on the potential for inter-practitioner variability, and acknowledged that the studies included were performed at academic centers or spine treatment units. Based on the available data and relative ease of performing the tests in a primary care practice, we recommend the compression test (side-lying) (Figure 2 A) and thigh thrust to satisfy consideration of the SIJ region as a pain generator in primary practice. Additional exam maneuvers, such as Patricks sign (FABERs) (Figure 3), distraction (Figure 4), compression (supine) (Figure 5), Gaenslen (Figure 6), and sacral thrust [16, 17] can be added to improve diagnostic accuracy based on the comfort level of the practitioner. These are shown in Figures 36. The sacral thrust test is not shown, as this is performed with the patient prone, a position that may be difficult for many older adults to comfortably assume. Of note, these physical exam maneuvers are performed most effectively using an adjustable or mat table. However, due to the frequent lack of availability of these exam tables in primary care offices, the exam technique is shown in its modified form using standard exam tables.
The algorithm presented (Figure 1) shows that the first step in addressing SI joint pain begins with identifying and treating potential contributory factors, including but not limited to hip osteoarthritis, kyphosis, scoliosis, leg length discrepancy, and osteoporosis.
This process should inform the next step: a referral to physical therapy. The therapist should educate the patient and teach them how to begin to manage their pain on their own, including instruction for a home exercise program. The therapist should target strengthening the hip abductors, correcting any impairments of strength or flexibility that may exist, and building both core and pelvic stability. These can include side-lying resistive exercises (clamshell, i.e., hip abduction with knees bent maintaining contact between the ankles, and straight leg abduction), weight-bearing exercises such as single leg standing, balance-related exercises, water-based training, or Tai Chi. [19] Some evidence also suggests that increasing balance may have the added benefit of reducing falls in older individuals [20] and there have been some promising results in programs integrating elements of CBT, specifically in patients with arthritis. [21, 22]
The third part of the initial plan should address pain directly, working with the patient to develop an approach to pain management that is sufficient to begin and maintain their therapeutic activity regimen. The patient should be counseled that the combination of physical therapy, self-care, and pharmacologic intervention should reduce pain by 30% at 6 weeks, noted previously to be a clinically important difference [23], and have a significant positive impact on their daily function. We recommend beginning with topical lidocaine or diclofenac gel alone or in combination with acetaminophen. It is also worth considering complementary and alternative medical (CAM) therapy such as acupuncture or massage for pain management. We do caution that limited evidence exists to confirm the efficacy for treating SI joint pain utilizing CAM interventions or the aforementioned topical preparations. Improvements in self-reported disability and pain have been reported with the use of sacroiliac joint belts (pelvic belts) [24] though this has not been explicitly studied in an older adult population. A wheeled walker may be prescribed if there is concern regarding stability or balance.
If these initial pharmacological interventions do not produce sufficient relief to allow for increased activity, the stepped care process outlined in Table 2 should be followed. Salsalate is recommended over other NSAIDs due to a lower risk of GI bleeding and renal toxicity from lack of effect on platelets. [25] If opioids are indicated, we recommend tramadol as an initial intervention, with appropriate precautions taken, particularly related to potential drug-drug interactions (e.g., serotonin syndrome when combined with other serotonergic medications), sedation, and fall risk. Opioids of increasing strength may be necessary to facilitate therapeutic interventions, though patient education on the risks, benefits, and expectations is critical and should be used with caution.
When pharmacological management is insufficient to permit return to activity or participation in an active physical therapy program, additional pain generators should be addressed (e.g., greater trochanteric bursitis), and interventional management may be considered. In a recent systematic review of the literature, it was concluded that it is unclear whether image-guided intra-articular diagnostic injections of local anesthetic predict positive responses to therapeutic injections. [26] The same systematic review revealed moderate quality of evidence of the effectiveness of therapeutic SIJ injection. Because of the low intra-articular placement of blind SIJ injections [27], fluoroscopic guidance is recommended. Pain can originate from the ligamentous structures of the sacroiliac complex in addition to the intra-articular structure. Sacral lateral branch thermal radiofrequency ablation has been evaluated for treatment of pain originating from the posterior elements of the sacroiliac complex. While the literature is limited, some evidence of moderate quality exists to support the use of sacral lateral branch thermal radiofrequency ablation when other treatments have been ineffective, though the specific indications for this procedure remain unclear. [7] Interdisciplinary pain rehabilitation programs, where available, may also be a viable option for patients in whom insufficient improvement has been achieved.
Resolution of Case
Following the reduction in pain and improvement in functional activities with physical therapy, the patient began an introductory yoga program to further strengthen her core. She reported ability to walk for longer distances and sleep was improved. She was independent in her activities of daily living and instrumental activities of daily living, and her improvements remained at 6 months.
Key Points
Physical examination of all older adults with CLBP should include examination of other potential pain generators, including sacroiliac joint provocative tests.
While x-rays can be used to determine the extent of SI joint involvement with systemic diseases such as ankylosing spondylitis, imaging should not be routinely used for evaluation of patients with SI joint symptoms.
Management begins with identifying and treating contributing factors, physical therapy and a home exercise program to address underlying weakness, and pharmacological intervention when needed to facilitate activity.Pharmacologic Recommendations
Topical treatments, acetaminophen, and salsalate, in that order, should comprise initial pharmacological pain management.
Non-cyclooxygenase-selective NSAIDs are included in Beers Criteria for Potentially Inappropriate Medication Use in Older Adults [ 25 ]. They are not recommended for chronic use in these patients.
When opioids are indicated, patient education on the risks and benefits must be thorough.
Interventional management may be necessary and should be used to facilitate physical therapy when feasible.
Conclusion
When seeing patients presenting with CLBP, the SI joint should be considered during any comprehensive evaluation. While pain may be correctly identified as originating from the SI joint, there can be a variety of contributing factors, which should be identified and addressed. This patient suffered from chronic lower extremity pain that caused a gait deformity leading to added stress and physical imbalances, contributing to SIJ symptoms. Treatment focuses on increased movement and, therefore, interventions to address physical deficits are paramount. Pharmacological interventions should target pain control to allow increased mobility and interventional management may be necessary. The algorithm described here can guide those steps, and prevent misdiagnosis and unnecessary procedures with associated potential morbidity.
Acknowledgments
Thanks to William George of the VA Pittsburgh for creating the photographs that accompany this article. The authors wish to thank Dave Newman for his valuable assistance in coordinating this project.
References:
Vleeming A Schuenke MD Masi AT , et al. . The sacroiliac joint: An overview of its anatomy, function and potential clinical implications . J Anatomy 2012 ; 221 ( 6 ): 537 67 .
Fortin JD Dwyer AP West S Pier J. Sacroiliac joint: Pain referral maps upon applying a new injection/arthrography technique. Part I: Asymptomatic volunteers . Spine 1994 ; 19 ( 13 ): 1475 82 .
Fortin JD Aprill CN Ponthieux B Pier J. Sacroiliac joint: Pain referral maps upon applying a new injection/arthrography technique. Part II: Clinical evaluation . Spine 1994 ; 19 ( 13 ): 1483 9 .
Kirkaldy-Willis WHHR. A more precise diagnosis for low-back pain . Scand J Rheumatol 1979 ; 4 ( 2 ): 102 9 .
Bernard TNK-WW. Recognizing specific characteristics of nonspecific low back pain . Spine 1987 ;Apr(217): 266 80 .
Slipman C Jackson H Lipetz J , et al. . Sacroiliac joint pain referral zones . Spine 2000 ; 81 ( 3 ): 334 8 .
King W Ahmed SU Baisden J , et al. . Diagnosis and treatment of posterior sacroiliac complex pain: A systematic review with comprehensive analysis of the published data . Pain Med 2015 ; 16 ( 2 ): 257 65 .
Braun J Sieper J Bollow M. Imaging of sacroiliitis . Clin Rheumatol 2000 ; 19 ( 1 ): 51 7 .
Feldtkeller E Khan MA van der Heijde D van der Linden S Braun J. Age at disease onset and diagnosis delay in HLA-B27 negative vs. positive patients with ankylosing spondylitis . Rheumatol Int 2003 ; 23 ( 2 ): 61 6 .
Weiner DK.
Deconstructing Chronic Low Back Pain in the Older Adult -
Shifting the Paradigm from the Spine to the Person
Pain Med 2015; 16 (5): 881885Weiner DK Fang M Gentili A , et al.
Deconstructing Chronic Low Back Pain in the Older Adult - Step by Step
Evidence and Expert-Based Recommendations for Evaluation and Treatment.
Part I: Hip osteoarthritis
Pain Med 2015; 16 (5): 886897Hicks GE Morone N Weiner DK. Degenerative lumbar disc and facet disease in older adults: Prevalence and clinical correlates . Spine 2009 ; 34 ( 12 ): 1301 6 .
Jarvik JJ Hollingworth W Heagerty P Haynor DR Deyo RA. The longitudinal assessment of imaging and disability of the back (LAIDBack) study: Baseline data . Spine 2001 ; 26 ( 10 ): 1158 66 .
Majlesi J Togay H Unalan H. ST , The sensitivity and specificity of the slump and the straight leg raising tests in patients with lumbar disc herniation . J Clin Rheum 2008 ; 14 ( 2 ): 87 91 .
Ege Rasmussen KJ Fano N. Trochanteric bursitis. Treatment by corticosteroid injection . Scand J Rheumatol 1985 ; 14 ( 4 ): 417 20 .
van der Wurff P Buijs EJ Groen GJ. A multitest regimen of pain provocation tests as an aid to reduce unnecessary minimally invasive sacroiliac joint procedures . Arch Phys Med Rehabil 2006 ; 87 ( 1 ): 10 4 .
Laslett M Aprill CN McDonald B Young SB. Diagnosis of sacroiliac joint pain: Validity of individual provocation tests and composites of tests . Man Ther 2005 ; 10 ( 3 ): 207 18 .
Szadek KM van der Wurff P van Tulder MW Zuurmond WW Perez RS. Diagnostic validity of criteria for sacroiliac joint pain: A systematic review . J Pain 2009 ; 10 ( 4 ): 354 68 .
Sled E Khoja L Deluzio K Olney S Culham E. Effect of a home program of hip abductor exercises on knee joint loading, strength, function, and pain in people with knee osteoarthritis: A clinical trial . Cochrane Database Syst Rev 2010 ; 90 ( 6 ): 895 904 .
Howe T Rochester L Neil F Skelton D Ballinger C. Exercise for improving balance in older people . Pain Med 2011 ;( 11 ): Cd004963.
Hadjistavropoulos T. Self-management of pain in older persons: Helping people help themselves . Pain Med 2012 ; 13 (suppl 2) : S67 71 .
Du S Yuan C Xiao X , et al. . Self-management programs for chronic musculoskeletal pain conditions: A systematic review and meta-analysis . Patient Educ Couns 2011 ; 85 ( 3 ): e299 310 .
Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole MR.
Clinical Importance of Changes in Chronic Pain Intensity
Measured on an 11-point Numerical Pain Rating Scale
Pain 2001 (Nov); 94 (2): 149-158Hammer N Mobius R Schloefenbaum S , et al. . Pelvic belt effects on health outcomes and functional parameters of patients with sacroiliac joint pain . PLoS One 2015 ; 10 ( 8 ): e0136375.
American Geriatrics Scoeity 2015 Beers Criteria Update Expert Panel. American geriatrics society 2015 updated beers criteria for potentially inappropriate medication use in older adults . J Am Geriatrics Soc 2015 ; 63 ( 11 ): 2227 46 .
Kennedy DJ Engel A Kreiner DS , et al. . Fluoroscopically guided diagnostic and therapeutic intra-articular sacroiliac joint injections: A systematic review . Pain Med 2015 ; 16 ( 8 ): 1500 18 .
Hansen HC. Is fluoroscopy necessary for sacroiliac joint injections? Pain Phys 2003 ; 6 ( 2 ): 155 8 .
Weiner DK Sakamoto S Perera S Breuer P. Chronic low back pain in older adults: Prevalence, reliability, and validity of physical examination findings . J Am Geriatr Soc 2006 ; 54 ( 1 ): 11 20 .
Cohen SP Chen Y Neufeld NJ. Sacroiliac joint pain: A comprehensive review of epidemiology, diagnosis and treatment . Expert Rev Neurother 2013 ; 13 ( 1 ): 99 116 .
Cohen SP Strassels SA Kurihara C , et al. . Outcome predictors for sacroiliac joint (lateral branch) radiofrequency denervation . Reg Anesth Pain Med 2009 ; 34 ( 3 ): 206 14 .
Patel N Gross A Brown L Gekht G. A randomized, placebo-controlled study to assess the efficacy of lateral branch neurotomy for chronic sacroiliac joint pain . Pain Med 2012 ; 13 ( 3 ): 383 98 .
Cheng J Pope JE Dalton JE Cheng O Bensitel A. Comparative outcomes of cooled versus traditional radiofrequency ablation of the lateral branches for sacroiliac joint pain . Clin J Pain 2013 ; 29 ( 2 ): 132 7 .

Return to LOW BACK PAIN
Since 8-30-2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |