

Model Simulations Challenge Reductionist Research Approaches
to Studying Chronic Low Back PainThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Orthop Sports Phys Ther. 2019 (Jun); 49 (6): 477–481 ~ FULL TEXT
OPEN ACCESS Jacek Cholewicki, PhD, Pramod K. Pathak, PhD, N. Peter Reeves, PhD, John M. Popovich, Jr., PT, DPT, ATC, PhD
Center for Orthopedic Research,
Michigan State University,
Lansing, MI.
BACKGROUND: Traditionally, low back pain (LBP) is studied using a reductionist approach, in which the factors contributing to the clinical presentation of LBP are studied in isolation to identify the primary pathology or condition linked to LBP. We argue that reductionism may not be suitable for studying LBP, considering the complex, multifactorial nature of this condition.
OBJECTIVES: To quantify the likelihood of successfully subclassifying patients with LBP and effectively targeting treatment based on a single dominant factor contributing to LBP.
METHODS: Both analytical and numerical simulations (Monte Carlo) of 1 million patients with LBP were performed. Several factors contributing to LBP were randomly assigned to each individual. The following outcome measures were computed, as a function of the number of factors: the percentage of individuals who could be subclassified by identifying a single factor exceeding a certain threshold, and the average reduction in LBP when treatment eliminates the largest contributing factor versus a multimodal treatment that eliminates a number of the randomly selected factors.
RESULTS: With an increasing number of factors, the probability of subclassifying an individual to a subgroup based on a single factor tends toward zero. A multimodal treatment arbitrarily addressing any 2 or more factors was more effective than diagnosing and treating a single factor that maximally contributed to LBP.
CONCLUSION: Results suggest that reductionism is not appropriate for subclassifying patients with LBP or for targeting treatment. The use of reductionist approaches may explain some of the challenges when creating LBP classification systems and designing effective treatment interventions. J Orthop Sports Phys Ther 2019;49(6):477-481. Epub 15 May 2019. doi:10.2519/jospt.2019.8791.
KEYWORDS: Monte Carlo simulation; classification; randomized clinical trials; risk factors; subgrouping
From the FULL TEXT Article:
Background
Lw back pain (LBP) is a multifactorial problem associated with many biological, psychological, and social factors. [8, 21, 28, 30] In most cases, the exact causes underlying LBP are unknown; hence, the term nonspecific LBP is often used. This nonspecificity makes selecting the appropriate treatment challenging for clinicians. Therefore, much of the current research efforts are directed toward identifying specific causal factors underlying the clinical presentation of LBP or toward subclassifying patients with specific characteristics (a collection of factors that determine the nature of an individual’s LBP) to formulate the appropriate intervention strategies addressing these specific factors (hereafter referred to as “factors contributing to LBP”). This approach is based on the rationale that when more is known about the etiology of LBP, the treatment can be more specific in addressing the factors contributing to LBP and result in better outcomes. Subsequently, randomized clinical trials (RCTs) are conducted to evaluate whether such matching between factors contributing to LBP and treatment leads to improved outcomes compared to other treatments, standard care, or sham treatment.
The above-outlined strategy in LBP research is termed a reductionist approach in the parlance of systems science. [1] In the reductionist approach, the system is broken down into smaller parts to isolate and study them comprehensively. The reductionist approach is well suited for containable diseases, such as local infection. However, reductionism is less helpful when the problem is multifactorial and where interactions between biological subsystems exist. [1] These features make the behavior of a complex system difficult to predict, even when the behavior of its parts is well defined. [1] For example, studying motor control in patients with LBP is a reductionist approach that evaluates the pathomechanics of neuromuscular control in isolation from other biological, psychological, and social factors to identify the primary pathology or condition linked to LBP. A natural extension of this approach is the development of intervention strategies attempting to correct those pathomechanics. [27]
Reductionism is not inherently wrong, as it allows for the identification of parts of the system (eg, factors associated with LBP) and has been useful for establishing factors associated with patient presentations (phenotypes), an important part of patient care. The problem lies in the assumption that information about individual parts is sufficient to explain the behavior of the entire system. In the example of studying motor control using a reductionist approach, the assumption is that other biological, psychological, and social factors have minimal or no influence on motor control. Perhaps in some patients this may be the case, but the evidence suggests that motor control interventions are not superior to other interventions in the management of patients with LBP, [27] which raises questions about other factors and interactions involved.
In contrast to reductionism, a systems approach takes the entire system into consideration when describing its behavior and identifying interdependence between its subsystems. [1] Attempts toward such an approach have been made with conceptual, structural equation, or collaborative modeling to account for a number of factors contributing to LBP simultaneously. [5, 6, 9, 18, 25] Yet, research in LBP lags substantially behind systems biology, which rapidly progressed in recent years with its effective application of systems science. [4, 14] There is a critical lack of knowledge regarding the number of factors and their interactions needed to adequately represent LBP, which in turn, limits the ability to target them through treatment modalities. As spine research evolves, the trend points toward more complexity, with more subsystems and their interactions requiring consideration. [6, 11]
There have been more than 1000 RCTs published evaluating various interventions for LBP, such as manual therapy, massage, acupuncture, dry needling, physical therapy, and specific exercise.15 Unfortunately, this literature collectively shows low to moderate effects and practically no differences between various interventions.3 More importantly, to date, “no classification system is supported by sufficient evidence to recommend implementation into clinical practice.” [2, 7, 13] Even a triage based on various clinical prediction rules has not led to better outcomes. [13] One possible explanation for the lack of success in documenting large positive treatment outcomes could be the reductionist approach, typically applied in LBP research, whereby unimodal intervention strategies targeting the dominant factor believed to be contributing to LBP are compared and studied in RCTs. While this approach has its place in research, considering the extreme biological complexity of the spine system, the multifactorial nature of LBP, and interactions among these factors, [21, 30] an approach that addresses these issues simultaneously is needed to advance LBP research and the development of more effective intervention strategies.
The goal of this study was to highlight the challenges of studying a complex condition using reductionist approaches. Specifically, using analytical and numerical simulations, we quantified the likelihood of correctly identifying the dominant factor contributing to LBP and of effectively treating LBP by modifying such a dominant factor. The following 2 hypotheses were tested:(1) when dealing with a large number of factors contributing to LBP, it is not possible to identify subgroups effectively based on the dominant factor; and
(2) on a population scale, providing a number of treatments targeting any 2 or more factors is more effective than identifying and treating a single factor that maximally contributes to LBP.If these hypotheses are true, perhaps a different research method, based on a systems approach,1 could lead to the development of more effective intervention strategies for LBP.
Methods
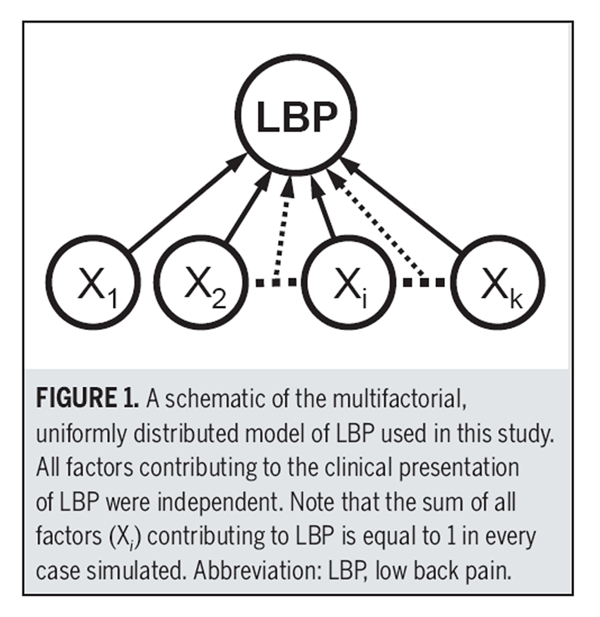
Figure 1 We performed both analytical and numerical simulations (Monte Carlo) of a large population (n = 1 million) with LBP. Factors contributing to LBP for each individual were uniformly distributed random variates (U1, U2, U3, ... Uk) between 0 and 1. For each individual, each factor Ui was normalized by dividing it by the sum of k factors to create a fraction contribution to LBP; ie, the total pain/disability effect of 1 is: (X1 + X2 + … + Xk) = 1 (Figure 1). For example, for 3 factors (k = 3), a person with LBP may have normalized factors such as X1 = 0.3, X2 = 0.1, and X3 = 0.6. This means that factor X1 contributes 30%, factor X2 contributes 10%, and factor X3 contributes 60% to the overall presentation of LBP, totaling 100%.
To test the 2 hypotheses, we calculated(1) the percentage of individuals who could be subclassified by identifying a single normalized factor (Xi) exceeding a certain threshold θ (where θ = 0.2, 0.3, 0.4), and
(2) the average reduction in pain/disability when the largest factor contributing to LBP is identified and eliminated with the targeted unimodal treatment, versus a number of treatments (multimodal treatment) eliminating a number of randomly selected factors.The analytical derivation and calculation of the hypothesized values are presented in the APPENDIX (available at www.jospt.org). To validate these analytical calculations, a numerical model simulation (Monte Carlo) was performed twice (macro feature in Excel 2010; Microsoft Corporation, Redmond, WA) by seeding an array with 1 million random variables between 0 and 1 and calculating the values derived analytically.
Results
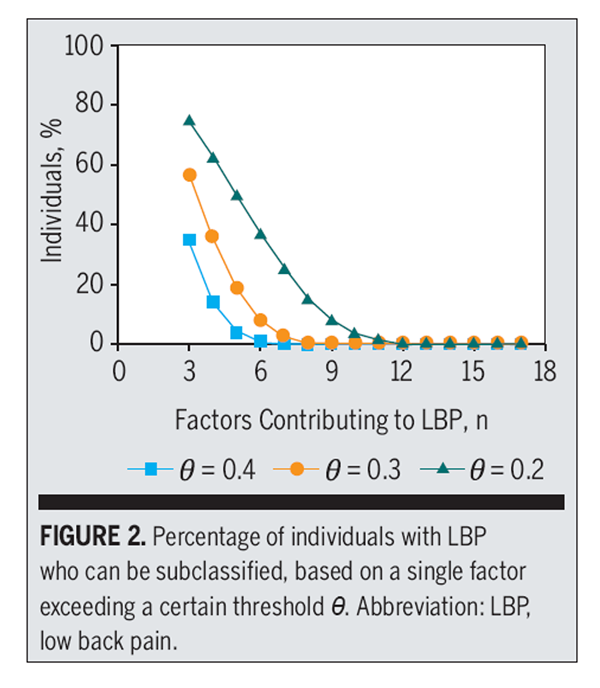
Figure 2

Figure 3 The maximum differences between any analytically derived values and the 2 simulation results were 5.28 × 10–4 and 4.75 × 10–4. These small differences indicate excellent agreement between the 2 methods, validating the analytical approach.
With an increasing number of factors, the probability of a single factor exceeding a certain threshold (Xi>θ) tends toward zero (Figure 2). In our model, this result represents the diminishing likelihood of classifying an individual to a subgroup of patients with LBP based on a single factor reaching some set threshold of contribution to the overall LBP (Figure 2). Even with a low threshold of θ = 0.2 (accounting for 20% of LBP symptoms), less than 1% of the LBP population can be subclassified when the number of factors exceeds 11.
On average, in a multifactorial model, the sum of any 2 or more factors is greater than the largest factor identified in each individual (Figure 3). This simulation result illustrates that a multimodal intervention addressing any 2 or more factors will likely be more effective in the population of patients with LBP than diagnosing and treating a single dominant factor that maximally contributes to LBP in each individual.
Discussion
The results from our analytical and numerical simulations of a multifactorial presentation of LBP are consistent with the data reported in the literature. With respect to the first hypothesis, our results show that with an increasing number of factors contributing to LBP, there is a diminishing likelihood of classifying an individual to a subgroup of patients based on the dominant factor. This could explain why attempts to identify subgroups of patients who would respond more favorably to a particular treatment have not yet been successful or reproduced. [2, 7, 13, 22, 23] Our simulations suggest that such a result would be expected if LBP were a large multifactorial problem. Reductionist research approaches, focusing at most on a few dominant factors contributing to LBP, are not able to address the entire complexity of this condition or document meaningful impact of interventions targeting those dominant factors. This scenario can be further complicated if many different mechanisms and factors interact and overlap, rendering the presence of pure subgroups rare. [16]
Based on the number of existing baseline predictors and the variance in outcomes they explain, Mistry et al [19] concluded that it is unlikely we can identify a single strong moderator of LBP treatment effects. None of the RCTs they reviewed were powered sufficiently to identify differential subgroup effects, and appropriately powered studies would be practically unrealistic. [19] To circumvent this problem, Patel et al [23] pooled data from 19 back pain trials that provided a data set of 9328 patients. Yet they, too, did not find any subgroups that would benefit from specific treatment, and, more importantly, they calculated that such an approach to identifying patients would not be cost-effective.
Our simulations are consistent with such findings. With only 12 factors contributing to LBP, only 0.5% of the LBP population could be subclassified based on a single factor and treated to achieve a minimal clinically important difference of a 20% reduction in pain [20] (θ = 0.2) (FIGURE 2). What if there were 21 factors,24 69 factors,8 or more6? Our simulation results indicate that this percentage would be 10–6 and 10–36 for 21 and 69 factors, respectively. Even if such an RCT could be conducted, it would likely have little clinical relevance.
With respect to the second hypothesis, it appears that multidisciplinary (ie, multimodal) rehabilitation strategies consistently show better results when compared to any single approach. [12] Likewise, our simulations suggest that when dealing with a multifactorial problem, it is more effective to treat several factors than to try to diagnose and treat the single dominant factor that contributes the most to LBP in each individual. Perhaps future research efforts should focus on designing effective multimodal, integrative, and adaptive approaches to the management of LBP. [17] As the management of patients with LBP continues to progress toward personalized medicine, multimodal treatment sequence, timing, and interaction effects will need to be considered.
There are, however, instances in the literature where the combination of 2 treatment approaches (eg, physical therapy and cognitive behavioral therapy [29]) was not superior to a unimodal treatment (physical therapy). One possibility in this example is that a single treatment modality (physical therapy) affected several factors contributing to LBP, [31] including those targeted by the cognitive behavioral therapy. In our model, such a situation could be simulated by a comparison of a single treatment targeting several factors contributing to LBP versus the same number of unimodal treatments targeting a single factor. Both interventions would show the same effectiveness in such a comparison. Alternatively, in the above example, the psychological factors targeted by cognitive behavioral therapy might not have been important factors contributing to LBP in these patients.
Several assumptions determine the behavior of this model simulation. The assumption having probably the biggest effect on the results was that various factors contributing to LBP are uniformly distributed across the population with LBP. That is, all factors have the same probability of being present in each individual, and there is no factor occurring more frequently in the LBP population. If some factors were occurring more frequently, it would have been easier to identify a cluster of patients with these factors. We submit, however, that in reality the distribution of factors contributing to LBP might be closer to uniform, because the studies thus far have failed to identify a dominant modifiable factor or subgroup of patients with LBP. [13] The simulated treatments were unrealistic because they completely eliminated the targeted factors contributing to LBP in every case. Most likely, the real treatment effects would have been much smaller, because interventions for LBP are not 100% effective, and not all individuals respond to them.
Another assumption that impacted the model results was that the model was unstructured (Figure 1). Such a model assumes that each factor is independent and directly linked to LBP, which is unlikely to be the case. However, we purposefully chose such a model, given that it represents the common factorial analyses used in LBP research. The addition of interactions between the factors, which could represent serial, parallel, and feedback connections, would make the model more complex, strengthening the argument that reductionist approaches are not appropriate to study the complex phenomena represented by such a model.
Conclusion
Research to identify the factors, or group of factors, that contribute to LBP and to understand the efficacy of individual treatment interventions is necessary but not sufficient to address the LBP problem effectively. As demonstrated by our unstructured multifactorial model of LBP, simply identifying components within the model and not the structure of the model (ie, the interactions between these components) is not likely to lead to robust classification or better treatment effects.
To advance LBP research, more sophisticated modeling methods that consider the structure of the system being studied [9, 18] and possibly the dynamics of the system[1] (LBP symptoms and treatment effects are not static and change with time) are needed. Future research should involve a paradigm shift toward a systems approach, which allows for integration of knowledge in a more systematic and effective way. [26] A systems approach has been specifically developed to address complexity and successfully implemented in engineering. Such an approach appears to be well suited for studying medical conditions that are multifactorial in nature. [1]
Key Points
FINDINGS: With an increasing number of factors contributing to low back pain (LBP), the probability of finding subgroups of patients, based on a single factor exceeding a certain threshold, tends toward zero. Arbitrarily applying treatments addressing any 2 or more factors was more effective in the simulated population of patients with LBP than diagnosing and treating a single factor that maximally contributed to LBP in each individual.
IMPLICATIONS: A reductionist approach aimed at identifying 1 or a few dominant factors contributing to LBP, or subclassifying patients based on those factors, will likely not result in the discovery of strong modifiers of treatment effects. The simulations suggest that multimodal management of LBP will likely be more effective than unimodal treatment.
CAUTION: The main assumptions influencing the specific numerical results were that factors contributing to LBP were uniformly distributed and that there were no interactions among them. While these assumptions affect the complexity of the modeled LBP problem, the simulation trends will likely hold for more complex models.
ACKNOWLEDGMENTS:
The forum on which this body of research was based, “State-of-the-Art in Motor Control and Low Back Pain: International Clinical and Research Expert Forum,” was supported by the National Health and Medical Research Council of Australia, in collaboration with the North American Spine Society. The forum was chaired by Dr Paul Hodges.
References:
Ahn AC, Tewari M, Poon CS, Phillips RS.
The limits of reductionism in medicine: could systems biology offer an alternative?
PLoS Med. 2006;3:e208.
https://doi.org/10.1371/journal.pmed.0030208Apeldoorn AT, Ostelo RW, van Helvoirt H, et al.
A randomized controlled trial on the effectiveness of a classification-based system for subacute and chronic low back pain.
Spine (Phila Pa 1976). 2012;37:1347-1356.
https://doi.org/10.1097/BRS.0b013e31824d9f2bArtus M, van der Windt DA, Jordan KP, Hay EM.
Low back pain symptoms show a similar pattern of improvement following a wide range of primary care treatments:
a systematic review of randomized clinical trials.
Rheumatology (Oxford). 2010;49:2346-2356. https://doi.org/10.1093/rheumatology/keq245Bose B.
Systems biology: a biologist’s viewpoint.
Prog Biophys Mol Biol. 2013;113:358-368.
https://doi.org/10.1016/j.pbiomolbio.2013.07.001Buchbinder R, Batterham R, Elsworth G, Dionne CE, Irvin E, Osborne RH.
A validity-driven approach to the understanding of the personal and societal burden of low back pain:
development of a conceptual and measurement model.
Arthritis Res Ther. 2011;13:R152. https://doi.org/10.1186/ar3468Cholewicki J, Popovich JM, Jr., Aminpour P, Gray SA, Lee AS, Hodges PW.
Development of a collaborative model of low back pain: report from the 2017 NASS consensus meeting.
Spine J. In press.
https://doi.org/10.1016/j.spinee.2018.11.014R.A. Deyo, S.F. Dworkin, D. Amtmann, G. Andersson, et al.,
Report of the NIH Task Force on Research Standards for Chronic Low Back Pain
Journal of Pain 2014 (Jun); 15 (6): 569–585Dolphens M, Vansteelandt S, Cagnie B, et al.
Multivariable modeling of factors associated with spinal pain in young adolescence.
Eur Spine J. 2016;25:2809-2821. https://doi.org/10.1007/s00586-016-4629-7Fritz JM, Koppenhaver SL, Kawchuk GN, Teyhen DS, Hebert JJ, Childs JD.
Preliminary investigation of the mechanisms underlying the effects of manipulation:
exploration of a multivariate model including spinal stiffness, multifidus recruitment, and clinical findings.
Spine (Phila Pa 1976). 2011;36:1772-1781.
https://doi.org/10.1097/BRS.0b013e318216337dHall P.
The distribution of means for samples of size N drawn from a population in which the variate takes values between 0 and 1, all such values being equally probable.
Biometrika. 1927;19:240-245.
https://doi.org/10.1093/biomet/19.3-4.240Hodges PW.
Adaptation and rehabilitation: from motoneurons to motor cortex and bahaviour.
In: Hodges PW, Cholewicki J, van Dieën JH, eds.
Spinal Control: The Rehabilitation of Back Pain. State of the Art and Science.
Edinburgh, UK: Elsevier/Churchill Livingstone; 2013: ch 6.Kamper SJ, Apeldoorn AT, Chiarotto A, et al.
Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis.
BMJ. 2015;350:h444.
https://doi.org/10.1136/bmj.h444Kamper SJ, Maher CG, Hancock MJ, Koes BW, Croft PR, Hay E.
Treatment-based subgroups of low back pain: a guide to appraisal of research studies and a summary of current evidence.
Best Pract Res Clin Rheumatol. 2010;24:181-191.
https://doi.org/10.1016/j.berh.2009.11.003Kesi? S.
Systems biology, emergence and antireductionism.
Saudi J Biol Sci. 2016;23:584-591.
https://doi.org/10.1016/j.sjbs.2015.06.015Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C.
An Updated Overview of Clinical Guidelines for the Management of Non-specific Low Back Pain
in Primary Care
European Spine Journal 2010 (Dec); 19 (12): 2075–2094Lemeunier N, Leboeuf-Yde C, Gagey O, Wedderkopp N, Kjaer P.
Do number of days with low back pain and patterns of episodes of pain have similar outcomes in a biopsychosocial prediction model?
Eur Spine J. 2016;25:2774-2787. https://doi.org/10.1007/s00586-016-4531-3Maiers MJ, Westrom KK, Legendre CG, Bronfort G.
Integrative Care for the Management of Low Back Pain: Use of a Clinical Care Pathway
BMC Health Serv Res. 2010 (Oct 29); 10: 298Melton BL, Moqbel M, Kanaan S, Sharma NK.
Structural equation model of disability in low back pain.
Spine (Phila Pa 1976). 2016;41:1621-1627.
https://doi.org/10.1097/BRS.0000000000001563Mistry D, Patel S, Hee SW, Stallard N, Underwood M.
Evaluating the quality of subgroup analyses in randomized controlled trials of therapist-delivered interventions for nonspecific low back pain: a systematic review.
Spine (Phila Pa 1976). 2014;39:618-629.
https://doi.org/10.1097/BRS.0000000000000231Ostelo RW, Deyo RA, Stratford P, et al.
Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change.
Spine (Phila Pa 1976). 2008;33:90-94.
https://doi.org/10.1097/BRS.0b013e31815e3a10O’Sullivan P, Caneiro JP, O’Keeffe M, O’Sullivan K.
Unraveling the complexity of low back pain.
J Orthop Sports Phys Ther. 2016;46:932-937.
https://doi.org/10.2519/jospt.2016.0609Patel S, Friede T, Froud R, Evans DW, Underwood M.
Systematic review of randomized controlled trials of clinical prediction rules for physical therapy in low back pain.
Spine (Phila Pa 1976). 2013;38:762-769.
https://doi.org/10.1097/BRS.0b013e31827b158fPatel S, Hee SW, Mistry D, et al.
Identifying Back Pain Subgroups: Developing and Applying Approaches Using Individual Patient Data Collected Within Clinical Trials.
Southampton, UK: National Institute for Health Research; 2016.Pincus T, Santos R, Breen A, Burton AK, Underwood M.
A review and proposal for a core set of factors for prospective cohorts in low back pain: a consensus statement.
Arthritis Rheum. 2008;59:14-24.
https://doi.org/10.1002/art.23251Poitras S, Rossignol M, Dionne C, et al.
An interdisciplinary clinical practice model for the management of low-back pain in primary care: the CLIP project.
BMC Musculoskelet Disord. 2008;9:54.
https://doi.org/10.1186/1471-2474-9-54Reeves NP, Cholewicki J.
Spine systems science: a primer on the systems approach.
In: Hodges PW, Cholewicki J, van Dieën JH, eds.
Spinal Control: The Rehabilitation of Back Pain. State of the Art and Science.
Edinburgh, UK: Elsevier/Churchill Livingstone; 2013:7-16.Saragiotto BT, Maher CG, Yamato TP, et al.
Motor control exercise for chronic non-specific low-back pain.
Cochrane Database Syst Rev. 2016:CD012004.
https://doi.org/10.1002/14651858.CD012004Serbic D, Pincus T, Fife-Schaw C, Dawson H.
Diagnostic uncertainty, guilt, mood, and disability in back pain.
Health Psychol. 2016;35:50-59.
https://doi.org/10.1037/hea0000272Smeets RJ, Vlaeyen JW, Hidding A, et al.
Active rehabilitation for chronic low back pain: cognitive-behavioral, physical, or both? First direct post-treatment results from a randomized controlled trial [ISRCTN22714229].
BMC Musculoskelet Disord. 2006;7:5.
https://doi.org/10.1186/1471-2474-7-5Sullivan MJ.
Toward a biopsychomotor conceptualization of pain: implications for research and intervention.
Clin J Pain. 2008;24:281-290.
https://doi.org/10.1097/AJP.0b013e318164bb15van Middelkoop M, Rubinstein SM, Verhagen AP, et al.
Exercise Therapy for Chronic Nonspecific Low-back Pain
Best Pract Res Clin Rheumatol. 2010 (Apr); 24 (2): 193–204
Return to LOW BACK PAIN
Return to CLINICAL PREDICTION RULES
Since 1-23-2020


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |