

Pediatric Integrative Medicine This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Pediatrics. 2017 (Sep); 140 (3): e20171961 ~ FULL TEXT
OPEN ACCESS Hilary McClafferty, MD, FAAP, Sunita Vohra, MD, FAAP, Michelle Bailey, MD, FAAP, Melanie Brown, MD, MSE, FAAP, Anna Esparham, MD, FAAP, Dana Gerstbacher, MD, FAAP, Brenda Golianu, MD, FAAP, Anna-Kaisa Niemi, MD, PhD, FAAP, FACMG, Erica Sibinga, MD, FAAP, Joy Weydert, MD, FAAP, Ann Ming Yeh, MD
Hilary McClafferty, MD, FAAP.
University of Arizona College of Medicine – Tucson
1501 N. Campbell Avenue | PO Box 245017 |
Tucson, Arizona 85724
hmcclafferty@email.arizona.edu

The American Academy of Pediatrics is dedicated to optimizing the well-being of children and advancing family-centered health care. Related to this mission, the American Academy of Pediatrics recognizes the increasing use of complementary and integrative therapies for children and the subsequent need to provide reliable information and high-quality clinical resources to support pediatricians. This Clinical Report serves as an update to the original 2008 statement on complementary medicine. The range of complementary therapies is both extensive and diverse. Therefore, in-depth discussion of each therapy or product is beyond the scope of this report. Instead, our intentions are to define terms; describe epidemiology of use; outline common types of complementary therapies; review medicolegal, ethical, and research implications; review education and training for select providers of complementary therapies; provide educational resources; and suggest communication strategies for discussing complementary therapies with patients and families.
There are more articles like this @ our:
Chiropractic Pediatrics Section
From the Full-Text Article:
Introduction
The National Center for Complementary and Integrative Health (NCCIH) of the National Institutes of Health (NIH) [1] defines complementary therapies as evidence-based health care approaches developed outside of conventional Western medicine that are used in conjunction with conventional care. Examples of complementary care include the use of acupuncture to treat migraine headache [2] and clinical hypnosis to improve symptoms of irritable bowel syndrome (IBS). [3] The term integrative health describes the blending of complementary and conventional therapies by the practitioner to include all appropriate therapies in a patient-centered and evidence-informed fashion. In an integrative approach, evidence-based complementary therapies may be used as primary treatments or used in combination with conventional therapies. In contrast, alternative therapies are not evidence-based, are used in place of conventional care, and are not covered in this report.
Interest in the field of pediatric integrative medicine is driven by a number of factors, including the prevalence of use in children living with chronic illness, [4, 5] the desire to reduce frequency and duration of pediatric prescription medication use, and the need for more effective approaches to preventive health in children. [6, 7] To date, consumer interest in and use of complementary therapies has outpaced training options in pediatric integrative medicine, leaving pediatricians with a desire for more training and familiarity with resources. [8] For example, a 2012 survey of academic pediatric training programs revealed that only 16 of 143 programs reported having an integrative medicine program.8 National initiatives to introduce pediatric integrative medicine into conventional pediatric residency training include programs such as the Pediatric Integrative Medicine in Residency program through the University of Arizona, initiated in 2012. [9] Other teaching initiatives are underway through the American Academy of Pediatrics (AAP) Section on Integrative Medicine and through academic institutions affiliated with the Academic Consortium for Integrative Medicine and Health (ACIMH), a prestigious organization of more than 65 medical schools that offer integrative medicine research, education, and clinical initiatives (eg, Harvard, Yale, Duke, Stanford). [10] This Clinical Report serves as an update to the original 2008 statement on complementary medicine. [11]
Epidemiology
Overview
Results of the 2012 National Health Interview Survey (NHIS) revealed that the prevalence of children <18 years using complementary therapies remained approximately 12% in the preceding 5 years, [12] reflecting the fact that more than 1 in every 10 children had used some form of complementary therapy in the preceding year. In both the 2007 and 2012 NHIS, complementary approaches were used most often for back or neck pain, head or chest cold, other musculoskeletal conditions, anxiety or stress, and attention-deficit/hyperactivity disorder (ADHD) and were more often chosen to treat a specific condition rather than to promote general well-being. [12] Nonvitamin, nonmineral dietary supplements (eg, herbal medicines, probiotics), osteopathic or chiropractic manipulation, and yoga, tai chi, or qigong were the complementary therapies used most frequently by children in both the 2007 and 2012 NHIS. [12] Zhang et al [13] conducted a study in which they used data from the Food and Drug Administration (FDA) and Infant Practices Feeding Study II of the Centers for Disease Control and Prevention, and they showed that 9% of infants, including newborn infants, received dietary botanical supplements or teas in the first year of life.
Use in Chronic Illness
The use of complementary therapies increases to >50% in children living with chronic illness, [6, 12, 14–18] with the most common category of complementary therapy being natural health products. [12] Children with multiple chronic conditions or greater functional disability from their chronic illness were more likely to use complementary therapies. [5, 14, 19, 20] Data from the National Comorbidity Survey Replication Adolescent Supplement revealed that for youth with any psychiatric disorder, 5.3% received mental health services in a complementary medicine setting within the past 12 months. [21]
In a study of 926 children attending 10 Canadian pediatric outpatient specialty clinics (cardiology, gastroenterology, neurology, oncology, and respiratory), Adams et al [4] showed that the prevalence of pediatric complementary therapy use reached up to 70%. Prevalence increased in older age groups and with severity of illness. [4] The top conditions for which children used complementary therapies included various heart disorders, Crohn disease, colitis, celiac disease, epilepsy, headache, migraine, cerebral palsy, leukemia, asthma, cystic fibrosis, and other respiratory disorders. The most common complementary treatments used by this study population included vitamins and minerals, massage, and homeopathic treatments. [4]
Use in Adolescents
Both the 2007 and 2012 NHIS results revealed that adolescents (ages 12–17 years) were more likely to use complementary therapies than younger children (ages 4–11 years). [12] In numerous reports, researchers have described the frequent use of complementary therapies by adolescents, [22–26] including those living with chronic illnesses such as IBS, juvenile idiopathic arthritis, [27, 28] and a range of mental health conditions. [21]
Adolescents use supplements to lose weight, increase energy, and improve their body image or athletic performance, among other reasons. Commonly used dietary supplements in this age group include ginseng, zinc, echinacea, ginkgo, weight loss supplements, and creatine. [29] The primary influences for use of complementary therapies among adolescents include their use by a family member and targeted marketing and advertising on television and the Internet. [30]
High Prevalence of Use, High Out-of-Pocket Costs
The 2012 NHIS showed that the prevalence of adult complementary medicine use in the preceding year remained steady at 33.2%, (approximately 1 in 3) compared with 35.5% in the 2007 survey. [18] This accounts for an estimated 354 million visits to complementary medicine practitioners and an estimated 835 million individual purchases of products, classes, and materials. According to the 2012 NHIS, an estimated 59 million adults spent $30.2 billion out of pocket (with $1.9 billion spent on children) for complementary medicine practitioners and purchases of complementary medicine products, classes, and materials in the preceding year, an estimated 1.1% of total health care costs in the United States and up to 9.2% of out-of-pocket health care expenditures in 2012. [31]
Predictors of Complementary Medicine Use and Low Disclosure Rates
Parental use of complementary medicine remains one of the most consistent predictors of complementary medicine use in children. [12] Other important predictors of complementary medicine use in children include higher parental education, higher family income, living in the western United States, and higher number of physician visits in the preceding year. [6] Adults have been shown to be more likely to discuss use of complementary therapies for themselves and their children if their physician is perceived as having patient-centered communication and specifically inquires about use,32 reinforcing the key message of asking patients about all therapies in use to reduce of potential supplement-drug interactions and to promote greater trust between parent and physician. [8]
Patient Characteristics
The use of complementary therapies spans the socioeconomic spectrum and varies considerably among cultural and ethnic groups. [19, 20, 33] According to the 2012 NHIS, non-Hispanic African American and Hispanic children have the lowest use of complementary therapies in the United States. [12] Researchers in several studies have indicated that complementary medicine use among children may be underreported because certain ethnic populations are less likely to disclose the use of these practices to their providers. [34–36] This may be in part because many cultures do not see their indigenous practices as “complementary”; rather, they are viewed as traditional approaches to health and health care indigenous to their culture. Language barriers may result in underrepresentation of non-English speakers because many of the large population-based surveys are conducted only in English. [37] Reasons for the use of complementary medicine vary and include alignment with family or patient beliefs, fear of adverse drug effects, supporting conventional treatments, and desire to improve overall health. [11, 38] Data from the 2007 NHIS showed that patients who delayed conventional care because of financial constraints were also more likely to use complementary therapies. [39]
Physician Awareness, Attitude, and Perception
In the 2001 AAP Periodic Survey number 49, “Complementary and Alternative Therapies in Pediatric Practice,” most pediatricians (72.8%) agreed they should provide patients with information about all potential treatment options but reported they had little or no knowledge of complementary or alternative therapies. They recognized patients’ frequent use of these therapies and expressed a strong desire for additional education on topics, including herbs, dietary supplements, special diets, and exercise. [40] More than one-third of the pediatricians reported that they or their families personally used some type of complementary therapy. Of those reporting complementary therapy use, 70% used massage therapy, 21% received chiropractic care, 13.5% consulted a spiritual or religious healer, and 13% had used acupuncture. [41] In a 2005 report, the Institute of Medicine [42] stated that health care professionals needed to be informed about complementary therapies and to be knowledgeable enough to discuss them with their patients. It also advocated that conventional health care professional training programs (eg, schools of medicine, nursing, pharmacy, and allied health) should incorporate sufficient information about complementary therapies into their curricula to enable licensed health care professionals to competently advise their patients about the various options. [42] As of 2012, only 16 of the 143 academic pediatric programs surveyed in the United States reported having pediatric integrative medicine programs. [8] As of 2015, 50% of US medical school Web sites (n = 130) listed at least 1 course or clerkship offering in complementary and alternative medicine (CAM). [43] These offerings embraced a wide range of topics and instructional methods. Although the extent to which pediatric residencies and postgraduate courses address educational needs about complementary therapies is unknown, [44–47] there is a growing number of Web-based educational training resources in the area of pediatric integrative medicine, including the AAP Section on Integrative Medicine [48] and the Pediatric Complementary and Alternative Medicine Research and Education Network. [49] Since 2012, a growing number of academic pediatric integrative medicine programs have offered a complementary therapy curriculum to medical students and residents as part of their standard medical education. [9] In the United States, board certification in integrative medicine is now offered to eligible candidates through the American Board of Physician Specialties. [50]
To ensure consistent, quality education across the spectrum of medical education, learning competencies for physician education on integrative medicine therapies should be considered for medical school, residency, and continuing medical education activities.
NIH: NCCIH
The Office of Alternative Medicine was established as part of the NIH by congressional mandate in 1992. In 1998, the Office of Alternative Medicine became the National Center for Complementary and Alternative Medicine, and in 2014 the name was changed to the National Center for Complementary and Integrative Health. The NCCIH has increased its fiscal-year appropriations from $50 million in 1998 to an estimated $124 million in 2014 (~0.4% of the total NIH budget). [1] In the early years, NCCIH’s focus on research emphasized the importance of basic and clinical research as the core of building the evidence base for CAM.
In 2005, at the request of the NIH and the Agency for Healthcare Research and Quality, the Institute of Medicine (now known as the National Academy of Medicine) released the report “Complementary and Alternative Medicine in the United States.” The report assessed what is known about Americans’ reliance on complementary therapies and assisted the NIH in developing research methods and setting priorities for evaluating such products and therapies. It advocated that conventional medical treatments and complementary and alternative treatments be held to the same standards for demonstrating clinical effectiveness. [42]
The 2016 NCCIH strategic plan identified 5 core objectives and 6 top scientific priorities and they are as follows. [51]
Objectives
Advance fundamental science and methods development;
improve care for hard-to-manage symptoms;
foster health promotion and disease prevention;
enhance the complementary and integrative health research workforce; and
disseminate objective evidence-based information on complementary and integrative health interventions.
Top Scientific Priorities
Nonpharmacologic management of pain;
neurobiological effects and mechanisms;
innovative approaches for establishing biological signatures of natural products;
clinical trials utilizing innovative study designs to assess complementary health;
disease prevention and health promotion across the lifespan;
clinical trials utilizing innovative study designs to assess complementary health approaches and their integration into health care; and
communications strategies and tools to enhance scientific literacy and understanding of clinical research.
The NCCIH divides the various complementary therapies into 1 of 2 main subgroups: natural products or mind and body practices. Natural products include botanicals, vitamins and minerals, and probiotics as a group (also widely known as dietary supplements). Mind and body practices include acupuncture, relaxation techniques, tai chi, qigong, healing touch, hypnotherapy, and movement therapies. A third category, other complementary heath approaches, includes practices such as traditional Chinese medicine (TCM), Ayurvedic medicine, homeopathy, and naturopathy.
https://nccih.nih.gov/health/integrative-health#types
Research
Pediatric integrative medicine involves the integration of complementary and conventional therapies on the basis of the best available data, with the goal of maximizing therapeutic benefit to the patient. Ideally, an approach to the integration of complementary therapies into practice would depend on the same evidenced-based decision-making used for conventional therapies, with the understanding that in both instances, evidence available for particular therapies in specific clinical situations may be variable. That said, formal expert evaluation has suggested that the quality of randomized controlled trials (RCTs) of CAM is as good as that of RCTs of conventional medicine [53] and that the quality of systematic reviews of CAM exceeds that of conventional medicine. [53] In addition, publication bias in complementary medicine research is opposite that of conventional medicine; that is, negative studies are more likely to be published in well-known journals, and positive studies are more likely to be published in foreign language journals. [53]
There are some unique considerations when conducting research on the efficacy of complementary therapies, including underlying theories, which may seem quite disparate from the conventional model, and heterogeneity of both products and practices. Some complementary therapies have traditions that date back thousands of years, which generates evidence of an iterative, experiential type. In recognition of the variety and value of different types of evidence, research studies to measure the effect of such complementary therapies should be designed to test the therapy within the context of its tradition. Rigorous N-of-1 trials (clinical trials in which a single patient receives both experimental and control intervention) are particularly useful for the evaluation of individualized therapies used in CAM. One useful N-of-1 resource can be found through the Agency for Healthcare Research and Quality monograph. [54]
To be comprehensive, high-quality data about both safety and effectiveness are needed. Most current safety data consist of case reports identified through passive surveillance, with little known about the true denominator of the number of people receiving the treatment and considerable concern about underreporting of the numerator. Researchers in a number of reviews of provider-delivered therapies have found reassuring evidence regarding the safety of complementary therapies. [55, 56] Although the need for rigorous safety evaluation is questioned by some who perceive “natural” as equivalent to “safe,” to support patient-centered integration of therapies, more rigorous data on safety are needed. In addition, in contrast to pharmaceuticals, there are limited requirements to demonstrate safety before marketing natural products, resulting in little motivation for detailed safety work from the manufacturer standpoint. Although consumer interest in complementary therapies continues to increase, there remains an important unmet need to develop rigorous safety data to inform policy and practice.

Figure 1 Although there are numerous challenges inherent in all clinical research, these difficulties are compounded when performing research in children and on therapies based on different theoretical approaches to health and well-being. The use of rigorous scientific methods to study the use of complementary therapies from other healing traditions has been greatly encouraged and supported by the NCCIH. Although much progress has been made, there remain significant opportunities to expand the evidence base for the integration of complementary therapies in our care of children. A useful research resource includes a data query and research resource Web site developed by the Data Resource Center for Child and Adolescent Health (http://www.childhealthdata.org/learn/nhis) to facilitate access to the data on CAM from the 2007 and 2012 NHIS (Figure 1). [57]
One issue that must be considered in all research, both conventional and complementary, is the placebo effect, a sophisticated psychobiological event that operates on multiple levels of the therapeutic relationship. It has been shown to involve conditioning, learning, memory, motivation, reward, and patient expectancy on the basis of interactions with the clinician.
It has been established that the placebo effect is real and holds significant therapeutic potential, although many questions remain about how best to harness the complexity of its effect and about its role as a potential compounding factor in clinical research. The ethics of deliberate use of the placebo effect continue to be debated in the medical literature for both conventional and complementary practices. [58]
Regulation of Dietary Supplements
Concerns exist about the purity and potency of herbal products and other dietary supplements sold in the United States, in part because of regulations that differ from those governing the use of pharmaceuticals. The Dietary Supplements Health and Education Act (DSHEA) of 1994 [59] amended previous FDA statutes to encompass dietary supplement–specific provisions, including the definition of a “dietary supplement” as food and not a drug, product safety, nutritional statements and claims, ingredient and nutritional labeling, good manufacturing procedures, and the classification of “new” dietary ingredients.59 Under the DSHEA, a dietary supplement is the following [59]:
"a product (other than tobacco) intended to supplement the diet that bears or contains 1 or more
of the following ingredients: a vitamin, a mineral, an herb or other botanical, or an amino acid;intended for ingestion in pill, capsule, tablet, or liquid form;
not used as a conventional food or as the sole item of a meal or diet; and
labeled as a dietary supplement."
In contrast, dietary supplements in Canada are regulated through Health Canada’s Natural and Non-prescription Health Products Directorate, formerly known as the Natural Health Products Directorate. Products manufactured or distributed in Canada are required to have a product license by Health Canada, certifying premarket safety, efficacy, and quality. [60]
The FDA can demonstrate that a supplement is unsafe only after it reaches the market and must prove that the product is unsafe before it can restrict a product’s use or take other legal action. The FDA relies largely on the MedWatch voluntary reporting system to collect safety data on dietary supplements. [61]
The DSHEA also regulates third-party literature regarding dietary supplements. Informational materials (ie, articles, fact sheets) may be displayed in commercial retail sites provided they are displayed separately from the product, do not contain false or misleading information, and do not promote a specific brand of supplement. Quality and standardization of natural health products also significantly affect research, in which reproducibility of results is a critical factor.
Perhaps most importantly, the DSHEA regulates the labeling of dietary supplements. Under this provision, any claims to prevent, treat, or cure a specific disease are expressly prohibited (unless approved by the FDA). Labels can include statements describing the supplement’s effects on the “structure and function” or general “well-being” of the body as long as they are truthful and bear the statement, “This statement has not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.”59 Just as with food products, dietary supplements are allowed to have suggested dosages on the label and must bear nutritional labeling. The label must include the name and quantity of each dietary ingredient, and if the ingredient is botanical in origin, the label must state the part of the plant from which the ingredient is derived. [59] To maximize patient safety, all primary care providers should be knowledgeable about correct labeling of dietary supplements. [62, 63]
Licensing, Medicolegal, and Ethical Considerations
Uncertainty about the scope of practice, licensing requirements, and credentialing of complementary medicine providers are common concerns, as are concerns about patient safety and legal liability when recommending complementary therapies or therapists.
Licensing
Licensing information about health care professionals who are not doctors of medicine or doctors of osteopathic medicine is maintained by state licensing boards and shows significant state-to-state variation. As with physicians, regulations, licenses, or certificates do not guarantee safe, effective treatment from any provider. [64] Local and state governments and professional organizations generally establish the credentials that complementary health providers need to treat patients.
Chiropractic is licensed in all 50 states. [65] Acupuncture [66] and massage therapy are licensed in more than half of the states. [67] At the time of writing, 17 states, 5 Canadian provinces, the District of Columbia, and the US territories of Puerto Rico and the US Virgin Islands all have laws regulating naturopaths. [68] Only 3 states currently offer licensing to doctors of medicine and doctors of osteopathic medicine to practice homeopathy (Arizona, Nevada, and Connecticut). [69] It is essential for physicians to understand local and state statutes and regulations governing specific therapeutic modalities. [70, 71]
Medicolegal Considerations
If a complementary medicine practitioner is licensed, then he or she must also practice within his or her scope of practice as defined by local and state statutes and regulatory boards.Informed Consent As the evidence base grows and standard of care evolves, some complementary therapy modalities may need to be included in discussions about informed consent for treatment. The informed consent process may require a discussion about potential benefits and harms associated with complementary therapies, notwithstanding the ability of a patient to acquire complementary treatments without the involvement of the pediatrician. An example is the practice of inquiring about dietary supplement use and discussing its potential benefit and harms. Ideally, the primary care provider will inquire about any complementary medicine use at every patient visit. [35]
Life-threatening Conditions Pediatricians also need to be aware of alternative therapies that may be used as a substitute for conventional medical care for children with life-threatening conditions and decide whether they believe such treatment is reportable under state abuse and neglect laws. [72] Another legal duty of pediatricians relates to the assurance that seeking reimbursement for complementary therapy does not trigger a potential violation of fraud and abuse laws for therapy deemed “medically unnecessary.” Ultimately, it is prudent to be cautious about any representations or guarantees. In certain circumstances, charging patients directly for services may violate medical insurance or system contracts; therefore, individual primary care providers should apprise themselves of rules and regulations relevant to their specific practice model.Ethical Considerations
Uncertainty about how to translate principles of medical ethics into integrative medicine is another common area of confusion. Primary care providers should know that case law has placed a burden on them to discuss viable options of treatment although they may be unwilling to offer the therapy. [73]
The first guideline of ethical practice is to seek reliable, evidence-based information about the safety and effectiveness of specific therapies and therapists, although the specific ethical questions in clinical practice vary in different clinical situations. If a therapy is both safe and effective, the pediatrician is ethically required to discuss its use as he or she would for any other such therapy in conventional care. [74]
The 2001 AAP Policy Statement, “Counseling Families Who Choose Complementary and Alternative Medicine for Their Child With Chronic Illness or Disability,” was reaffirmed in 2010 and continues to recommend that pediatricians seek information, evaluate the scientific merits of specific therapeutic approaches, and identify risks or potential harmful effects. [75] Pediatricians may want to be familiar with the complementary medicine providers in their area so that they are able to advise patients on providers who are appropriately working within their scope of practice. [42] Similarly, pediatricians are encouraged to advise parents and patients about the importance of establishing the safety and quality of any product sold in a complementary medicine provider’s office or in any commercial venue.
A common-sense guide to balancing risks and benefits when making therapeutic decisions provides a framework for decision-making surrounding treatment recommendations. [76]
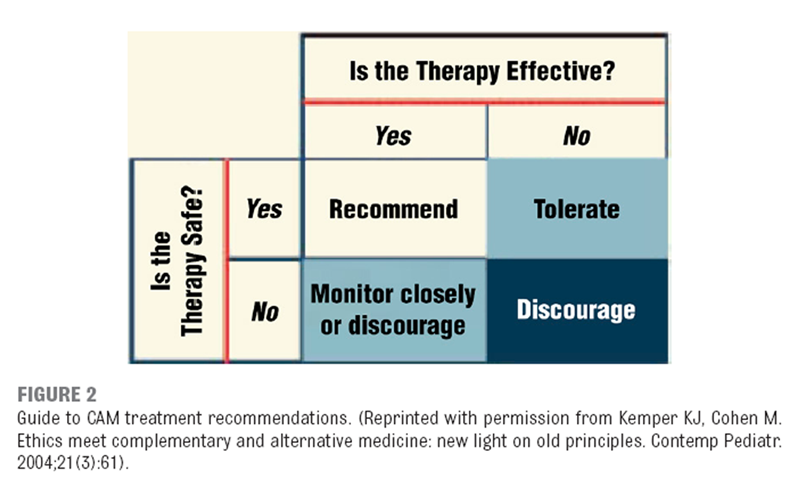
Figure 2 Factors to be included in a risk/benefit analysis when considering complementary and integrative therapies are the severity and acuteness of illness; curability with conventional care; degree of invasiveness; toxicities and adverse effects of conventional treatment; quality of evidence for efficacy and safety of the complementary therapy; and the family’s understanding of the risks and benefits of the treatment, voluntary acceptance of those risks, and persistence of the family’s intention to use complementary or integrative therapy (Figure 2). [77, 78]
The level of evidence required for evaluating efficacy can be small when there is little to no risk of harm from a therapy, especially when other therapies are likely to be futile. Likewise, the level of evidence for efficacy required to endorse a particular complementary therapy would be quite high when that therapy is risky and when safer, more effective therapies are available.
Situation-specific variables can also affect ethical decision-making. For example, the patient’s and parents’ personal beliefs, cultural values and practices, and therapeutic goals; the type and severity of illness; and the lack of efficacy and safety data in a specific patient can affect the decision to use complementary therapy. Even when such data are known for other populations, application of population data to individual pediatric patients requires inference and implies some degree of uncertainty. The tolerance of the patient, family, and primary care provider for uncertainty varies from one situation to another. [79] As experts in assessing safety and efficacy, pediatricians’ input into treatment decisions is critical in enabling families to make the best evidence-based decisions regarding these therapies.
Informed consent for any proposed treatment includes a discussion of the risks, benefits, and reasonable alternatives. Failure to discuss reasonable alternatives can create legal risk for a physician. [73] Although courts have not yet ruled that failure to offer reasonable complementary medicine alternatives is actionable, the potential for liability exists. Children should be allowed to participate in their care and decision-making in a manner that is appropriate and specified by state law; most states have very specific laws regarding age for assent for treatment.
Finally, primary care providers should be aware of and apply the 4 basic principles of biomedical ethics as described by Beauchamp and Childress:(1) respect for patients’ autonomy,
(2) nonmaleficence (avoiding harm),
(3) beneficence (putting the patient’s interest and well-being first), and
(4) justice (fairness in providing access to essential care). [42]In summary, if recommending complementary therapies, pediatricians are strongly encouraged to use an evidence-informed approach and give due consideration to issues of liability with relation to patient referral and/or a shared-care approach to treatment. A 2011 series in Pediatrics on legal and ethical issues pertaining to pediatric complementary and integrative medicine provides an excellent foundation of information on licensing and other specific medicolegal considerations. [64, 70–72, 74, 79–83]
Training and Education
Training in Complementary Therapies
Many complementary therapy providers provide care for children; however, most are trained as generalists in their fields. Pediatric specialty training is the exception, not the rule, in most CAM disciplines. The Committee on the Use of Complementary and Alternative Medicine by the American Public recommends that the national professional organizations for all CAM disciplines ensure the presence of training standards and develop practice guidelines. Ideally, health care professional licensing boards and accrediting and certifying agencies (for both complementary and conventional medicine) should set competency standards in the appropriate use of both conventional medicine and complementary therapies, consistent with practitioners’ scope of practice and standards of referral across health professions. [42]
Medical Education in Integrative Medicine
Despite high demand for integrative care, [42] a lack of systematic education about the safety and effectiveness of complementary and integrative therapies in pediatrics still exists. [9] One example of educational initiatives underway in pediatric integrative medicine to fill this gap is the Pediatric Integrative Medicine in Residency program, a 100-hour online educational curriculum that was implemented as a pilot in 5 pediatric residency training programs in the United States, and in 2016 it reached >500 residents nationally and internationally. [9] Osteopathic physicians receive extensive training in integrative medicine with regard to osteopathic principles and osteopathic manipulative treatment (OMT).
Other opportunities include online case-based training [44, 46] and educational courses at national meetings of the AAP through the Section on Integrative Medicine and collaborating sections and a variety of educational resources through the Complementary and Alternative Research and Education Program for Integrative Health and Healing (University of Alberta) [84] and the ACIMH. [10]
Common Complementary Therapies
What follows is an overview of each of these categories with resources for further reading, rather than an exhaustive review of individual therapies. The level of evidence evaluating the use of these therapies varies greatly. For some interventions, there are numerous high-quality investigations, but for others the data are sparser. It is important for individuals to weigh the best available evidence and risk/benefit ratio for any intervention used in children, either conventional or complementary.
Biologically Based Practices
The NCCIH designates natural products to include dietary supplements, herbal or botanical products, traditional medicine formulations, folk medicine, homeopathic remedies, probiotics, and food-based phytochemicals.51 It may be most important for the pediatrician to recognize that thousands of natural health products exist, many are routinely marketed to children and adolescents, hundreds of studies have been published in this area, good sources of synthesized information exist, and consistent caution is needed in assessing quality of natural health products and their potential for adverse interactions with prescription or over-the-counter medications.
Parents may use natural products for their children for a variety of reasons, including a desire to avoid prescription medication or a preference for a natural approach to preventive health.[6] Despite the fact that natural health products may be perceived as safe because of their natural origins, researchers have demonstrated the potential for serious toxicity and possible adverse reactions or events, especially in patients taking prescription medications concurrently. [85] Compounding this risk is the fact that safety standards that specifically address the pediatric population are lacking, [86] and parents may be reluctant to disclose the use of natural products for fear of censure or ridicule. [6] Failure of pharmacists and physicians to routinely inquire about natural health product use is another significant compounder. [86] Another challenge in this area is widespread reliance on passive surveillance systems that depend on health care providers or consumers to recognize and appropriately report adverse reactions, which may result in a serious underestimation of adverse reactions. [86]
One useful resource for primary care providers to address some of these concerns is the natural health products–drug interaction grid developed by Complementary and Alternative Research and Education Program. [87] Additional high-quality resources on drug–natural product interactions include these subscription natural product databases:
Natural Medicines (formerly Natural Standard and Natural Medicines Comprehensive Database) [88]; and ConsumerLab.com.
Dietary Supplements Commonly Used in ChildrenFish Oil The 2012 NHIS results revealed that fish oil is one of the most commonly used natural products in children. Docosahexaenoic acid found in fish oil has convincing evidence for supporting full-term gestation and is integral in the development of the brain, nervous system, retina, testes, and renal cortex. [89] It has also been associated with improvement of symptoms of neuropsychiatric disorders, such as ADHD in some children, with minimal adverse effects noted. [90, 91]
Melatonin Melatonin is another commonly cited dietary supplement in the NHIS in children. Melatonin is primarily produced by the pineal gland and is closely regulated by the suprachiasmatic nucleus, which regulates the sleep-wake cycle. Melatonin is used for functional sleep disorders to decrease sleep latency and in some children with neurodevelopmental disorders who have associated sleep disturbances. [92–94] Despite wide use, long-term studies on the safety and efficacy of pediatric melatonin use are lacking.
Probiotics Probiotics are a third commonly used category of dietary supplements. Probiotics are live microorganisms that offer benefit to their host. [95] In children, some probiotic strains have been demonstrated to shorten the duration of acute infectious diarrhea [96] and to decrease functional abdominal pain symptoms in some children. [97] Other important applications of probiotics and/ prebiotics include the prevention of atopic dermatitis in predisposed children. [98] Evidence supporting the use of probiotics in the prevention of necrotizing enterocolitis [99] and late-onset sepsis in preterm infants is strong and continues to accrue. [100]
Well-designed RCTs are expanding the evidence on natural products in a variety of other pediatric conditions, including the following: pain, headaches, ADHD, asthma, atopic disease, and colic, [101] among others.
Herbal Products
There are a number of excellent review articles on the use of herbal products in pediatric populations. [102–109] As with other natural products, due caution must be taken with herbal remedies, especially for individuals with allergic reactions to certain plants. Recognition and avoidance of potential herb-drug interactions will help pediatricians optimize patient safety. [110]
An example of a potential serious interaction includes the combination of prescription drugs with St. John’s wort, which can affect therapeutic dose of medications that are substrates of cytochrome P450s and/or P-glycoprotein, such as oral contraceptives, anticoagulants, calcium-channel blockers, digoxin, and benzodiazepenes. [111]
Another potential problem is seen in the aggressive marketing of energy drinks to adolescents. Many brands contain dietary supplements in addition to high levels of caffeine and sugar. [112] The AAP Clinical Report on sports drinks and energy drinks encourages pediatricians to screen for use of energy drinks and hidden sources of dietary supplements and to provide education to youth and parents on the inappropriate use of these supplements. [113]
Diet
The use of diets with what have been termed “functional foods” is an evolving research topic in pediatrics. One familiar example is the ketogenic diet, used for children with refractory and severe epilepsy, which has shown benefit in seizure control in some children comparable to antiepileptic drugs. [114] Elimination diets have been studied in IBS, [115] gastrointestinal food sensitivities or allergies, [116] atopic disease, [117] ADHD, [118] autism spectrum disorders, [119] and migraines. [120] A common concern about each of these types of diets are the risks of macro and micronutrient deficiencies.
A newer area of nutrition research in pediatrics is the use of the balanced Mediterranean diet pattern as a preventive tool in childhood obesity and its associated comorbidities, such as cardiovascular disease and metabolic syndrome. [121] A protective effect of the Mediterranean diet has also been noted against asthma, rhinitis, and eczema in certain pediatric populations. [122–124] Larger-scale studies are needed, including assessment of long-term outcomes of various diets in children.
Manipulative, Movement, and Body-Based Practices
The most commonly used manipulative, movement, and body-based practices in pediatrics include osteopathic manipulation, chiropractic, and massage. [1] According to the most recent NHIS, 3.3% of US children (1.9 million) used chiropractic or osteopathic spinal manipulation in 2012. [12, 125] Yoga is a popular movement therapy also widely considered a mind-body–based practice [11] and is discussed under the Mind-Body Therapies section of this report. Research on manipulative, movement, and body-based practices in children or adolescents is limited and available mostly for osteopathic manipulation, chiropractic, and massage. The studies primarily consist of case reports or small series with only a handful of small RCTs. A brief overview of the modalities follows.
Osteopathic medicine, practiced by those who have earned Doctor of Osteopathic Medicine (DO) degrees, emphasizes preventative medicine and holistic care. [126] In addition, OMT, a form of manual manipulation, is taught to all osteopathic medical students, emphasizing the importance of maintaining healthy muscle and lymphatic balance. DOs incorporate OMT to varying degrees in clinical practice, although it has been established that many DOs do not use OMT regularly in their care of patients. [127] Historically, osteopathic medicine has emerged as a separate discipline but has been accepted as an effective treatment modality in today’s health care climate in the United States. [128, 129] Although a small community of DOs maintains that osteopathy is a distinct discipline, [128] most consider OMT to be conventional therapy. The AAP Section on Osteopathic Pediatricians serves as an important resource for further education and evidence-based study in osteopathic medicine and provides an overview of evidence-based research.
https://www.aap.org/en-us/about-the-aap/Committees-Councils-Sections/Section-on-Osteopathic
-Pediatricians/Pages/Research.aspx?
Some chiropractors limit care to primarily musculoskeletal issues, but others see patients for wide variety of concerns. Infants and children are seen by chiropractors for many different reasons. A bias against childhood vaccinations has been shown to exist in chiropractic care; children 1 through 17 years of age in the care of a chiropractic practitioner were significantly less likely to receive recommended vaccinations, leading to higher risk of vaccine-preventable disease. [130] The AAP supports interventions to increase immunization awareness and recommends that primary care providers encourage and support families in fully immunizing children. High-quality evidence supporting effectiveness of spinal manipulation for nonmusculoskeletal concerns is lacking, especially in infants and children, for whom the risks of adverse events may be the highest because of immature stability of the spine. [56]Safety and Adverse Events Serious complications are possible with chiropractic treatment of children, but such adverse effects are rare and related to high-velocity, extension, and rotational spinal manipulation. [56, 131] It is essential that any known preexisting underlying pathology be discussed and an age-appropriate, thorough history and physical examination be conducted to exclude abnormal anatomic or neurologic findings before any type of manual or manipulative therapy is used on a child or adolescent.132 Prospective population-based active surveillance is recommended to accurately assess the rates of adverse events related to manual and manipulative therapies in children. [56] Studies are ongoing.
Massage Massage therapy is a common body-based practice often provided at home by parents to children and by licensed massage therapists and nurses in clinical settings. According to the latest NHIS, approximately 0.7% of US children (n = 385,000) used massage therapy, [12] which seems to be the same number as in many other countries. [132] Massage has become routine practice in many NICUs and has been shown to promote weight gain, growth, and development in preterm infants [133, 134] and may lead to shorter hospital stays and, thus, cost savings. [135] Infant massage may also have beneficial effects on the bilirubin concentrations of preterm infants, likely through increased stooling frequency. [135]
Massage has also been shown to increase weight gain in term infants [136] and has a beneficial effect on symptoms of colic, [137] pain in hospitalized children, [138] ADHD, [139] and depression. [137, 140] Although massage can be a beneficial adjunctive therapy in some childhood conditions mentioned previously, further studies are needed on the effectiveness of massage on many other childhood conditions.
Mind-Body Therapies
The NCCIH1 has reclassified complementary health approaches into 2 broad categories: natural products or mind and body practices. According to the NCCIH, [1] examples of mind-body therapies include, but are not limited to, mindfulness, meditation, yoga, tai chi, hypnosis, biofeedback, guided imagery, and journal writing. In a review of the overarching use of mind-body therapies in children, researchers found a low prevalence of adverse effects and good acceptance of these noninvasive therapies, even in children of preschool age, for several modalities, such as progressive muscle relaxation, music therapy, and guided imagery. [141]
Evidence for the use of selected mind-body therapies in children has recently been published in the first AAP Clinical Report on mind-body therapy use in children. [142] The following therapies were reviewed: biofeedback, clinical hypnosis, guided imagery, yoga, meditation, and mindfulness-based stress reduction. The range of therapies were successfully applied in a broad range of conditions, including chronic pain, migraine headache, tension headache, functional disorders of elimination, procedural anxiety, depression and anxiety, coping and self-regulatory skills, and sleep disorders, among other conditions.1 In emerging literature, benefits of school-based mindfulness in coping and self-regulation as well as reduction in psychological symptoms have been demonstrated. [143–146]Yoga Yoga has its historical origins in ancient Indian philosophy and has become a popular form of exercise and movement practice in Western nations. According to the 2012 NHIS, for children 4 to 17 years of age, there was a statistically significant increase in the use of any yoga, tai chi, or qigong between 2007 (2.5%) and 2012 (3.2%). Most of this increase can be attributed to the increased use of yoga (2.3%–3.1%), reflecting an estimated 429,000 more children using yoga in 2012 than in 2007. [12]
In a systematic review of yoga in children, Rosen et al [147] showed that yoga has a positive effect on psychological functioning, particularly to address emotional, behavioral, and mental problems in children, and proposed that schools may be an ideal place to introduce yoga programs. Yoga was found to be especially beneficial in children with asthma, IBS, juvenile idiopathic arthritis, and fibromyalgia in the review. [147] Authors of a systematic review of literature and a meta-analysis on yoga in the treatment of ADHD including 8 RCTs (n = 249 patients) suggested that yoga improves the core symptoms of ADHD. [148] Yoga has also been suggested to improve symptoms of IBS in adolescents [149] and asthma [150] and has been shown to help in stress reduction in children. [151]
Prenatal yoga has also been shown to reduce maternal anxiety and depression, according to a systematic review, [151] and to improve birth weight, decrease preterm labor, and reduce the risk of intrauterine growth restriction. [153, 154] More systematic studies are needed on the effects of prenatal yoga and yoga in other health conditions in children.
Spirituality Spiritual healing includes prayer and has traditionally been identified as one of the most prevalent complementary therapies in the United States. [155] Eighty-two percent of Americans believe in the healing power of personal prayer, 73% believe that praying for someone else can help cure their illness, and 77% believe that God sometimes intervenes to cure people who have a serious illness. [156] Prayer is used by up to two-thirds of parents for their children. [157, 158] Studies have suggested that spiritual and/or religious beliefs and practices may contribute to decreased stress and increased sense of well-being and enhanced immune system functioning. [157] In a large systematic literature review, Best et al [159] demonstrated that the majority of patients express interest in a discussion of religion and spirituality in the medical visit. Spirituality in health care is especially relevant to children in oncology and palliative care settings, in which skillful intervention can be of benefit to both child and family. [160]
RCTs of the clinical therapeutic effects of prayer in pediatrics are lacking, although work is active on a national level to introduce more structure into the use of spirituality in health care via the FICA Spiritual History tool for use in the clinical setting. Categories covered include Faith and belief, Importance, Community, and Address in care. [161] Some states have pursued legal measures against parents seeking prayer or spiritual healing as an alternative to conventional medical therapy for children with serious medical problems, such as cancer. The AAP report of the Task Force on the Family recommends that, although the religious beliefs of the family must be respected, parents must be held accountable for withholding medical care when doing so would likely result in death or suffering. [162] The majority of families surveyed viewed spiritual healing as a personal practice that is complementary to medical care rather than a replacement for it. [156]
Mind-body medicine is a rapidly growing area of research in children that shows low risk of adverse events. The 2016 AAP Clinical Report on the use of mind-body therapies in children provides a detailed overview of the current research in this area. [142] Potential concerns associated with the use of mind-body therapies may include delays in diagnosis or treatment of serious illness or use in a child with a history of trauma or who suffers posttraumatic stress disorder. Open discussion of all therapeutic approaches is important so that parents feel safe and supported in bringing their questions on the use of complementary therapies to conventionally trained health care providers. Additional studies are needed to evaluate safety and effectiveness of individual and combination mind and body therapies for specific medical conditions and overall well-being.
Biofield Therapies
Biofield therapies encompass several healing practices that include therapeutic touch, healing touch, and spiritual healing, among others. [163] The biofield therapies are “intended to affect energy fields that purportedly surround and penetrate the human body” and are “rooted in concepts of compassion, positive intention, self-empowerment, the mind-body-spirit triad, and the body’s innate tendency toward healing.” [164] Therapeutic touch and healing touch have been used successfully in pediatric oncology patients as a nonpharmacologic approach to reduction of pain and stress. [165–167]
Acupuncture
Acupuncture is an integral component of TCM, which has been practiced for thousands of years. The use of acupuncture is thought to address blockages, excess, or deficiency of “Qi,” defined in TCM as the circulating life force that flows through the body in meridians. [167] Acupuncture is performed using solid-core, small-gauge sterile needles to penetrate the skin, which are then commonly stimulated manually. Acupuncture points can also be stimulated by massage or pressure in a therapy called acupressure. Some children and adolescents may be more willing to try acupressure than acupuncture, especially patients with a fear of needles. [168]
The use of acupuncture is widespread in the United States, with increasing numbers of Americans having been shown to seek acupuncture treatments each year. [18] Researchers conducting the 2007 NHIS estimated that 150,000 children had received acupuncture treatment in the preceding year. [39]
In a 2011 systematic review of reported adverse events associated with pediatric acupuncture, Adams et al [55] concluded that acupuncture is generally safe in the pediatric population when practiced by an appropriately trained practitioner. The body of literature on the efficacy of acupuncture in specific conditions is accruing, although interpretation is hampered by study size and design variability. In a review of 24 systematic reviews involving 142 RCTs and >12,000 children, Yang et al [169] showed there is promise for the use of acupuncture in pediatric pain, nocturnal enuresis, tic disorders, amblyopia, and cerebral palsy, with few adverse events reported. In a review of the literature in a 2016 paper, Brittner et al [170] reflected a similar variability in study design and quality, with the strongest evidence seen in the treatment of pediatric headache and migraine and in treatment of postoperative pain.
Whole and Traditional Medical Systems
Whole medical systems involve complete systems of theory, diagnosis, and practice that have evolved independently from or parallel to conventional Western medicine. [1] The most commonly recognized whole medical systems include TCM, Ayurvedic medicine (India’s traditional system of medicine), and naturopathy. [171] Each generally relies on the use of a detailed diagnostic process and uses highly individualized treatment protocols that may involve diet and exercise, along with herbal treatment, making them more challenging to evaluate, especially in pediatrics.TCM TCM is a complete medical system that includes a variety of practices such as acupuncture, herbal medicine, moxibustion (burning an herb above the skin to apply heat to acupuncture points), tui na (Chinese therapeutic massage), acupressure, cupping, dietary therapy, and tai chi and qigong (see Mind-Body Therapies). [172] Herbal medicines used in TCM can have powerful therapeutic but also toxic effects on the body’s biochemistry and may also affect the metabolism of other drugs. [173, 174]
Ayurveda Ayurvedic medicine is one of the oldest whole medical systems in the world and is widely used in India and South Asia. [175] The word Ayurveda means “the knowledge of life” and comes from the Sanskrit words “ayur” (life) and “veda” (science, knowledge). Ayurvedic medicine concepts include universal interconnectedness (people, health, universe), the body’s constitution (prakriti), and life forces (dosha). Ayurvedic physicians prescribe individualized treatments, including diet, herbs, spices, exercise, and lifestyle. [176] Similar to herbs used in TCM, Ayurvedic herbal medicines can have both powerful therapeutic and toxic effects and may expose patients to heavy metals, especially lead, mercury, and arsenic. [168, 177–179] Ayurvedic approaches have been studied in children for treatment of certain conditions (for example, iron-deficiency anemia). [168] Curcumin is valued in Ayurvedic medicine for its antiinflammatory properties and has been evaluated for safety and tolerability in children with IBS. Further studies on its specific clinical application and dosing in pediatric conditions are needed. [180] A 2012 Cochrane Systematic Database review commented that curcumin may be safe and effective as an adjunct treatment in the maintenance of remission in ulcerative colitis. [180] Further studies are needed to determine the efficacy and safety of Ayurvedic treatment modalities in pediatrics.
Naturopathy Naturopathy is guided by a philosophy that emphasizes the healing power of nature. Naturopaths use both traditional and modern therapies (approaches they consider to be the most natural and least invasive) and view their role as supporting the body’s inherent ability to maintain and restore health. [172, 181] There is currently little evidence on the use of naturopathy in medical conditions in children.
Insurance Coverage
The Patient Protection and Affordable Care Act [182] was signed into law in 2010 and ensured coverage for essential health benefits. The initial list of 10 essential health benefits included ambulatory care, emergency services, hospitalizations, laboratory services, maternity and newborn care, mental health and addiction treatment, rehabilitation services, pediatric care, prescriptions, and preventive, wellness, and chronic disease treatment. Although the Patient Protection and Affordable Care Act promotes wellness, the effect on compensation for integrative medicine services is still unclear. States have discretion regarding which services are considered part of the essential health benefits. For example, some states include acupuncture as an essential health benefit (at the time of writing, this includes California, Florida, Minnesota, New Mexico, and Oregon). Many states include chiropractic as an essential benefit, typically under rehabilitation services. Section 2706a of the Public Health Service Act states that an insurer “shall not discriminate with respect to participation under the plan or coverage against any health care provider who is acting within the scope of that provider’s license or certification under applicable State law.” The type of health care provider is not specified and, therefore, is open to a level of interpretation. An ongoing obstacle for health insurance companies is a lack of standardization in credentialing and coding of complementary medicine services, compounded by the sparse number of Current Procedural Terminology codes that adequately cover these services. [183]
Conclusions and Recommendations
Pediatricians and other primary care providers who care for children are encouraged to advise and counsel patients and families about relevant, safe, effective, and age-appropriate health services and therapies, regardless of whether they are considered conventional or complementary therapies. In the 2001 AAP Periodic Survey of Fellows, 73% of pediatricians agreed that it is the role of pediatricians to provide patients and/or families with information about all potential treatment options for the patient’s condition, and 54% agreed that pediatricians should consider the use of all potential therapies, not just those of mainstream medicine, when treating patients. Because most families use complementary and integrative health services without spontaneously reporting this use to their primary care provider, pediatricians can best provide appropriate advice and counseling if they regularly inquire about all the therapies the family is using to help the child.
Pediatricians should seek continued and updated knowledge about therapeutic options available to their patients (whether they are mainstream or complementary) and about the specific services used by individual patients to promote discussion about the safety, appropriateness, and advisability of complementary therapies. Only then can pediatricians appreciate the concerns of their patients and families and offer them the thoughtful and knowledgeable guidance they may require. Given accruing supporting evidence and the potential of integrative approaches to improve preventive care in children, policy and health insurance coverage should evolve accordingly to provide fair coverage for patients and equitable payment for physicians.
Tips on Talking to Patients
The NCCIH provides a toolkit [184] with materials to help both patients and providers talk about the use of complementary health practices. The following practical tips will help health care providers feel “ARMED” to address the topic of complementary approaches with more confidence and ease.A: Ask about the different therapies used by patients. Patients and parents often do not disclose use of complementary therapies because many of them believe that it is not relevant or not within the primary care provider’s interest or expertise. [185, 186] By asking routinely, pediatricians can learn whether a child is receiving complementary therapies. This knowledge is essential for the pediatrician to evaluate and counsel about potential adverse effects and to enhance the probability of correctly attributing improvements or adverse effects to the specific intervention. Questions that include examples are often helpful in jogging memories and enhancing disclosure. Rather than asking whether a patient is using any alternative therapies, the pediatrician might ask whether the patient is using any “vitamins, herbs, supplements, teas, home remedies, back rubs, chiropractic, acupuncture, or other services to enhance health.” It is also often useful to ask how the patient manages stress; examples here may include exercise, prayer, music, or talking with friends or trusted adults;
R: Respect the family’s perspectives, values, and cultural beliefs in open, ongoing communication centered on the patient’s well-being. Recognize cultural or educational differences. Demonstrate respect for families and their values. Work together with the parents as a team to consider and evaluate all appropriate treatments. A discussion of an array of conventional and complementary treatment options may be required. By actively listening to families and patients, pediatricians can become important allies in examining all potential treatment options for children. Maintaining a dialogue to promote the best interests of the child is critical to the integrity of the medical home;
M: Monitor the patient’s response to treatment and establish measurable outcomes for evaluation. Measurable outcomes, such as specific goals for symptom relief, can be established. The concept of primum non nocere (“first do no harm”) is central to all clinical practice. If there is a lack of response or an untoward response, the therapy needs to be reevaluated;
E: Educate yourself and the patient and/or family by identifying credible, evidence-based resources on complementary therapies. Complementary medicine is an evolving field, and maintaining current knowledge of popular complementary therapies is important in evaluating safety and effectiveness of integrative health approaches. Become familiar with the definitions, terms, and uses of complementary practices and learn about specific complementary therapies patients are using in your community. Identify the most common modalities and professionals that are available in your pediatric practice area; and
D: Distribute evidence-based information about relevant therapies available from the NCCIH, the ACIMH member institutions, and an increasing number of publications in peer-reviewed journals and professional review articles.
Abbreviations:
AAP — American Academy of Pediatrics
ACIMH — Academic Consortium for Integrative Medicine and Health
ADHD — attention-deficit/hyperactivity disorder
CAM — complementary and alternative medicine
DO — Doctor of Osteopathic Medicine
DSHEA — Dietary Supplements Health and Education Act
FDA — Food and Drug Administration
IBS — irritable bowel syndrome
NCCIH — National Center for Complementary and Integrative Health
NHIS — National Health Interview Survey
NIH — National Institutes of Health
OMT — osteopathic manipulative treatment
RCT — randomized controlled trial
TCM — traditional Chinese medicine
Acknowledgment
We thank Kathleen Kennedy for administrative support.
FINANCIAL DISCLOSURE:
The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING:
No external funding.
POTENTIAL CONFLICT OF INTEREST:
The authors have indicated they have no potential conflicts of interest to disclose.
ReferencesPlease refer to the Full-Text article
NOTE: Opens in a second browser screen for your convenience
Return to PEDIATRICS
Return to INTEGRATED HEALTH CARE
Since 3-22-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |