

Infant and Child Chiropractic Care:
An Assessment of the ResearchThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




By Anthony L. Rosner, Ph.D., LL.D.[Hon.], LLC
Foundation for Chiropractic Education and Research
Norwalk, IA. 2003
Dr. Anthony L. Rosner, a 1972 graduate of Harvard University (PhD in biological chemistry/medical sciences), was the Director of Research and Education for the Foundation for Chiropractic Education and Research (FCER), and was then the Director of Research Initiatives at Parker College of Chiropractic. He is currently the Research Director for the International College of Applied Kinesiology.
OUTLINE:
I. Pediatric Health Concerns
II. Theory
III. Practice
IV. Managing Pain
A. Epidemiological Considerations
Back Pain
Neck and Shoulder Pain
Headache
Otitis Media
Infantile Colic and Constipation
Nocturnal Enuresis
Asthma
B. Outcomes as Demonstrated by Research Reports
Back Pain
Headache
Otitis Media
Infantile Colic and Constipation
Nocturnal Enuresis
Asthma
Retrolisthesis and Scoliosis
Neurological Disorders: Epilepsy, Autism, Attention Deficit/Hyperactivity Disorder
C. Positioning the Chiropractic Practitioner
Physical Attributes and Applications
Chiropractic Paradigms As Guiding Principles
V. Safety
VI. Concluding Remarks
Appendix I: Response To Systematic Review on Pediatric Safety
REFERENCES




I. PEDIATRIC HEALTH CONCERNS:
Load the References in a separate window for easy viewing
In addition to our parental instincts, consider that the welfare of our children and adolescents is no less than the welfare of our future. That is why we need to pay serious attention to the following pediatric health issues.
Pediatric back pain is far more prevalent than was assumed a decade ago. [1]
The lifetime prevalence of low back pain among schoolchildren has been reported to be anywhere from 20% to 51%. [2–6]
Surveys of 10,000 children conducted in 101 elementary schools indicate that pupils often use chairs or desks that are of inappropriate height or size for their grade level; 30–54% of students carry backpacks significantly exceeding recommended weights; and physical education sessions are inadequate. [7]
Backpack use and weight are associated with back pain in children. [8–9]
Up to 97% of school children may use backpacks; [9] however, the vast majority of childhood patients in the clinic rarely attribute their back pain to backpacks. [10]
In addition to back pain, the use of backpacks has been associated with reduced lung capacity, especially evident in children experiencing adolescent idiopathic scoliosis. [11]
Over 20% of adolescent girls and 10% of boys experience chronic, recurrent neck and shoulder symptoms. [12] But in some populations, headache prevalence in schoolchildren during a given year may be as high as 80–90%. [13–14]
Otitis media [ear infections], the most common pediatric disorder in the United States, accounts for over 35% of all visits to the pediatrician in the United States, [15] resulting in over 25 M office visits in 1990. [16] Yet the most common means of medical treatment [antibiotics and tympanostomy], have been shown to be woefully inadequate [17–19] with clear risks. [20–21]
Infantile colic—unexplainable and uncontrollable crying in infants from 0–3 months old, occurs in 8%–49% of newborns with an average of 22.5%. [22] Yet its cause remains a medical mystery. [23]
Nocturnal enuresis—the persistent wetting of the bed at night in the absence of urological and neurological pathology after the age of 4, occurs in a fifth of all 4–5 year olds [24] and persists in 7% of 8–year olds. [25]
While the annual incidence of asthma in children in the United States is 7%, [26] the fact remains that it is the most common chronic disease in childhood [27] with its debut during the first year in life in about 30% of infants and in more than 50% before 2 years of age. [28]
As will be pointed out in this monograph, there is evidence that in all of above conditions the conventional, more widely accepted regimes of medical treatment are beset with severe limitations. It is therefore imperative for us to consider alternative treatments which have demonstrated efficacy, cost-effectiveness, and safety. With more children having used chiropractic than any other form of alternative therapy [homeopathy, naturopathy, acupuncture, osteopathy, oligotherapy, others], [29] this should be the form of healthcare intervention given priority as we seek improved pediatric care. This is both apparent and timely since it has been shown that the gaps between what we know and what we need to know and what we know and what we do in pediatric practice is substantial. [30]
II. THEORY:
Load the References in a separate window for easy viewing
Heiner Biedermann, a German Practitioner in Conservative Orthopedics and Member of the European Workgroup in Manual Medicine, has pointed out that children in early development are subjected to two formidable challenges to their musculoskeletal system. [31] The first is the trauma of passage through the birth canal, one of the most dangerous journeys to be traversed in a lifetime, according to a variety of sources–mostly obstetricians. Here it appears that intracranial structures of apparently healthy newborn individuals display a high percentage of indications of microtrauma of brainstem tissues in the periventricular region, [32] and it is believed that exposed structures of the occipito-cervical junction suffer at least as much as the cranium. [33] In summary, it appears that injury to both the intracranial and subcranial structures is the rule rather than the exception. [31] The second major onslaught to the child’s emerging musculoskeletal system occurs when the infant has to master the transition from a quadruped to a biped, mastering the task of maintaining an upright spine in learning how to walk. Superimposed upon this burdensome task is the fact that the last major growth spurt usually occurs between the ages of 11 and 13, at just the time that such risks to the integrity and alignment of the spinal curve as backpacks, [6–7] and other factors in the elementary school environment are imposed. After all these events, both the complaints and treatment regimens of such individuals become congruent with those of adults.
Prior to adolescence, the infant and the juvenile are highly susceptible to developmental irregularities that may exert a lifetime influence if not properly attended to. At the same time, these same individuals appear to be logical candidate for conservative forms of corrective treatment. This leads to an essential piece of information regarding manipulative therapy for small children: As pointed out by Biedermann, it [spinal manipulative therapy] is not a scaled-down version of the procedures used for adults. [31, 34]
The kinematic imbalances brought on by the suboccipital strain at birth give rise to a concept in which symptoms and signs associated with the cervical spine manifest themselves into two easily recognizable clinical presentations. The leading characteristic is a fixed lateroflexion [called KISS I] or fixed retroflexion [KISS II]. KISS I may be associated with torticollis, asymmetry of the skull, C–scoliosis of the neck and trunk, asymmetry of the gluteal area and of the limbs, and retardation of the motor development of one side. KISS II, on the other hand, displays hyperextension during sleep, occipital flattening that may be asymmetrical, hunching of the shoulders, fixed supination of the arms, orofacial muscular hypotonia, failure to lift the trunk from a ventral position, and difficulty in breast feeding on one side. [34] The leading trademarks of both KISS I and KISS II are illustrated in Figure 1. [31]

In essence, these birth experiences lay the groundwork for rationalizing the wisdom of providing chiropractic healthcare to the pediatric population. What follows is a brief description of practice, followed by descriptions of the evidence supporting chiropractic for managing a wide variety of childhood conditions such that chiropractors have earned the privilege of treating children for a variety of conditions on a first-contact basis without requiring referral.
III. PRACTICE:
Load the References in a separate window for easy viewing
Manipulation of children appears to date from at least 1727, at which time Nicholas Andry coined the term "Ortho-Paedics" to depict "straightening the young" and became the defining principle of the medical procedures that he published. [31] In this context, the goal of all chiropractic interventions is to alleviate or eliminate perceived asymmetries in spinal structure, posture or gait, as well as reduce symptoms for a variety of conditions which will be described below. No chiropractic adjustment is ever prescribed without evidence of a relative decrease in mobility at a particular articulation.
Examination procedures preceding the chiropractic adjustment include static or motion palpation. It has been suggested by some that radiography may be useful to assess asymmetries and confirm the direction of the impulse to be applied. [31] The elastic properties of the developing spine require that vectors which would introduce extraneous forces into the spine [such as from mobilization or long-lever contacts] should be kept at a minimum. Nonspecific maneuvers which are discouraged include supine, prone or seated rotary break, hyper lateral flexion and rotation, longitudinal traction, extension, flexion, and extension. Instead, the increased flexibility of the child's spine requires a preload tension that is greater than that experienced by adults. This is followed by a high acceleration thrust considerably gentler than that applied to adults. A deceleration period and 1–2 second holding period, increases the effectiveness of the adjustment. [35] Especially with infants, specific contacts are made more often through the fingertips rather than the hypothenar or pisiform applications experienced with adults. Craniosacral procedures primarily limited to non-force indirect methods have also been proposed and implemented. [36] In managing the aforementioned KISS syndromes,
Biedermann describes an impulse manipulation in which the direction of the manipulation may be guided by radiological findings, orientation of the torticollis, palpation of the segmental dysfunction, or the local pain reaction. The intervention itself involves a short thrust of the proximal paland of the medial edge of the second finger, primarily lateral but with the possibility of adding a rotational component. [34] Finally, extensive attention to nutritional matters—including counselling in issues related to vitamin and mineral intake, balanced diets, and food allergies—has long been a component found in most chiropractic practices. [37]
IV. MANAGING PAIN:
Load the References in a separate window for easy viewing
According to the widely recognized International Association for the Study of Pain, "Inadequate prevention and relief of children's pain are still widespread, a deficiency highlighted during the current IASP Global Year Against Pain in Children." [38] Furthermore, both the physical and psychological responses to pain in children may very well increase their risk of incurring chronic pain in adulthood. [39–41] Research into the nature and assessment as well as treatment of children's pain is said to have grown "exponentially" over the past two decades. [42] It is thus imperative that the most efficacious, cost-effective, and minimally invasive interventions learned from research be put into practice by the most qualified and accessible practitioners available. The purpose of this monograph will be to justify the role of chiropractic as being able to fulfill that need. This should be apparent from [a] epidemiological considerations, [b] outcomes as demonstrated by research reports, and [c] the qualifications of the practitioner.
A. Epidemiological Considerations:1. Back Pain:
It is clear that low back pain can begin in childhood. 10% of children aged 9–10 have been reported to suffer from it with 2% of schoolchildren experiencing disability because of it. [43] In schoolchildren, the lifetime prevalance of low back pain has been estimated to be anywhere from 20% to 51%. [2–6] As shown in Table 1, point, 1-month and 1-year prevalences of back pain in childhood and adolescent populations come close to these figures, ranging from 12–56%. Some 35% of children with low back pain at age 15 participating in one study still were reporting continuous or recurrent pain at 18 and 23 years of age. Furthermore, nearly all [89%] of those who reported pain at all three ages displayed various stages of disc degeneration by MRI at age 15–whereas the aberrant MRI images were evident in only 26% of subjects without recurrent low-back pain. [52]
TABLE 1: PREVALENCE OF BACK PAIN IN PEDIATRIC AND ADOLESCENT POPULATIONS
NATIONALITY AGE PREVALENCE [%] United States [4] 13–16 30.4, point United Kingdom [44] Adolescent 11.5, point United Kingdom [45] 11–14 24, 1 month United Kingdom [46] 11–15 12, annual 11 22, lifetime 15 50, lifetime Switzerland [47] Schoolchildren 27, point Denmark [1] 8–10; 14–16 39, 1 month Denmark [48] 12 56, 1–year Turkey [49] 17–20 lifetime Finland [50] 11.8 53.8, 1–year Finland [51] 14 8, point [female] 14 10, point [male] 16 14, point [female] 16 11, point [male] 18 13, point [female] 18 17, point [male]
Ergonomic factors play a major role in this problem. Children in 101 elementary schools revealed that 10,000 children were using chairs or desks of improper height or size for their grade level. [8–9] But the lion's share of back problems has been attributed to the improper use of backpacks. [8–11]
As many as 97% of schoolchildren may be using backpacks. [9] According to a recent news release, this may result in several casualties: [53]
Over 75% of adolescents aged 12–18 experience some form of back pain, with the weight of their back pack having been identified as a leading contributor to this pain.
One study of Italian schoolchildren revealed that over a third carried more than 30% of their body weight at least once a week, in excess of the limits proposed for adults.
The average backpack weight for students has been found to be 17% of their body weight, in excess of the 10% proposed by pediatric chiropractors and orthopedic surgeons.
In other studies:
Female students who used backpacks during the day had twice the odds of developing back pain. [8]
Back pain was more likely to be reported in students who carried heavier loads or who used backpacks more frequently during the average school day. [8]
Students without back pain were more likely to attend a school that banned the use of backpacks between classes. [8]
The increased contact pressure and asymmetric shoulder loading apparent with average backpack loads of 22% of body weight were associated with significant pain and injury. [54]
In addition to back pain, the use of backpacks has been linked to reduced lung capacity, especially evident in children afflicted with adolescent idiopathic scoliosis. [11]
In active adolescents, spondylolysis has been identified as the most common cause of low back pain. It is seen in 5–6% of the population and usually is triggered by injuries to the posterior elements of the spine, most commonly L–5, L–4 and L–3. Primary causes include sporting activities involving hyperextension combined with rotation such as experienced in gymnastics, wrestling, and weightlifting. [55]
What is of paramount importance is that back pain in childhood and adolescence becomes a risk factor for experiencing back pain in adulthood. Thus its proficient management in the early and formative years would be expected to diminish the pain and disability experienced later in life.
One 25-year prospective cohort study showed an increased lifetime prevalence of low back pain in individuals who had incurred low back pain in their adolescence. It was shown that low back pain in the gowth period and familial occurrence of back disease are important risk factors later in life, the increase of probability reaching 88% if both factors are present. [56–57]
If back pain becomes chronic, its very nature has shown that it tends to recur again and again over several years. [58–60]
2. Neck and Shoulder Pain
Load the References in a separate window for easy viewing
From a database of 62,677 12, 14, 16 and 18 year olds and 127,217 14–16 year olds taken from national and classroom surveys in Finland, the prevalence of neck and shoulder pain was found to be increasing from the 1980s steadily through 2001. As shown by Table 2, prevalence increased with age in both genders. Most dramatic was the fact that the authors concluded that, for the low back, neck, and shoulder in adolescents. "This pain suggests a new disease burden of degenerative musculoskeletal disorders in future adults." [51]
TABLE 2: PREVALENCE OF NECK AND SHOULDER PAIN IN ADOLESCENT POPULATIONS
NATIONALITY AGE PREVALENCE [%] Finland [51] 14 24, point [female] 14 12, point [male] 16 38, point [female] 16 16, point [male] 18 45, point [female] 18 19, point [male] Netherlands [61] 12–16 12, point Canada [62] Grades 7–9 28, annual
This is not surprising, in that another Finnish study indicated that the risk of neck and shoulder pain increases markedly with computer usage exceeding 2–3 hours per day. The population studied was a sample of 14–, 16–, and 18–year olds. [63] A recent Dutch study, however, attributed the neck and shoulder pain in a similarly aged population to depression and stress, but not computer usage and physical activity. [61] Finally, a study from New Mexico reignites the debate over backpacks discussed above by suggesting from a descriptive study that a correlation exists between backpack weight per body mass index in adolescent girls. [64]
The message to keep in mind is that prevalences are seen to be increasing with age, again suggesting that these conditions can be expected to extend into adulthood without proper management. Yet further evidence supporting this assertion can be found in a South Australian cohort of 13–17 year-old boys and girls in which the prevalence of neck and upper back pain was found to be steadily increasing through 5 years of schooling. [65]
3. Headache
As shown in Table 3, headache prevalence in pediatric populations are significant, having been reported to be as elevated as 80–90% over the past year in schoolchildren, [66–67] ranging downward to 23% in 10–17 year-olds [68] with a marked elevation [as high as 40%] in girls over boys in Sweden. [73] Classification of headache types has been reported to be difficult due to the fact that there are no specific criteria pertaining to this population. [75] Of the 35% of patients that could be classified in one study, the majority [63%] had chronic tension-type headache according to the International Classification of Headache Disorders. Another 14% were identified due to the probable overuse of medications. [76] From the multivariate regression analysis conducted in another study of Norwegian adolescents aged 12 to 14 years, frequent headaches at 1-year followup could be significantly predicted by:
(1) numerous headaches at first assessment,
(2) impairment [reduced leisure time activities],
(3) high depressive scores, and
(4) gender–in which girls had a worse outcome. [77]
TABLE 3: PREVALENCE OF HEADACHE IN PEDIATRIC AND ADOLESCENT POPULATIONS
NATIONALITY AGE PREVALENCE [%] Brazil [66,67] Schoolchildren 80–90, 1-year period Netherlands [68] 10–17 23, weekly Finland [69] 6 15, 1-year period Finland [70] 6.7–8.7 12, 6-year period Finland [71] 12 12, point Sweden [72] 11–17 7 boys, 2-year period 14 girls, 2-year period Sweden [73] 7th Grade 29 weekly [female] 7th Grade 31 weekly [male] 8th Grade 43 weekly [female] 8th Grade 11 weekly [male] 9th Grade 40 weekly [female] 9th Grade 10 weekly [male] Norway [74] 12.5–15.7 8.1, 1-year period
Family histories of headache are common in children with headache. [68] Two recent studies have shown that anxiety and depressive symptoms are not elevated in children with migraine and tension-type headache as compared to those without these disorders. [78] Regarding tension-type headache, however, shoulder pain, depression, and oromandibular dysfunction have been independently associated with this disorder. [71]
4. Otitis Media
Load the References in a separate window for easy viewing
a. Prevalence and Cost: Otitis media is an inflammation of the middle ear which is seen most commonly in children from birth to the age of 7. As the most common pediatric disorder in the United States, otitis media is responsible for over a third of all visits to the pediatrician in the United States, [15] totalling 25M office visits in 1990 [16] at a national direct cost for management at $5.3 billion [79] with other estimates reaching $8 billion [80] factoring in such indirect expenses as failed treatments or overuse of questionable methods to be discussed below. Acute otitis media is reported to occur in 60% of all children during their first year and in 85% by the age of 3, with 17% of children at one year reporting recurrent episodes. [81] By the age of 3, 50% of children will have had more than three episodes of acute otitis media, [82] and recent studies suggest that its incidence is increasing. [83] Certainly from 1975 to 1990, despite the routine use of antibiotics, the incidence of otitis media with effusion in the United States is estimated to have increased by 250%. [84]
Risk factors for otitis media include allergies [85, 86] attending a daycare center with a large population, [86] and pacifier use past the age of 10 months. [87] Children whose parents smoke experience 50% more ear infections than children whose parents do not smoke. [88] Potential morbidities include hearing loss or a delay in development. [89, 90] The good news is that otitis media is rarely fatal, with perhaps one patient in 10,000 who would experience such infectious complications as meningitis or mastoiditis leading to serious illness or death. [91]
b. Rationale: The approach to managing otitis media should begin with understanding the function of the eustachian tube. Collection of either clear or purulent fluid in this region is the identifying characteristic of otitis media. A likely reason as to why this is so much more prevalent in children than adults has to do with the anatomic variation of the adult and pediatric cranium. The cross-sectional area of the adult eustachian tube, for example, is 2.25–2.75 times larger than that of the 2-year old child. [92] In addition, it’s inclination from the temporal bone to the nasopharynx is 45° in the adult, but only 10° in children, impeding natural drainage. Finally, a component of the eustachian tube believed to be critical in its active opening [elastin] is sparse in children as compared to adults. [93] Finally, the muscles responsible for the opening and closing of the eustachian tube are thought to become more developed at ages beyond childhood. [94] As shown in Figure 2, this function is primarily regulated by the tensor veli palatini muscle which in turn is innervated by the trigeminal nerve. [95, 96] Secondary regulation of the tube might also be affected by the levator veli palatini and salphingopharyngeus muscles.

Misalignment of the C1 vertebra and/or occiput, affecting components of the superior cervical sympathetic ganglion, would be expected to influence, in turn, the tonus of the tensor veli palatini muscle, the vagus nerve, the inferior vagal ganglion, and ultimately the levator veli palatini, salhingopharyngeus, and superiorconstrictor muscles. All these sequelae would be presumed to lead to the undesirable construction or closure of the eustachian tube. Treatments such as manipulation in an effort to alleviate this vertebral misalignment would therefore appear to be the most direct and attractive possibility. [97]The other major fact to consider is the case against the premature and indiscriminate use of medical alternatives in treating otitis media.
c. Risks of Medical Alternatives:
ANTIBIOTICSAs medical practices evolve with our increasing knowledge as well as a changing environment, so must theadvisability of using antibiotics as a first line of treatment for otitis media. To continue the indiscriminate use of such medications in the face of mounting evidence constitutes significant health risks to both the individual patient and the population as a whole. Prescribing antibiotics without even examining the patient is particularly problematical. There are at least 5 reasons to seriously question the use of antibiotics as a first line of treatment for otitis media:
1. A significant percentage of otitis media cases are not even caused by bacteria
According to numerous studies outlined by Schmidt, anywhere from 20–40% of otitis media cases in which the middle ear fluid has been cultured fail to yield bacterial strains in culture. [98] One would therefore deduct that these represent otitis media cases caused by either viruses or sterile effusions–both of which by definition would not be expected to ever respond to antibiotics. Strong support for this conclusion has been recently provided by Pikaranta, who demonstrated that viruses without pathogenic bacteria were found in the middle ear fluid of the majority of samples taken from children with otitis media with effusion. [99] Should fluid cultures not be obtainable, examination of the ear by otoscopy and/or tympanometry [100] would be expected to yield clear indications of the etiology of the ear infection, helping to segregate those cases which theoretically would be amenable to treatment with antibiotics. The remainder of otitis media cases would have no chance of responding to antibiotics, making their prescription without the direct examination of the patient untenable.
2. Widespread use of antibiotics for any condition could lead to calamitous bacterial resistance
The remarkable ability of bacteria to develop resistance to antibiotics is well-documented. This would include [i] enzyme mutations which allow bacteria to inactivate beta-lactam drugs, [ii] development of intracellular pumps to remove antibiotics before they can destroy the host cell, [iii] cell wall protein changes which block antibiotics from entry, and [iv] synthesis of substitute proteins which escape the lethal effects of antibiotics. [101] To make matters worse, antibiotic resistance may be transferred via plasmids from a resistant bacterial strain to a nonresistant strain that is not even the same species. [101] Among clinical isolates of some bacterial species, strains resistant to all available antibacterial agents have been identified. [102] Simply put, each time an antibiotic is used there is the risk that a resistant mutation may develop and proliferate–meaning that the use of antibiotics does not come without a price. Increasing populations of multidrug resistant bacteria from 1995–1998 have been extensively described within the United States. [103]
The consequences of this problem for the world's population could be disastrous. The increased morbidity, mortality, and costs of worldwide resistance of bacteria to antimicrobial drugs is already a matter of record; in fact, a recent article in Forbes reports that drug-resistant infections kill more Americans than AIDS and breast cancer combined. [104] Both the Institute of Medicine in the United States in 1992 [105] and the Centers for Disease Control in 1994 [106] have warned of this growing threat. Remedies linked to a global plan of the World Health Organization [107] include the request to educate parents to avoid asking for antimicrobials when they are not useful and to urge that physicians prescribe them conservatively. [108]
The indiscriminate use of antibiotics appears to have risen to abusive levels. In a lead editorial published ithin the past year, The International Herald Tribune suggests that a major health problem in developed ountries is the overutilization drugs, including the fact that the Centers for Disease Control estimates that one-third of antibiotics taken on an outpatient basis in the United States are unnecessary. Should we continue to use antibiotics at our present level, protection will not be available 50 years from now since almost every major infectious disease is becoming resistant to currently available medicine. [109]
The problem becomes even more acute when one considers otitis media. According to Ambrose Evans-Pritchard, the situation is described as follows:"In the U.S., there are 24.5 million doctor-visits a year by children with ear infections. They are typically given antibiotics, and in many cases they care kept on a constant, low dosage course for the whole winter. U.S. parents expect no less. But we now know that there is price to be paid for this: more people will die of pneumonia, which is treated with variants of the same drugs. A quarter of all cases of streptomyces pneumoniae in the U.S. are now resistant to know drugs, compared with 0.002 per cent a decade ago." [110]
In this regard, it is important to note that in The Netherlands, where a waiting period of 1–2 days is routinely observed before antibiotics are given for otitis media, occurrence of antibiotic resistance is 1%, compared to the 25% level in the U.S. where antibiotics are given immediately. [111] A 1992 study suggested that more than 90% of the colds and respiratory tract infections for which antibiotic prescriptions were written for adults were viral in origin, rendering these antimicrobial drugs ineffective. In fact, it was presumed that antibiotics are overprescribed by 50% in the United States and Canada. [112]
The take-home message from all the previous arguments would be that antibiotics should be considered as a later [instead of a first] resort.
3. Side-effects have been linked to the use of antibiotics for otitis media
By destroying bacteria, antibiotics may wreak havoc upon beneficial species as well as those presumed to be causing harm. A perfect example would be their disruption of the ecological balance of intestinal flora. In so doing, the bacteriocidal effects of antibiotics might be expected to allow proteins which are normally blocked from adsorption to pass through the intestinal wall, leading to what is commonly known as a "leaky gut" syndrome. In so doing, antibiotics could allow foreign proteins to be introduced into the bloodstream, leading to the raising of antibodies and the creation of allergic responses within the host. [98]
A recent report is disturbing in that it suggests that there is an increased risk of asthma symptoms with antibiotic use. Specifically, the odds ratio for the risk of asthma rises to 2.7 if antibiotics were ever used, and this risk increases to over 4 if antibiotics were used in the first year of life. Furthermore, the risk increases from 2.3 with 1–2 courses of antibiotics to over 4 if 3 or more courses are used, making the risk appear to be dose-dependent. [113] This phenomenon [an association, not a causation] could well be explained by the aforementioned "leaky gut" phenomenon, in which allergic responses could be manifested by the constriction of bronchial airways and the resulting development of asthmatic symptoms.
A further complication with antibiotics is suggested by the work of Jochen Schacht at the University of Michigan. Animal studies have shown a profound hearing loss [61 db auditory threshold shift at 18 kHz] in in guinea pigs receiving gentamicin, possibly due to a free-radical mechanism of toxicity of aminoglycoside antibiotics [114] which destroys hair cells in the cochlea and the lower turns of the outer ear. [115, 116] L–carnitine, a naturally occurring neuroprotective agent which is required for the transport of long-chain fatty acids across the mitochondrial membrane prior to their oxidation resulting in ATP formation, has been shown to prevent both neonatal mortality and sensorineural hearing loss induced by gentamicin. [117]
Finally one has to note a recent report which indicates that the antibiotic oral erythromycin, sometimes used in treating otitis media, prolongs cardiac repolarization and is associated with case reports of torsades de pointes—a cardiac arrhythmia which causes blackouts. Worse, because erythromycin is ex tensively metabolized by cytochrome P–450 3A [CYP3A] enzymes, commonly used medications which inhibit the effects of CYP3A [nitromidazole antifungal agents, certain calcium-channel blockers, some antidepressants] increase plasma erythromycin concentrations which in turn increase the risk of ventricular arrhythmias with resultant risk of sudden death from cardiac causes. An elevation of sudden cardiac death that could be traced to erythromycin use was, in fact, actually observed in a Medicaid cohort of about 1.2M person-years of follow-up in the state of Tennessee. [118]
All of these findings clearly point out that the use of antibiotics does not come without consequences, the majority of which are unwanted, detrimental, and ultimately preventable if antibiotics are not used inappropriately.
4. The effectiveness of antibiotic use in treating otitis media has been questioned in the literature
Within the past decade, a reevaluation of a major clinical trial, a second clinical trial, and a meta-analysis all question the effectiveness of amoxicillin in managing middle-ear effusions. The reevaluation suggested that the antibiotic was not effective [119] and the meta-analysis suggested that to prevent one child from experiencing pain by 2–7 days after presentation, 17 children must be treated with the antibiotic early [suggesting only modest benefits]. [120] The remaining clinical trial not only echoed the findings of the metaanalysis but went so far as to suggest that "this modest effect does not justify prescription of antibiotics at the first visit, provided close surveillance can be guaranteed. [121]
One would imagine that, given this weak evidence regarding the capacity of the routine use of antimicrobials to decrease the duration and severity of otitis media, there should be cries for a revision of this policy. Indeed, requests for such reassessments have appeared recently in the scientific literature, [103] including a review and plea from the International Primary Care Network. [122]
5. The basis for prescribing antibiotics for pediatric problems may not be based upon scientific principles
To compound the problem of prescribing antimicrobials to treat nonbacterial conditions as suggested in item #1 above, a recent report suggests that when physicians merely thought that the parent wanted antimicrobials to treat their children's illnesses, physicians were significantly more likely to give a bacterial diagnosis. [123] The link between patients' expectations and physicians' prescribing responses has been extensively documented in the literature. [124–128] Patients do seem to expect antibiotics for prescriptions, and their satisfaction rises when these expectations are met. [129, 130] What is remarkable in these studies is how physicians' diagnostic capabilities as well as their prescriptive responses appear to have been influenced by their perceptions of patients' attitudes.
The question that one would pose in this circumstance is as disturbing as it is elementary: Are sound scientific principles being followed in the current paradigm of prescribing antibiotics?
To conclude, a substantial body of literature now exists to refute the contention that antibiotics should be prescribed as a first line of defense for the treatment of otitis media. It is only through the education of both patients and physicians that one would hope that more efficient, less expensive, and especially less invasive means are developed to manage the patient with otitis media.
TYMPANOSTOMY In certain instances with persistent otitis media with effusion, tympanostomy tubes have been inserted through the eardrum to attempt to reduce hearing loss caused by the accumulation of fluid or to attempt to lessen the frequency of recurrent bouts of otitis media. In 1988, some 670,000 surgeries were performed in the United States, making it the most common operation for children. [131–133]
It would appear that puncturing the eardrum by such an intervention should be a means of last resort. Potential complications of tube insertion would include prolonged otorrhea, persistent perforation of the tympanic membrane, and scarring of the tympanic membrane which may be associated with low-grade, long-term hearing loss. [131–136] The results from a variety of epidemiological studies have not been encouraging: one study found that one quarter of tube insertions for children were proposed for inappropriate indications and another third for equivocal ones; [137] another indicated that for children younger than three years of age with persistent otitis media, prompt tympanostomies did not measurably improve developmental outcomes. [138]
5. Infantile Colic and Constipation
Load the References in a separate window for easy viewing
First described in 1894 as dyspepsia, colic has acquired varying sets of diagnostic criteria to the present. The most widely accepted definition is the unexplainable and uncontrollable crying in babies from 0–3 months old, more than 3 hours a day, and more than 3 days a week for 3 weeks or more. This usually occurs in the afternoon or evening hours. [139] The crying is characterized by a higher frequency pitch, [140] and there is frequently motor unrest marked by the flexing of the knees against the abdomen, extension and straightening of the trunk and extremities, and clenching of the fists. Otherwise, the infants affected have been found to be healthy and thriving with normal weight gain. [139]
The incidence of colic among newborns averages 22.5% [ranging from 8–49%]. With 4,058,814 live births having been reported in the U.S. in 2000, [141] that would translate to 913,233 cases of colic every year. Despite the fact that colic has often been described as "benign" and "self-limiting," one observational study has indicated that more than half [53%] of colic cases persist beyond 3 months and that 12% of these continue beyond 6 months. [142] Even though the condition may appear to be short-lived, it runs the risk of damaging the mother-child relationship which could persist for up to 3 years after the disappearance of the symptoms of colic. [143, 144] This condition would also be expected to increase the risk of continuing ill treatment of the child and even death from being shaken. [140, 145]
The cause of colic remains unknown, as [a] radiological studies have shown that the amount of air in the intestines of colicky infants is the same as in normal babies; [139] [b] constriction of the intestines has not been found; [139] [c] gastrointestinal transit time is normal; [139] [d] intestinal hormones and microflora, fecal analysis, occult blood in the stools, hydrogen ion concentration in the breath, and markers of intestinal damage have all shown unremarkable characteristics in infants with colic. [139]
Later in childhood is the problem of chronic childhood constipation, which accounts for 3% of visits to general practitioners and almost 30% of visits to pediatric gastroenterologists. [146] In followup studies, 30–50% of these children continue to have symptoms many years after the initial diagnosis, [147] the symptoms in perhaps 30% being intractable. [147, 148] Contradicting the notion that childhood constipation disappears during puberty was a longitudinal study that revealed no such tendency. [149]
Large quantities of hard, dry feces in the descending colon due to the overabsorption of fluid are the hallmark of constipation. [150] Reduced frequency of defecation, hard stool consistency, and difficult or painful bowel movements are the clinical earmarks of constipation. [151, 152]
6. Nocturnal Enuresis
According to the Diagnostic and Statistical Manual of Mental Disorders, enuresis has been defined as the involuntary voiding of urine at least twice a month for children aged 5 and 6 and once a month for older children. The most common form of enuresis is nocturnal, in which urine is passed during sleep. [153] This condition is primary if the child has never been consistently dry for more than 1–2 weeks; in secondary enuresis, the child is seen to wet again after an extended period of dryness. [154] The primary form customarily begins by the age of 5, while the secondary variety is experienced between ages 5 and 8. [153]
Nocturnal enuresis is seen in about 15% of 5–year olds, 7% of 8–year olds, and 3% of 12–year olds [155] By the age of 18, it virtually disappears in girls and occurs in 1% of boys. [153] Overall, it is estimated that it affects 5–7 million children in the United States alone. [156]
7. Asthma
Load the References in a separate window for easy viewing
Asthma is described as a multifactorial condition characterized by spontaneous attacks of wheezing, dyspnea, thoracic constriction and labored breathing. [157] Mild onsets will display symptoms of tachypnea, tachycardia, and wheezing upon expiration, where as more severe forms will present increased breath sounds with pursed lips and the lack of expansion of the rib cage due to intercostal muscle constriction. [157] The hallmark is a thick, white mucous which is produced by the respiratory epithelium of the bronchi, creating an obstruction of the airways with considerable difficulty in breathing. [158]
Estimates of asthma occurrence indicate that it affects 4–5% of the general population in industrialized countries [159] and is the most common chronic disease of childhood. [160] In Australia, its prevalence among children has been calculated to a figure of 20% [161] with one estimate from Victoria running as high as 46%. [162] In the Australian population overall, there are reports that the mortality of asthma has increased from 400 deaths per year in 1979 to around 900 in 1990–with a similar trend having been observed in both the United States and United Kingdom. [163] Direct costs of treatment have ranged from $209 million in New South Wales in 1989 [163] to 400 million pounds in the United Kingdom as calculated by the National Health Service. [164] For children, the prevalence of asthma has been reported to increase more than 50% since 1980 and the mortality more than 70%. [165]
In the United States, the increase in asthma sufferers has risen 75% since 1980 to 1998, while the death rate for children during this period increased by 78%. The year 1995 alone produced 1.8 million visits to the emergency room for asthma. The Centers for Disease Control, in assessing this situation, believed that this problem was due to pollution and other environmental factors. [166]
B. Outcomes as Demonstrated by Research Reports:1. Back Pain:
Despite the wealth of studies regarding low-back pain outcomes in adult populations [167] and the fact that low back pain is the condition most frequently associated with chiropractic care, [168] there have been no con trolled trials to date on the outcomes of chiropractic treatment for low-back pain in pediatric and adolescent populations, according to searches on MEDLINE from 1987–2006 and MANTIS from 1992–2006. As shown ty Table 4, one cohort [169] and three case studies [170–172] involving spinal manipulation by a chiropractor have been reported.
TABLE 4: SUMMARY OF LEADING OUTCOMES STUDIES INVOLVING
SPINAL MANIPULATION FOR MANAGING BACK PAIN
AUTHOR DESIGN # SUBJ AGE INTERVENTION OUTCOMES RESULTS |
Hayden [169] Cohort 54 4–18 SMT Pain [VAS] 87% improved |
Likert 62% improved |
Hession [170] CASE 1 16 EMS Pain [VAS] 100% improved F–D SMT |
R SMT |
Kazemi [171] Case 1 14 S–P Mob ROM Can touch tibia |
I Current Tx Pain Pain Free |
Cryo Tx |
Lumbar traction |
S–P SMT |
Exercise |
IR Laser Tx |
King [172] Case 1 14 S–P SMT Radiating pain Pain free |
Soft tissue Tx Activity limited Unrestricted |
I Current Tx |
AIM |
Surgery
KEY:
EMS = Electrical Muscle Stimulation
F–D = Flexion-Distraction
R = Rotational
S–P = Side-Posture
I = Interferential
IR = Infrared
AIM = Anti-inflammatory medicationsThis gap in the pediatric low back pain literature fortunately has begun to be addressed with a more recent prospective study of consecutive pediatric patients with low-back pain seeking treatment from randomly selected chiropractors within the cities of Calgary, Alberta and Toronto, Ontario, Canada. Chiropractors were eligible to participate if they were in practice for a minimum of 5 years and saw a minimum average of two pediatric patients per week. A maximum of 5 consecutive cases between the ages of 4 and 18 with a new episode of mechanical low back pain [not previously treated by a chiropractor] were accepted. Low back pain was defined as pain or discomfort in the area bounded by the lowest set of ribs in the patient's back to the lower edge of the buttocks. A total of 15 chiropractors provided data on 54 patients, 61% of which were acute presentations and 47% relating to the onset of a traumatic event. All patients were followed until they reported resolution of the problem, discharge, referral, or discontinuation of treatment. Assessment of low back pain was accomplished by means of two indices: [i] the visual analog scale [VAS], and [ii] a subjective 5-point Likert scale. The mean VAS upon presentation was 5.6.
The most commonly used form of intervention was spinal manipulation, with 95% of follow-up visits including this therapy. Included in additional treatments were passive manual therapy, such as soft tissue treatmentsand mobilization and such modalities as interferential current and ultrasound. Just 7.7% of patients underwent active management, such as patient-directed home exercises, nutrition, and other education.
Within a 6-week course of management, "much improvement" [Grade 4 on the Likert scale] was attained in 62% of the patients, with a median time of 16 days. "Important improvement"" [Grade 3.8 on the VAS] was reported from 87% of the patients with a median time of 28 days. Patients with chronic low back pain were less likely to respond within the median number of treatments. [169]
Given the fact that chronic patients were less likely to respond and that relatively few practitioners employed active management strategies, it appeared to the authors that further education of chiropractors regarding this particular mode of treatment was indicated. Because there was no natural history comparison group, it is not possible to directly implicate cause and effect from this particular study. However, there does seem to be a clear implication that the majority of pediatric patients with low back pain [especially acute] respond positively to chiropractic treatment. [169]
The case studies, all addressing lumbar disc herniation experienced by adolescents, require our further attention. All clearly demonstrate the most prudent course of healthcare, beginning with the most conservative and least invasive modalities and progressing until a positive outcome is attained. [170–172] The study by Hession describes a progression from flexion-distraction to side-posture manipulation, with full recovery experienced by 8 weeks with no recurrence of complaints by 16 months after treatment. [170] Kazemi depicts a far more involved and lengthy course of treatments–all conservative–for 20 weeks, yielding a patient who is pain-free at one year of follow-up. What is even more remarkable is that the patient, a Tae Kwon Do martial artist, was clearly subjected to extreme physical challenge. [171] King's report describes an adolescent who begins treatment conservatively [even with a return referral from a neurosurgical consultation] but ultimately undergoes surgery for disc removal after just 3 weeks of visits to both chiropractic and allopathic providers. [172] Taken together, these three case studies cannot establish cause-and-effect but clearly give us an excellent blueprint as to how pediatric musculoskeletal conditions might best be managed by both the chiropractic and allopathic communities. It is also clear that further clinical research including the more controlled design of randomized clinical trials would add invaluable evidence to further support the chiropractic care of pediatric and adolescent populations with back pain.
2. Headache:
Despite the multiplicity of outcome studies for adults [173–177] which have gained recognition in a study conducted by Duke University and endorsed by the Agency for Health Research and Quality, [178] there have not been formally constructed manipulation outcome trials with pediatric populations. Rather, there have been numerous case studies and case series, a portion of which have appeared in the peer-reviewed journals. As shown in Table 5, tension-type, cervicogenic, and even migraine headache have been described with positive outcomes. [179–184] Lisi's investigation is noteworthy in that it reports that the cervicogenic headachefrequency decreased to just twice a month after only a single treatment. [184] Other than Hewitt's positive case repor, 180] no published outcome studies pertaining to neck and shoulder pain specifically in children could be located. For the present, the encouraging results of the adult clinical trials [173–177] can be interpolated and melded with the aforementioned positive pediatric case outcomes [179–184] to suggest that spinal manipulation in the treatment of pediatric headaches enjoys a base of evidence that cannot be ignored.
TABLE 5: CHIROPRACTIC TREATMENT OF PEDIATRIC HEADACHE
Author # Subj Age Diagnosis Diagnostic Procedues Adjustive Procedures |
Haney [179] 1 11 Subluxation X-ray, AK muscle Diversified |
Hewitt [180] 1 13 TTH Passive MP Diversified |
Kastner [181] 12 Unspecified TTH, M, U Unspecified Unspecified SMT |
Cochran [182] 1 10 M X-ray, MP Thompson, diversified |
Anderson- Peacock [183] 5 6–15 CEH [2] ROM, M [3] xray, MP Diversified |
Lisi [184] 1 8 CEH ROM, MP Diversified |
Modified rotary break |
Side posture mamillary push |
Myofasical release Legend:
CEH = cervicogenic headache;
M = migraine headache;
TTH = tension-type headache;
U = unspecific;
ROM = range of motion,
AK = applied kinesiology;
MP = motion palpation;
SMT = spinal manipulative therapy
3. Otitis Media:
Load the References in a separate window for easy viewing
Although still lacking a randomized clinical trial, arguably the strongest case for chiropractic intervention can be made for managing otitis media. To complement the prevalence, rationale and risks of medical alternatives outlined above in Section IV.A.4. are the results of large cohort and case studies shown in Table 6 supporting the effectiveness of manipulative therapy for treating this condition. [97, 100, 185–197] It can be seen that the majority of otitis media cases treated with spinal manipulation appear to be resolved within 10 days, most responding to fewer than 5 adjustments [100, 186] and many requiring only one or two treatments. [97, 185] Particularly intriguing is the fact that patients with no history of prior ear discomfort were much more likely to show early improvement, avoiding the cost and time of further interventions. [185] Normalization of otoscopic and tympanographic results likely occurred more quickly in cases of acute rather than chronic otitis media as shown in two studies. [100, 186] Fewer surgeries and episodes of acute otitis media were also encountered by patients undergoing osteopathic manipulative treatments. [187]
TABLE 6: SUMMARY OF LEADING OUTCOMES STUDIES INVOLVING
SPINAL MANIPULATION FOR MANAGING OTITIS MEDIA
AUTHOR DESIGN # SUBJ AGE INTERVENTION OUTCOMES RESULT |
Froehle [185] Cohort 46 <5 yr A SMT Parental decision 93% ep improved SOT AK Fallon Case series 332 [100] <5 yr RF Otoscopy Resolved 401 [186] D, G SMT Tympanography Resolved Phillips [97] Case 1 23 mo A SMT Ear drainage, pain Reduction Mills [187] RCT 57 6 mo RC AOM episodes Reduction 6yr RC + OMT Surgeries Reduction Tympanograms More normals Legend:
RC = Regular care,
OMT = Osteopathic manipulative therapy,
SMT = Spinal manipulative therapy,
A = Activator,
SOT = Sacro-occipital technique [occasionally],
AK = Applied kinesiology [occasionally],
D = Diversified,
G = Gonstead,
STE = Soft tissue effleurage,
RF = 3o rotation, 5o lateral flexion,
ep = Episodes
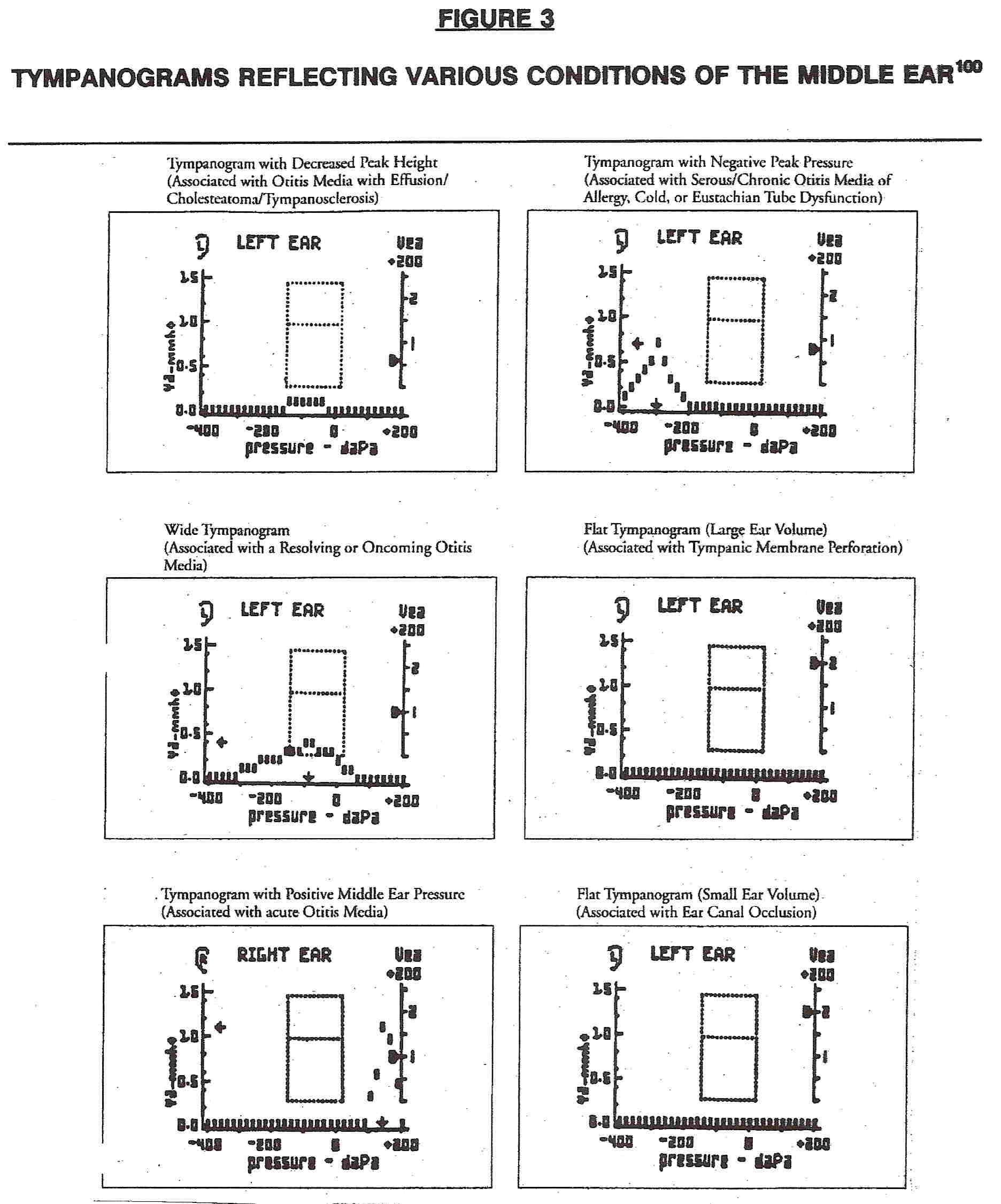
The importance of direct examination of the middle ear, such as outlined in extensive detail by a chiropractor who practices in the New York metropolitan area with frequent referrals to and from major hospitals in NewYork, [100] points out the variety of conditions that can be distinguished by tympanography. As shown by the tympanograms in Figure 3, it is possible to distinguish ear conditions which are most likely to respond to antibiotic treatment [positive peak pressure, brought on by purulent bacterial cultures] from those that are not [negative peak pressure, indicative of viral or serous effusions]. This stands in stark contrast to the questionable standards for ordering antibiotics outlined above (Section IV.A.4.c.1]), including the almost surreal bases sometimes chosen for prescribing antimicrobials, as published by Mangione-Smith and her colleagues in the journal Pediatrics. In that particular study, it was shown that physicians both prescribed antibiotics and diagnosed a bacterial origin largely from the mere anticipation of what they believed the parents of affected patients desired in their treatment. [123]
Mastoiditis [the chief complication of otitis media] occurs only 0.2–2% of the time, even without antibiotic treatment; [188] it behooves the physician to not only consider spinal manipulation as a treatment option for otitis media, but as a possible first alternative in light of the more rapid responses achieved in acute cases. Clearly, this strategy serves the patient well also in avoiding the complications attending the medical options discussed above. In none of the studies reported in Table 6 were any side effects or complications reported.
Other than the osteopathic report published by Mills, [187] data from a randomized clinical trial directly comparing the effectiveness of spinal manipulation to standard medical treatment have yet to appear in any of the refereed medical journals. This is an omission that hopefully will be resolved in the near future. In the meantime, there seems to be little reason to deny qualified chiropractors the opportunity to manage this extremely widespread condition with greater efficiency, an absence of side effects, and at lower cost.
4. Infantile Colic and Constipation:
To buttress years of promising clinical observations, a number of interventions have recently been conducted [Table 7], [189–193] with results that are mostly suggestive. All involve spinal manipulation either applied by fingertip or a computer-assisted solenoid adjusting device. What is most dramatic is the comparison shown with the surfactant dimethicone [Figure 4], which not only produced a considerably lesser effect from 5–10 days after the start of treatment, but showed worsening of symptoms as was apparent in 7 of the medicated group of patients. [189] While the effects of manipulation compared to a hand-held placebo group did not appear to differ statistically, a trend toward superiority in the numbers of patients affected is apparent. Furthermore, greater numbers of the manipulated group indicated "some" or "marked" improvement. [190] Other explanations as to why the latter study did not reveal a statistically significant effect in contrast to the former [in addition to their uses of different control groups] are the following: [i] the infant's mother was blinded; [ii] the former study required infants to cry for more than 3 hours for 5 of the previous 7 days rather than for 3 days per week in the previous 3 weeks; [iii] the intervention in the former study was slightly more intensive [3–5 adjustments over 14 days as opposed to 3 adjustments over 8 days]; and [iv] the latter study required two additional criteria for colic, which could have screened out individuals who displayed an enhanced response in the former investigation. A pilot randomized clinical trial suggested that the complete resolution of symptoms could be found in 93% of the subjects undergoing up to 6 treatment sessions over a 2-week period. [191] What remains unclear is whether Olafsdottir [190] adjusted areas of the spine that were different from the other two investigations, [189, 191] accounting for the differences in results.
TABLE 7: SUMMARY OF LEADING OUTCOMES STUDIES INVOLVING
SPINAL MANIPULATION FOR MANAGING INFANTILE COLIC
AUTHOR DESIGN # SUBJ AGE INTERVENTION OUTCOMES RESULT |
Wiberg [185] RTC 25 4–6 wk F SMT Crying [hrs] 70% drop in 5 days |
20 Dimethicone Crying [hrs] 20% drop in 5 days |
Olasfdottir [190] RTC 32 3–9 wk F SMT Symptom scale Improvement in 70% |
24 Held 10 min Symptom scale Improvement in 60% |
Mercer [191] RTC 15 0–8 wk SMT Parent diary 93% resolved, 2 wk |
15 Detuned ultrasound |
Klougart [192] Cohort 316 1–5 wk F SMT Crying [hrs] 75% drop in 14 days |
Leach [193] Case 2 6–9 wk I SMT Crying [hrs] 50% drop after 1–4x Legend:
F = Spinal manipulation applied with light fingertip pressure,
I = Instrument [PulStar FRAS Sense Technology, Inc.],
x = Number of treatments

While spinal manipulation is usually associated with the treatment of musculoskeletal disorders, these data create two possible interpretations. As indicated by Wiberg, [189] either spinal manipulation has been shown to be effective in the treatment of a visceral disorder or infantile colic is, in fact, a musculoskeletal disorder rather than the visceral condition it is assumed to be. In either case, these data provide a further basis to continue the use of spinal manipulation in treating specified pediatric conditions.
Supported by ONLY case studies at this writing, chiropractors have reported notable success in managing constipation in young children. As shown by Table 8, a wide variety of chiropractic interventions in children aged from 5 months to 8 years have resulted in significant improvements in this condition. [151, 194–196] Particularly noteworthy is the communication from Quist, which reports that the constipation which had plagued an 8-year old child since birth despite allopathic treatments with laxatives and high fluid and fiber intake was resolved after just 3 adjustments with massage. Bowel movements immediately became much more frequent and smaller and softer. After 8 more patient visits within a month, the patient was discharged and bowel function remained normal for at least 13 years after the completion of this course of care. [197]
TABLE 8: SUMMARY OF CASE STUDIES INVOLVING
SPINAL MANIPULATION FOR MANAGING CONSTIPATION
AUTHOR AGE INTERVENTION Hewitt [151] 7–month Full-spine, cranial Eriksen [194] 5–year Grostic upper cervical Marko [195] 10–month Chiropractic biophysics Quist [196] 8–year Diversified [drop adjustments], massage
5. Nocturnal Enuresis:
This condition has been described as having multifactorial origins. [197] It has been proposed that spinal joint dysfunction could disrupt the integration of somatic, spinal, parasympathetic and sympathetic nerve pathways–constituting a significant contribution to the patient's enuretic condition. Thus, a few clinical studies have appeared in the literature [198–200] and suggest that spinal manipulative therapy may play a role in managing this condition [Table 9].
While the majority of cases did not appear to respond in one of the studies, [199] it was felt that more information could have been obtained in the presence of a control group given a sham procedure in a randomized controlled trial. In that particular study, the manipulated group did indeed display a significant improvement over its own baseline values while the placebo group did not. However, the mean pre- to post-treatment night frequency group for the test group compared with that of the control group was not quite statistically significant at the 5% level. [199] A larger sample size would most likely have created a statistically robust difference between the groups. In addition, despite its minuscule n of 1 design, Gemmell's study displayed a time-series improvement following manipulation which defied the natural course of improvement. [200] The one trial that did indicate improvement utilized an adjusting technique developed at the Palmer College of Chiropractic. [201]
TABLE 9: SUMMARY OF LEADING OUTCOMES STUDIES
INVOLVING SPINAL MANIPULATION FOR MANAGING NOCTURNAL ENURESIS
AUTHOR DESIGN # SUBJ AGE INTERVENTION OUTCOMES RESULT |
Reed [198] RTC 31 8–11 yr P SMT Wet nights/2 wk 16% < baseline |
15 Sham 0% < basline |
LeBoeuf [199] Cohort 171 4–15 yr SMT Wet nights/wk 75% no response |
Gemmell [200] Case 1 14 yr T SMT Dry/damp/wet Trend to dryness Legend:
P = Spinal manipulation, Palmer Package Adjusting Technique [201],
T = Spinal manipulation, Toggle Recoil,
Sham = Activator at nontension setting
6. Asthma:
Load the References in a separate window for easy viewing
The typical control of asthma by medication is primarily through antiinflammatory agents [inhaled steroids] or beta-2-agonists [bronchodilators], the last of which when used excessively may actually contribute to an increase of mortality and morbidity. [202] There has thus been a shift toward using anti-inflammatory agents; at the same time, questions have been raised as to whether alternative and less invasive means are available for controlling this condition.
Spinal manipulation has been proposed as an option primarily for two reasons. The first is that vertebral dysfunctions assumed to underlie chiropractic management could produce reflex irritations of the somatic and autonomic nervous system; second, from both a neurological and biomechanical point of view, chestwall function or bronchial airway tone and/or responsiveness might be expected to be adversely affected by such a lesion–leading to a increased risk for an asthmatic attack. [203] Reduction or elimination of these joint aberrations might thus be expected to reduce the incidence of asthmatic events.
A third and perhaps central element to keep in mind is the stress response in the asthmatic. In the attempt to maintain homeostasis, bronchial hyperresponsiveness is the defining characteristic in asthma. What has been ignored for too long until very recently in asthmatic research is the role of the endocrine system; in particular, glucocorticoid secretion from the adrenal cortex in response to adrenocorticoid secretion from the anterior lobe of the pituitary. The role of the adrenal secretions in stress was first described by Hans Selye in 1936, [204] the connection between stressful events and increased cortisol levels being subsequently described. [205–207] The role of the hypothalamic-pituitary-adrenal [HPA] axis as the means by which close communication is established between the central nervous system, the immune system, and hormones–and the means by which this is related to stress and chiropractic has been elegantly presented by Morgan [208] and is depicted in Figure 5A, while Figure 5B indicates in more detail how corticosteroids are produced. [209] The point of this discussion is that interventions which control stress may have a significant palliative effect in the management of asthma, with cortisol appearing to be an important marker.

In terms of actual asthma management, there are some indications from randomized clinical trials that such interventions as acupuncture, yoga, hypnosis, and relaxation are beneficial as adjunctive measures in the management of chronic asthma. [210] A particularly elegant study by Tiffany Field has demonstrated that two groups of asthmatic children, aged 4–8 and 9–16, displayed profound changes in pulmonary functions, attitude and behavior scores, and cortisol levels following massage as compared to a noncontact control group. No other treatments were applied in addition to massage, nor were nighttime symptoms evaluated. [211]
In addition to descriptive or anecdotal data which have reported a positive clinical effect of spinal manipulation for asthma, [212–213] two randomized clinical trials and a cohort study as shown in Table 10 offer qualified support for spinal manipulative therapy in the management of this condition. Lung function improvements per se may not be detectable, [214–215] but quality of life scores improved by 10–28%, led by activity scale changes. [215] The largest randomized clinical trial to date which is attempting to compare different manipulative techniques in the management of asthma is currently underway in Australia; although data on symptoms, quality of life and distress are forthcoming in this study, preliminary cortisol measurements indicate that with manipulation [as opposed to simply visiting the treatment center], levels do decrease. [158] Immunoglobulin A, on the other hand, appears to increase in patients attending chiropractic centers; [158] this result is particularly noteworthy in that transient deficiencies of mucosal and salivary IgA have been shown to lead to the development of bronchial hyperresponsiveness and asthma. [216]
TABLE 10: SUMMARY OF LEADING OUTCOMES STUDIES
INVOLVING SPINAL MANIPULATION FOR MANAGING NOCTURNAL ENURESIS
AUTHOR DESIGN # SUBJ AGE INTERVENTION OUTCOMES RESULT |
Balon [214] RCT 38 7–16 yr D SMT +S PEF Small rise |
42 Sham FEV No change |
QOL Improved |
Bronfort [215] Cohort 22 6–17 yr SMT Dr PEF N.S. change |
12 FEV N.S. change |
QOL Significant rise |
Severity Significant drop |
Symptoms No change |
Ali [158] RTC 150 C AC |
c SF-36 |
h DASS |
w Cortisol SMT decreases |
IgA Centers increases Legend:
D = Spinal manipulation, Diversified,
S = Soft tissue techniques
Dr = Spinal manipulation with drop table,
PEF = Peak expiratory flow
FEV = Forced expiratory volume,
QOL = Pediatric Quality of Life Questionnaire
C = Treatment at centers,
c = Nontreatment at centers
h = Nontreatment at home,
w = Nonsymptomatic patients at home
AQ = Asthma questionnaire,
DASS = Depression and anxiety stress scale
The apparently negative study appearing in The New England Journal of Medicine, stating that "the addition of chiropractic spinal manipulation to usual medical care for four months had no effect on the control of childhood asthma," requires further comment. This statement was based upon the failure of active and sham manipulated patient groups aged 7 to 16 years to be differentiated in terms of their outcomes in both quality of life and airway function. What is indisputable is that there were major improvements from baseline to followup observed in each of the groups. [214] The problem arises when one considers what was actually done in the sham procedures. Prolonged applications to no less than 3 distinct anatomical areas [gluteal, scapular, cranial] to the patient were described. Admittedly, these were not high-velocity contact procedures, but this appears to obscure an important phenomenon. Two pieces of evidence strongly suggest that simple contact with patients through sham procedures may produce significant effects in terms of asthma relief. The first indicates that, with respect to the reflexive inhibition of the alpha-motoneuron pool in human subjects, sham and active manipulative procedures display little difference. This is to suggest that cutaneous receptors, muscle spindles, and joint mechanoreceptors individually or in concert are significantly affected by so-called sham procedures. [217] The second arises from the studies of Field [211] described above, in which low-force massage as opposed to no contact was sufficient to elicit a differential, beneficial response in overcoming asthma symptoms. This more than anything else should indicate that physical contact with the patient is sufficient to trigger a cascade of physiological changes, which Balon erroneously dismissed in the asthma study.
In this particular condition, the reader must take note that chiropractic extends beyond high-velocity, low amplitude adjustments. It encompasses a broad range of both high-velocity and low-force techniques together with ancillary procedures, many of which have obviously been embedded in the sham procedures described. In its attempt to craft a fastidious design, the Balon trial [214] appears to have missed the forest for the trees by attempting to portray the essence of chiropractic care as the lack of differentiation between the sham and manipulated experimental groups.
7. Retrolisthesis and Scoliosis:
The outcomes for the chiropractic management of these next two sections is of such a preliminary nature that a discussion of the epidemiology of the conditions addressed [retrolisthesis/scoliosis and neurological disorders] has been omitted. As shown by Table 11, very few outcome studies have yet been conducted regarding scoliosis, the obstacles to designing a clinical trial comparing the natural progression of spinal curvature to that seen after a particular intervention being formidable.
Reductions in retrolisthesis were apparent among the 49 consecutive chiropractic patients sampled in Plaugher's investigations. After patients with spondylolisthesis were excluded, patients with retrolisthesis were identified by means of a marking procedure on radiographs of good quality, comparing the positions of the anterosuperior and posterosuperior corners of adjacent vertebral bodies. [218] While Lantz' cohort study did not yield apparent changes after intervention, [219] questions have been raised regarding its [i] inclusion/exclusion/exclusion criteria of patients, [ii] dropouts, [iii] changes in subgroups that may have been overlooked, and [iv] whether there was sufficient statistical power to draw the conclusions reported.
With regard to the subgroup question, a complex reanalysis of Lantz' data by Menke painted a substantially more optimistic picture of responsiveness to chiropractic treatment. Menke indicated that the ratio of patients who improved to those who worsened in their scoliosis was at least 2:1 for the milder curves of 1° , 3°, and 5° as measured by two methods [Risser-Fergusson and Cobb]. Neither the numbers of treatments nor their durationwere associated with improvement. A measure of curve compression–the number of segments below the curve apex–served as a possible indicator of success in that three or fewer intra-apex segments were associated with improvement in scoliosis. The initial Cobb angle as a clinical predictor was not supported. Improvements could be attributed to either a transient type of scoliosis resolving on its own or [more likely] a subgroup of patients actually responding to manipulation. [220]
While cessation of back pain in scoliotic patients has been reported in case studies involving older patients under chiropractic care, [221] this particular outcome is underresearched and has yet to be evaluated in children and adolescents. Also, we need to know whether the progression of curvature observed in scoliosis is to any extent retarded or halted by chiropractic intervention.
TABLE 11: SUMMARY OF LEADING OUTCOMES STUDIES
INVOLVING SPINAL MANIPULATION FOR MANAGING SCOLIOSIS
AUTHOR DESIGN # SUBJ AGE INTERVENTION OUTCOMES RESULT |
Plaugher [218] Case series 49 NS G SMT Retrolisthesis 34% reduction |
Sacral base angle No change |
Cervical lordosis No change |
Cobb's angle No change |
Scapular base angle No change |
Lantz [219] Cohort 42 6–12 D, G SMT Cobb's angle No change |
Heel lifts |
Postural counseling |
Lifestyle counseling Legend:
G = Gonstead, D = Diversified
8. Neurological Disorders: Epilepsy, Autism,
and Attention Deficit/Hyperactivity Disorder:
Load the References in a separate window for easy viewing
Given that the activation of neuronal receptors in the spine might lead to vagus nerve stimulation, known to have antiepileptic effects, [222] it is conceivable that spinal manipulation could limit seizure spread in a particular region of the brain. Numerous case reports of positive effect of manipulation abound in the literature, with one study indicating positive results in all 15 patients administered upper cervical manipulation, [223] and others pertaining to favorable outcomes in individual children in case studies. [224, 225]
A variety of encouraging responses of children with autism having undergone an assortment of manipulativeinterventions have also been reported. [226, 227] Finally, reversal of symptoms associated with attention-deficit hyperactivity have been reported from several children undergoing chiropractic adjustments, with or without nutritional supplements. [228, 229] While these are clearly harbingers to spur further, more rigorous research efforts, the reader must bear in mind that the level of evidence for these neurological disorders is at the present anecdotal only, nor are spinal manipulations yet indicated to replace current and more widely accepted means of treatment. The fact remains that observations such as these warrant further investigation rather than being categorically barred for childhood conditions which remain refractory to conventional medical treatment. It is only with closer investigation that particular strengths and limitations of any proposed healthcare intervention, including chiropractic healthcare, may be properly assessed.
C. Positioning the Chiropractic Practitioner1. Physical Attributes and Applications:
To bring all this research information into today's setting, however, what is that chiropractors have to offer? To begin, in many locales, chiropractic care has been firmly established for children. Both the Kentuckiana and Oklahaven Center are dedicated treatment centers for children with a full spectrum of conditions. [230, 231] In the Boston area, for example, a cross-sectional descriptive survey of 90 chiropractors revealed that each averaged 13 visits per week from children and adolescents, ranging from 1 to 3 visits weekly for each patient. An estimated 420,000 pediatric visits to chiropractors were made in the Boston area in 1998 at a cost of approximately $14M. [232] In Canada, a survey of 1200 practitioners reveals that almost all are to some degree involved in treating patients under the age of 18. [233]
Regarding musculoskeletal care, chiropractors have taken the offensive in counselling parents and schoolchildren on how to avoid the injuries caused by backpacks, as discussed above in Section IV.A.1. [234–236] The American Chiropractic Association, in particular, provides a checklist of items to assure that the best possible backpack is chosen for children and adolescents: [237]
Is the backpack the correct size for the child?
The backpack should never be wider or longer than the child's torso, and it should not hang more 4 inches below the waistline. A backpack that hangs too low increases the weight on the shoulders, causing the child to lean forward while walking.
Does the backpack have two wide, padded shoulder straps?
Non-padded straps are not only uncomfortable, but also they can place unnecessary pressure on the neck and shoulder muscles.
Does the child use both straps?
Lugging a heavy backpack by one strap can cause a disproportionate shift of weight to one side, leading to neck and muscle spasms, low-back pain and poor posture.
Are the shoulder straps adjustable?
The shoulder straps should be adjustable so that the backpack can be fitted to the child's body. The backpack should be evenly centered in the middle of the child's back.
Does the backpack have a padded back?
A padded back not only provides increased comfort, but also protects the child from being poked by the sharp edges of school supplies [such as pencils, rulers, and notebooks] inside the pack.
Does the pack have several compartments?
A backpack with individualized compartments helps position the contents most effectively. Make sure that pointy or bulky objects are packed away from the area that will rest on the child's back, and try to place the heaviest items closest to the body.In terms of preventive measures overall, a study of 88 Norwegian adolescents aged 14–16 has shown that low extension strength is strongly correlated with the development of low-back pain 3 years later. Thus, a preventive measure might be to encourage low-back strengthening exercises, but not activities which simply increase mobility. [238] A second investigation describes the presentation of 11 sessions on correct postural behaviors to a subgroup of 106 third-grade students, the remaining groups either educated on health related themes or receiving no related education at all. The postural behavior instructions included lifting and bending activities at the pupils' homes, classrooms, and physical education classes. In addition to demonstrating far superior posture habits, the experimental group at four years follow-up were found less likely to have developed back problems. [43]
Postural education efforts have been taken a step further with the release of a program in 2003 by Ronald Kirk of a program known as Straighten Up America. [239, 240] This public awareness effort seeks to:
(1) improve posture and function;
(2) to stabilize core musculature;
(3) to enhance spinal and neurological health; and
(4) to prevent spinal subluxations.
Straighten Up America has cooperated with the United States Bone and Joint Decade and is a 50th Anniversary Partner with Get America Moving, an initiative of the President's Council on Physical Fitness and Sports which observed its 50th anniversary in 2006. It maintains a public service website in conjunction with the Congress of Chiropractic State Associations and Life University. The lifestyle choices which it urges both children and adults to follow are shown in Figure 6, with specific exercises for children recommend directly on the program's website. [240]
Separate from posture and musculoskeletal problems is the entire issue of childhood obesity, known in studies in western industrial countries to be rapidly increasing. From 1984 to 1996–1997 to 2003, for instance, the prevalence of obesity in caucasian children in the United Kingdom aged 5–10 years has risen from 1.2% to 3.0% to 6.0%, while in girls it has jumped from 1.8% to 4.5% to 6.6%. [241] In the U.S. for children, the trend for overweight occurrence from 1988–1994 to 1999–2000 was 10.5% to 15.5% for 12–19 year olds, 11.3% to 15.3% for 6–11 year olds, and 7.2% to 10.4% for 2–5 year olds. [242] This trend has extended at least to China and Brazil as well. [243] The cardiovascular risk factors for obesity are well known, pertain directly to children, yet can be reversed with intervention, [244] for which chiropractors have been shown to be well-positioned. [245]
A variety of measures advocated by chiropractors and others which are commensurate with a preventive paradigm of health care rather than a disease-oriented one has been advocated in a recent journal publication from one of the chiropractic institutions. [245] It points out that children should not be dieting to reduce weight but rather should be directed to maintain their current weight with an increase of physical activity, as they are still in a growing stage. [246]
2. Chiropractic Paradigms As Guiding Principles:
What is essential to keep in mind is that all these strategies for the practice of preventive health for children and adolescents are simply manifestations of what are widely regarded as the tenets of a paradigm of healthcare universally embraced by the chiropractic profession. It is distinctly different from the current disease-oriented model of healthcare which has been found to be lacking to the point of requiring an extensive overhaul if healthcare is to be adequately delivered to the world's population in the next century. [247, 248]
Traditional chiropractic has always viewed the patient as the center of healthcare, the patient's interest taking precedence over all. By influencing function through structure, [249] chiropractic care has embraced a multiplicity of elements identified as vitalism, holism, naturalism, humanism, conservatism, and rationalism. [250–252] Essentially, the profession and the practitioner are positioned as taking a proactive position in healthcare, attempting to move closer to presumed causes of dysfunction and ill health and thus emphasizing preventive measures.
This orientation is perhaps best articulated by the paradigm adopted in 1996 by the Association of Chiropractic Colleges, designed to identify chiropractors on a course no less significant than the Hippocratic Oath does for allopathic medicine. The position of the drafting body of this document can be best understood by the following excerpt:"Chiropractic is a health care discipline that emphasizes the inherent recuperative power of the body to heal itself without the use of drugs or surgery. The practice of chiropractic focuses on the relationship between structure [primarily the spine] ad function [as coordinated by the nervous system] and how that relationship affects the preservation and restoration of health. In addition, Doctors of Chiropractic recognize the value and responsibility of working in cooperation with other health care practitioners when in the best interest of the patient."
The chiropractic paradigm itself, as expressed by the ACC, includes:
Purpose: The purpose of chiropractic is to optimize health.
Principle: The body's innate recuperative power is affected by and integrated through the nervous system.
Practice: The practice of chiropractic includes:
Establishing a diagnosis;
Facilitating neurological and biomechanical integrity through appropriate chiropractic care management; and "Promoting health". [253]
V. SAFETY:
Load the References in a separate window for easy viewing
The best documented reports indicate that the risk of serious events which result from chiropractic treatment range from 1 in 400,000 [254] to 1 in 5.85 million [255] cervical spine manipulations, with the risk of lumbar complications at 1 per 100 million manipulations. [256] For pediatric populations, the most comprehensive database to date comes from a comprehensive search of 8 major electronic databases including MEDLINE, AMED, and MANTIS from inception to June 2005. It identified a total of 14 cases attributable to intervention and an additional 20 cases related to delayed or missed diagnoses. [257] It is clear from these figures that the risk estimates for pediatric manipulations would be substantially below the 400 deaths per million attributable to the use of NSAID medications, [258] the 700 deaths per million occurring with spinal surgery, [259] the 40 deaths per million seen with venipuncture, [260] or the 13,500 deaths per million reported for appendectomies. [261]
The serious adverse events include subarachnoidal hemorrhage and/or paraplegia [10 cases] and such minor or moderate occurrences as headache or mid-back soreness. Since this was passive surveillance only, a more accurate prospective population-based active surveillance study is needed. [257] A variety of flaws found in this systematic review have compromised its validity to the extent that numerous rebuttals have been written. One such rebuttal [my own] has been provided in Appendix I
VI. CONCLUDING REMARKS:
Issues regarding the controversies surrounding childhood vaccinations have been capably summarized elsewhere [262] and are beyond the scope of this discussion. The same situation applies to childhood birth trauma. [263] One matter worth mentioning is the recent demonstration that expanding, then removing the mercury preservative thimerosal from pediatric vaccines has been positively correlated with both the increase and then the decrease of both autism and speech disorders. [264]
Evidence from many different types of experimental designs [basic and clinical, the latter comprised of randomized controlled trials and cohort and case studies] has been emerging at a rapid rate over the past two decades and provides a promising basis with which to consider chiropractic management for such childhood conditions as otitis media, colic, enuresis, asthma, and various neurological disorders. Denial of this treatment represents no less than the suppression of important medical information (which in at least one state has been ruled to be a form of medical negligence [265]). Because the frequency of serious side effects associated with spinal manipulation has been reported to be exceedingly low, [258] our continued use and further inquiry into the more detailed aspects of this type of therapy does not appear to constitute any particular health risk to the patient–certainly not any greater and decidedly less than some of the medical side-effects presented in this discussion.
In our review of child healthcare based upon evidence, it is interesting to note that the dosage rates of medications in allopathic medicine for children are routinely calculated from body surface areas, merely representing scaled-down versions of the adult formularies. [266, 267] Direct evidence from outcome studies involving medications and children appears to be lacking. In striking contrast are the manipulative procedures given to children, which as Biedermann had stated at the beginning of this report are not at all simply proportional reductions of the techniques applied to adults. [31, 34] From the evidence at hand, therefore, excluding chiropractic management as a treatment option for infants and children would seem to egregiously violate the overarching principle of providing meaningful risk/benefit ratios of treatment alternatives to the patient, which should be the hallmark of any credible and viable medical practice.
Appendix I: Response To Systematic Review on Pediatric Safety
Safety issues surrounding spinal manipulation have received much attention in recent years. However, there has been very little discussion of this topic as it applies to pediatric patients. A new review recentty published in the journal Pediatrics [257] addresses this very concern, in what has been labelled as a “systematic review”. This is supposed to mean that all the published material In the medical journals been retrieved, with specific articles having passed certain criteria for their more intensive review and analysis.
Because this approach has not been previously followed for pediatric populations who have experienced spinal manipulation, this study pursues an important goal in today's world of assessing risks and benefits of all medical interventions. It also avoids a common limitation in reviews of this type, in that it embraces case and cohort studies which occur in live doctors' offices as well as clinical trials.
Described in the 13 papers accepted for review are 14 cases of direct adverse events following spinal manipulation. These include 9 cases of serious events [subarachnoidal hemorrhage and paraplegia], 2 moderately adverse events requiring medical attention [severe headache], and 3 minor occurrences [mid-back soreness]. Another 20 cases of indirect adverse events involved delayed diagnosis or the inappropriate provision of spinal manipulation for such serious medical conditions as meningitis or rhabdomyosarcoma.
It is both important and commendable that these events have been brought to light In Vohra's report. However, they must be viewed in the larger framework of three factors:(1) the total number of treatments administered to children;
(2) the relative risks of medical procedures for the same conditions treated; and
(3) the benefits of spinal manipulation in children which have been amply described in the research literature. Lacking these considerations, this review presents a distorted and one-sided assessment of pediatric spinal manipulation.
Unfortunately, the review by Vohra falls short of its goals in its pursuits:
Important studies involving pediatric patients who have successfully undergone spinal manipulation in resolving their complaints of ear infections [otitis media] have gone unnoticed.
Another study in which the authors attribute adverse events to chiropractors in the United States instead involves physical therapists, most likely practicing in Germany.
Yet another citation of adverse events occurring in a clinical trial describes nothing more than a short period of mid-back soreness and irritability, difficult to distinguish from a period of extended crying in another subject who was not even manipulated but was instead assigned to the placebo group.
A final group of patients suffered from delayed diagnosis— which the authors erroneously attribute to one study that made no such mention of diagnoses at all, but rather focused upon the direct consequences of manipulation per se.
So, the question remains whether the authors have truly accomplished their minimaI objective. Did they actually present an accurate and balanced assessment of the literature addressing the adverse events associated with spinal manipulation? The answer appears to be in the negative.
It is also not at all clear whether all the spinal manipulations described were in fact administered by qualified chiropractors, an important consideration when one considers the risks involved with individuals who have not received complete training in manipulating areas of the neck. Only when the following criteria are met will a truly “accurate and balanced” assessment of the scientific literature have been made:
The precise maneuvers applied to the patient;
The complete qualifications of those administering these treatments;
The several benefits of manipulations of the cervical area which in the literature have been shown to include the relief of headache, carpal tunnel syndrome, otitis media, colic, and enuresis (bed-wetting).
None of these standards have been met by Vohra's review, such that it can only be greeted with extreme skepticism.
REFERENCES:
1 Wedderkopp N, Leboeuf-Yde C, Andersen LB, Froberg K, Hansen HS.
Back Pain Reporting Pattern in a Danish Population-based Sample of Children and Adolescents
Spine (Phila Pa 1976). 2001 (Sep 1); 26 (17): 1879–1883 .
2 Viry P, Creveuil C, Marcelli C.
Nospecific back pain in children: A search for associated factors in 14-year old schoolchildren.
Review of Rheumatology [English Edition] 1999; 66(7-9): 381-388.
3 Balague F, Troussier B, Salminen JJ.
Non-specific low back pain in children and adolescents: Risk factors.
European Spine Journal 1999; 8(6): 429-438.
4 Olsen TL, Anderson RL, Dearwater SR, Kriska AM, Cauley JA, Aaron DJ, LaPorte RE.
The epidemiology of low back pain in an adolescent population.
American Journal of Public Health 1992; 82(4): 606-608.
5 Taimela S, Kujala UM, Salminen JJ, Viljanen T.
The prevalence of low back pain among children and adolescents: A nationwide, cohort-based questionaire survey in Finland.
Spine 1997; 22(10): 1132-1136.
6 Korovessis P, Koureas G, Zacharatos S, Papazizis S.
Backpacks, back pain, sagittal spial curves and trunk alignments in adolescents: A logistic and multinomial logistic analysis.
Spine 2005; 30(2): 247-255.
7 Limon S, Valinsky LJ, Ben-Shalom Y.
Children at risk: Risk factors for low back pain in the elementary school environment.
Spine 2004; 29(6): 697-702.
8 Sheir-Neiss GI, Kruse RW, Rahman T, Jacobson LP, Peli JA.
The Association of Backpack Use and Back Pain in Adolescents
Spine 2003; 28(9): 922-930.
9 Skaggs DL, Early SD, D'Ambra GP, Tolo VT, Kay RM.
Back pain and backpacks in school children.
Journal of Pediatrics and Orthopedics 2006; 26(3): 338-363.
10 Wall EJ, Foad SL, Spears J.
Backpack and back pan: Where's the epidemic?
Journal of Pediatrics and Orthopedics 2003; 23(4): 437-439.
11 Chow DH, Ng XH, Holmes AD, Chang JC, Yao RY, Wong MS.
Effect of backpack loading on the pulmonary capacities of normal schoolgirls and those with adolescent idiopathic scoliosis.
Spine 2005; 30(21): E649-E654.
12 Ehrmann-Feldman D, Shrier I, Rossignol M, Abenhaim L.
Risk factors for the development of neck and upper limb pain in adolescents.
Spine 2002; 27(2): 523-528.
13 Barea LM, Tannhauser M, Rotta NT.
An epidemiologic study of headache among children and adolescents of South Brazil.
Cephalalgia 1996; 16(8): 545-549.
14 Antoniuk S, Kuzak MF, Michelon L, Montemor Netto MR.
Prevalence of headache in children of a school in Curitiba, Brazil comprising data from children and parents.
Arg Neuropsiquiatr 1998; 56(4): 727-733.
15 Croteau N, Hai V, Pless B, Infante-Rivard C.
Trends in medical visits and surgery for otitis media among children.
American Journal of Diseases of the Child 1990; 144(5): 535-538.
16 Schappert SM.
Office visits for otitis media: United States.
Vital and Health Statistics of the Centers for Disease Control 1992; 214: 1-18 [National Center for Health Statistics].
17 Pitkaranta A, Jero J, Arruda E, Virolainen A, Hayden FG.
Polymerase chain-reaction based detection of rhinovirus, respiratory syncytial virus, and coranovirus in otitis media with effusion.
Journal of Pediatrics 1998; 133(3): 390-394.
18 Cantekin EI, McGuire Tw, Griffith TL.
Antimicrobial therapy for otitis media with effusion ["secretory" otitis media].
Journal of the American Medical Association 2991; 266(23): 3309-3317.
19 Kleinman LC, Kosecott J, Dubois RW, Brook RH.
The medical appropriateness of tympanostomy tubes proposed for children younger than 16 years in the United States.
Journal of the American Medical Association 1994; 271(16): 1250-1255.
20 Falkow S, Kennedy D.
Antibiotics, animals, and people--again!
Science 2001; 291: 397.
21 Le CT, Freeman DW, Fireman BH.
Evaluation of ventilating tubes and myringotomy in the treatment of recurrent or persistent otitis media.
Pediatric Infectious Disease Journal 1991; 10(1): 2-11.
22 Wiberg JMM, Nordsteen J, Nilsson N.
The Short-Term Effect of Spinal Manipulation in the Treatment of Infantile Colic:
A Randomized Controlled Clinical Trial with a Blinded Observer
Journal of Manipulative and Physiological Therapeutics 1999; 22(8): 517-522.
23 Leach RA.
Differential Compliance Instrument in the Treatment of Infantile Colic: A Report of Two Cases
Journal of Manipulative and Physiological Therapeutics 2002; 25(1): 58-62.
24 Bennet-Johnson S. Enuresis: In Daltzman RJ [ed.].
Clinical Behaviour Therapy and Behaviour Modification
New York, NY: Graldn SPM Press, 1980, pp. 80-141.
25 Young DE, Young RR.
Nocturnal enuresis: A review of treatment approaches.
American Family Physician 1985; 31: 141-144.
26 Centers for Disease Conrol and Prevention.
Asthma mortality and hospitalization among children and young adults: United States, 1980-1993.
Morbidity and Mortality Weekly Report 1996; 45: 350-353.
27 Gergen PJ, Weiss KB.
Changing patterns of asthma hospitalization among children, 1979 to 1987.
Journal of the American Medical Association 1990; 264: 1688-1692.
28 Cropp GJ.
Special features of asthma in children.
Chest 1985; 87: 55S-62S.
29 Spiegelblatt L, Laine-Ammara G, Pless IB, Guyver A.
The use of alternative medicine by children.
Pediatrics 1994; 94(6): 811-814.
30 Gazarian M.
EBP in practice: Pediatrics.
Medical Journal of Australia 2001; 174(11): 586-587.
31 Biedermann H.
Manual therapy in children: With special emphasis on the upper cervical spine.
In Vernon H [ed]. The Cranio-Cervical Syndrome. Oxford, UNITED KINGDOM: Butterworth Heinemann, 2001, pp. 207-230.
32 Valk J. et al.
The role of imaging modalities in the diagnosis of posthypoxic-ischaemic and haemorrhagic conditions of infants.
Klin Neuroradiology 1991; 2: 83-140.
33 Lierse W, Das Becken. In Wachsmuth VL. Praktische Anatomie.
New York, NY: Springer-Verlag, 1984.
34 Biedermann H.
Manual Therapy in Children: Proposals for an Etiologic Model
Journal of Manipulative and Physiological Therapeutics 2005; 28(3): e1-e15.
35 Plaugher G.
Clinical anatomy and biomechanics of the spine.
In Plaugher G [ed], Textbook of Clinical Chiropractic: A Specific Biomechanical Approach. Baltimore, MD: Williams & Wilkins, 1993, pp. 12-51.
36 Phillips CJ. Craniosacral therapy.
In Anrig C, Plaugher G [eds], Pediatric Chiropractic. Baltimore, MD: Williams & Wilkins, 1998, pp. 424-454.
37 St Claire SM, Picardi RJ.
Pediatric nutriton.
In Anrig C, Plaugher C [eds], Pediatric Chiropractic. Baltimore, MD: Williams & Wilkins, 1998, pp. 455-465.
38 Liossi C.
Psychological interventions for acute and chronic pain in children.
Pain Clinical Updates 2006; 14(4): 1.
39 Ross DM, Ross A.
Childhood pain: Current issues, research, and management.
Baltimore, MD: Urban & Schwarzzenberg, 1988.
40 Schechter NL, Berde CB, Yaster M [Eds.],
Pain in Infants, Children, and Adolescents, 2nd edition.
Philadelphia, PA: Lippincott, Williams and Wilkins, 2003.
41 Finley GA, Franck LS, Gronau RE, von Baeyer CL.
Why children's pain matters.
Pain Clinical Update 2005; 13(4): 1-6
42 McGrath PA. Children--Not simply "Little adults."
In Merskey H, Loeser JD, Dubner R [Eds.] The Paths of Pain, 1975-2005. Seattle, WA: IASP Press, 2005, pp. 443-446.
43 Mendez FJ, Gomez-Conesa A.
Postural hygiene program to prevent low back pain.
Spine 2001; 26(11): 1280-1286.
44 Grantham VA.
Backache in boys--a new problem.
Practitioner 1977; 218(1304): 226-229.
45 Watson KD, Papageorgiou AC, Jones GT, Taylor S, Symmons DPM, Silman AJ, Macfarlane GJ.
Low back pain in schoolchildren: Occurrence and characteristics.
Pain 2002; 97(1-2): 87-92.
46 Burton AK, Clarke RD. McClune TD, Tellotson KM.
The natural history of low-back pain in adolescents.
Spine 1996; 21: 2323-2328.
47 Balague F, Dutoit G, Waldburger M.
Low back pain in schoolchildren: An epidemiological study.
Scandinavian Journal of Rehabilitative Medicine 1988; 20(4): 175-179.
48 Hestbaek L, Lebouef-Yde C, Kyvik O, Vach W, Russell MB, Skadhauge L, Svendsen A, Manniche C.
Comorbidity with low back pain: A cross-sectional population-based survey of 12- to 22-year-olds.
Spine 2004; 29(13): 1483-1491.
49 Cakmak A, Yucel B, Ozyalcin SN, Bayraktar B, Ural HI, Durouz T, Genc A.
The frequency and associated factors of low back pain among a younger population in Turkey.
Spine 2004; 29(14): 1567-1572.
50 El-Metwayy A, Salminen JJ, Auvinen A, Kautianen H, Mikkelsson M.
Prognosis of non-specific musculoskeletal pain in preadolescents: A prospecive 4-year follow-up study till adolescence.
Pain 2004; 550-559.
51 Hakala P, Rimpelä A, Salminen JJ, Virtanen SM, Rimpelä M.
Back, Neck, and Shoulder Pain in Finnish Adolescents: National Cross Sectional Surveys
British Medical Journal 2002 (Oct 5); 325 (7367): 743–745
52 Salminen JJ, Erkintalo MO, Pentti J, Oksanen A, Kormano MJ.
Recurrent low back pain and early disc degeneration in the young.
Spine 1999; 24(13): 1316-1321.
53 Ancaster News, September 1, 2006:
www.ancasternews.com/an/news_65044.html. Downloaded 09/08/06.
54 Macias BR, Murthy G, Chambers H, Hargens AR.
High contact pressure beneath backpack straps of children contributes to pain.
Archieve of Pediatric and Adolescent Medicine 2005; 159(12): 1186-1187.
55 Moeller JL, Rifat SF.
Spondylolysis in active adolescents: Expediting return to play.
The Physician and Sportsmedicine 2001; 29(12).
56 Harreby MS, Neergaard K, Hesselsoe G, Kjer J.
Are low back pain and radiological changes during puberty risk factors for low back pain in adult age? A 25-year prospective cohort study of 640 school children.
Ugeskr Langer 1997; 159(2): 171-174 [In Danish].
57 Harreby MS, Neergaard K, Hesselsoe G, Kjer J.
Are radiological changes in the thoracic and lumbar spine risk factors for low-back pain in adults? A 25-year prospective study of 640 school children.
Spine 1995; 20(21): 2298-2302.
58 Croft PR, Macfarlane GJ, Papageorgiou AC, Thomas E, Silman AJ.
Outcome of low back pain in general practice: A prospective study.
British Medical Journal 1998; 316: 1356-1359.
59 Reis S, Hermoni D, Borkan JM, Biderman A, Tabenkin C, Orat A.
A new look at low back complaints in primary care: A RAMBAM Israeli family practice research network study.
The Journal of Family Practice 1999; 48(4): 299-303.
60 McGorry RW, Webster BS, Snook SH, Hsiang SM.
The relation between pain intensity, disability, and the episodic nature of chronic and recurrent low back pain.
Spine 2000; 25(7): 834-841.
61 Diepenmaaat AC, van der Wal MF, de Vet HC, Hirasing RA.
Neck/shoulder, low back and arm pain in relation to computer use, physical activity, stress, and depression among Dutch adolescents.
Pediatrics 2006; 117(2): 412-416.
62 Ehrmann Feldman D, Shrier I, Rossignol M, Abenhaim L.
Risk factors for the development of neck and upper limb pain in adolescents.
Spine 2002; 27(5): 523-528.
63 Hakala PT, Rimpela AH, Saami LA, Salminen JJ.
Frequent computer-related activities increase the risk of neck-shoulder and low back pain in adolescents.
European Journal of Public Health 2006; 16(5): 536-541.
64 Navuluri N, Navuluri RB.
Study on the relationship between backpack use and back and neck pain among adolescents.
Nursing Health Science 2006; 8(4): 206-215.
65 Grimmer K, Nyland L, Milanese S.
Repeated measures of recent headache, neck and upper back pain in Australian adolescents.
Cephalalgia 2006; 26(7): 843-851.
66 Barea LM, Tannhauser M, Rotta NT.
An epidemiologic study of headache among children and adolescents of South Brazil.
Cephalalgia 1996; 16(8): 545-549.
67 Antoniuk S, Kuzak MF, Michelon L, Montemor Netto MR.
Prevalence of headache in children of a school in Curitiba, Brazil comprising data from children and parents.
Arg Neuropsiquiatr 1998; 56(4): 727-733.
68 Bandell-Hoekstra IENG, Abu-Saad HH, Passchier J, Fredericks CMA, Feron KLM, Knipschild P.
Preponderance and characteristics of headache in Dutch school children.
European Journal of Pain 2001; 5: 145-153.
69 Aromaa M, Rautava P, Helenius H.
Factors of early life as prediction of headaches in children at school entry.
Headache 1998; 38(1): 23-30.
70 Anttila P, Metsahonkala L, Lillanpaa M.
School start and occurrence of headache.
Pediatrics 1999; 103(6): e80.
71 Antilla P, Metsahonkala L, Aromaa M, Sourander A, Salminen J, Helenius H, Alanen P, Silanpaa M.
Determinants of tension-type headache in children.
Cephalalgia 2002; 22(5): 401-408.
72 Brattberg G, Wickman V.
[Longitundinal study of school children: Rehabilitate early with back and head pain].
Lakartidninen 1993; 90(15): 1452-1460.
73 Leonardsson-Hellgren M, Gustavsson UM, Lindbland U.
Headache and assocation with lifestyle among pupils in senior level elementary school.
Scandinavian Journal of Primary Health Care 2001; 19(2): 107-111.
74 Larsson B, Sund AM.
One-year incidence, course, and outcome predictors of frequent headaches among early adolescents.
Headache 2005; 45: 684-691.
75 Koenig MA, Gladstein J, McCarter RJ, Hershey AD, Wasiewski W.
Chronic deaily headache in children and adolescents presenting to tertiary headache clinic.
Headache 2002; 42: 491-500.
76 Wiendels NJ, van der Gues MCM, Neven AK, Ferrari MD, Laan LAE.
Chronic daily headache in children and adolescents.
Headache 2005; 45: 678-683.
77 Laurell K, Larsson B, Eeg-Olofsson O.
Headache in schoolchildren: Association with other pain, family history and psychosocial factors.
Pain 2005; 119: 150-158.
78 Anttila P, Sourander A, Metsahonkala L, Aromaa M, Helenius H.
Psychiatric symptoms in children with primary headache.
Journal of the American Academy of Child and Adolescent Psychiatry 2004; 43: 412-419.
79 Bondy J, Berman S, Slazner J, Lezotte D.
Direct expenditures related to otitis media diagnoses: Extrapolations from a pediatric Medicaid cohort.
Pediatrics 2000; 105: E72.
80 Alsarraf R, Jung CJ, Perskins J, Crowley C, Alsarraf NW, Gates GA.
Measuring the direct and indirect costs of acute otitis media.
Archives of Otolaryngology, Head and Neck Surgery 1999; 125(1): 12-18.
81 National Center for Compementary and Alternative Medicine.
A randomized controlled trial of the use of craniosacral osteopathic manipulative treatment and of botanical treatment in recurrent otitis media in children.
http://clinicaltrials.gov/ct2/show/NCT00010465?term=craniosacral+osteopathic+manipulative+treatment+AND+recurrent+otitis+media&rank=1
Downloaded 09/11/02.
82 Casselbrant ML, Mandel EM. Epidemiology.
In Rosenfeld RM, Bluestone CD [Eds.].
Evidence-Based Otitis Media. Hamilton, Ontario, CANADA: BC Decker, 1999, pp. 117-136.
83 Daly KA, Casselbrant ML, Hoffman HJ, Ingyarsson LB, Kvaener KJ, Tos M, van Cauwenberge PB.
Recent advances in otitis media 2. Epidemiology, natural history, and risk factors [review].
Annals of Otolaryngology, Rhinology, and Laryngology Supplement 2002; 188: 19-25.
84 Adam D, Ehrlich GD.
Otitis media: Prospects for management.
Royal Turnbridge Wells, Kent, UNITED KINGDOM: Wells Medical Limited, 1996. Chapel Place International Clinical Practice Series.
85 Hurst DS.
Association of otitis media with effusion and allergy as demonstrated by intradermal skin testing and eosinophil cationic protein levels in both middle ear effusions and mucosal biopsies.
Laryngoscope 1996; 106: 1128-1137.
86 Nsouli TM, Nsouli SM, Linde RE, O'Mara F, Scanlon RT, Bellanti JA.
Role of food allergy in serous otitis media.
Annals of Allergy 1994; 73(3): 215-219.
87 Niemela M, Uhari M, Mottonen M.
A pacifier increases the risk of recurrent otitis media in children in day care centers.
Pediatrics 1995; 96: 884-888.
88 Adair-Bischoff Ce, Sauve RS.
Environmental tobacco smoke and middle ear disease in preschool age children.
Archives of Pediatric and Adolescent Medicine 1998; 152(2): 127-133.
89 Lohr KN, Beck S, Kamberg KJ, Brook RH, Goldberg GA.
Measurement of Physiologic Health for Children: Middle Ear Disease and Haring-Impairment.
Santa Monica, CA: RAND Health Experiment Series, 1983.
90 Teele DW, Klein JO, Rosner BA.
Otitis media with effusion during the first three years of life and development of speech and language.
Pediatrics 1984; 74(2): 282-287.
91 Kohl M.
Otitis media: Treating an effect when you do not know the cause.
Alternative Therapies in Health and Medicine 1996; 2(1): 68-70.
92 Karma P, Palva T. Kouvalnainea K, Karja J, Makela PH, Prinssi VP, Ruuskanen O, Launiala K.
Finnish approach to the treatment of acute otitis media: Report of the Finnish Consensus Conference.
Annals of Otolaryngology, Rhinology, and Laryngology Supplement 1987; 129: 1-19.
93 Sando I, Takahashi H, Matsune S.
Update on functional anatomy and pathology of human eustachian tube related to otitis media with effusion [review].
Otolaryngologic Clinics of North America 1991; 24: 795-811.
94 Holborow C.
Eustachian tube function: Changes throughout childhood and neuro-muscular control.
Journal of Laryngology and Otolaryngology 1975; 89: 47-55.
95 Hendricks CL, Larkin-Thier SM.
Otitis media in young children.
Journal of Chiropractic Research 1989; 2(1): 9-13.
96 Snell RS.
Clinical Anatomy for Medical Students, 3rd Edition.
Boston, MA: Little, Brown & Company, 1986, pp. 843-852.
97 Phillips N.J.
Vertebral Subluxation and Otitis Media: A Case Study
Chiropractic: The J of Chiro Res and Clin Inves 1992; 8 (2): 38–40
98 Schmidt MA.
Childhood Ear Infections. Berkeley, CA: North Atlantic Books, 1990, p. 75.
99 Pitkaranta A, Jero J, Arruda E, Virolainen A, Hayden FG.
Polymerase chain-reaction based detection of rhinovirus, respiratory syncytial virus, and coranovirus in otitis media with effusion.
Journal of Pediatrics 1998; 133(3): 390-394.
100 Fallon JM.
The role of the chiropractic adjustment in the care and treatment of 332 children with otitis media.
Journal of Clinical Chiropractic Pediatrics 1997; 2(2): 167-183.
101 Travis J.
Reviving the antibiotic miracle?
Science 1994; 264(5157): 360-362.
102 Tomasz A.
Multiple-antibiotic-resistant pathogenic bacteria: A report on the Rockefeller University Workshop.
New England Journal of Medicine 1994; 330(17): 1247-1251.
103 Whitney CG, Farley MM, Hadler J, Harrison LH, Lexau C, Reingold A, Lefkowitz L, Cieslak PR, Cetron M, Zell CR, Jorgensen JH, Schuchat A.
Active Bacterial Core Surveillance Program of the Emerging Infections Program Network. Increasing prevalence of multidrug resistant Streptococcus pneumoniae in the United States.
New England Journal of Medicine 2000; 343(26): 1917-1924.
104 Herper RLM.
Germ warfare.
Forbes June 19, 2006.
105 Neu HC.
The crisis in antibiotic resistance.
Science 1992; 257(5073): 1064-1073.
106 Lederberg J, Shope RE, Oaks SC, eds.
Emerging infections: Microbial threats to health in the United States.
Washington, DC: Institute of Medicine, National Academy Press, 1992.
107 LeDuc JW.
World Health Organization strategy for emerging infectious diseases.
Journal of the American Medical Association 1996; 275(4): 318-320.
108 Cohen ML.
Epidemiology of drug resistance: Implications for a post-antimicrobial era.
Science 1992; 257 (5073): 1050-1055.
109 Abuse of antibiotics. Lead editorial,
International Herald Tribune, June 19, 2000, p. 8.
110 Evans-Pritchard, A.
Science in the dock as the antibiotic miracle crumbles.
Sunday Times [London], May 3, 1998. p. 1.
111 Management of acute otitis media. Summary, evidence report/technology assessment No. 15, AHRQ Publication No. 01-E007, Rockville, MD:
Agency for Health Research and Quality, Public Health Service, U.S.Department of Health and Human Services, December 2000.
112 The Nation's Health [official newspaper of the American Public Health Association], November 2000, pp. 1,12.
113 Wickens K, Pearce N, Crane J, Beasley R.
Antibiotic use in early childhood and the development of asthma.
Clinical and Experimental Allergy 1999; 29(6): 766-771.
114 Sha SH, Schacht J.
Are aminoglycoside antibiotics excitotoxic?
Neuroreport 1998; 9(17): 3893-3895.
115 Sha SH, Schacht J.
Prevention of aminoglycoside-induced hearing loss.
Keio Journal of Medicine 1997; 46(3): 115-119.
116 Dehne N, Rauen U, deGroot H, Lautermann J.
Involvement of the mitochondiral permeability transition in gentamicin ototoxicity.
Hearing Research 2002; 169: 47-55.
117 Kalinec GM, Fernandez-Zapico ME, Urrutia R, Esteban-CrucianN, Chen S, Kalinec F.
Pivitol role of Harakiri in the induction and prevention of gentamicin-induced hearing loss.
Proceedings of the National Academy of Sciences 2005; 102(44): 16019-16024.
118 Ray WA, Murray KT, Meredith S, Narasimhulu SS, Hall K, Stein CM.
Oral erythromycin and the risk of sudden death from cardiac causes.
New England Journal of Medicine 2004; 351(11): 1089-1096.
119 Cantekin EI, McGuire Tw, Griffith TL.
Antimicrobial therapy for otitis media with effusion ["secretory" otitis media].
Journal of the American Medical Association 2991; 266(23): 3309-3317.
120 Del Mar C, Glasziou P, Hayem M.
Are antibiotics indicated as initial treatment for children with acute otitis media? A meta-analysis.
British Medical Journal 1997; 314(7093): 1526-1529.
121 Damoiseaux RAMJ, van Balen FAM, Hoes AW, Verheij TJM, de Melker RA.
Primary are based randomized double blind trial of amoxicillin versus placebo for acute otitis media in children aged under 2 years.
British Medical Journal 2000; 320(7231): 350-354.
122 Froom J, Culpepper L, Jacobs M, DeMelker RA, Green LA, van Buchem L, Grob P, Heeren T.
Antimicrobials for acute otitis media? A review from the International Primary Care Network.
British Medical Journal 1997; 315(7100): 98-102.
123 Mangione-Smith R, McGlynn EA, Elliott MN, Krogstad P, Brook RH.
The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior.
Pediatrics 1999; 103(4 Pt1): 711-718.
124 Virji A, Britten N.
A study of the relationship between patients' attitudes and doctors' prescribing.
Family Practice 1991; 8: 314-319.
125 Macfarlane J, Holmes W, Macfarlane R, Britten N.
Influences of patients' expectations on antibiotic management of acute lower respiratory tract illness in general practice: Questionnaire study.
British Medical Journal 1997; 315(7117): 1211-1214.
126 Britten N, Ukoumunne O.
The influence of patients' hopes of receiving a prescription on doctors' perceptions and the decision to prescribe: A questionnaire study.
British Medical Journal 1997; 315(7121): 1506-1510.
127 Vinson DC. Lutz LJ.
The effect of parental expectations on treatment of children with a cough: A report from the ASPN.
Journal of Family Practice 1993; 37(1): 23-27.
128 Webb S, Lloyd M.
Prescribing and referral in general practice: A study of patients' expectations and doctors' actions.
British Journal of General Practice 1994; 44(381): 165-169.
129 Hamm RN, Hicks RJ, Bemben DA.
Antibiotics and respiratory infections: Are patients more satisfied when expectations are met?
Journal of Family Practice 1996; 43(1): 56-62.
130 Himmel W, Lippert-Urbanke E, Kochen MM.
Are patients more satisfied when they receive a prescription? The effect of patient expectations in general practice.
Scandinavian Journal of Primary Health Care 1997; 15: 118-122.
131 Moss AI, Hamburger S, Moore RM Jr, Jeng LL, Howie LG.
Use of Selected Medical Device Implants in the United States: Advance Data.
Hyattsville, MD: National Center for Health Statistics, 1988. p. 191.
132 Paradise JL.
On tympanostomy tubes: Rationale, results, reservations, and recommendations.
Pediatrics 1977; 60(1): 86-90
133 Bluestone CD, Klein JO.
Otitis Media in Infants and Children.
Philadelphia, PA: WB Saunders Company, 1988. p. 175.
134 Pichichero ME, Berghash LR, Hengerer AS.
Anatomic and audiologic sequelae after tympanostomy tube insertion or prolonged antibiotic therapy for otitis media.
Pediatric Infectious Disease Journal 1989; 8(11): 780-787.
135 Bernard PAM, Stenstrom RJ, Feldman W, Durieux-Smith A.
Randomized, controlled trial comparing long-term sulfanilamide therapy to ventilation tubes for otitis media with effusion.
Pediatrics 1991; 88(2): 215-222.
136 Le CT, Freeman DW, Fireman BH.
Evaluation of ventilating tubes and myringotomy in the treatment of recurrent or persistent otitis media.
Pediatric Infectious Disease Journal 1991; 10(1): 2-11.
137 Kleinman LC, Kosecott J, Dubois RW, Brook RH.
The medical appropriateness of tympanostomy tubes proposed for children younger than 16 years in the United States.
Journal of the American Medical Association 1994; 271(16): 1250-1255.
138 Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Colborn DK, Bernard BS, Rockette HE, Janosky JE, Pitcairn DL, Sabo DL, Kurslasky M, Smith CG.
Effect of early or delayed insertion of tympanostomy tubes for persistent otitis media on developmental outcomes at age of three years.
New England Journal of Medicine 2001; 344(16): 1179-1187.
139 Wiberg, JM, Nordsteen, J, and Nilsson, N.
The Short-term Effect of Spinal Manipulation in the Treatment of Infantile Colic:
A Randomized Controlled Clinical Trial with a Blinded Observer
J Manipulative Physiol Ther 1999 (Oct); 22 (8): 517–522
140 Lester BM, Boukydis CFZ, Garcia-Coll CT, Hole WT.
Colic for developmentalists. Symposium on infantile colic:
Infant Mental Health Journal 1990; 11: 320-333.
141 National Center for Health Statistics, Department of Health and Human Services, http://www.dhhs.gov.
142 Hide DW, Guyer BM.
Prevalence of infantile colic.
Archives of Disease of Childhood 1983; 57(7): 559-560.
143 Rautava P, Lehonten L, Helenius H, Sillanpaa M.
Infantile colic: Child and family three years later.
Pediatrics 1995; 96(1 Pt. 1): 43-47.
144 Keefe Mr.
Irritable infant syndrome: Theoretical perspectives and practice implications.
ANS Advances in Nursing Science 1988; 10(3): 70-78.
145 Frodi AM.
Contributions of infant characteristics to child abuse.
American Journal of Mental Deficiency 1981; 85: 341-349.
146 Borowiz SM, Cox DJ, Tam A, Ritterband LM, Sutphen JL, Penberthy JK.
Preciptants of constipation during arly childhood.
Journal of the American Board of Family Practitioners 2003; 16: 213-218.
147 Nurko S.
Advances in the management of pediatric constipation.
Current Gastroenterology Reports 2000; 2: 234-240.
148 DiLorenzo C.
Childhood constipation: Finally some hard data about hard stools!
Journal of Pediatrics 2000; 136: 4-7.
149 van Ginkel R, Reitsma JB, Buller HA, van Wijk MP, Tamimiau J, Benninga MA.
Childhood constipation: Longitudunal follow-up beyond puberty.
Gastroenterology 2003; 125: 357-363.
150 Guyton AC, Hall JE.
Textbook of Medical Physiology, 11th edition.
Philadelphia, PA: Elsevier Saunders 2006; pp. 771-779, 822.
151 Hewitt EG.
Chiropractic treatment of a 7-month old with chronic constipation: A case report.
Chiropractic Technic 1993; 5: 101-103.
152 Hollbrook B.
Chiropractic treatment of childhood constipation: A review of the literature.
Journal of Clinical Chiropractic and Pediatrics 2005; 6: 427-431.
153 Spitzer RL. Chairperson.
Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition. Philadelphia,
PA: American Psychiatric Association Task Force on Nomenclature and Statistics, 1980.
154 Rudolph A.
Rudolph's Pediatrics, 19th edition.
Norwalk, CT: Appleton and Lange, 1991.
155 Young DE, Young RR.
Nocturnal enuresis: A review of treatment approaches.
American Family Physician 1985; 31: 141-144.
156 Rosenfeld J, Jerkins GR.
The bed-wetting child.
Post Graduate Medicine 1991; 69: 63-70.
157 Cessna RM.
The asthmatic patient.
American Chiropractor 1989; 4: 48-50.
158 Ali S, Hayek R, Holland R, McKelvy S-E, Boyce K, Curson P.
Effect of Chiropractic Treatment on the Endocrine and Immune System in Asthmatic Patients
Proceedings of the 9th International Conference on Spinal Manipulation.
Des Moines, IA: Foundation for Chiropractic Education and Research. In press, 2002.
159 McFadden ER, Gilbert IA.
Asthma: Medical progress.
New England Journal of Medicine 1992; 327: 1928-137.
160 Gergen PJ, Weiss KB.
Changing patterns of asthma hospitalization among children: 1979 to 1987.
Journal of the American Medical Association 1990; 264: 1688-1692.
161 Roberts CF.
Paediatric asthma.
Australian Family Physician 1991; 8: 1093-1098.
162 Munro-Ford R.
Asthma fight falters as the nation's death toll mounts.
Medical Forum, Weekend Australia 4 January 1992, p. 22.
163 Mellis CM, Peat JK, Bauman AE, Woolcokc AJ.
The cost of asthma in New South Wales.
Medical Journal of Australia 1991; 155: 522-524.
164 Potterton D.
The politcs of asthma: Out of control.
Nursing Times 1992; 88(2): 26-31.
165 Clark NM, Brown RW, Parker E, Robins TGH, Remick DG, Philbert MA, Keeler GJ, Israel BA, Remick DG Jr.
Environmental Health Perspectives 1999; 107[Supplement]: 421-429.
166 Health Letter on the CDC, via Newsedge Corporation. May 11, 1998.
167 Meeker WC, Mootz RD, Haldeman S.
Back to basics: The state of chiropractic research.
Topics in Clinical Chiropractic 2002; 9(1): 1-13.
168 Shekelle PG, Brook RH.
A community-based study of the use of chiropractic services.
American Journal of Public Health 1991; 81(4): 439-442.
169 Hayden JA, Mior SA, Verhoef MJ.
Evaluation of chiropractic management of pediatric patients with low back pain: A prospective cohort study.
Journal of Manipulative and Physiological Therapeutics 2003; 26(1): 1-8.
170 Hession EF, Donald GD.
Treatment of multiple lumbar disk herniations in an adolescent athlete utilizing flexion distraction and rotational manipulation.
Journal of Manipulative and Physiological Therapeutics 1993; 16: 185-192.
171 Kazemi M.
Adolescent lumbar disc hernatioin in a tae kwon do martial artist: A case report.
Journal of the Canadian Chiropractic Association 1999; 43: 236-242.
172 King L, Mior SA, Devonshire-Zielonka K.
Adolescent lumbar disc herniation: A case report.
Journal of the Canadian Chiropractic Association 1996; 40: 15-18.
173 Boline, PD, Kassak, K, Bronfort, G, Nelson, C, and Anderson, AV.
Spinal Manipulation vs. Amitriptyline for the Treatment of Chronic Tension-type Headaches:
A Randomized Clinical Trial
J Manipulative Physiol Ther 1995 (Mar); 18 (3): 148–154
174 Nilsson N, Christensen HW, Hartvigsen J.
The Effect of Spinal Manipulation in the Treatment of Cervicogenic Headache
J Manipulative Physiol Ther 1997 (Jun); 20 (5): 326–330
175 Nelson CF, Bronfort G, Evans R, Boline P, Goldsmith C, Anderson AV:
The Efficacy of Spinal Manipulation, Amitriptyline and the Combination of Both Therapies
for the Prophylaxis of Migraine Headache
J Manipulative Physiol Ther 1998 (Oct); 21 (8): 511–519
176 Kjellman GV, Skagren EI, Oberg BE.
A critical analysis of randomised clinical trials on neck pain and treatment efficacy: A review of the literature.
Scandinavian Journal of Rehabilitative Medicine 1999; 31(3): 139-152.
177 Bronfort G, Assendelft WJJ, Evans R, Haas M, Bouter L.
Efficacy of spinal manipulation for chronic headaches: A systematic review.
Journal of Manipulative and Physiological Therapeutics 2001; 24(7): 457-466.
178 McCrory DC, Penzien DB, Hasselblad V, Gray RN.
Evidence Report: Behavioral and Physical Treatments for Tension-type and Cervicogenic Headache
Des Moines, IA: Foundation for Chiropractic Education and Research, 2001.
179 Haney V.
Chronic pediatric migraine-type headache treated by long-term inderol prior to chiropractic care: A case report.
Proceedings of the National Conference on Chiropractic Pediatrics, Palm Beach, FL, October 1993, pp. 132-140.
180 Hewitt EG.
Chiropractic care of a 13-year old with headache and neck pain: A case report.
Journal of the Canadian Chiropractic Association 1994; 34(3): 160-162.
181 Kastner U, Deutsch J, Lackner R.
Chronic headache in children and chiropractic manipulation.
Conference Proceedings of the Chiropractic Centennial Foundation, Washington, DC, July 1995, pp. 286-287.
182 Cochran JA.
Chiropractic treatment of childhood migraine headache: A case study.
Proceedings of the National Conference on Chiropractic Pediatrics, Vancouver, British Columbia, CANADA, October 1994, pp.85-90.
183 Anderson-Peacock ES.
Chiropractic care of children with headaches: Five case reports.
Journal of Clinical Chiropractic Pediatrics 1996; 1(1): 18-27.
184 Lisi AJ, Dabrowski Y.
Chiropractic spinal manipulation for cervicogenic headache in an 8-year old.
Journal of the Neuromusculoskeletal System 2002; 10(3): 98-103.
185 Froehle R.M.
Ear Infection: A Retrospective Study Examining Improvement From
Chiropractic Care and Analyzing Influencing Factors
J Manipulative Physiol Ther 1996 (Mar); 19 (3): 169–177
186 Fallon J, Edelman MJ.
Chiropractic care of 401 children with otitis media: A pilot study.
Alternative Therapies in Health and Medicine 1998; 4(2): 93.
187 Mills MV, Henley CE, Barnes LLB, Carreiro JE, Degenhardt BF.
The use of osteopathic manipulative treatment as adjuvant therapy in children with recurrent acute otitis media.
Archives of Pediatrics and Adolscent Medicine 1003; 157(9): 861-866.
188 Diamant M, Diamant B.
Abuse and timing of use of antibiotic in acute otitis media.
Archives of Otolaryngology 1974; 100(3): 226-232.
189 Wiberg JMM, Nordsteen J, Nilsson N.
The Short-Term Effect of Spinal Manipulation in the Treatment of Infantile Colic:
A Randomized Controlled Clinical Trial with a Blinded Observer
Journal of Manipulative and Physiological Therapeutics 1999; 22(8): 517-522.
190 Olafsdottir E, Forshei S, Fluge G, Markestad T:
Randomised Controlled Trial of Infantile Colic Treated With Chiropractic Spinal Manipulation
Archives of Disease in Childhood 2001 (Feb); 84 (2): 138–141
191 Mercer C, Nook BC.
The efficacy of chiropractic spinal adjustments as a treatment protocol in the management of infantile colic.
Proceedings of the 5th Biennial Congress, Auckland, NEW ZEALAND, May 17-22, 1999, pp. 170-171.
192 Klougart N, Nilsson N, Jacobsen J.
Infantile Colic Treated by Chiropractors: A Prospective Study of 316 Cases
J Manipulative Physiol Ther 1989 (Aug); 12 (4): 281–288
193 Leach RA.
Differential Compliance Instrument in the Treatment of Infantile Colic: A Report of Two Cases
Journal of Manipulative and Physiological Therapeutics 2002; 25(1): 58-62.
194 Eriksen K.
Effects of upper cervical correction on chronic constipation.
Chiropractic Research Journal 1994; 3: 19-22.
195 Marko SK. Case study:
The effect of chiropractic care on an infant with problems of constipation.
Chiropractic Pediatrics 1994; 1: 23-24.
196 Quist DM, Duray SM.
Resolution of symptoms of chronic constipation in an 8-year-old male after chiropractic treatment.
Journal of Manipulative and Physiological Therapeutics 2007; 30(1): 65-68.
197 Bennet-Johnson S. Enuresis. In Daitzman RJ [Ed],
Clinical Behaviour Therapy and Behaviour Modification.
New York, NY: Garland STPM Press, 1980, pp. 81-141.
198 Reed WR, Beavers S, Reddy SK, Kern G.
Chiropractic management of primary nocturnal enuresis.
Journal of Manipulative and Physiological Therapeutics 1994; 17(9): 596-600.
199 Lebouef C, Brown P, Herman A, Leembruggen K, Walton D, Crisp TC.
Chiropractic care for children with nocturnal enuresis: A prospective outcome study.
Journal of Manipulative and Physiological Therapeutics 1991; 14(2): 110-115.
200 Gemmell HA, Jacobson BH.
Chiropractic management of enuresis: Time-series descriptive design.
Journal of Manipulative and Physiological Therapeutics 1989; 12(5): 386-389.
201 Palmer College of Chiropractic Adjusting Manual.
Davenport, IA: Palmer College of Chiropractic, 1983.
202 Sears MR, Taylor DR, Print CG, Lake DC, Li QQ, Flannery EM, Yates DM, Lucas MK, Herbison GP.
Regular inhaled beta-agonist treatment in bronchial asthma.
Lancet 1990; 336(8728): 1391-1396.
203 Dhami MSI, DeBoer KF.
Systemic effects of spinal lesions.
In Haldeman S [ed], Principles and Practice of Chiropractic, 2nd Edition. Norwalk, CT: Appleton & Lange, 1992, pp. 115-135.
204 Selye H.
Stress and duress.
Comprehensive Therapy 1975; 1: 9-13.
205 Bassett JR, Marshall PM, Spillane R.
The physiological measurement of acute stress [public speaking] in bank employees.
International Journal of Psychophysiology 1987; 5(4): 265-273.
206 Kirschbaum C, Hellhammer DH.
Salivary control in psychobiological research: An overview.
Neuropsychobiology 1989; 22(3): 150-169.
207 Guyton AC, Hall JE.
Textbook of Medical Physiology. Philadelphia, PA: WB Saunders & Company, 1986, p. 914.
208 Morgan LG.
Psychoneuroimmunology, the placebo effect and chiropractic.
Journal of Manipulative and Physiological Therapeutics 1998; 21(7): 484-491.
209 Rosner A. Endocrine disorders.
In Masarsky CS, Todres-Masarsky M,
Somatovisceral Aspects of Chiropractic: An Evidence-Based Approach. New York, NY: Churchill Livingstone, 2001, pp. 187-202.
210 Lane DJ.
What can alternative medicine offer for the treatment of asthma?
Journal of Asthma 1994; 31(3): 153-160.
211 Field T, Henteleff T, Hernandez M, Martinez E, Mavunda K, Kuhn C, Schanberg S.
Children with asthma have improved pulmonary functions after massage therapy.
Journal of Pediatrics 1998; 32(5): 854-858.
212 Beyeler W.
Experiences in the management of asthma.
Annals of the Swiss Chiropractic Association 1965; 3: 111-117.
213 Nilsson N, Christiansen B.
Prognostic factors in bronchial asthma in chiropractic practice.
Journal of the Australian Chiropractic Association 1988; 18: 85-87.
214 Balon J, et al.
A Comparison of Active and Simulated Chiropractic Manipulation
as Adjunctive Treatment for Childhood Asthma
New England Journal of Medicine 1998; 339(15): 1013-1020
215 Bronfort G, Evans RL, Kubic P, Filkin P.
Chronic Pediatric Asthma and Chiropractic Spinal Manipulation:
A Prospective Clinical Series and Randomized Clinical Pilot Study
Journal of Manipulative and Physiological Therapeutics 2002; 24(6): 369-377.
216 Gleeson M, Clancy RL, Hensley MJ, Cripps AW, Henry RL, Wlodarczy JH, Gibson PG.
Development of bronchial hyperreactivity following transient absence of IgA.
American Journal of Respiratory and Critical Care Medicine 1996; 153[6 Pt 1]: 1785-1789.
217 Dishman JD, Dougherty PE, Burke JR.
Evaluation of the postural perturbation on motoneural activity following various methods of spinal manipulation.
The Spine Journal 2005; 5: 650-659.
218 Plaugher, G, Cremata EE, Phillips, R.
A retrospective consecutive case analysis of pretreatment and comparative static radiological parameters following chiropractic adjustments.
Journal of Manipulative and Physiological Therapeutics 1990; 13(9): 498-506.
219 Lantz CA, Chen J.
Effect of Chiropractic Intervention on Small Scoliotic Curves in Younger Subjects: A Time-series Cohort Design
J Manipulative Physiol Ther. 2001 (Jul); 24 (6): 385–393
220 Menke JM, Plaugher G, Carrari CA, Coleman RR, Vannetiello L, Bachman TR.
Likelihood-evidential support and Bayesian re-analysis on a prospective cohort of children and adolescents with mild scoliosis chiropractic management.
Journal of the Arizona-Nevada Academy of Sciences 2006; Supplemental issue; Accepted for publication, 10/06.
221 Tarola GA.
Manipulation for the Control of Back Pain and Curve Progression
in Patients with Skeletally Mature Idiopathic Scoliosis: Two Cases
Journal of Manipulative and Physiological Therapeutics 1994; 17(4): 253-257.
222 Fisher RS, Krauss GL, Ramsay E, Laxer K, Gates J.
Assessment of vagus nerve stimulation for epilepsy: Report of the Therapeutics and Technology Assessment.
Neurology 1997; 49(1): 293-297.
223 Pistolese RA.
Epilepsy and Seizure Disorders: A Review of Literature Relative to Chiropractic Care of Children
Journal of Manipulative and Physiological Therapeutics 2001; 24(3): 199-205.
224 Sandefur R, Adams E.
The effect of chiropractic adjustments on the behavior of autistic children: A case review.
Chiropractic Journal 1987; 24(12): 21-25.
225 Hyman CA.
Chiropractic adjustments and the reduction of petit mal seizures in a five-year old male: A case study.
Journal of Clinical Chiropractic Pediatrics 1996; 1(1): 28-32.
226 Langley CA.
Epileptic seizures, nocturnal enuresis, ADD.
Chiropractic Pediatrics 1994; 1: 22.
227 Aguilar AL, Grostic JD, Pfleger B.
Chiropractic care and the behavior in autistic children.
Journal of Clinical Chiropractic Pediatrics 2000; 5 (1): 293-304.
228 Giesen JM, Center DB, Leach RA.
An Evaluation of Chiropractic Manipulation as a Treatment of Hyperactivity in Children
Journal of Manipulative and Physiological Therapeutics 1989; 12 (5): 353-363.
229 Tanaka ST, Martin CJ, Thibodeau P.
Clinical neurology.
In Anrig C, Plauger G [eds], Pediatric Chiropractic. Baltimore, MD: Williams & Wilkins, 1998, pp. 479-611.
230 Barnes T.
Kentuckiana children's center: A 40-year history.
Journal of Chiropractic Humanities 1997; 7 (1): 18-22.
231 Oklahaven celebrates 40 years.
Dynamic Chiropractic September 2002; 20 (18).
232 Lee ACC, Li DH, Kemper KJ.
Chiropractic care for children
Archives of Pediatrics and Adolescent Medicine 2000; 154 (4): 401-407.
233 Verhoef MJ, Papadopoulos C, Durant DL.
Chiropractors' involvement in the treatment of patients under age 18.
Proceedings of the International Conference on Spinal Manipulation.
Vancouver, British Columbia, CANADA, July 16-19, 1998, pp. 147-149.
234 American Chiropractic Association.
Improper Use of Backpacks Leads to Chronic Back Pain
Journal of the American Chiropractic Association, 1999; 37: 1-2.
235 International Chiropractic Pediatric Association.
Backpacks… Your Child's Spine Is At Stake
ICPA Newsletter November/December 1998, pp. 1-2.
236 Legg SJ.
Subjective perceptural methods for comparing backpacks.
Ergonomics 1997; 40(8): 809-817.
237 http://www.acatoday.org. Downloaded 09/08/06.
238 Sjolie AN, Ljunggren AE.
The significance of high lumbar mobility and low lumbar strength for current and future low back pain in adolescents.
Spine 2001; 26(23): 2629-2636.
239 http://www.cocsa.org/pubs/resources/88_1958_12646.cfm. Downloaded 02/15/07.
240 http://www.straightupamerica.org. Downloaded 02/15/07.
241 Stamatakis, E, Primatesta P, Chinn S, Rona R, Falascheti E.
Overweight and obesity trends in English children: What is the role of socioeconomic status?
Archives of Diseases of Childhood 2005; 90(10): 999-1004.
242 Ogden CL, Flegal KM, Caroll MD, Johnson CL.
Prevalance and trends in overweight among US children and adolescents, 1999-2000.
Journal of the American Medical Association 2002; 288(14): 1728-1732.
243 Wang Y, Monteiro C, Popkin BM.
Trends in obesity and underweight in older children and adolescents in the United States, Brazil, and Russia.
American Journal of Clinical Nutrition 2002; 75 (6): 971-977.
244 Reinehr T, de Sousa G, Toschke AM, Andler W.
Long-term follow-up of cardiovascular disease factors in children after an obesity intervention.
American Journal of Clinical Nutrition 2006; 84 (3): 490-496.
245 Hall A.
Chiropractic influence on childhood obesity.
Topics in Clinical Chiropractic 2001; 8 (4): 8-11.
246 U.S. Department of Health and Human Services.
Put Prevention into Practice.
http://odphp.osophs.dhhs.gov/pubs/prevrpt/98/sprpr/98sprfoc.htm [1998], Accessed 29 April 2001.
247 Zerhouni E. Director of the National Institutes of Health, at the Harvard School of Public Health, April 14, 2005, quoted in the Boston Globe April 19, 2005, pp. D1, D4.
248 Institute of Medicine Committee on Quality of Health Care in America.
Crossing the Quality Chasm: A New Health System for the 21st Century
Washington, DC: National Academies Press; 2001
249 Phillips RB, Mootz RD.
Contemporary chiropractic philosophy
In Haldeman S [ed], Principles and Practice of Chiropractic, 2nd edition. Norwalk, CT: Appleton and Lange, 1992, p. 45.
250 Coulter ID,
Alternative and investigatory paradigms for chiropractic.
Journal of Manipulative and Physiological Therapeutics 1993; 16(5): 319-326.
251 Jamison JR.
The conundrum of contemporary chiropractic.
Chiropractic Journal of Australia 1993; 23: 136-140.
252 Phillips RB, Gatterman MI.
Chiropractic paradigms
In Gatterman MI [ed], Foundations of Chiropractic Subluxation Gatterman MI [Ed.]. St. Louis, MO: Elsevier Mosby, 2005, pp. 19-29.
253 The ACC chiropractic paradigm.
Association of Chiropractic Colleges, 1996.
254 Dvorak J, Orelli F.
How dangerous is manipulation of the cervical spine?
Manual Medicine 1985; 2: 1-4.
255 Haldeman S, Carey P, Townsend M, Papadopoulos C.
Arterial Dissections Following Cervical Manipulation: The Chiropractic Experience
Canadian Medical Association Journal 2001; 165(7): 905-906.
256 Shekelle PG, Adams AH, Chassin MR, Hurwitz EL, Brook RH.
Spinal manipulation for back pain.
Annals of Internal Medicine 1992; 117: 590-598.
257 Vohra, S, Johnston, BC, Cramer, K, and Humphreys, K.
Adverse Events Associated with Pediatric Spinal Manipulation: A Systematic Review
Pediatrics. 2007 (Jan); 119 (1): e275–e283
258 Dabbs V Lauretti WJ
A Risk Assessment of Cervical Manipulation vs. NSAIDs for the Treatment of Neck Pain
J Manipulative Physiol Ther 1995 (Oct); 18 (8): 530–536
259 Deyo RA, Cherkin DC, Loesser JD, Bigos SJ, Ciol MA.
Morbidity and mortality in association with operations on the cervical spine: The influene of age, diagnosis, and procedure.
Journal of Bone and Joint Surgery Am 1992; 74(4): 536-543.
260 Horwowitz SH.
Peripheral nerve injury and causalgia secondary to routine venipuncture.
Neurology 1994; 44: 962-964.
261 Stremple JS, Boss DS, Davis CH, McDonald GO.
Comparison of post-operative mortality and morbidity in Veterans Affairs and nonfederal hospitals.
Journal of Surgical Research 1994; S6: 4-50416.
262 Colley F, Haas M.
Attitudes on immunizations: A survey of American chiropractors.
Journal of Manipulative and Physiological Therapeutics 1994; 17 (9): 584-590.
263 Forrester JA, Anrig CA.
The prenatal and perinatal period.
In Anrig C, Plauger G [eds], Pediatric Chiropractic. Baltimore, MD: Williams & Wilkins, 1998, pp. 152-160.
264 Geier DA, Geier MR.
Early downward trends in neurodevelopmental disorders following removal of
thimerosal-containing vaccines.
Journal of American Physicians and Surgeons 2006; 11 (1): 8-13.
265 Jean Matthies v. Edward D. Mastromonaco, D.O.
Supreme Court of New Jersey [A-9-98], Pollock J, Judgment dated July 8, 1999.
266 Lack JA, Stuart-Taylor ME.
Calculation of drug dosage and body surface areas of children.
British Journal of Anaesthesiology 1997; 78 (5): 601-605.
267 Wildhaber JH, Monkhoff M, Sennhauser FH.
Dosage regimens for inhaled therapy in children should be reconsidered.
Journal of Pediatric and Child Health 2002; 38 (2): 115-116

Return to PEDIATRICS
Since 3-03-2010


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |