

Description of Recurrent Headaches in 7-14-year-old Children:
Baseline Data From a Randomized Clinical Trial on
Effectiveness of Chiropractic Spinal Manipulation
in Children with Recurrent HeadachesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Chiropractic & Manual Therapies 2023 (Jan 30); 31 : 5 ~ FULL TEXT
OPEN ACCESS Kristina Boe Dissing, Werner Vach, Susanne Lynge, Henrik Wulff Christensen & Lise Hestbaek
Chiropractic Knowledge Hub,
Campusvej 55, 5230,
Odense M, Denmark.

Background: Headaches in children are poorly described and diagnosing can be challenging. Objectives are: (1) to describe headache characteristics and child characteristics, (2) to explore whether data can suggest a more diverse way to categorize headaches than traditionally.
Methods: Baseline data for a clinical trial included a questionnaire and a physical screening. Children's characteristics and detailed description of headache symptoms were provided. Children were classified for migraine or tension-type-headache based on questionnaire data reported by children and parents. This required to apply slightly modified classification criteria and a "non-classifiable" group was added. Severity and symptoms, related to the migraine versus tension type distinction, were investigated to define a migraine-tension-type-index.
Results: 253 children were included. Mean pain intensity was 5.9/10. Over 2/3 of the children had headache for > 1 year, and > 50% for several days/week. Half of the children were non-classifiable, 22% were classified as migraine and 23% as tension-type headache. A migraine-tension-type-index was constructed and describes a continuous spectrum rather than two distinct groups.
Conclusions: Children with recurrent headaches are often severely affected. A questionnaire-based classification appeared feasible to distinguish between migraine and tension-type headaches in children but leaving many children unclassified. A migraine-tension-type-index can be generated allowing to regard the traditional distinction as a continuum (including mixed headache), and potentially serving as an instrument to improve headache management.
Trial registration: ClinicalTrials.gov, identifier NCT02684916.
Keywords: Children; Classification; Diagnosis; Headache.
From the FULL TEXT Article:
Introduction
Headache in children is common, often recurring, and prevalence rises from 5% at the age of three to more than 50% in puberty. [1, 2] Recurrent headaches may impact many aspects of childhood, such as quality of life and school performance [3, 4], social life [3], mental health [5, 6], and participation in physical activities. [7] Furthermore, children with recurrent headaches suffer from more comorbid physical conditions, such as abdominal pain, neck and back pain, overweight, sleep problems, and allergies. [5, 8–12] This emphasizes the need for early identification and proper management of children with recurrent headache, to minimize the risk of long-term consequences, not least because children experiencing recurrent headaches also have a higher risk of suffering from headaches in adulthood. [13, 14]
Basic knowledge of headache characteristics and demographic factors is important to aid proper management and prevention. Treatment strategies for headaches are typically founded on the diagnosis of headache type, based on the International Classification of Headache Disorders (ICHD). [15] It can be challenging to categorize younger children with headaches, because they may have difficulties describing their symptoms, especially regarding pain quality, pain score and presence of pain-aggravating factors. [16, 17] Furthermore, it seems that children often are unclassifiable or have coexisting headaches, primarily migraine and tension-type headache [16], which are the most commonly recurring headaches in children. [18, 19] It would be desirable for both clinicians and researchers to take this uncertainty into account. Regarding the distinction as the end points of a continuum may be one way to approach this.
To improve our knowledge about children with recurrent headaches we will take advantage of a population sampled for a randomized controlled trial (RCT) investigating the effectiveness of chiropractic spinal manipulation in children aged 7–14 with recurrent headaches. [20, 21] This study collected extensive baseline information on more than 200 children and therefore a detailed description of these children will be reported regarding headache characteristics, co-morbidity, trauma, and physical activity.
Thus, the objectives of this study are(1) to describe headache characteristics and child characteristics in children with recurrent headaches, and
(2) to explore whether data can suggest a more diverse way to categorize headaches than traditionally, by generating a new index.
Materials and methods
Setting
Data were collected at two clinics (one chiropractic clinic and one pediatric specialty practice) in Northern Denmark. Screenings were performed by the same investigating chiropractor. All details can be seen in the study protocol of the RCT. [20]
Participants
From November 2015 to August 2019, children aged 7–14 years with recurrent headaches were recruited to the trial through the Danish School Information Network, local newspapers, television, social media, and radio.
Participants were included in the trial if they(1) were between 7–14 years old,
(2) had experienced at least one episode of headache per week for the past 6 months, and
(3) had at least one musculoskeletal dysfunction in the spine, pelvis or temporomandibular joints found at the physical screening.Before the screening for the trial, all eligible children and their parents answered three questions each week for four weeks via a text message system on their mobile (number of days with a headache, intensity of headaches and number of pills taken for headache during the previous week), thereby verifying having at least one episode of headache per week for four weeks. In addition, a baseline questionnaire was completed.
Variables
Data for this study were based on the baseline questionnaire (“Appendix 1”) as well as clinical data from the physical screening. The questionnaire was based on relevant literature and knowledge obtained from a non-published scoping review by the primary investigator, as part of her dissertation for a master’s degree in Musculoskeletal Pediatrics. It was completed by the parents/caregiver and the child. All children with data from both the baseline questionnaire and the screening were included, regardless of participation or non-participation in the subsequent trial. All included variables in this study are described in detail in “Appendix 2”, including specification of content, response format and source.
Classification of headaches

Table 1 To develop the index, we needed to categorize the children into having migraine or tension-type headaches. The standard method when diagnosing headaches are using interviews and headache diaries, and optionally validated questionnaires. The children evaluated for participation in the trial were included due to experiencing recurrent headaches and not by diagnosis, and therefore the available data does not cover the ICHD criteria entirely, so the categorization had to be slightly modified (Table 1).
Criteria A was considered to be fulfilled for both migraine and tension-type headaches since the children were having weekly headache. A migraine diagnosis was allocated if criteria B–D were fulfilled. For tension-type headaches, we ignored information on duration since the response options were not detailed enough. Hence a diagnosis was allocated if criteria C + D was fulfilled. We chose not to distinguish between migraine with or without aura symptoms and used the criteria for migraine without aura. Children not fulfilling the criteria for migraine or tension-type-headache were regarded as a third group labeled as having “non-classifiable headache”.
Statistical analyses
The child- and headache characteristics are described by absolute and relative frequencies and means with 10th and 90th percentiles for all children and stratified by headache type. The statistical significance of differences between the three groups were assessed using the Kruskal Wallis test for continuous and ordinal variables, and an extension of Fisher’s exact test for binary and categorical variables. Kernel density estimates were used to depict distributional differences in continuous variables between subgroups of children.
Construction of a migraine-tension-type-index
Instead of applying an existing categorization, it is possible to use our data to investigate whether the distinction between migraine and tension-type headache also makes sense in children, and to explore whether our data can suggest a more diverse way to categorize headaches than the traditional categorization. If there is evidence for this, it might be possible to develop an index helping to identify those children who can be assigned definitely to one type and to evaluate the degree of either migraine or tension type headache in children with mixed headaches.
According to the ICHD, migraine and tension-type-headache differ with respect to severity, co-occurring symptoms (nausea/vomiting, photophobia and phonophobia), relation to routine physical activity, and location. As pointed out above, closely corresponding information was available in our data. Consequently, we explored the correlation among these variables to check, whether corresponding dimensions were identifiable and tried to combine the emerging dimensions into one index. We approached this step by inspection of association measures (Pearson correlation, Odds ratios) for each pair of variables. We used a factor analysis with varimax rotation to identify latent variables/dimensions. To summarize the information from several variables into one index, the first principal component score was used. In this score, the weights of each variable are chosen in the way maximizing the variance of the resulting score.
The following variables were included in this analysis:
Aspects of severity: Intensity, frequency, length of headache episode, duration of headache prior to entering the project, the use of medicine and number of days absent from school.
Co-occurring symptoms: nausea, vomiting, phonophobia, photophobia
Aggravation: Physical activity
Location of headache
Extending the categorization to include a “probable” state
The ICHD classification allows to define also probable migraine and probable tension-type headaches in those children fulfilling only 3 of the 4 criteria. Following this idea, we extended our classification system accordingly. “Probable migraine” was considered if 2 out of 3 criteria B–D were fulfilled, and “probable tension-type headache” was considered if 1 out of 2 criteria C + D was fulfilled.
Results
Description of children with recurrent headaches

Table 2

Table 3 There were 283 children eligible for the pre-screening data collection period, 30 children did not fulfill the inclusion criteria for the screening process and were therefore excluded, and hence, the baseline cohort consisted of 253 children, with 44% boys and a median age of 11. [21] Descriptive information about the cohort can be found in the “total” column of Tables 2 and 3.
The mean pain intensity at baseline was 5.9 measured on a numerical rating scale. More than 2/3 of the children had been suffering from headache for more than a year and more than 50% for several days a week. The duration of attacks varied, but most commonly they lasted from two to twelve hours per day.
More than 90% of the children were engaged in sports one or more times per week, screen time per day was most commonly two to four hours, and more than 90% slept well. All children experienced some co-occurring symptoms, most often nausea, dizziness, phonophobia or photophobia. The most frequent triggering factors of headache were sports and use of computer/tv, and the most frequent relieving factors were sleep and medicine. Cervical dysfunctions and decreased cervical range of motion was found in 3/4 of the children, and 60% had experienced neck pain within the last year. Around 2/3 of the children had experienced trauma to the head and/or neck without seeing a doctor or going to the hospital, and 1/3 had experienced trauma needing medical attention.
More than half of the children had been examined by a general practitioner and 20% had received treatment for headache before entering the study. More than 1/3 of the children used non-prescriptive medicine one or more days a week.
Differences between children classified with migraine, tension-type headache, or non-classifiable headache
Half of the children did not fall into one of the two diagnostic types, 22% of the children were categorized with migraine and 23% with tension-type headache. Table 2 depicts the differences in headache characteristics defining the diagnoses. The differences between tension-type headache and migraine were most pronounced with respect to co-occurring symptoms and aggravation by sports.
Non-classifiable children tend to have headache less frequently, a lower episode duration and more varying pain or pain in the forehead.
Table 3 shows the differences between diagnostic groups for variables not used as diagnostic criteria. For most variables no distinct differences could be observed. However, in the tension-type group the duration before screening was shorter, children with migraine took more medication and consulted health care professionals more often (both for examination and treatment). Only few of these differences were statistically significant.Construction of a migraine-tension-type-index
For the six variables related to severity, we observed only very moderate correlations (“Appendix 3”). Interestingly, the number of sick days was correlated with all aspects, suggesting that this variable might be seen as a summary measure.
A factor analysis suggested to reduce the severity variables to two factors: one factor related to all variables except frequency, and another factor related to frequency and length of episode (“Appendix 4”).
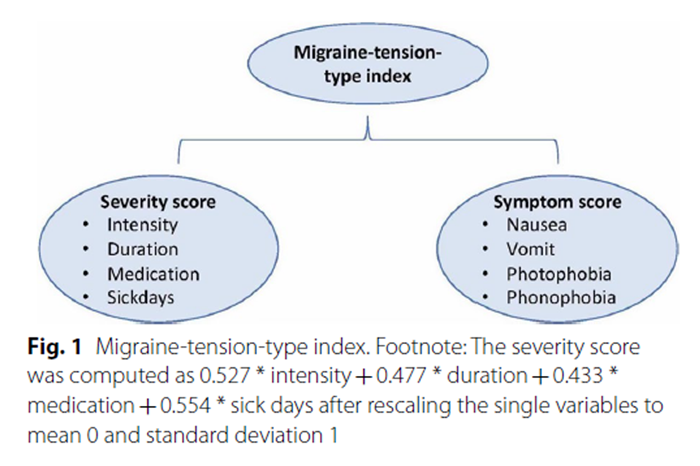
Figure 1 This is in line with the distinction between migraine and tension-type headache, where intensity plays a major role, whereas the role of frequency is less clear. To compute the first summary variable (severity score), we applied a principal component analysis (PCA) based on the severity variables except frequency and length of episode (i.e. intensity, duration of headache prior to entering the project, the use of medicine, and the number of days absent from school), and obtained the weights indicated in Figure 1.
The four co-occurring symptoms nausea, vomiting, phonophobia and photophobia tended to be rather distinctly associated (ORs between 1.8 and 43.2, see “Appendix 5”) with the highest association between nausea and vomiting (OR = 43.2). We defined a symptom score by counting the presence of the single symptoms, resulting in a symptom score from 0 to 4 (Fig. 1).
We observed a distinct association between the severity score and the symptom score (r = 0.45), which supports the assumption that the distinction between migraine and tension-type headache using severity and co-occurring symptoms is as reasonable in children as in adults. We therefore defined a migraine-tension-type-index as a PCA-based summary score based on both the severity and the symptom scores.
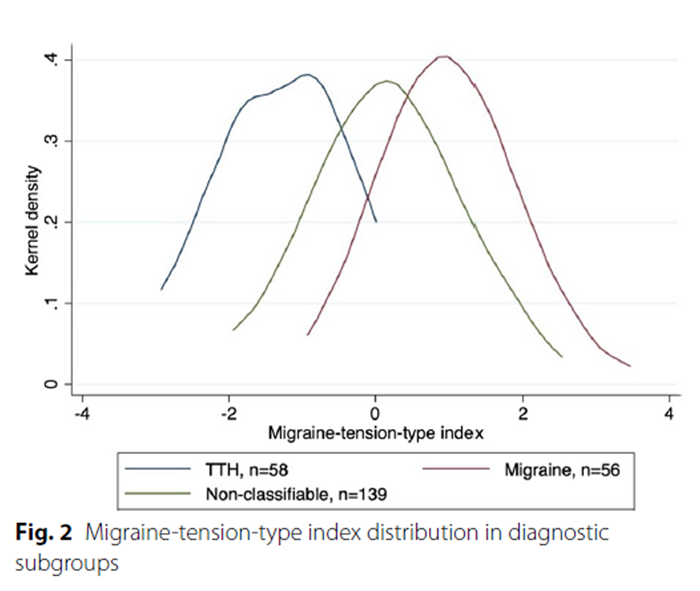
Figure 2 This new index describes a continuous spectrum and not just two distinct groups, but probably with migraine in the high end of the index and tension-type headache in the low end. This is supported by the distribution of the index in the three diagnostic subgroups (Figure 2): Children classified as migraine and tension-type headache, respectively, define two rather well separated groups.
Interestingly, the non-classifiable children do not just constitute a distinct in-between-group, but partially include children with rather low or high index values.
One advantage of this index is the possibility to include all children in investigations of the relation between the migraine-tension-type distinction and other variables.
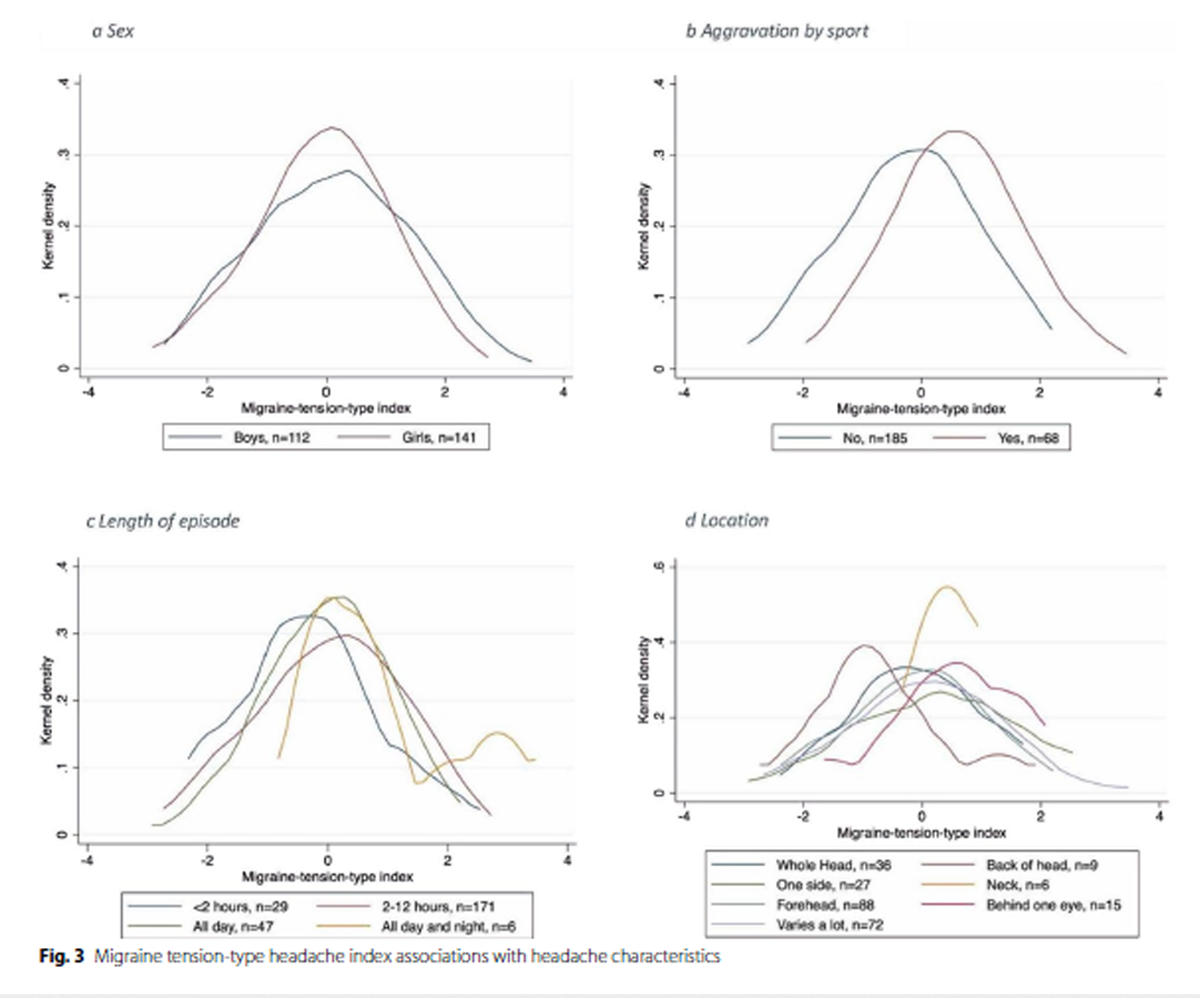
Figure 3

Table 4
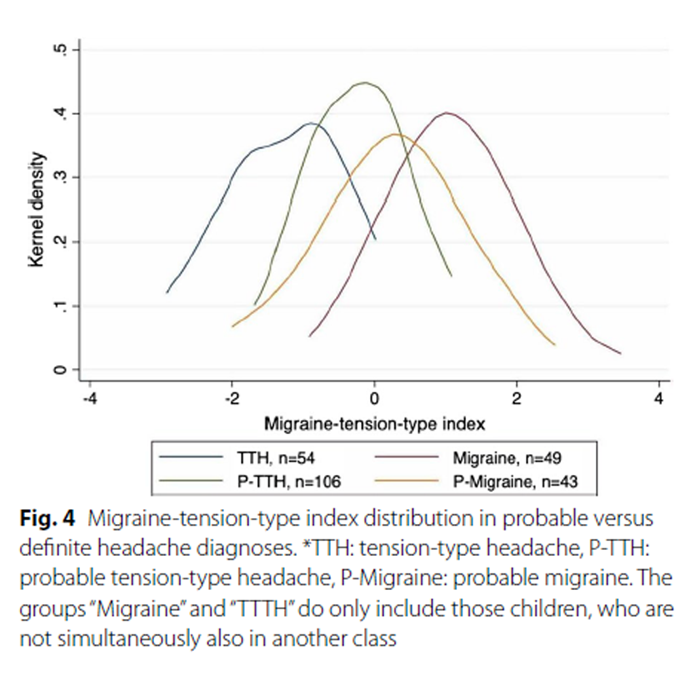
Figure 4 Figure 3a depicts the distribution of the index within boys and girls, and we can observe that girls have a rather symmetric distribution, whereas in boys there is a slightly skewed distribution with a tendency to more extreme values in the direction of migraine. Furthermore, we investigated the relation of the migraine-tension-type distinction to the classification variables not included in the index; that is length of episode, aggravation by sports and location of headache (Fig. 3b–d). Figure 3b depicts that aggravation by sports is associated with index values in the direction of migraine which is in line with the diagnostic criteria. Regarding length of episode (Fig. 3c) there is a tendency towards low index values in the direction of tension-type headache for those with short-lasting episodes and for high values for those with long-lasting episodes. As for location, the most distinct differences seen in Fig. 3d are between ‘Back of head’ trending towards low values, i.e. tension-type headache, and ‘Behind one eye’ trending towards high values, i.e. migraine. The latter holds also for ‘Neck’, but these three groups include very few children and thus this should be interpreted with caution.
Extending the classification system
Table 4 indicates the distribution of the number of criteria fulfilled by each child. It illustrates a basic limitation when trying to extend the classification system by allowing two additional “probable” states. Due to the low number of criteria available, a substantial number of children is now classified into two classes. Although this limits the practical usefulness of this extension, it allows to illustrate the ability of the new index to define a continuum. The four groups of children differ in the mean values of the index but are substantially overlapping as shown in Figure 4.
Discussion
The cohort
The cohort included more girls than boys which has also been reported elsewhere for children with recurrent headache. [2, 22, 23] The distribution of sex and age is the same across the three types of headaches. Most of the children have been suffering for headache for a long time before entering the study, especially children in the migraine group. This supports the importance of being alert to children with headaches early in their life, to minimize the risk of lifelong recurrent suffering.
Kroner-Herwig et al. [12] conducted a study on 7–14–year-old German children, and they provided a diagnosis on migraine, tension-type headache, and non-classifiable headache, based on questionnaire data, like we did. In contrast to our study, this was a population-based study and not restricted to a certain severity. However, the distribution of the co-occurring symptoms between the three groups were somewhat similar to ours but with more symptoms related to migraine and non-classifiable headache than to tension-type headache.
Most of the children in our study were physically active with less than 10% not participating in sports. However, those not participating in sports may do a lot of active leisure time activities, which are not considered ‘sports’ and therefore not captured by the questionnaire. Interestingly, children in the tension-type headache group were least physically active but had less severe pain than the other two groups. According to the ICHD, tension-type headache is usually not aggravated by physical activity in contrast to migraine, and hence the assumption would be, that children with migraine were the least active, also since they have the highest level of pain. This contradiction could indicate that pain is not the most bothersome issue for children with headache, maybe the quality of the headache has a higher impact on daily life, or maybe physical activity prevents or diminishes tension-type headache.
This cohort consists of children with recurrent or chronic headaches. Nevertheless, only half of the children had consulted a general practitioner due to their headache, which was also found in the study by Kroner-Herwig et al. [12] In our study distinctly more children with migraine, (and to a lesser extent also non-classifiable headache) consulted a general practitioner or a pediatrician than children with tension-type headache. Interestingly, only 20% of the participants reported the child to have received treatment, but the medication rate was rather high with 90% of the children taking medicine, and more than 1/3 of the children using non-prescriptive medication more than once a week. The high medication use emphasizes the need for optimizing non-pharmacological means of preventing or treating headache, and to improve knowledge among both parents and healthcare practitioners. Overall, the frequencies with respect to the different variables related to seeking help indicate a great variation in whether and how parents seek help.
Classification of headaches
There can be several explanations for the high number (55%) of non-classifiable children in our study. One explanation is the challenge of classifying headaches in children using the available questionnaire-based data. Some of the ICHD criteria could not be checked, and for some we only had limited degree of information, which could mean that some headaches may meet the criteria for “probable migraine” or “probable tension-type headache”. An attempt to extend our classification system in this direction failed, as too few criteria could be applied. Part of the explanation for the substantial number of unclassifiable children could be co-existing headache types (mixed headaches) making a specific diagnosis difficult due to overlapping symptoms. [24, 25] However, other diagnoses might also be present in this patient population. One potential diagnosis could be medication overuse headache, which — considering the high use of non-prescriptive medication (more than 1/3 of the children in this cohort used non-prescriptive medicine one or more days a week, Table 3) — is highly likely. Another diagnosis could be cervicogenic headache. This might be an important diagnosis in this age group, where children are prone to frequent trauma. In the non-classifiable group, there were 20% with concussions, 64% with neck pain and 85% with decreased cervical ROM; the latter two frequencies were higher than the migraine and tension-type groups. According to the ICHD criteria, the cervicogenic headaches include several migrainous features (nausea, vomit, and photo/phonophobia), and for our cohort the co-occurring symptoms were generally more prevalent in the non-classifiable group than for tension-type headache. Unfortunately, we lack the necessary variables to define these two diagnoses in this study.
Furthermore, it can be challenging for parents and children to answer items related to pain (intensity, quality, and aggravation factors), which are highly relevant for distinguishing between migraine and tension-type headache. [17] In our study, the questionnaire was assumed to be filled out by the child and the parents together, but discrepancies in the grading of pain between a child and a parent have been reported elsewhere and is a common source of uncertainty in studies investigating paediatric pain [26–28], making the validity of the pain intensity variable uncertain.
The migraine-tension-type-index
An index based on a combination of severity and co-occurring symptoms appeared to be useful by allowing children to be placed on a continuum between tension-type headache and migraine rather that in dichotomized categories, thereby also taking mixed headaches into account. The index could indicate that the state of headache may be more fluent between diagnoses and not so distinctly defined.
Such an index could be advantageous as it allows for combination of headaches with overlapping symptoms, which is supported by the results shown in Table 4 and Fig. 4. Furthermore, it allows inclusion of all children into further investigations of the relevance of the migraine versus tension-type-headache distinction. We found the clearest association between the index and aggravation by sports, which is in line with the diagnostic criteria, stating that migraine often is aggravated by physical activity whereas tension-type headache is not. For the other variables, the associations were less clear, but lower index values were found for short-lasting episodes and higher values for long-lasting. This could imply that children with migraine are more affected than those with tension-type headache.
Further studies are necessary to explore the usability of such an index and it should be compared to the gold standard for headache classification to assess the potential utility. Hypothetically, if a certain cut point could be established in order to increase knowledge on appropriate treatment strategy, that could be very helpful for the clinician in charge. This seems especially important due to the high variation in management of headaches in this cohort. Given the known risk of medication overuse headache [29, 30] and the known side effects of migraine medications [31], it is important to end up with the most likely diagnosis, so the children in need of relevant medicine will receive it, and those who don’t will not.
Strengths and limitations
The basic limitation of the study was the lack of information on some of the criteria of the ICHD classification, possibly implying an imperfect classification. In contrast, we had information on many other aspects of interest in children suffering from headache. However, we are aware that there are weaknesses associated with using questionnaire data. It can never be as nuanced as an interview, where it would be possible to get more nuanced answers and thereby minimize the amount of non-classifiable headaches. The insights obtainable from this type of epidemiological research may, however, also inform the clinical setting characterized by one-to-one interviews.
This population is a selected sample of parents and children willing to participate in a trial and to receive chiropractic treatment and is therefore not directly generalizable. However, there were no fees involved and therefore participation was an option for everyone despite income.
This study included children with recurrent or chronic headaches. However, children with less serious headaches also requires attention since early prevention could decrease the prevalence of more serious cases and thereby have a huge impact on future health and quality of life. Since headaches in general are very common, the full picture is better achieved if we not only consider the most bothersome headaches. [32]
Conclusions
This study describes a selected cohort of children with recurrent headaches and highlights that they are quite severely affected, has a rather large intake of medication and that there is a great variation in management.
Although only questionnaire data could be used, requiring a modification of the ICHD criteria, it was feasible to distinguish between migraine and tension-type headaches in nearly half of the children. The large group of non-classifiable headaches might include probable migraines and probable tension-type headaches, as well as mixed, cervicogenic and medication overuse headaches. A migraine-tension-type-index can be generated allowing to include all children in the diagnostic assessment and may be used for further management decisions.
Given the risk of lifelong trajectories of recurrent headaches, good diagnostic tools are essential to explore the options of best possible care and management as early as possible.
Supplementary Material
Appendix 1: Headache in children: Baseline questionnaire
Appendix 2: See Table 5.
Appendix 3: See Table 6.
Appendix 4: See Table 7.
Appendix 5: See Table 8.Funding
This research was primarily funded by the Foundation for Chiropractic Research and Postgraduate Education (Grant no 09/2518). The Danish Migraine and Headache Society also made a financial contribution. The funding bodies did not have any influence on the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Authors and Affiliations
Chiropractic Knowledge Hub, Campusvej 55, 5230, Odense M, Denmark
Kristina Boe Dissing, Werner Vach, Henrik Wulff Christensen & Lise Hestbaek
Basel Academy, Spalenring 145, 4055, Basel, Switzerland
Werner Vach
Private Practice, Vivaldisvej 6, 9700, Brønderslev, Denmark
Susanne Lynge
University of Southern Denmark, Campusvej 55, 5230, Odense M, Denmark
Lise Hestbaek
Contributions
Conceptualization, SL and LH;
methodology, SL and LH and HWC;
formal analysis, KBD and WV;
investigation, SL;
writing—original draft preparation, KBD;
writing—review and editing, KBD;
project administration , HWC and LH;
funding acquisition , LH
All authors have read and agreed to the published version of the manuscript.
Ethical approval and consent to participate
The project was approved by the Regional Committee on Health Research Ethics for the Region of Northern Denmark (#N-20150025) and data were handled according to the General Data Protection Regulations. [33] The trial was registered with ClinicalTrials.gov (Identifier: NCT02684916). All parents were required to give written informed consent allowing their child to participate in the RCT and they were informed orally and in writing that participation in the trial was voluntary and that parents could withdraw their child from the trial at any time with no negative consequences for the child. All results were presented in aggregated form and no individuals could be identified. The study was conducted according to the Declaration of Helsinki. [34]
Competing interests
K.B.D. and L.H. and H.W.C. are supported partly by the Foundation for Chiropractic Research and Postgraduate Education; W.V.s work at the Basel Academy has been financed by the Chiropractic Knowledge Hub; S.L. and H.W.C. and K.B.D. are in private practice, treating the patients in question. No other relationships or activities that could appear to have influenced the submitted work.
References:
Singhi S, Jacobs H, Gladstein J.
Pediatric headache: where have we been and where do we need to be.
Headache. 2014;54(5):817–29.Nieswand V, Richter M, Gossrau G.
Epidemiology of Headache in Children and Adolescents-
Another Type of Pandemia
Curr Pain Headache Rep 2020 (Aug 25); 24 (10): 62Powers SW, Patton SR, Hommel KA, Hershey AD.
Quality of life in childhood migraines: clinical impact
and comparison to other chronic illnesses.
Pediatrics. 2003;112(1 Pt 1):e1-5.Termine C, Ozge A, Antonaci F, Natriashvili S, Guidetti V.
Overview of diagnosis and management of paediatric headache.
Part II: therapeutic management.
J Headache Pain. 2011;12(1):25–34.Pogliani L, Spiri D, Penagini F, Nello FD, Duca P, Zuccotti GV.
Headache in children and adolescents aged 6–18 years in northern Italy:
prevalence and risk factors.
Eur J Paediatr Neurol. 2011;15(3):234–40.Hetlevik O, Bjorna CH, Lundring IT, Gjesdal S.
Adolescents consulting general practitioners for psychological problems—
a nationwide, register-based study in Norway.
Fam Pract. 2019;36(1):77–83.Bektas O, Ugur C, Gencturk ZB, Aysev A, Sireli O, Deda G.
Relationship of childhood headaches with preferences in leisure time activities,
depression, anxiety and eating habits: a population-based, cross-sectional study.
Cephalalgia. 2015;35(6):527–37.Lateef TM, Merikangas KR, He J, Kalaydjian A, Khoromi S, Knight E, Nelson KB.
Headache in a National Sample of American Children:
Prevalence and Comorbidity
J Child Neurol 2009 (May); 24 (5): 536–543Jacobs H, Gladstein J.
Pediatric headache: a clinical review.
Headache. 2012;52(2):333–9.Hershey AD.
Pediatric headache: update on recent research.
Headache. 2012;52(2):327–32.Torres-Ferrus M, Vila-Sala C, Quintana M, Ajanovic S, Gallardo VJ, Gomez JB, et al.
Headache, comorbidities and lifestyle in an
adolescent population (The TEENs Study).
Cephalalgia. 2019;39(1):91–9.Kroner-Herwig B, Heinrich M, Morris L.
Headache in German children and adolescents:
a population-based epidemiological study.
Cephalalgia. 2007;27(6):519–27.Connelly M.
Recurrent pediatric headache: a comprehensive review.
Childrens’s Health Care. 2003;32(3):153–89.Larsson B, Sigurdson JF, Sund AM.
Long-term follow-up of a community sample
of adolescents with frequent headaches.
J Headache Pain. 2018;19(1):79.Headache Classification Committee of the International Headache Society
(IHS) The International Classification of Headache Disorders, 3rd edition.
Cephalalgia. 2018;38(1):1–211.Rossi LN, Vajani S, Cortinovis I, Spreafico F, Menegazzo L.
Analysis of the International Classification of Headache Disorders
for diagnosis of migraine and tension-type headache in children.
Dev Med Child Neurol. 2008;50(4):305–10.Wager J, Hirschfeld G, Zernikow B.
Tension-type headache or migraine?
Adolescents’ pain descriptions are of little help.
Headache. 2013;53(2):322–32.Battistella PA, Fiumana E, Binelli M, Bertossi E, Battista P, Perakis E, et al.
Primary headaches in preschool age children:
clinical study and follow-up in 163 patients.
Cephalalgia. 2006;26(2):162–71.Genizi J, Bugdnoskya V, Aboud A, Segal I, Assaf N, Srugo I, et al.
Migraine and tension-type headache among children and adolescents:
application of international headache society criteria in a clinical setting.
J Child Neurol. 2021;36(8):618–24.Lynge S, Hartvigsen J, Christensen HW, Vach W, Hestbaek L.
Effectiveness of Chiropractic Manipulation Versus Sham
Manipulation on Recurrent Headaches in Children Aged
7-14 Years, Protocol for a Randomized Clinical Trial
Chiropractic & Manual Therapies 2019 (Aug 23); 27: 40Lynge S, Dissing KB, Vach W, Christensen HW, Hestbaek L.
Effectiveness of Chiropractic Manipulation Versus Sham Manipulation
for Recurrent Headaches in Children Aged 7-14 Years -
A Randomised Clinical Trial
Chiropractic & Manual Therapies 2021 (Jan 7); 29: 1Gassmann J, Morris L, Heinrich M, Kroner-Herwig B.
One-year course of paediatric headache in children and adolescents aged 8–15 years.
Cephalalgia. 2008;28(11):1154–62.Wilkes MJ, Mendis MD, Bisset L, Leung FT, Sexton CT, Hides JA.
The prevalence and burden of recurrent headache in Australian adolescents:
findings from the longitudinal study of Australian children.
J Headache Pain. 2021;22(1):49.Kaniecki RG.
Migraine and tension-type headache: an assessment of challenges in diagnosis.
Neurology. 2002;58(9 Suppl 6):S15-20.Zebenholzer K, Wöber C, Kienbacher C, Wöber-Bingöl Ç.
Migrainous disorder and headache of the tension-type not fulfilling
the criteria: a follow-up study in children and adolescents.
Cephalalgia. 2000;20(7):611–6.Kamper SJ, Dissing KB, Hestbaek L.
Whose Pain Is It Anyway? Comparability of Pain Reports
From Children and Their Parents
Chiropractic & Manual Therapies 2016 (Aug 1); 24: 24Kroner-Herwig B, Morris L, Heinrich M, Gassmann J, Vath N.
Agreement of parents and children on characteristics of pediatric headache,
other pains, somatic symptoms, and depressive symptoms in an epidemiologic study.
Clin J Pain. 2009;25(1):58–64.Sundblad GM, Saartok T, Engstrom LM.
Child-parent agreement on reports of disease, injury and pain.
BMC Public Health. 2006;6:276.Chiappedi M, Balottin U.
Medication overuse headache in children and adolescents.
Curr Pain Headache Rep. 2014;18(4):404.Diener HC, Holle D, Solbach K, Gaul C.
Medication-overuse headache:
risk factors, pathophysiology and management.
Nat Rev Neurol. 2016;12(10):575–83.Whyte CA, Tepper SJ.
Adverse effects of medications commonly used in the treatment of migraine.
Expert Rev Neurother. 2009;9(9):1379–91.Krogh AB, Larsson B, Linde M.
Prevalence and disability of headache among
Norwegian adolescents: a cross-sectional school-based study.
Cephalalgia. 2015;35(13):1181–91.General Data Protection Regulation. 2016.
World Medical Association Declaration of Helsinki.
ethical principles for medical research involving human subjects.
JAMA. 2013;310(20):2191–4.Cole TJ, Bellizzi MC, Flegal KM, et al.
Establishing a standard definition for child overweight
and obesity worldwide: international survey.
BMJ. 2000;320(7244):1240–3.
https://doi.org/10.1136/bmj.320.7244.1240.
Return to HEADACHE
Return to PEDIATRICS
Since 1-31-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |