

Attitudes Towards Chiropractic:
A Repeated Cross-sectional Survey
of Canadian Family PhysiciansThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: BMC Family Practice 2021 (Sep 15); 22 (1): 188 ~ FULL TEXT
OPEN ACCESS Jason W. Busse, DC, PhD; Sushmitha Pallapothu, BSc; Brian Vinh, BSc; Vivienne Lee, BSc; Lina Abril, BSc; et. al.
Department of Health Research Methods,
Evidence, and Impact,
McMaster University,
Hamilton, ON, Canada.
Department of Anesthesia,
Michael G. DeGroote School of Medicine,
McMaster University,
HSC-2V9, 1280 Main St. West,
Hamilton, ON, L8S 4K1, Canada.
Background: Many primary care patients receive both medical and chiropractic care; however, interprofessional relations between physicians and chiropractors are often suboptimal which may adversely affect care of shared patients. We surveyed Canadian family physicians in 2010 to explore their attitudes towards chiropractic and re-administered the same survey a decade later to explore for changes in attitudes.
Methods: A 50-item survey administered to a random sample of Canadian family physicians in 2010, and again in 2019, that inquired about demographic variables, knowledge and use of chiropractic. Imbedded in our survey was a 20-item chiropractic attitude questionnaire (CAQ); scores could range from 0 to 80 with higher scores indicating more positive attitudes toward chiropractic. We constructed a multivariable regression model to explore factors associated with CAQ scores.
Results: Among eligible physicians, 251 of 685 in 2010 (37% response rate) and 162 of 2429 in 2019 (7% response rate) provided a completed survey. Approximately half of respondents (48%) endorsed a positive impression of chiropractic, 27% were uncertain, and 25% held negative views. Most respondents (72%) referred at least some patients for chiropractic care, mainly due to patient request or lack of response to medical care. Most physicians believed that chiropractors provide effective therapy for some musculoskeletal complaints (84%) and disagreed that chiropractic care was beneficial for non-musculoskeletal conditions (77%). The majority agreed that chiropractic care was a useful supplement to conventional care (65%) but most respondents (59%) also indicated that practice diversity among chiropractors presented a barrier to interprofessional collaboration. In our adjusted regression model, attitudes towards chiropractic showed trivial improvement from 2010 to 2019 (0.31 points on the 80-point CAQ; 95%CI 0.001 to 0.62). More negative attitudes were associated with older age (- 1.55 points for each 10-year increment from age 28; 95%CI - 2.67 to - 0.44), belief that adverse events are common with chiropractic care (- 1.41 points; 95% CI - 2.59 to - 0.23) and reported use of the research literature (- 6.04 points; 95% CI - 8.47 to - 3.61) or medical school (- 5.03 points; 95% CI - 7.89 to - 2.18) as sources of knowledge on chiropractic. More positive attitudes were associated with endorsing a relationship with a specific chiropractor (5.24 points; 95% CI 2.85 to 7.64), family and friends (4.06 points; 95% CI 1.53 to 6.60), or personal treatment experience (4.63 points; 95% CI 2.14 to 7.11) as sources of information regarding chiropractic.
There is more like this @ our:
COST-EFFECTIVENESS Section and the:
ALL ABOUT CHIROPRACTIC SectionConclusions: Although generally positive, Canadian family physicians' attitudes towards chiropractic are diverse, and most physicians felt that practice diversity among chiropractors was a barrier to interprofessional collaboration.
Keywords: Attitude of health personnel; Chiropractic; General practice; Interprofessional relations; Physicians; Survey; Surveys and questionnaires.
From the FULL TEXT Article:
Background
One in eight Canadians report attending a chiropractor in the past year, primarily for low back or neck pain [1, 2], and many patients receive care from both a family physician and a chiropractor during the course of their complaint. [3] Medicine and chiropractic, however, have a contentious history. [4] In 1972, the Canadian Medical Association reaffirmed its policy that physicians may not make referrals to chiropractors or acquire x-rays on behalf of chiropractors [5], and until 1983 the American Medical Association held that it was unethical for medical doctors to associate with chiropractors. [6] Some evidence suggests that integrated models of care, in which physicians and chiropractors work in the same clinic, enhance care coordination, referral between disciplines, and trust among providers. [7] Although family physicians have become more accepting of chiropractic [8, 9], current interprofessional relationships between family physicians and chiropractors remain suboptimal. [10–14]
Chiropractic in Canada exists on a spectrum. While most providers focus on management of musculoskeletal complaints, approximately 1 in 5 Canadian chiropractors adhere to vitalist traditions of chiropractic which maintain that malpositioned spinal vertebrae (subluxations) interfere with the nervous system causing disease. [15] Vitalist practitioners in Canada are more likely to hold anti-vaccination beliefs, less likely to adhere to guideline recommendations for use of radiographic imaging [15], and receive fewer referrals from physicians. [16] This schism within the profession has been longstanding [17], and some opinion leaders have argued for formally separating the chiropractic profession into evidence-based and vitalist factions. [18]
Many patients do not reveal their use of chiropractic to their primary care physician, in part over concerns of disapproval. [19] When patients do report receipt of chiropractic care, communication between physicians and chiropractors is often poor. [20] Understanding how family physicians view chiropractic may provide opportunities to enhance interprofessional relations and improve care of shared patients. The aim of the current study was to survey the attitudes of Canadian family physicians towards chiropractic in 2010 and re-administer the same survey a decade later to explore for changes in attitudes. We hypothesized that family physicians’ attitudes towards chiropractic would show improvement between survey administrations.
Methods
Questionnaire development
With the assistance of epidemiologists and content experts, and reference to the previous literature [8, 10, 21–23], we developed a 50-item, English and French-language questionnaire to examine family physicians’ attitudes towards chiropractic (Additional file 1). The final questionnaire provided response options as checkboxes, as a previous report has shown that closed-ended questions result in fewer incomplete questionnaires than open-ended formats. [24]
We pre-tested our survey with three family physicians, two clinicians with both medical and chiropractic training, and two chiropractors, to evaluate if the questionnaire adequately measured attitudes towards chiropractic, and if the individual questions adequately reflected the domains of formation of attitudes, referral practices, and impressions towards chiropractic. The pre-test participants also commented on the clarity and comprehensiveness of the questionnaire and the time required for completion.
Thirty survey questions requested demographic data from respondents and asked about their knowledge of chiropractic and referral practices for chiropractic care. The survey also included a 20-item chiropractic attitude questionnaire (CAQ). Each of the 20 questions comprising the CAQ was graded on a 5-point Likert scale (i.e., strongly agree, agree, undecided, disagree, strongly disagree), from 0 to 4. After re-coding so that all reply options were qualitatively in the same direction, the responses were summed to arrive at a total score ranging from 0 (most negative attitude towards chiropractic) to 80 (most positive attitude towards chiropractic). The internal consistency of the CAQ, using all respondents from both administrations, was high (Cronbach’s alpha, 0.83). The last item of the CAQ asked about the respondent’s general attitude towards chiropractic and served as an embedded validation question. The Spearman correlation between responses to this item and the total CAQ score (excluding the last question) was 0.85 (p < 0.01), further supporting construct validity of the CAQ.
Questionnaire administration
We used the 2009 Scott’s Canadian Medical Directory [25] to acquire a random sample of 1000 Canadian family physicians with a random-number generator. The Scott’s Directory contains telephone and fax numbers for physicians, but email addresses are infrequently provided. Between October and December 2010, all physicians’ offices were called to establish if they were in active practice, confirm a working fax number, and inquire if an English or French-language survey was preferred. Eligible physicians (those in active practice and for whom a working fax number was identified) were sent a survey by fax. Recipients were provided with a disclosure letter detailing the intent of the survey and explicit instructions that, should they choose not to complete the survey, they could provide this decision by fax or email to avoid further requests. Therefore, informed consent was implied if physicians provided a completed survey.
At 4 and 8 weeks following the initial survey, we re-faxed the questionnaire to all non-responders (i.e., those fax numbers from which we did not receive a completed survey) unless they indicated they did not wish to participate. We telephoned each office that received a 3rd (final) survey prior to faxing to encourage completion of the instrument, which has been shown to improve response rates. [26] Our survey was performed in accordance with the Declaration of Helsinki and approved by the Hamilton Integrated Research Ethics Board (project no. 10–305), and all methods were performed in accordance with relevant guidelines and regulations. [27]
We subsequently used the 2019 Scott’s Canadian Medical Directory [22] to acquire a random sample of 2996 Canadian family physicians selected using a computer-based random number generator. From September to November 2019, we administered the same 50-item survey to physicians in this sample who were in active practice and for whom we confirmed a working fax number, in the same manner as in 2010. The Hamilton Integrated Research Ethics Board granted approval for re-administration of our survey (project no. 7355).
Data management and storage
Members of our study team transferred information from surveys with single-key entry, as they were received, to an electronic database (SPSS) on a password-protected computer. Data was checked by a second team member for inconsistencies or unusual answers (e.g., age > 100). Once data was entered and verified, all paper surveys were shredded and disposed of.
Statistical analysis
We generated frequencies for all collected data and, for purposes of presentation, collapsed responses to individual CAQ items into agree (strongly agree + agree), undecided, and disagree (strongly disagree + disagree). We reported categorical data as proportions and continuous data as means and standard deviations (SDs) if normally distributed and as medians and interquartile ranges (IQRs) if not. To reduce the risk of spurious associations due to multiple testing, we identified any individual question within the CAQ in which the proportion of respondents who agreed or disagreed changed by ≥10% between the 2010 and 2019 survey administrations and used an independent samples Mann-Whitney U test to explore for statistical significance.
Based on previous surveys [28–30], we hypothesized, a priori, the following associations of respondents’ attitudes towards chiropractic:(1) older physicians would hold more negative attitudes;
(2) more positive attitudes if they saw a greater proportion of patients with musculoskeletal complaints;
(3) physician’s endorsing patient feedback, a relationship with a specific chiropractor, personal treatment experience, or feedback from family and friends as sources of information on chiropractic would hold more positive attitudes; and
(4) physician’s endorsing the scientific literature, professors, the media, or lectures during medical school as sources of information on chiropractic would hold more negative attitudes.We also hypothesized that re-administration of the survey in 2019 would show more positive attitudes versus the original administration in 2010. These variables were entered into a generalized linear model. The dependent variable, attitude towards chiropractic, was defined as the aggregate score of the CAQ. We calculated that we would require at least 110 completed surveys to ensure that our regression model was reliable (10 respondents for each independent variable considered). [31]
All comparisons were 2-tailed and an independent factor was considered statistically significant if it had a p-value < 0.05 in the final multivariable model. We report the unstandardized regression coefficient and 95% confidence interval (CI) for each variable in our regression model. The value of the unstandardized regression coefficient represents the change in response score on the 80-point CAQ. Multicollinearity was deemed concerning if the variance inflation factor for any independent variable was greater than five. [32] We performed all analyses using IBM SPSS 26.0 statistical software (Armonk, NY: IBM Corp).
Results
Characteristics of respondents
In 2010, among 685 of 1,000 family physicians who were in active practice and for whom we confirmed a working fax number and sent our survey, 251 returned a completed questionnaire (37% response rate; Additional file 1: Fig. 1). Among 2,429 eligible family physicians identified in 2019, 162 provided a completed survey for a 7% response rate (Additional file 1: Fig. 2).

Table 1 The mean age of respondents was 50 (SD 10) and 56% were men, although there was a higher prevalence of women in the more recent survey (40% in 2010 and 49% in 2019). Most respondents had been active clinically for > 20 years and worked in a community-based practice focused on general family medicine. Most physicians attended to patient populations of which > 30% presented with musculoskeletal complaints (Table 1).
Knowledge of and experience with chiropractic

Table 2 Respondents endorsed multiple sources of information regarding chiropractic, but feedback from their patients was the most common. Seventy-one percent of family physicians reported referring patients for chiropractic care and, among these, most referred ≤25 patients per year. Referrals were usually prompted by patient request (57%; 237 of 413) or non-response to medical treatment (40%; 166 of 413) (Table 2).
Only 13% of physicians (53 of 413) worked in a multidisciplinary environment where chiropractic care was available, and 40% (165 of 413) had sought chiropractic care for themselves. Most had not received information on chiropractic during their medical training, and the majority (80%) felt their education should (52%; 214 of 413) or possibly should (28%; 115 of 413) include such information. Most respondents’ opinions on chiropractic were formed after medical school (82%; 337 of 413), and most (51%; 209 of 413) described themselves as a little knowledgeable. In 2010, most respondents (52%) felt that adverse events were uncommon with chiropractic care, and in 2019 most physicians believed that adverse events were common but serious events were rare (47%). In 2010, most respondents (46%) were very comfortable discussing chiropractic with their patients, whereas in 2019 most (41%) were only somewhat comfortable (Additional file 1: Table 1).
Fifteen percent (62 of 413) of physicians felt that chiropractic care should be available in multidisciplinary settings (29% were unsure), and 25% felt that chiropractic should be available in hospitals, either with (17%; 69 of 413) or without (8%; 34 of 413) physician referral. Respondents varied on whether chiropractic care should be offset by government funding: 35% agreed, 33% were unsure, and 27% disagreed. Forty-three percent of family physicians definitely (17%) or somewhat (26%) perceived chiropractors as primary care providers, and most (81%; 335 of 413) wanted consultation notes from chiropractors who attended their patients. Seventy-five percent of respondents had received requests from chiropractors to refer patients for imaging studies. Most physicians (59%; 245 of 413) believed that practice diversity within the chiropractic profession was a barrier to interprofessional collaboration. (Additional file 1: Table 2).
Attitudes towards chiropractic
Forty-eight percent of family physicians (198 of 413) endorsed a positive impression of chiropractic, 27% were unsure, and 25% held negative views. Respondents endorsing a positive view had an average CAQ score of 50.2 out of 80 (SD 7.5), undecided respondents had an average CAQ score of 39.4 (SD 5.8), and physicians with negative impressions had a mean CAQ score of 24.9 (SD 9.1). An important change in continuous outcome measures can be estimated as half a SD of the aggregate score for a given population [33], and by this standard, a 6-point difference on the CAQ would be considered meaningful.

Table 3 Responses to individual items on the CAQ are provided in Table 3. Most physicians felt that chiropractors provide effective management for some musculoskeletal disorders (84%), that chiropractic was a useful supplement to medical care (65%), and chiropractors could reduce patient overload for family physicians (52%). Many physicians endorsed that chiropractors provide a patient-centred approach (45%) and use approaches from which medicine could benefit (43%). Alternately, most respondents disagreed that chiropractic was effective for non-musculoskeletal conditions (77%) and were unsure whether chiropractors treat in accordance with evidence-based practices (52%). Many felt that chiropractic manipulation of the neck was unsafe (47%) and 37% agreed that chiropractors provide patients with misinformation regarding vaccination.
There were 5 items on the CAQ in which the proportion of respondents who agreed or disagreed shifted by ≥10% between administrations in 2010 and 2019, of which three were statistically significant. Canadian family physicians surveyed in 2019 were more likely to:(1) disagree that chiropractors promote unnecessary treatment plans (28% in 2019 vs. 18% in 2010; p < 0.001),
(2) agree that chiropractors provide effective care for post-surgical rehabilitation (24% vs. 14%; p = 0.05), and
(3) agree that chiropractors treat in accordance with evidence-based practices (26% vs. 14%; p = 0.05).

Table 4 In our adjusted regression model, overall impressions towards chiropractic showed trivial improvement from 2010 to 2019 (0.31 points on the 80-point CAQ; 95%CI 0.001 to 0.62). More negative attitudes were associated with older age (– 1.55 points for each incremental decade from age 28; 95%CI – 2.67 to – 0.44), belief that adverse events are common with chiropractic care (– 1.41 points; 95% CI – 2.59 to – 0.23) and reported use of the research literature (– 6.04 points; 95% CI – 8.47 to – 3.61) or medical school (– 5.03 points; 95% CI – 7.89 to – 2.18) as a source of knowledge on chiropractic. More positive attitudes were associated with endorsing a relationship with a specific chiropractor (5.24 points; 95% CI 2.85 to 7.64), family and friends (4.06 points; 95% CI 1.53 to 6.60), or personal treatment experience (4.63 points; 95% CI 2.14 to 7.11) as sources of information regarding chiropractic. (Table 4) The variance inflation factor was less than 2 for each independent variable, suggesting no issues with multicollinearity. Our model explained approximately 26% of the variation (adjusted R2 = 0.26) in family physician’s attitudes toward chiropractic.
Discussion
Canadian family physician’s attitudes towards chiropractic have remained similar over the past decade. Most physicians held favourable perceptions of chiropractic, including the belief that chiropractic care is effective for some musculoskeletal complaints, provides a useful complement to conventional medicine, and can reduce family practitioner workload. However, attitudes are diverse, and respondents also highlighted several concerns, including uncertainty whether chiropractors provide evidence-base care, dependency on short-term symptom relief, and vaccine misinformation. The majority also agreed that practice diversity among chiropractors presented a barrier to interprofessional collaboration. Negative attitudes toward chiropractic care were associated with older age, belief that adverse events are common with chiropractic care, and reported use of the research literature or medical school as a source of knowledge on chiropractic. Endorsing a relationship with a specific chiropractor, family and friends, or personal treatment experience as sources of information were associated with more positive attitudes towards chiropractic.
Strengths and limitations
Strengths of our study include random sampling of all Canadian family physicians, and survey design and administration consistent with best practices. [27] Our assessment of attitudes towards chiropractic was based on the CAQ, which has been validated among other groups of Canadian healthcare providers. [28–30] Our study does have limitations, including an overall response rate of 13%, which was lower for the re-administration of the survey. Non-responders may have differed systematically from responders, and the generalizability of our findings to family physicians practicing outside of Canada is uncertain. Our model explained 26% of the variation in respondent’s attitudes toward chiropractic, indicating that there remain additional variables of importance that our survey did not capture.
Relevant literature
In August 2018, the Canadian Chiropractic Association (CCA) published a statement emphasizing a focus on promoting interprofessional collaboration [34], and the CCA advocates for integration of chiropractors into interprofessional health teams. [35] We found that although most Canadian family physicians endorse chiropractic care as a useful supplement to conventional medicine, only one in eight physicians reported working with a chiropractor, and practice diversity within the chiropractic profession was perceived as a barrier to interprofessional collaboration.
Most family physicians disagreed that chiropractic care was effective for non-musculoskeletal conditions, and systematic reviews on this topic have not found evidence to challenge this assertion. [36–39] Most respondents agreed that chiropractic care is effective for certain musculoskeletal complaints, and spinal manipulation, which is commonly provided by chiropractors, has received support for management of axial complaints from recent systematic reviews [40–45] and clinical practice guidelines. [46–48] Paradoxically, support from the scientific literature was a common reason given for referring patients for chiropractic care, while reliance on research literature for information on chiropractic was associated with more negative attitudes. Reasons for this disconnect are uncertain.
Close to half of respondents disagreed that chiropractic manipulation of the cervical spine was generally safe; however, although some observational studies have suggested a rare association with stroke [49–51], studies with greater methodologic safeguards against bias have failed to confirm either an association between greater utilization of chiropractic and risk of stroke [52], or an association between chiropractic care and an increased risk of stroke compared to care by primary care physicians. [53, 54] The associations reported in some studies between chiropractic care and stroke may be due to patients with early dissection-related symptoms seeking care prior to developing their strokes. [55–57]
Musculoskeletal complaints, particularly low back pain, are common in primary care. [58] Our findings suggest that most Canadian family physicians believe chiropractors can provide effective care for some musculoskeletal complaints; however, many physicians are uncertain whether chiropractors treat in accordance with evidence-based practices and have concerns regarding the safety of cervical manipulation. The chiropractic profession may help address such concerns by continuing to assess the concordance between evidence and practice [59–62] and promoting greater standardization of care where important variability exists. Further research on the benefits and harms of cervical manipulation is needed to establish the appropriate role of this modality. [63, 64]
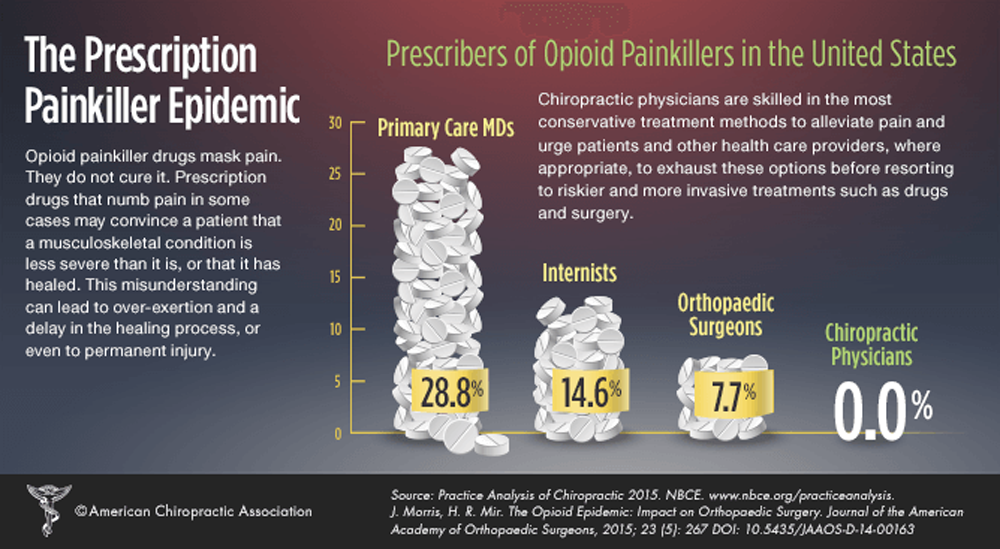
Despite the many challenges that exist, there are good reasons to pursue improved relations between chiropractors and family physicians; interprofessional collaboration among healthcare providers is associated with improved patient satisfaction and outcomes. [65, 66] Moreover, preliminary evidence suggests that collaboration between chiropractors and physicians for shared patients may reduce use of prescription medication, including opioids, unnecessary imaging studies, and inappropriate referrals for surgical consultation. [67, 68] Efforts to improve relations may benefit from increased opportunities for family physicians and chiropractors to work together and learn from each other. [7, 69, 70]
Conclusions
Although generally positive, Canadian family physicians’ attitudes towards chiropractic range from very positive to extremely negative, and most physicians acknowledge that practice diversity within the chiropractic profession presents a barrier to interprofessional collaboration. Efforts to improve relations could include providing evidence-based information on chiropractic during medical training, and increased opportunities for family physicians and chiropractors to interact.
Supplementary Information
Additional File 1 (80K, docx)
Acknowledgements
We regret to inform readers that Dr. Moore is recently deceased.
Authors’ contributions
JWB conceived and designed the study. SP, BV, VL, LA, AC, JJR, DV, MD, AB, SS, OM and MH called physicians’ offices and administered surveys. JWB carried out the statistical analysis. JWB, SP, BV, JJR, M-PH, IP, AM, CAG and DJP interpreted the data. JWB drafted the manuscript. All authors critically revised the article for important intellectual content and gave final approval for the article. The corresponding author attests that all listed authors meet authorship criteria.
Funding
Our 2010 survey was supported by a $2,500 research grant from the Ontario Chiropractic Association. The funding source had no role in the conduct of the study; the collection, management, analysis, or interpretation of the data; or the preparation or approval of the manuscript. We have no other conflicts of interest to declare.
Declarations
Ethics approval and consent to participate
Recipients were provided with a disclosure letter detailing the intent of the survey and explicit instructions that, should they choose not to complete the survey, they could provide this decision by fax or email to avoid further requests. Therefore, informed consent was implied if the questions were answered by the participants. The Hamilton Integrated Research Ethics Board granted approval of our survey in 2010 (project no. 10–305), and for re-administration of our survey in 2019 (project no. 7355).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References:
Beliveau PJH, Wong JJ, Sutton DA, Simon NB, Bussieres AE, Mior SA, et al.
The Chiropractic Profession: A Scoping Review of Utilization Rates,
Reasons for Seeking Care, Patient Profiles, and Care Provided
Chiropractic & Manual Therapies 2017 (Nov 22); 25: 35Lawrence, DJ and Meeker, WC.
Chiropractic and CAM Utilization: A Descriptive Review
Chiropractic & Osteopathy 2007 (Jan 22); 15: 2Bath B, Lawson J, Ma D, et al.
Self-reported Use of Family Physician, Chiropractor and Physiotherapy Services
Among Adult Canadians with Chronic Back Disorders: An Observational Study
BMC Health Serv Res 2018 (Dec 17); 18 (1): 970Sutherland DC.
The development of chiropractic in the Canadian health care system.
JCCA. 1993;37:164–176Geekie DA.
CMA’s slashing attack on chiropractors.
CMAJ. 1972;107:73–75Wilk v. American Medical Association,
895 F.2d 352 (7th Cir. 1990)Davis MA, McDevitt L, Alin K.
Establishing a chiropractic service in a rural primary health care facility.
J Altern Complement Med. 2007;13:697–702. doi: 10.1089/acm.2007.7199Cherkin D, MacCornack FA, Berg AO.
Family physicians’ views of chiropractors: hostile or hospitable?
Am J Public Health. 1989;79:636–637. doi: 10.2105/AJPH.79.5.636Greene B, Smith M, Allareddy V, Haas M.
Referral patterns and attitudes of Primary Care Physicians towards chiropractors.
BMC Complement Altern Med. 2006;6:5. doi: 10.1186/1472-6882-6-5Greene BR, Smith M, Allareddy V, Haas M.
Referral patterns and attitudes of primary care physicians towards chiropractors.
BMC Complement Altern Med. 2006;6:5–15. doi: 10.1186/1472-6882-6-5Allareddy V, Greene BR, Smith M, Haas M, Liao J.
Facilitators and barriers to improving interprofessional referral
relationships between primary care physicians and chiropractors.
J Ambul Care Manage. 2007;30:347–354. doi: 10.1097/01.JAC.0000290404.96907.e3Mainous AG, 3rd, Gill JM, Zoller JS, Wolman MG.
Fragmentation of patient care between chiropractors and family physicians.
Arch Fam Med. 2000;9:446–450. doi: 10.1001/archfami.9.5.446Penney LS, Ritenbaugh C, Elder C, Schneider J, Deyo RA, DeBar LL.
Primary Care Physicians, Acupuncture and Chiropractic Clinicians,
and Chronic Pain Patients: A Qualitative Analysis of
Communication and Care Coordination Patterns
BMC Complement Altern Med. 2016 (Jan 25); 16: 30Jensen CB.
The Intraprofessional continuum and cleft.
Integr Med (Encinitas) 2016;15:36–40McGregor M, Puhl AA, Reinhart C, Injeyan HS, Soave D.
Differentiating intraprofessional attitudes toward paradigms in health care delivery
among chiropractic factions: results from a randomly sampled survey.
BMC Complement Altern Med. 2014;14:51. doi: 10.1186/1472-6882-14-51Blanchette MA, Rivard M, Dionne CE, Cassidy JD.
Chiropractors' characteristics associated with physician referrals:
results from a survey of Canadian doctors of chiropractic.
J Manip Physiol Ther. 2014;38(6):395–406. doi: 10.1016/j.jmpt.2014.11.001Meeker, W., & Haldeman, S. (2002).
Chiropractic: A Profession at the Crossroads of Mainstream and Alternative Medicine
Annals of Internal Medicine 2002 (Feb 5); 136 (3): 216–227Leboeuf-Yde, C., Innes, S.I., Young, K.J., Kawchuk, G.N., et. al.
Chiropractic, One Big Unhappy Family: Better Together or Apart?
Chiropractic & Manual Therapies 2019 (Feb 21); 27: 4Eisenberg DM, Kessler RC, Van Rompay MI, Kaptchuk TJ, Wilkey SA, Appel S, Davis RB.
Perceptions among complementary therapies relative to conventional therapies
among adults who use both: results from a national survey.
Ann Intern Med. 2001;135:344–351. doi: 10.7326/0003-4819-135-5-200109040-00011Peter Morrison,
Adjusting the Role of Chiropractors in the United States: Why Narrowing
Chiropractor Scope of Practice Statutes Will Protect Patients, 19 Health Matrix 493 (2009) (Available at:
https://scholarlycommons.law.case.edu/healthmatrix/vol19/iss2/21;
Accessed 5 Feb 2021)Marja J. Verhoef and Stacey a page.
Physicians’ perspectives on chiropractic treatment.
JCCA. 1996;40:214–219Reiter HH.
Some physicians’ perceptions of chiropractors, osteopaths, and podiatrists.
Percept Mot Skills. 1965;20(suppl):1167–1168. doi: 10.2466/pms.1965.20.3c.1167King-Isaacs D, Lichti J, Newton-Leo L.
Knowledge and opinions of Downsview physicians regarding the chiropractic profession.
JCCA. 1994;38:90–97Griffith LE, Cook DJ, Guyatt GH, Charles CA.
Comparison of open and closed questionnaire formats in obtaining
demographic information from Canadian general internists.
J Clin Epidemiol. 1999;52:997–1005. doi: 10.1016/S0895-4356(99)00106-7Scott’s Directories (Available at:
https://www.scottsdirectories.com/canadian-directories/canadian-medical-directory/
; Accessed 5 Feb 2021).Nakash RA, Hutton JL, Jørstad-Stein EC, et al.
Maximising response to postal questionnaires: a systematic review
of randomised trials in health research.
BMC Med Res Methodol. 2006;6:5. doi: 10.1186/1471-2288-6-5Burns KE, Duffett M, Kho ME, et al.
A guide for the design and conduct of self-administered surveys of clinicians.
CMAJ. 2008;179:245–252. doi: 10.1503/cmaj.080372Busse JW, Jacobs C, Ngo T, et al.
Attitudes toward chiropractic: a survey of North American orthopedic surgeons.
Spine (Phila Pa 1976); 34: 2818–25Weis CA, Cheung G, Dion L, et al.
Attitudes towards chiropractic: A survey of Ontario midwives.
Podium presentation at the DC 2017. Washington. March 15-18, 2017.Weis CA, Stuber K, Nash J, et al.
Attitudes towards chiropractic: a survey of Canadian obstetricians.
J Evid Based Complementary Altern Med. 2016;21:92–104. doi: 10.1177/2156587215604073Harrell FE.
Multivariate modeling strategies.
In: Harrell FE, editor. Regression modeling strategies with applications
to linear models, logistic regression and survival analysis.
New York: Springer; 2001. pp. 53–85Belsley DA, Kuh E, Welsch RE.
Regression diagnostics: identifying influential data and sources of collinearity.
New York: John Wiley & Sons; 1980Norman GR, Sloan JA, Wyrwich KW.
Interpretation of changes in health related quality of life:
the remarkable universality of half a standard deviation.
Med Care. 2003;41:582–592Canadian Chiropractic Association.
Interprofessional Collaboration (Available at:
https://chiropractic.ca/about-cca/code-of-ethics/inter-professional-collaboration/
; Accessed 5 Feb 2021).Canadian Chiropractic Association.
Advocacy (Available at:
https://chiropractic.ca/about-cca/advocacy/
; Accessed 5 Feb 2021).Bronfort G, Haas M, Evans R, Leiniger B, Triano J.
Effectiveness of Manual Therapies: The UK Evidence Report
Chiropractic & Osteopathy 2010 (Feb 25); 18 (1): 3Huang T, Shu X, Huang YS, Cheuk DK.
Complementary and miscellaneous interventions for nocturnal enuresis in children.
Cochrane Database Syst Rev. 2011;12:CD005230Hondras MA, Linde K, Jones AP.
Manual Therapy for Asthma
Cochrane Database Syst Rev. 2005;2:CD001002Côté P, Hartvigsen J, Axén I, et al.
The global summit on the efficacy and effectiveness of spinal manipulative therapy
for the prevention and treatment of non-musculoskeletal disorders:
a systematic review of the literature.
Chiropr Man Therap. 2021;29:8Paige NM, Myiake-Lye IM, Booth MS, et al.
Association of Spinal Manipulative Therapy with Clinical Benefit and Harm
for Acute Low Back Pain: Systematic Review and Meta-analysis
JAMA. 2017 (Apr 11); 317 (14): 1451–1460Rubinstein SM, de Zoete A, van Middelkoop M, et al.
Benefits and Harms of Spinal Manipulative Therapy for the Treatment
of Chronic Low Back Pain: Systematic Review and Meta-analysis
of Randomised Controlled Trials
British Medical Journal 2019 (Mar 13); 364: l689Masaracchio M, Kirker K, States R, Hanney WJ, Liu X, Kolber M.
Thoracic spine manipulation for the management of mechanical neck pain:
a systematic review and meta-analysis.
PLoS One. 2019;14:e0211877. doi: 10.1371/journal.pone.0211877Shekelle PG, Paige NM, Miake-Lye IM, Beroes JM, Booth MS, Shanman R.
The Effectiveness and Harms of Spinal Manipulative Therapy for the Treatment of
Acute Neck and Lower Back Pain: A Systematic Review [Internet].
Washington (DC): Department of Veterans Affairs (US); 2017 PMID: 28704021.Fernandez M, Moore C, Tan J, Lian D, Nguyen J, Bacon A, Christie B, Shen I, Waldie T, Simonet D, Bussières A.
Spinal manipulation for the management of cervicogenic headache:
a systematic review and meta-analysis.
Eur J Pain. 2020;24:1687–1702. doi: 10.1002/ejp.1632Kolber MR, Ton J, Thomas B, Kirkwood J, Moe S, Dugré N, Chan K, Lindblad AJ, McCormack J, Garrison S, Allan GM, Korownyk CS, Craig R, Sept L, Rouble AN, Perry D.
PEER systematic review of randomized controlled trials:
management of chronic low back pain in primary care.
Can Fam Physician. 2021;67:e20–e30National Institute for Health and Care Excellence (NICE):
Low Back Pain and Sciatica in Over 16s: Assessment and Management (PDF)
NICE Guideline, No. 59 2016 (Nov): 1–1067Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530North American Spine Society (NASS)
Evidence-Based Clinical Guidelines for Multidisciplinary Spine Care:
Diagnosis & Treatment of Low Back Pain. 2020Ernst E.
Manipulation of the cervical spine: a systematic review of
case reports of serious adverse events, 1995–2001.
Med J Aust. 2002;176:376–380. doi: 10.5694/j.1326-5377.2002.tb04459.xRothwell DM, Bondy SJ, Williams JI.
Chiropractic Manipulation and Stroke: A Population-based Case-control Study
Stroke 2001 (May); 32 (5): 1054-1060Smith WS, Johnston SC, Skalabrin EJ, et al.
Spinal manipulative therapy is an independent risk factor for
vertebral artery dissection.
Neurology. 2003;60:1424–1428. doi: 10.1212/01.WNL.0000063305.61050.E6Boyle E, Côté P, Grier AR, Cassidy JD.
Examining vertebrobasilar artery stroke in two Canadian provinces.
Spine (Phila Pa 1976) 2008;33(4 Suppl):S170–S175. doi: 10.1097/BRS.0b013e31816454e0Cassidy JD, Boyle E, Cote P, et al.
Risk of Vertebrobasilar Stroke and Chiropractic Care: Results of
a Population-based Case-control and Case-crossover Study
J Stroke Cerebrovasc Dis. 2017;26:842–850Cassidy JD, Boyle E, Cote P, et al.
Risk of Vertebrobasilar Stroke and Chiropractic Care: Results of
a Population-based Case-control and Case-crossover Study
Spine (Phila Pa 1976) 2008 (Feb 15); 33 (4 Suppl): S176–183Arnold M, Bousser M.
Clinical manifestations of vertebral artery dissection.
Front Neurol Neurosci. 2005;20:77–86. doi: 10.1159/000088152Moser N, Mior S, Noseworthy M, Côté P, Wells G, Behr M, Triano J.
Effect of cervical manipulation on vertebral artery and cerebral haemodynamics
in patients with chronic neck pain: a crossover randomised controlled trial.
BMJ Open. 2019;9:e025219. doi: 10.1136/bmjopen-2018-025219Futch D, Schneider MJ, Murphy D, Grayev A.
Vertebral artery dissection in evolution found during chiropractic examination.
BMJ Case Rep. 2015; 2015: bcr2015212568Finley CR, Chan DS, Garrison S, Korownyk C, Kolber MR, Campbell S, Eurich DT, Lindblad AJ, Vandermeer B, Allan GM.
What are the most common conditions in primary care?
Systematic review. Can Fam Physician. 2018;64:832–840Shekelle PG, Coulter I, Hurwitz EL, Genovese B, Adams AH, Mior SA, Brook RH.
Congruence Between Decisions To Initiate Chiropractic Spinal Manipulation
For Low Back Pain and Appropriateness Criteria in North America
nnals of Internal Medicine 1998 (Jul); 129 (1): 9-17Grod JP, Sikorski D, Keating JC., Jr
Unsubstantiated claims in patient brochures from the largest state,
provincial, and national chiropractic associations and research agencies.
J Manip Physiol Ther. 2001;24:514–519. doi: 10.1067/mmt.2001.118205Herman PM, Vernon H, Hurwitz EL, Shekelle PG, Whitley MD, Coulter ID.
Clinical Scenarios for Which Cervical Mobilization and Manipulation
Are Considered by an Expert Panel to Be Appropriate (and Inappropriate)
for Patients with Chronic Neck Pain
Clin J Pain 2020 (Apr); 36 (4): 273–280The Canadian Chiropractic Guideline Initiative. (Available at:
https://www.ccgi-research.com/
; Accessed 5 February 2021).Wand BM, Heine PJ, O'Connell NE.
Should we abandon cervical spine manipulation for mechanical neck pain? Yes
BMJ. 2012;344:e3679. doi: 10.1136/bmj.e3679Cassidy JD, Bronfort G, Hartvigsen J.
Should we abandon cervical spine manipulation for mechanical neck pain? No
BMJ. 2012;344:e3680. doi: 10.1136/bmj.e3680Pascucci D, Sassano M, Nurchis MC, Cicconi M, Acampora A, Park D, Morano C, Damiani G.
Impact of interprofessional collaboration on chronic disease management:
findings from a systematic review of clinical trial and meta-analysis.
Health Policy. 2021;125:191–202. doi: 10.1016/j.healthpol.2020.12.006.Lutfiyya MN, Chang LF, McGrath C, Dana C, Lipsky MS.
The state of the science of interprofessional collaborative practice:
a scoping review of the patient health-related outcomes based
literature published between 2010 and 2018.
PLoS One. 2019;14:e0218578. doi: 10.1371/journal.pone.0218578Mior S, Gamble B, Barnsley J, Côté P, Côté E.
Changes in Primary Care Physician's Management of Low Back Pain
in a Model of Interprofessional Collaborative Care:
An Uncontrolled Before-After Study
Chiropractic & Manual Therapies 2013 (Feb 1); 21 (1): 6Zarrabian M, Bidos A, Fanti C, Young B, Drew B, Puskas D, Rampersaud R.
Improving spine surgical access, appropriateness and efficiency
in metropolitan, urban and rural settings.
Can J Surg. 2017;60:342–348. doi: 10.1503/cjs.016116.Spaulding EM, Marvel FA, Jacob E, Rahman A, Hansen BR, Hanyok LA, et al.
Interprofessional education and collaboration among healthcare students
and professionals: a systematic review and call for action.
J Interprof Care. 2019:1–10.Medicine Health Care Practitioners' Perspectives on Interprofessional Communication:
A Qualitative Rapid Review.
Medicina (Kaunas) 2019;55:650. doi: 10.3390/medicina55100650.
Return to COST-EFFECTIVENESS
Return to ALL ABOUT CHIROPRACTIC
Return to INITIAL PROVIDER/FIRST CONTACT
Since 1-14-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |