

Initial Integration of Chiropractic Services into
a Provincially Funded Inner City Community
Health Centre: A Program DescriptionThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Can Chiropr Assoc 2015 (Dec); 59 (4): 363–372 ~ FULL TEXT
OPEN ACCESS Steven R. Passmore, DC, PhDm Audrey Toth, DC, Joel Kanovsky, DC. Gerald Olin, BSc, DC
University of Manitoba,
College of Rehabilitation Sciences;
University of Manitoba,
Faculty of Kinesiology & Recreation Management.
Background: The burden of fees for chiropractic services rendered often falls on the patient and must be provided out-of-pocket regardless of their socioeconomic status and clinical need. Universal healthcare coverage reduces the financial barrier to healthcare utilization, thereby increasing the opportunity for the financially disadvantaged to have access to care. In 2011 the Canadian Province of Manitoba initiated a pilot program providing access to chiropractic care within the Mount Carmel Clinic (MCC), a non-secular, non-profit, inner city community health centre.
Objective: To describe the initial integration of chiropractic services into a publically funded healthcare facility including patient demographics, referral patterns, treatment practices and clinical outcomes.
Method: A retrospective database review of chiropractic consultations in 2011 (N=177) was performed.
Results: The typical patient referred for chiropractic care was a non-working (86%), 47.3 (SD=16.8) year old, who self-identified as Caucasian (52.2%), or Aboriginal (35.8%) and female (68.3%) with a body mass index considered obese at 30.4(SD=7.0). New patient consultations were primarily referrals from other health providers internal to the MCC (71.2%), frequently primary care physicians (76%). Baseline to discharge comparisons of numeric rating scale scores for the cervical, thoracic, lumbar, sacroiliac and extremity regions all exceeded the minimally clinically important difference for reduction in musculoskeletal pain. Improvements occurred over an average of 12.7 (SD=14.3) treatments, and pain reductions were also statistically significant at p<0.05.
Conclusion: Chiropractic services are being utilized by patients, and referring providers. Clinical outcomes indicate that services rendered decrease musculoskeletal pain in an inner city population.
Keywords: chiropractic; low-income population; multidisciplinary; musculoskeletal; populations, underserved; program description; spinal manipulation.
From the FULL TEXT Article:
Introduction
A predominant reason for seeking healthcare is for the treatment of back pain. [1] The lifetime prevalence of back pain, specifically low back pain, for the general population is thought to be as high as 84%, with up to 48.9% of affected individuals experiencing pain in the previous 6 months. [2, 3] Chiropractors are healthcare providers that deliver conservative non-pharmacological, and non-surgical management of mechanical muscle and joint pain, most typically back pain. [4] Chiropractors do not oppose pharmacological or surgical treatment options when such approaches are clinically necessary. [5] Chiropractic intervention targets the muscles and joints, using manual and physical procedures, most commonly including manipulation, massage, exercise and nutrition. [6] Typically chiropractic patients report high levels of satisfaction with care. [7] Chiropractic services are considered relatively cost effective. [8, 9] Chiropractic intervention is considered safe, as there are a low number of adverse events that occur directly as a result of treatment. [10]
Low-income populations utilize chiropractic care less than the general population. [11] The financially disadvantaged must carefully manage their limited economic resources. Engaging in a course of chiropractic care typically involves financial consideration as it is excluded from many public and private health insurance plans. [12] Out of pocket expense for healthcare forces low income individuals to weigh the costs and benefits of healthcare against their other basic necessities of life. [12] The poor are more likely to utilize healthcare services when they can be provided by a universal healthcare system. The reason is that universal healthcare coverage reduces the financial barrier to healthcare utilization. [13, 14]
A lower income results in a greater propensity toward having unmet healthcare needs in both Canada and the United States. [15] A possible reason, at least in Canada, is that healthcare services such as dentistry, optometry, physical therapy and chiropractic are largely not reimbursed by provincial healthcare plans. Delisted services, that were previously partially covered, have specifically been less accessed by the lowest income groups of the population. [14] User fees are the barrier to utilization of services for chiropractic and optometry, according to a study on the provision of free supplemental health care benefits for low-income families. [16] The result is that in order to be provided with reimbursement for services such as chiropractic, patients require coverage from a worker’s compensation board, motor vehicle accident insurance provider, or other supplemental health insurance benefits provided by an employer. Without healthcare coverage, the burden of fee for services rendered falls on the patient and must be provided out-of-pocket regardless of their socioeconomic status and clinical need.
In 2011, the Mount Carmel Clinic (MCC), a provincially funded health centre in Winnipeg, Manitoba, Canada implemented fully government subsidized chiropractic services, alongside its existing medical and dental services. The public funding of the chiropractic clinic addresses an issue raised by Soklaridis, Kelner, Love and Cassidy (2009) regarding the typical lack of funding allocated by the Canadian healthcare system toward complementary and alternative medicine. [17] Manitoba Health Family Services is demonstrating an interest in exploring universal and equitable access to health care that includes chiropractic services for underprivileged Manitobans.
The MCC serves a demographic of the poor and under-served within Winnipeg, specifically an area with the highest unemployment rate, and lowest average family income in the city. Since the chiropractic clinic was implemented a prospective quality assurance (QA) database has been maintained by the on-site chiropractors in collaboration with the administration at the MCC. The purpose of maintaining a prospective QA database is that the data can be used to evaluate service utilization, and relevant impacts of clinic implementation. [18] The purpose of this manuscript is to evaluate what the outcome of the initial integration has been in the first year of a publically funded inner city chiropractic clinic integrated within a multidisciplinary health centre targeting the poor and underserved.
Methods
The study utilized a cross-sectional, retrospective examination of prospectively collected QA data attained from the MCC chiropractic clinic database. All data were collected during calendar year 2011. The database is maintained at the MCC by the chiropractic clinicians on site. A university-based researcher, with a clinical background, summarized all data. Patient data was completely de-identified upon entry into an anonymous database prior to analysis and interpretation. Permission to conduct the study of the database was attained from the officer of records at the MCC as well as the University of Manitoba Health Research Ethics Board.

Table 1 The MCC is a provincially funded, non-secular, non-profit, inner city multidisciplinary community health centre located centrally in Winnipeg, Manitoba, Canada. The MCC chiropractors receive an hourly wage, on par with physician pay grade as approved by Manitoba Health. There is no financial incentive to see patients for a longer course of care than the minimum clinically warranted to induce difference, or long enough to determine that their presentation does not respond to chiropractic care and an appropriate referral can be identified. The two chiropractors are part-time independent contractors, each spending 1–day per week at the clinic. Services that the chiropractors at the MCC provide are summarized in Table 1.
New patients referred to the clinic received a new patient assessment and then either underwent informed consent procedures to initiate a course of chiropractic management, or were referred to another appropriate health care provider if chiropractic intervention was not clinically warranted. Follow up visits during a typical course of care included spinal or extremity joint manipulation and/ or mobilization, soft tissue therapy, and potentially other modalities including contemporary medical acupuncture. Re-evaluation visits were scheduled after every 4–6 treatment visits to assess whether patients were responding to care, not responding to care, or had reached a plateau in therapeutic response to intervention. Time slot durations for new patient assessments, re-evaluations, and follow up visit time duration allotments were designed by the clinicians in tandem with the MCC. Typical new patient assessments were scheduled for 30–60 minutes, while treatment visits and re-evaluation visits were 15–30 minutes in duration.
Analysis
Analysis of reported data consists of interpretation of raw numbers, and percentages of respondents to items from the database. Most unique patients (N=177) attended the clinic on multiple occasions, which is why the completed treatment visit total is 1,803. Any discrepancies between the number of patients in the study (N=177), and the numbers used for comparison to derive percentages, is due to participants choosing to abstain from a question, or if the course of care was completed (from intake to discharge) during calendar year 2011.
Paired two-tailed Student’s T-tests were used for analysis comparing baseline, and discharge outcome measures. Specifically, separate analyses were performed for the numeric rating scale (NRS) scores of completed courses of management that were targeted to the cervical, thoracic, lumbar, sacroiliac, and extremity regions. Some patients had multiple regions of complaint, and treatment and thus reported separate NRS scores for each region. Raw NRS point change, and percentages of baseline at discharge changes were also reported.
Results

Table 2 Female patients represented just over two-thirds (68.3%) of patient treatment visits at the MCC chiropractic clinic. While there was a diverse range for ages of patients, that data is skewed toward the aging population, with 48.9% of all treatment visits going to patients 51 years of age or older. Patients self reported their height and weight, which facilitated body mass index (BMI) calculation. The average BMI was 30.4 (SD=7.0) based on 120 unique respondents, which is considered obese. Of all unique patients who visited the chiropractic clinic, 91/177 (54.8%) patients had a BMI < 30 and were not considered obese. Patients were asked to voluntarily self-identify their ethnic background. While a full spectrum of cultural backgrounds were reported Caucasian, and Aboriginal individuals made up 52.2% and 35.8% of the clinic’s population respectively. Details of the specific breakdown of all collected patient demographic data can be found in Table 2. Patients not currently working (86%) utilized the majority of chiropractic clinic visits. Only 9 of 161 (6.0%) of new patients who completed treatment required new radiographs that were not already in their medical record, prior to initiating a course of care. A typical course of care from intake to discharge on average consisted of 12.7 (SD=14.3) treatment visits based on 160 completed cases in calendar year 2011.
Of appointments scheduled 74.5% (1763/2365) of total clinic visits were kept, presently there is no penalty for failing to attend a scheduled visit. Only 2.9% (52/1803) of patient visits to the clinic were unscheduled “walk-ins”. When patients were asked if their “initial chiropractic visit saved them from making an additional PCP visit” of the 161 respondents, 132 (82.0%) stated “yes” it did. When discharged from chiropractic only 7 (4.0%) of 161 respondents required referral to another healthcare provider for additional care.

Table 3
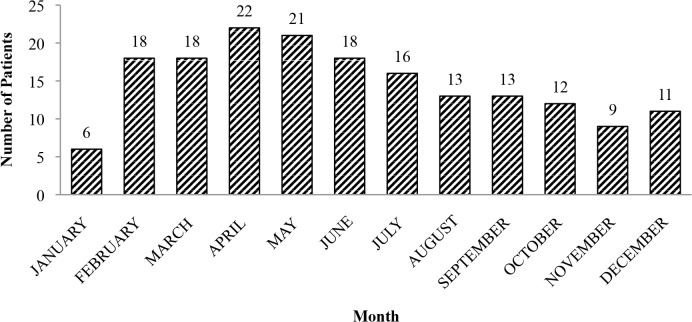
Figure 1
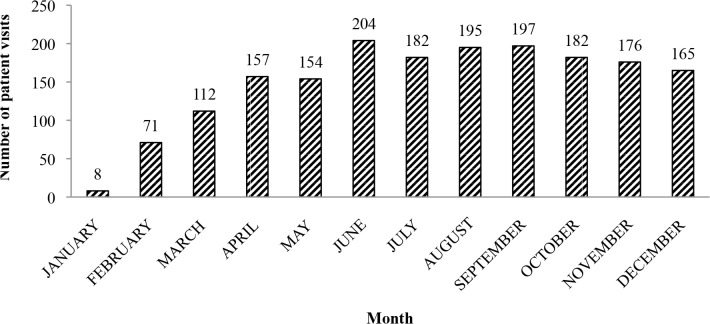
Figure 2

Table 4

Table 5

Table 6 Referral by other healthcare providers on-site within the MCC made up the majority (71.2%) of new patients at the chiropractic clinic (Table 3). Referral by healthcare providers from outside of the MCC consisted of a small number of patients (4.0%). Primary care physicians were the greatest referral source from healthcare providers (76.0%).
During the first four months of clinic operation both new patient visits (Figure 1), and total patient visits (Figure 2) increased steadily. During the final five months of the year it appeared that a steady state of clinic operation had been reached. There was a mean of 14.8 new patients (177/12) per month, and 135.5 ([1803-177]/12) follow-up visits per month during the inaugural clinic year.
There were consistently more patients seeking management for chronic conditions (symptoms >3 months in duration) as revealed by examination of the ratio of acute to chronic condition patients (Table 4). For those with acute pain seeking treatment, there was a relatively even distribution of patients by spinal region with the exception of those with sacroiliac joint pain who were substantially fewer in number (8.0%) (Table 4). For patients with chronic pain seeking treatment, the fewest number of patients had extremity region pain (13.0%), while the greatest proportion of patients sought care for pain in the lumbar region (26.8%).
Patients who received high-velocity low-amplitude (HVLA) joint manipulation, mobilization, and soft tissue intervention, had those interventions directed most often toward the thoracic and lumbar spinal regions followed by the cervical region (Table 5). Similar numbers of patients received HVLA joint manipulation, mobilization, and soft tissue intervention to the same treatment regions, likely due to the multifaceted nature of chiropractic intervention (Table 5). Contemporary medical acupuncture when used (48 cases) was most commonly targeted toward the cervical (16/48 cases; 33.3%) and extremity (14/48 cases; 29.2%) regions. The greatest use of other care modalities within a course of chiropractic management were those directed toward the lumbar spine (67 cases; 25.4%) and the sacroiliac regions (62; 23.5%).
Statistically, all five regions assessed by the NRS demonstrated significant improvement when comparing baseline and follow up scores for a completed course of management. Beyond statistical significance, when considering clinical populations the minimally clinically important difference (MCID) is an important and meaningful metric. According to Salaffi et al. (2004), the MCID for chronic musculoskeletal pain is a NRS change of –15.0% or at least –1 point. [19] A change of –33.0% or at least –2 points is associated with a patient reporting they feel “much better”. Based on the NRS data collected from baseline compared to discharge all four spinal (cervical, thoracic, lumbar, and sacroiliac) and the extremity regions responded to chiropractic intervention in excess of a MCID (Table 6). In terms of percent improvement, a course of care directed to the extremity regions attained improvement beyond 33.0% (Table 6). In terms of point change, the LS, SI and extremity regions (Table 6) all demonstrated change beyond 2 points, an improvement associated with patients feeling “much better”, following chiropractic intervention. Upon completion of a course of care of 161 chiropractic cases, 154 (96%) did not warrant referral to another healthcare provider.
Discussion
While the integration of chiropractic care into an inner city government funded multidisciplinary healthcare facility is relatively novel, there are isolated examples that can be used for comparison. For example integration of chiropractic services occurred a decade ago within the United States Veterans Health Administration, and a unique community health centre example in the province of Ontario, Canada. The characteristics of a typical MCC chiropractic patient differ drastically from those who are seen in a United States Veterans Affairs hospital chiropractic clinic most notably in age and gender representation. The typical veteran chiropractic patient was a 54.8 (SD=15.9) year old male (88.4%). [20] MCC patients referred for chiropractic care were typically 47.3 (SD=16.8) year old females (68.3%), who self identified as Caucasian (52.2%), or Aboriginal (35.8%) and non-working (86%) (Table 2). The MCC chiropractic patient population more closely resembled the Southern Ontario Community Health Centre (CHC) chiropractic clinic population in terms of age and gender representation. [21] Patients over the age of 50 made up 44.1% of the CHC population, and 48.9% of the MCC population. Also similar was that the gender representation of the CHC was 73.0% female. The CHC is a chiropractic clinic that was created in Ottawa, Ontario, Canada as a demonstration project by the Ontario Ministry of Health and Long Term Care, who were also exploring the integration of chiropractors into multidisciplinary primary care settings.
Differences between the populations seen by the CHC chiropractic clinic and the MCC chiropractic clinic include the distribution of regions of complaint. The CHC data reveals their clinic largely treated the low back region (56.0%) with no other spinal region exceeding 11.6% of their population, or extremity region exceeding 6.6%. [21] In contrast, treatment of the lumbar region made up only 19.8% (acute pain) and 26.8% (chronic pain) of MCC chiropractic visits. Treatment of the cervical and thoracic spinal regions (Table 4) was greater at the MCC as was treatment of extremity regions that were 27.6% (acute pain) and 13.0% (chronic pain) visits respectively (Table 4). Baseline, discharge, and change in NRS pain scores were similar between the CHC chiropractic clinic, and the MCC chiropractic clinic. Garner et al., did not report the NRS by region, but the typical NRS at baseline was M=6.2(SD=2.4), and discharge M=3.9(SD=2.7) for a change of –2.3 points. [21] If the MCC chiropractic lumbar region data is used for comparison, NRS at baseline was M=6.8(SD=2.5) and discharge was M=4.8(SD=2.9) for a change of –2.0 points, which is similar to the CHC findings.
At the MCC chiropractic clinic while 74.5% of scheduled visits were kept, 25.5% is a noteworthy no-show rate. Higher no-show rates are predicted in underserved populations. [22] In a primary care setting no-show rates as high as 50% have been reported. [23] Strategies to decrease no-show rates include implementing a phone-call reminder system, and discharging the patient from care following 2 or more no-show visits. Strategies to lessen the burden of no-show visits on clinic performance include using predictions of no-show rates to strategically over-book a clinic or encouraging “walk-in” treatment visits. [23] The observation that nearly three quarters of chiropractic appointments are kept is an indication that patients value the care they are receiving.
There are examples of other health clinics that target inner city or include low-income populations and deliver chiropractic services. At least twenty-four chiropractic programs in academic institutions provide free or low-cost services targeted to those who live in poverty. [5] The programs take place around the globe in countries such as Canada, England, South Africa, The United States, Brazil, Korea, France, and Australia. The MCC differs from those sites in three specific ways. The first difference is financial, the MCC chiropractic clinic is directly supported by provincial healthcare family services funding for its operating costs including clinician salaries, as opposed to being funded by an academic institution. [24] The second difference is that the services provided come directly from an experienced chiropractor. Clinical student interns supervised by academic clinicians deliver care in other “outreach” model clinics. [25] The third difference is that patients do not require a specific vocational or service background (veterans) to qualify as a patient. [20]
At the MCC to be eligible for care you must simply be:1) on social assistance, or classified as “working poor”;
2) have a postal code that reflects you are a resident of the Point Douglas neighbourhood or North End of Winnipeg;
3) be a refugee who has recently moved to Manitoba; or
4) be referred by another community outreach program.Also, all MCC patients must not having standing claims with organizations that would otherwise pay for healthcare services such as the Workers Compensation Board (WCB), or Manitoba Public Insurance (MPI) which covers services related to automobile accidents.
While the QA database was maintained prospectively, the concept of data utilization for research purposes is retrospective. A limitation of the present study is that research questions and interpretation are limited as to the headings included for data capture in the initial design of the database. In addition caution should be taken with the generalization of the results. The study population was the entire intake in the first year of chiropractic patients in an inner city clinic in Manitoba, and may not exactly reflect a rural population, or other urban centers across North America.
Lessons Learned
In order to integrate a new clinical specialty for under-privileged patients, a clinic requires adequate funding. In the case of the MCC that funding comes from provincial taxpayers through Manitoba Health Family Services. The support of Manitoba Health Family Services provided the salary lines to attract highly skilled professionals. By providing funding as an hourly wage, and not fee for service, providers are not motivated to see a patient any more than is clinically warranted to induce a positive therapeutic change. Our results indicate that bringing a chiropractor into a publically funded healthcare team anecdotally decreases the number of primary care visits a patient perceives they need. Reduction in number of primary care visits made by the aforementioned patients, increases the amount of time the primary care provider can spend interacting with patients who are in absolute need of the services of a medical physician.
Upon discharge from clinical care very few patients who benefited from chiropractic intervention required other clinical services. No longer requiring other clinical services further unburdens other care providers in the clinic who may have heavy clinic loads, or even patient waiting lists.
According to our results the implementation of chiropractic services to a publically funded clinic was:1) a service that is utilized for referral by other healthcare providers;
2) reduces pain in patients with acute and chronic spine or extremity pain, and;
3) a service that is valued by patients who would otherwise be unable to afford chiropractic services.Federal, and provincial policy makers, academics or philanthropic agencies may utilize the presented findings to gain insight as to QA measures to record, and what the potential benefit of adding chiropractic services to an inner city multidisciplinary healthcare facility targeted to the poor and underserved may be. Chiropractors typically practice in private outpatient clinics, or multidisciplinary clinics alongside physical therapists, registered massage therapists, or athletic therapists. [6] Popularity of inclusion of chiropractic services in private hospital facilities, [26, 27] veterans hospital facilities, [20, 28–30] and active military base settings31, are endeavours that have occurred in the past decade but continue to grow. [26, 20, 30]
The data presented in this manuscript reflect clinic performance and patient demographics during the inaugural year in which the clinic was created. Follow-up studies exploring the evolution of this type of clinic are warranted to determine the need for expansion or reduction of services, or if a steady-state plateau is attained based on current clinic size and operation. Future studies will be able to compare year-year clinic growth/reduction, patient demographics, outcomes and overall clinical performance from a broader perspective.
Future considerations in working with chiropractic integration of inner city populations include greater utilization of empirically validated outcome measures. Although, questionnaire-based outcome measures should be applied with caution as results may be limited by the literacy and comprehension abilities of the population. [21] Objective performance-based outcome measures may provide better clinical insight in this and other populations. [32] In future studies, the comparison of chiropractic care to other services provided at the MCC with regard to utilization, efficacy and patient satisfaction should be explored.
In conclusion, chiropractic services within a provincially funded, non-secular, non-profit, inner city multi-disciplinary community health centre are being utilized with positive results in pain reduction. Prospectively maintained QA data provides a useful window into clinic operation, and performance during clinic implementation. The outcome of the initial integration in the first year of a publically funded chiropractic clinic targeting the poor and underserved has been successful in terms of exceeding minimally clinically important differences in all painful regions of the body targeted for treatment. The high clinic attendance rate and percentage of referrals for chiropractic services from primary healthcare providers in the MCC facility highlights the value that both patients and other clinicians place on the integration of chiropractic services.
Publically funded inner city chiropractic clinics targeting the poor and underserved allow chiropractic services to be offered and utilized, specifically for more chronic pain conditions, by a component of the population that would otherwise likely be unable to attain healthcare due to a financial barrier. Future research on chiropractic clinic implementation into publically funded multidisciplinary facilities may include the number of primary care visits saved via integration, clinic model sustainability, and the cost/benefit of having chiropractic services added to a government funded healthcare system.
Conflicts of interest
The authors report no conflict of interest. The authors alone are responsible for the content and composition of the manuscript
Acknowledgments
The authors wish to thank Taylor Post for her services as a research assistant, the administration, board and members of the Manitoba Chiropractors Association and the Mount Carmel Clinic for their encouragement to pursue this project.
References:
Cassidy JD, Côté P, Carroll LJ, Kristman V.
Incidence and course of low back pain episodes in the general population.
Spine. 2005;30:2817–2823Balagué F, Mannion AF, Pellisé F, Cedraschi C.
Non-specific low back pain.
Lancet. 2012;379:482–491Cote P, Cassidy JD, Carroll L.
The Saskatchewan Health and Back Pain Survey.
The Prevalence of Neck Pain and Related Disability in Saskatchewan Adults
Spine (Phila Pa 1976). 1998 (Aug 1); 23 (15): 1689–1698Hart LG, Deyo RA, Cherkin DC.
Physician office visits for low back pain. Frequency, clinical evaluation,
and treatment patterns from a U.S. national survey.
Spine. 1995;20:11–19Johnson C.
Poverty and human development: contributions from
and callings to the chiropractic profession.
J Manipulative Physiol Ther. 2007;30:551–556Dagenais S, Haldeman S.
Chiropractic.
Prim Care. 2002;29:419–437Cherkin, D.C. and MacCornack, F.A.
Patient Evaluations of Low Back Pain Care From
Family Physicians and Chiropractors
Western Journal of Medicine 1989 (Mar); 150 (3): 351–355Mosley CD, Cohen IG, Arnold RM.
Cost-effectiveness of Chiropractic Care in a Managed Care Setting
Am J Managed Care. 1996;2:280–282Smith M, Stano M.
Costs and Recurrences of Chiropractic and Medical Episodes of Low-back Care
J Manipulative and Physiological Therapeutics 1997 (Jan); 20 (1): 5–12Walker, BF, Hebert, JJ, Stomski, NJ et al.
Outcomes of Usual Chiropractic.
The OUCH Randomized Controlled Trial of Adverse Events
Spine (Phila Pa 1976). 2013 (Sep 15); 38 (20): 1723–1729Krastins M, Ristinen E, Cimino JA, Mamtani R.
Use of alternative therapies by a low income population.
Acupunct Electro-Therap Res. 1998;23:135–142Dagenais S.
Why not everyone with low back pain chooses chiropractic care.
J Can Chiropr Assoc. 2013;57:6–9Pylypchuk Y, Sarpong EM.
Comparison of health care utilization: United States versus Canada.
Health Services Res. 2013;48:560–581Jin J, Sklar GE, Oh MSV, Chuen LS.
Factors affecting therapeutic compliance:
A review from the patient’s perspective.
Therapeut Clin Risk Management. 2008;4:269–286Lasser KE, Himmelstein DU, Woolhandler S.
Access to care, health status, and health disparities in the United States
and Canada: results of a cross-national population-based survey.
Am J Pub Health. 2006;96:1300–1307Livingstone T, Lix L, McNutt M, Morris E, Rosenbluth D, Scott D, Watson F.
An investigation of the impact of supplementary health benefits
for low-income families in Saskatchewan.
Can J Pub Health. 2004;95:74–78Soklaridis S, Kelner M, Love RL, Cassidy JD.
Integrative health care in a hospital setting:
communication patterns between CAM and biomedical practitioners.
Journal Interprof Care. 2009;23:655–667Squillace J.
Study of a rural practice dental hygienist in a public health setting:
analysis of an administrative dataset.
J Health Care Poor Underserved. 2012;23:739–751Salaffi F, Stancati A, Silvestri CA, Ciaetti A, Grassi W.
Minimal clinically important changes in chronic musculoskeletal
pain intensity measured on a numerical rating scale.
Eur J Pain. 2004;8:283–291Dunn, AS and Passmore, SR.
Consultation Request Patterns, Patient Characteristics, and Utilization of
Services within a Veterans Affairs Medical Center Chiropractic Clinic
Military Medicine 2008 (Jun); 173 (6): 599–603Garner MJ, Aker P, Balon J, Birmingham M, Moher D, Keenan D, Manga P.
Chiropractic Care of Musculoskeletal Disorders in a Unique
Population Within Canadian Community Health Centers
J Manipulative Physiol Ther 2007 (Mar); 30 (3): 165–170Kaplan-Lewis E, Percac-Lima S.
No-show to primary care appointments: why patients do not come.
J Prim Care Comm Health. 2013;4:251–255Daggy J, Lawley M, Willis D, Thayer D, Suelzer C, DeLaurentis PC, Turkcan A.
Using no-show modelling to improve clinic performance.
Health Inform J. 2010;16:246–259Kopansky-Giles D, Vernon H, Steiman I, Tibbles A, Decina P, Goldin J, et al.
Collaborative Community-Based Teaching Clinics at the Canadian Memorial
Chiropractic College: Addressing the Needs of Local Poor Communities
J Manipulative Physiol Ther 2007 (Oct); 30 (8): 558–565Stevens GL.
Behavioral and access barriers to seeking chiropractic care:
a study of 3 New York clinics.
J Manipulative Physiol Ther. 2007;30:566–572 Hospital-Based Chiropractic Integration Within a Large
Private Hospital System in Minnesota: A 10-Year Example
J Manipulative Physiol Ther. 2009 (Nov); 32 (9): 740–748Paskowski I, Schneider M, Stevens J, Ventura JM, Justice BD.
A Hospital-Based Standardized Spine Care Pathway:
Report of a Multidisciplinary, Evidence-Based Process
J Manipulative Physiol Ther 2011 (Feb); 34 (2): 98–106Dunn AS, Passmore SR, Burke J, Chicoine D.
A Cross-sectional Analysis of Clinical Outcomes Following Chiropractic Care
in Veterans With and Without Post-traumatic Stress Disorder
Military Medicine 2009 (Jun); 174 (6): 578–583Lisi AJ, Goertz C, Lawrence DJ, Satyanarayana P.
Characteristics of Veterans Health Administration
Chiropractors and Chiropractic Clinics
J Rehabilitation Research & Development 2009; 46 (8): 997–1002Passmore SR, Lisi AJ.
Integration of chiropractic services into the United States Veterans Health Administration.
In: Aiken AB, Belanger SAH, editors.
Beyond the line: military and veteran health research.
Montreal, QC: McGill-Queen’s University Press; 2013. pp. 231–248Green BN, Johnson CD, Lisi AJ, Tucker J.
Chiropractic Practice in Military and Veterans Health Care:
The State of the Literature
J Can Chiropr Assoc. 2009 (Aug); 53 (3): 194–204Passmore SR, Descarreaux M.
Performance based objective outcome measures and spinal manipulation.
J Electromyog Kinesiol. 2012;22:697–707
Return to INTEGRATED HEALTH CARE
Return to INITIAL PROVIDER/FIRST CONTACT
Since 11-05-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |