Association Between Forward Head, Rounded Shoulders,
and Increased Thoracic Kyphosis:
A Review of the LiteratureThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Chiropractic Medicine 2017 (Sep); 16 (3): 220–229 ~ FULL TEXT
OPEN ACCESS Deepika Singla, MPT Sports, BPT and Zubia Veqar, PhD, MPT Ortho, BPT
Centre for Physiotherapy and Rehabilitation Sciences,
Jamia Millia Islamia,
Jamia Nagar, Okhla, Delhi, India.OBJECTIVE: The purpose of this review was to explore the association between forward head posture, rounded shoulders, and increased thoracic kyphosis.
METHODS: The PubMed, ERIC, and Cochrane databases were searched using the key words posture, head, shoulder, forward scapular posture, and thoracic kyphosis through December 2016.
RESULTS: Our initial search yielded 6,840 research studies, 6,769 of which were excluded because they either were duplicates or did not satisfy the inclusion criteria. After the abstracts of the remaining studies were read, 15 were assessed for eligibility, and only 4 papers were included in the present review. Cervical lordosis values were found to be significantly associated with thoracic kyphosis values. Also, there were significant correlations between rounded shoulders and increased thoracic kyphosis.
CONCLUSION: Forward head posture, rounded shoulders, and increased thoracic kyphosis can exist alone or in any combination.
KEYWORDS: Kyphosis; Posture; Shoulder
From the FULL TEXT Article:
Introduction
Various occupations require people to assume static postures for long periods, which causes continuous contractions of the head and neck muscles. [1, 2] The head constitutes 6% of the total body weight, which is linked to the cervical spine and all other joints through the kinematic chain [3] by various muscles.
Normally, the cervical spine is lordotic. Other than flexion and extension movements of the neck that take place in the sagittal plane, protraction and retraction movements also come into play in this plane. Protraction movement is a result of extension of the upper cervical spine and flexion of the lower cervical spine, whereas retraction movement results from flexion of the upper cervical spine and extension of the lower cervical spine. If the cervical spine is held in protracted position for prolonged duration, it can lead to alterations in head posture ultimately leading to poor posture known as forward head posture (FHP), which is thought to be a deviation from neutral or normal posture. [4, 5]
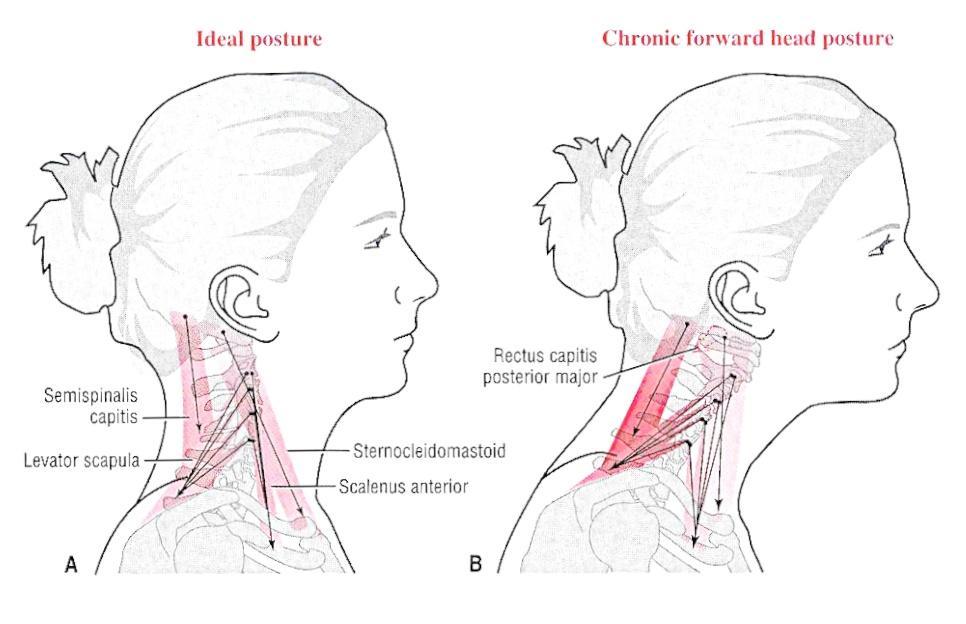
Normal posture is defined as when the line of gravity (LOG) passes through the external auditory meatus, the bodies of the cervical spine, and the acromion and anterior to the thoracic spine [6] (Fig 1). Normally, the external moment produced by gravity and ground reaction forces at a joint is offset by the internal moment produced by various muscles and other soft tissue structures around that joint. However, presence of postural malalignments may require greater internal forces to balance the external torque produced by gravity, which in turn is exaggerated owing to the altered location of the LOG. [7–9]
Failure of the head to align with the vertical axis of the body [3, 10] (Fig 2) can lead to further malalignments in the body, namely, rounded shoulders and increased thoracic kyphosis, [11, 12] to compensate [13] for the altered location of the LOG, leading to further impairments. [14] Combination of all these postural deviations is often known as “slouched posture” [15, 16] or “slumped posture.” [3, 17]
According to Kendall et al, [6] there should be vertical alignment between the midline of the shoulder and the mastoid process. If the acromion processes are more anteriorly positioned compared with the mastoid processes, a condition known as forward shoulder posture (FSP) or rounded shoulders or protracted shoulders [11, 15] occurs (Fig 3); this condition is characterized by protracted, internally rotated, anteriorly tilted, elevated, and abducted scapula along with winging of scapula. [15, 18, 19] This poor alignment of the shoulders leads to greater torque production by gravitational forces, which is being offset by greater internal forces generated by muscles and other soft tissues around the shoulder.
Normally, a flexion moment is being created by the passage of LOG anterior to the thoracic spine that is offset by the extensor muscles, ligamentum flavum, supraspinous ligaments, and posterior longitudinal ligament. This gravitational moment would increase if there is an increase in the thoracic spine’s posterior convexity causing increased distance between joint axes and LOG (Fig 4). In such a case, to maintain an upright posture, ligaments and muscles would be required to produce a greater moment to counterbalance the increased gravitational moment, [7–9, 20] thus leading to an increase in posterior convexity or kyphosis of the thoracic spine, also known as round back. [9]
Figure 4. Increased kyphosis.
Note that t is the distance
between the line of gravity
and thoracic spine.

Posture can be assessed using different methods such as a plumb line, photography, photogrammetry, radiography, Flexicurve, moiré topography, and an electromagnetic tracking device. Any of these methods can be used to detect the presence of abnormal posture. [21–23] Electromyography is also very commonly used in postural assessment studies to ascertain the changes in muscular activities that occur as a result of postural changes. [24]
Most previous studies mention the causes and consequences of FHP, rounded shoulders, and increased thoracic kyphosis. However, there is a dearth of studies focused on the association between forward head, rounded shoulders, and hyperkyphosis. Therefore, the aim of this review was to explore the relationship between FHP, FSP, and increased kyphosis of the thoracic spine.
Methods
Studies were included if they reported association between FHP and FSP, or between FHP and thoracic kyphosis, or between FSP and thoracic kyphosis, and if they were available in free full text online entirely in the English language. Review articles, conference papers, and unpublished dissertations were excluded, as were studies that involved subjects having pain or some pathology other than a postural problem. Studies were also excluded if they described the impact of exercise training or any other modality on posture.
PubMed, ERIC, and Cochrane databases were searched using the key words posture, head, shoulder, forward scapular posture, and thoracic kyphosis in various combinations to find and describe an association between forward head, forward shoulders, and increased kyphosis. The last search was performed in December 2016.
Results

Figure 5

Table 1

Table 2

Table 3 Figure 5 illustrates the numbers of articles retrieved, read, and rejected. Only 4 research studies [12, 25–27] were found to best explain the objective of this study. Other studies used in this review do not explain any relationship among the 3 pathologies, that is, FHP, FSP, and increased kyphosis of the thoracic spine, but instead focus on 1 of the pathologies. Information obtained from such studies has been condensed in Tables 1 and 2. Table 3 summarizes studies that present associations between forward head, rounded shoulders, and increased thoracic kyphosis.
Forward Head Posture
FHP can be linked to computer use, [28] carriage of backpacks, [29] use of smartphones, [16] headache, [30] mouth breathing, bad habit, [31] or shoulder overuse [15, 23, 32] (Table 1).
FHP has been associated with shortened levator scapulae, sternocleidomastoids, upper trapezius, and posterior cervical spine muscles, [18] that is, suboccipital muscles. [30] FHP has been linked to chronic tension-type, cervical, and tension type headaches. [30, 33] Watson and Trott [33] reported a significantly smaller craniovertebral angle value in the headache group than in the non-headache group. Lesser craniovertebral angle meant poorer FHP. The headache group also had lesser isometric strength of the upper cervical flexors as well as a lesser isometric endurance of these muscles when compared with the non-headache group.
Apart from headache, a greater FHP has also been reported to be associated with trigger points in the suboccipital muscles (rectus capitis posterior minor and major and oblique capitis superior). [30] Trigger points associated with taut bands of suboccipital muscles can give rise to referred pain over the occipital and temporal aspects of the head, which is perceived as headache. This headache is thought to be mediated through the spinal cord and trigeminal nucleus caudalis of the brainstem. This means that FHP (shortened suboccipital muscles) leads to the activation of trigger points and, thus, causes tension-type headache. [30]
FHP can cause accumulation of nociceptive substances in the muscles that counteracts FHP, increased compression of cervical facet joints and posterior vertebral bodies, stretching of anterior neck musculature, and shortening of posterior neck musculature. [32, 34] Increased compression of the zygapophyseal joints can result in the inception of degenerative changes leading to spondylosis. The greater and lesser occipital nerves might be compressed because of a reduction in the intervertebral space, leading to stimulation of the trigeminal nerve. This, in turn, can lead to facial pain and headache. [31, 35]
Shoulder pain, neck pain, interscapular pain, craniofacial pain, radiating pain to the scalp, temporomandibular disorders, subacromial impingement syndrome, thoracic outlet syndrome, restricted range of motion at the cervical spine and scapula and shoulder dyskinesis, [4, 11, 12, 31, 32, 35–38] decreased respiratory capcities, [2] poor static balance, [13] and so on (Table 2) can also occur. Assumption of a neutral head posture might be biomechanically beneficial while performing loaded isometric shoulder flexion activities to reduce work-related neck and shoulder pain. [32]
Forward Shoulder Posture
FSP can be linked to, among other factors, repetitive overhead activities, backpack carriage, bad habit, mouth breathing, computer and laptop use, and prolonged study hours [19, 29, 39, 40] (Table 1).
FSP could lead to muscle imbalance in the form of shortening of the anterior shoulder muscles such as the pectoralis minor and major, serratus anterior, and upper trapezius and lengthening of the posterior shoulder muscles, middle and lower trapezius and rhomboids. [7, 19] This muscle imbalance leads to alteration in the scapular and glenohumeral orientation, as well as kinematics, [41, 42] thus increasing the risk of developing neck, shoulder, and nonspecific arm pain. Also, reduction of range of motion and loss of function have been reported. [14, 17, 43] This sequence of events has been well demonstrated in the research report presented by Borstad, who reported that reduced pectoralis minor muscle length would alter the scapular kinematics, which can predispose the person to subacromial impingement syndrome. [14] Patients with subacromial impingement also present with increased scapular abduction, elevation, anterior tilting, and internal rotation, which is very similar to the postural alterations that occur with FSP [15] (Table 2).
A protracted shoulder has been implicated in the restricted sliding of the cords of the brachial plexus, thus increasing strain on the various nerves passing through the shoulder region, especially the median nerve. [17] Also, coracoid pain and malposition, scapular dyskinesis, and prominent inferomedial border of the scapula have been reported (described as “SICK” scapula). The scapula of the dominant side has been found to be more anteriorly tilted and protracted in overhead athletes because of high training volume and repeated overhead activities, reflecting an association between scapular position, scapular dyskinesis and shoulder pathology is there. Decreased range of motion, decreased strength, and diminished performance with respect to velocity and accuracy can be the manifestations of shoulder pathology in sports persons. [44] In a study conducted on 372 players involved in upper arm sports events such as basketball, badminton, gymnastics, swimming, squash, tennis, table tennis, volley ball, and field events, 163 players were having shoulder problems such as shoulder pain, crepitus, weakness, and decreased range of motion. [45]
Thoracic Kyphosis
Increased thoracic kyphosis has been thought to be 1 of the most frequently seen abnormalities in patients with lumbar lordosis, [9] low back pain, [46] and osteoporosis [47] as well as in postmenopausal women [48] (Table 1).
Christie et al [46] measured head position, shoulder position (relative measure of protraction and retraction), shoulder height discrepancy, and thoracic kyphosis of subjects with low back pain and without low back pain. Subjects with low back pain were experiencing either chronic pain or acute pain. Thoracic kyphosis was found to be significantly greater in the acute pain group compared with the control group in both standing and sitting positions. Also, the acute pain group exhibited an increased forward head position compared with the control group in standing position only. It is noteworthy that the values for thoracic kyphosis and shoulder position were always greater in the back pain groups than in the control group, in both standing and sitting positions, irrespective of the existence of significant differences between the groups.
With increased kyphosis at the thoracic spine, anterior longitudinal ligament and upper abdominal muscles are shortened and the anterior aspect of vertebral bodies is compressed, leading to increases in intradiscal pressures. Also, the extensor muscles and posterior ligaments of the dorsal spine are stretched along with the capsules of the facet joints and the posterior fibers of the annulus fibrosus. [7] The condition might lead to pain, [49] expansion of rib cage, poor balance, and, thus, the risk of falls in geriatric participants. [20] With increasing age, gradually the connective tissues lose their elasticity and become inefficient in counteracting the torque produced by gravity. [48] However, kyphosis associated with increasing age is mild and does not cause much of a problem. [4] However, an excessive degree of kyphosis (hyperkyphotic posture) might be a risk factor for fractures (Table 2). Hyperkyphosis might lead to complications such as poor respiratory function, compromised physical function, and increased mortality. [50] Thus, it is plausible to say that this type of posture deserves clinical attention.
Discussion
Alteration in the resting scapular position is thought to occur with abnormal alignment of the cervical and thoracic spine. [51] forward shoulder posture (FSP) can be associated with forward head posture (FHP), [52] increased thoracic kyphotic posture, [19, 25, 26] or both [12, 15] (Table 3). The scapula has been found to be anteriorly tilted, downwardly rotated, and protracted during elevation of the arm in persons with FHP. A decrease in serratus anterior activity has been observed in persons with FHP while doing arm elevation and lifting activities. This reduction in serratus anterior activity leads to anterior tilting of the scapula, as well as winging of the scapula (because the serratus anterior stabilizes the scapula on the thorax). [32]
Increased forward angulation of the scapula can be observed with an increase in slope of the upper thoracic spine. The angle formed between the clavicle and the scapula in the transverse plane increases too much owing to the rib cage expansion and increased anteroposterior diameter of the chest caused by increased thoracic kyphosis. Thoracic spine posture also influences scapular and glenohumeral kinematics. Increased flexion at the thoracic spine could lead to reduced elevation range of motion at the glenohumeral joint. Also, reduced scapular posterior tilting and increased scapular elevation might be evident while doing elevation at the shoulder. [15, 25, 51, 53]
The thoracic spine is less mobile and, thus, more stable in comparison to the cervical region. This stability is attributed to the presence of ribs, lesser intervertebral disk height, and the plane of facet joints. [7, 49] The literature contains scientific evidence that increased cervical lordosis can lead to more pronounced thoracic kyphosis. In a recent study, [27] the amount of cervical lordosis was found to correlate with the degree of thoracic kyphosis. Two hundred twenty-eight subjects were divided into two groups based on the radiological findings. Group 1 subjects were characterized by loss of cervical lordosis, and group 2 subjects had physiologic lordotic cervical curvature. Whole (T1–12), lower (T6–12), and upper (T1–6) thoracic kyphosis was determined using the Cobb method. The mean values for group 1 were found to be lower for upper, lower, and whole thoracic kyphosis than the mean values for group 2. Another study found a significant correlation between FHP and thoracic kyphosis. [43]
The aforementioned studies hence provide evidence of an association between FHP and rounded shoulders, [5, 52] between FHP and thoracic kyphosis, [27, 46] and between rounded shoulders and thoracic kyphosis. [19, 25, 26] To the best of our knowledge, only 4 papers were found that best supported the objective of this review. As can be observed in Tables 1 and 2, there is heterogeneity in the methods employed by these studies to observe posture; thus, we could not reach a definitive conclusion regarding the cause of FHP, FSP, or thoracic kyphosis, that is, what happens first among the 3 and what happens next. More research studies are required to answer the question and report that it is a cascade of biomechanical changes starting with 1 of the 3 deviations leading to the other 2 deviations.
Although there is consensus on the coexistence of FHP, FSP, and increased thoracic kyphosis, there remains doubt about 1 being the cause or the consequence of the other. Research is required to test the cause-and-effect relationship between the 3 postural deviations. Researchers are encouraged to explore the link between forward head, forward shoulder, and thoracic kyphotic posture so that these conditions can be treated effectively.
Limitations
This study was limited by the search terms and indexes searched. Therefore, it is possible that other studies may exist that were not included. Because so few studies were found, the conclusions based on the findings are limited as well.
Conclusion
On the basis of the literature, there appears to be a relationship between FHP, FSP, and thoracic kyphosis. Current evidence limits our understanding of the association between these 3 conditions. It is unclear whether any of these 3 postural deviations is a cause or a consequence of the other 2 deviations. However, it is clear that 2 or all 3 deviations can co-exist.
Practical Applications
FHP has been found to be associated with FSP or protracted shoulders
and increased kyphosis at the thoracic spine.Combination of all these postural deviations is often referred to as
a “slouched posture.”Causes of FHP include computer use, carriage of backpacks, mouth
breathing, bad habit, rounded upper back, and rounded shoulders.FHP can lead to headache, shoulder pain, neck pain, craniofacial pain,
radiating pain to the scalp, temporomandibular disorders,
subacromial impingement syndrome, restricted range of motion at
the cervical spine, and scapula and shoulder dyskinesis.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): D.S.
Design (planned the methods to generate the results): D.S., Z.V.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): Z.V.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): D.S.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): D.S., Z.V.
Literature search (performed the literature search): D.S.
Writing (responsible for writing a substantive part of the manuscript): D.S.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): Z.V.
References:
Vakili L, Halabchi F, Mansournia MA, Khami MR, Irandoost S, Alizadeh Z.
Prevalence of common postural disorders among academic dental staff.
Asian J Sports Med. 2016;7(2):e29631Han J, Park S, Kim Y, Choi Y, Lyu H.
Effects of forward head posture on forced vital capacity and respiratory muscles activity.
J Phys Ther Sci. 2016;28(1):128–131Szczygie? E, W?glarz K, Piotrowski K, Mazur T, M?tel S, Golec J.
Biomechanical influences on head posture and the respiratory movements of the chest.
Acta Bioeng Biomech. 2015;17(2):143–148Neumann DA.
Mosby; Philadelphia, PA: 2002.
Kinesiology of the Musculoskeletal System: Foundations for Physical Rehabilitation.Thigpen CA, Padua DA, Michener LA.
Head and shoulder posture affect scapular mechanics and muscle activity in overhead tasks.
J Electromyogr Kinesiol. 2010;20(4):701–709Kendall FP, McCreary EK, Provance PG, Rodgers M, Romani W.
5th ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2005.
Muscles: Testing and Function, With Posture and Pain.Levangie PK, Norkin CC.
3rd ed. Jaypee Brothers; New Delhi, India: 2001.
Joint Structure and Function: A Comprehensive Analysis.Oatis CA.
2nd ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2008.
Kinesiology: The Mechanics and Pathomechanics of Human Movement.Saxton JB.
Normal and abnormal postures in the sagittal plane and their relationship to low back pain.
Physiother Pract. 1988;4(2):94–104.Harman K, Hubley-Kozey CL, Butler H.
Effectiveness of an exercise program to improve forward head posture in normal adults: A randomized, controlled 10-week trial.
J Man Manip Ther. 2005;13(3):163–176.Raine S, Twomey LT.
Head and shoulder posture variations in 160 asymptomatic women and men.
Arch Phys Med Rehabil. 1997;78(11):1215–1223Raine S, Twomey LT.
Posture of the head, shoulders and thoracic spine in comfortable erect standing.
Aust J Physiother. 1994;40(1):25–32Lee JH.
Effects of forward head posture on static and dynamic balance control.
J Phys Ther Sci. 2016;28(1):274–277Borstad JD.
Resting position variables at the shoulder: Evidence to support a posture-impairment association.
Phys Ther. 2006;86(4):549–557Michener LA, McClure PW, Karduna AR.
Anatomical and biomechanical mechanisms of subacromial impingement syndrome.
Clin Biomech (Bristol, Avon) 2003;18(5):369–379Jung SI, Lee NK, Kang KW, Kim K, Lee DY.
The effect of smartphone usage time on posture and respiratory function.
J Phys Ther Sci. 2016;28(1):186–189Julius A, Lees R, Dilley A, Lynn B.
Shoulder posture and median nerve sliding.
BMC Musculoskelet Disord. 2004;5(23):1–7Ruivo RM, Pezarat-Correia P, Carita AI.
Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain.
Braz J Phys Ther. 2014;18(4):364–371Ghanbari A, Ghaffarinejad F, Mohammadi F, Khorrami M, Sobhani S.
Effect of forward shoulder posture on pulmonary capacities of women.
Br J Sports Med. 2008;42(7):622–623Briggs AM, van Dieën JH, Wrigley TV.
Thoracic kyphosis affects spinal loads and trunk muscle force.
Phys Ther. 2007;87(5):595–607Singla D, Veqar Z.
Methods of postural assessment used for sports persons.
J Clin Diagn Res. 2014;8(4):LE01–LE04Guedes PF, João SM.
Postural characterization of adolescent federation basketball players.
J Phys Act Health. 2014;11(7):1401–1407Greenfield B, Catlin PA, Coats PW, Green E, McDonald JJ, North C.
Posture in patients with shoulder overuse injuries and healthy individuals.
J Orthop Sports Phys Ther. 1995;21(5):287–295Lee ST, Moon J, Lee SH.
Changes in activation of serratus anterior, trapezius and latissimus dorsi with slouched posture.
Ann Rehabil Med. 2016;40(2):318–325Kebaetse M, McClure P, Pratt NA.
Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics.
Arch Phys Med Rehabil. 1999;80(8):945–950Lee JH, Cynn HS, Yi CH, Kwon OY, Yoon TL.
Predictor variables for forward scapular posture including posterior shoulder tightness.
J Bodyw Mov Ther. 2015;19(2):253–260Ludewig PM, Reynolds JF.
The association of scapular kinematics and glenohumeral joint pathologies.
J Orthop Sports Phys Ther. 2009;39(2):1–26Straker LM, O'Sullivan PB, Smith A, Perry M.
Computer use and habitual spinal posture in Australian adolescents.
Public Health Rep. 2007;122(5):634–643Chansirinukor W, Wilson D, Grimmer K, Dansie B.
Effects of backpacks on students: Measurement of cervical and shoulder posture.
Aust J Physiother. 2001;47(2):110–116Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML.
Trigger Points in the Suboccipital Muscles and Forward Head Posture in Tension-Type Headache
Headache: J of Head and Face Pain 2006 (Mar); 46 (3): 454—460Gadotti IC.
University of Alberta; Edmonton, AB, Canada: 2010.
Measurement Properties of the Sagittal Craniocervical Posture Photogrammetry [PhD thesis]
Available at:
https://era.library.ualberta.ca/public/datastream/get/uuid:79b6a715-a0cd-4f71
-9a5b-a9b642629f01/DS1
Accessed March 14, 2012.Weon JH, Oh JS, Cynn HS, Kim YW, Kwon OY, Yi CH.
Influence of forward head posture on scapular upward rotators during isometric shoulder flexion.
J Bodyw Mov Ther. 2010;14(4):367–374Watson DH, Trott PH.
Cervical headache: An investigation of natural head posture and upper cervical flexor muscle performance.
Cephalalgia. 1993;13(4):272–284Silva AG, Punt TD, Sharples P, Vilas-Boas JP, Johnson MI.
Head posture assessment for patients with neck pain: Is it useful?
Int J Ther Rehabil. 2009;16(1):43–53.Wang W.
Queen’s University; Kingston, ON, Canada: 1997.
Measurement of Neutral Cervical and Cervicothoracic Posture in Healthy Adults [master’s thesis]
Available at:
http://www.collectionscanada.gc.ca/obj/s4/f2/dsk3/ftp04/mq22420.pdf
Accessed April 21, 2012.Aitken A.
Unitec; New Zealand: 2008.
Reliability of Visual Assessment of Forward Head Posture in Standing [master’s research project]
Available at:
http://unitec.researchbank.ac.nz/bitstream/handle/10652/1613/Andrew_Aitken
%20MOst.pdf?sequence=1
Accessed April 23, 2012.Lau HM, Chiu TT, Lam TH.
Measurement of craniovertebral angle with electronic head posture instrument: Criterion validity.
J Rehabil Res Dev. 2010;47(9):911–918Patwardhan AG, Havey RM, Khayatzadeh S.
Postural consequences of cervical sagittal imbalance.
Spine. 2015;40(11):783–792Hibberd EE, Laudner K, Berkoff DJ, Kucera KL, Yu B, Myers JB.
Comparison of upper extremity physical characteristics between adolescent competitive swimmers and nonoverhead athletes.
J Athl Train. 2016;51(1):65–69Neiva PD, Kirkwood RN, Godinho R.
Orientation and position of head posture, scapula and thoracic spine in mouth-breathing children.
Int J Pediatr Otorhinolaryngol. 2009;73(2):227–236Phadke V, Camargo P, Ludewig P.
Scapular and rotator cuff muscle activity during arm elevation: A review of normal function and alterations with shoulder impingement.
Rev Bras Fis. 2009;13(1):1–9Borstad JD, Ludewig PM.
The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals.
J Orthop Sports Phys Ther. 2005;35(4):227–238Lewis JS, Wright C, Green A.
Subacromial impingement syndrome: The effect of changing posture on shoulder range of movement.
J Orthop Sports Phys Ther. 2005;35(2):72–87Wilk KE, Obma P, Simpson CD, Cain EL, Dugas JR, Andrews JR.
Shoulder injuries in the overhead athlete.
J Orthop Sports Phys Ther. 2009;39(2):38–54Lo YPC, Hsu YCS, Chan KM.
Epidemiology of shoulder impingement in upper arm sports events.
Br J Sports Med. 1990;24(3):173–177Christie HJ, Kumar S, Warren SA.
Postural aberrations in low back pain.
Arch Phys Med Rehabil. 1995;76(3):218–224Rodrigues ACC, Romeiro CAP, Patrizzi LJ.
Evaluation of thoracic kyphosis in older adult women with osteoporosis by means of computerized biophotogrammetry.
Rev Bras Fis. 2009;13(3):205–209.Hinman MR.
Comparison of thoracic kyphosis and postural stiffness in younger and older women.
Spine J. 2004;4(4):413–417Edmondston SJ, Singer KP.
Thoracic spine: Anatomical and biomechanical considerations for manual therapy.
Man Ther. 1997;2(3):132–143Huang MH, Barrett-Connor E, Greendale GA, Kado DM.
Hyperkyphotic posture and risk of future osteoporotic fractures: The Rancho Bernardo study.
J Bone Miner Res. 2006;21(3):419–423Culham E, Peat M.
Functional anatomy of the shoulder complex.
J Orthop Sports Phys Ther. 1993;18(1):342–350Kwon JW, Son SM, Lee NK.
Changes in upper-extremity muscle activities due to head position in subjects with a forward head posture and rounded shoulders.
J Phys Ther Sci. 2015;27(6):1739–1742Erkan S, Yercan HS, Okcu G, Ozalp RT.
The influence of sagittal cervical profile, gender and age on the thoracic kyphosis.
Acta Orthop Belg. 2010;76(5):675–680
Return to FORWARD HEAD POSTURE
Since 3-15-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |