Epidural Steroid Injections:
Are long-term Risks Worth Short Term Benefits?This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: ACA News ~ February 2014 ~ FULL TEXT
By William Morgan, DCOutpatient procedures are where the money is in medicine these days. Such procedures are invasive treatments that are not quite surgery but are not conservative care either. Non-surgical procedura lists are falling over themselves at an alarming rate to learn these lucrative businesses. This is true in several medical specialties: cardiac catheterization labs, GI endoscopies and colonoscopies, interventional radiology procedures, PMR pain procedures, urologic cystoscopies, chiropractic manipulation under anesthesia, epidural steroid injection therapies and many other pain procedures. If utilized correctly, these procedures may be valuable tools in the treatment of patients by preventing more invasive procedures, and in the case of cystoscopies and colonoscopies, aid in the early detection of cancer.
These procedures can be done quickly with assembly line efficiency and are very profitable for the physicians. In the case of epidural steroid injections (ESI), a ten-minute epidural procedure will generally yield anywhere from a couple hundred to a couple thousand dollars, though I have heard of a series of three epidurals going for as much as $8,000. Furthermore, if done in an outpatient facility, the physician does not have to split the fees with a hospital, and the insurance company does not need to pay the higher costs that normally accompany hospital-based procedures. Last year in the United States, the Centers for Medicare and Medicaid Services (CMS) paid for nearly nine million ESI. This number may not appear surprising at first, but when you consider that ESI therapies are neither approved by the FDA [1] nor recommended by the manufacturers [2] due to reports of severe adverse events, it becomes alarmingly relevant. Note that the CMS number is not the total number of ESI performed in the United States. The nine million number represents only those ESI paid for by CMS. When we add in the number of ESI performed in the DOD, VA, workers’ compensation systems and private insurance, that number could conceivably be in the tens of millions.
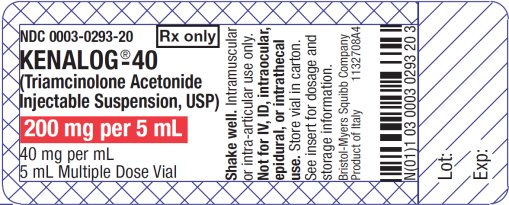
While it is true that epidural steroid injections (ESI) are not FDA approved, Medicare, Medicaid, workers’ compensation and most other insurers continue to pay hundreds of millions of dollars per year for this controversial procedure. Ironically, on every vial of Kenalog (a popular steroid used for epidural injections) there is actually a warning against its use for epidural injections, yet proceduralists continue to use it.
Although there is inadequate evidence to support the high use of ESI in the United States, it remains a very popular growth industry. This is partially due to ESI being purported to reduce the number of spine surgeries. However, studies like one performed by Arden, et al. [3] show that ESI did not offer sustained benefits nor did it reduce the need for spinal surgery. Arden’s study did show that there was a transient reduction of symptoms in patients with sciatica. Carette, et al. performed a separate study with similar results. [4]
In the ten-year period between 2000 and 2010, the use of ESI increased 160 percent. Dr. Manchikanti, chairman of the American Society of Interventional Pain Physicians, stated:“We are doing too many of these spinal injections, and
many of those don’t meet the proper criteria.” [5]He attributed this remarkable increase in spinal injections to the increased number of patients seeking pain relief and the financial incentives afforded to the treating physicians.
The overutilization of this profitable model of care is out of control and in my opinion is the next healthcare bubble growing at such an alarming pace that it can only burst. When it does burst, these physicians will scramble to the next profitdriven model of care. My hope is that the next profit model will be based on value of care versus quantity of care.
Risks of ESI
While major damage associated with ESI is rare according to the literature, we are seeing a surge in the total number of patients with complications like chemical meningitis and adhesive arachnoiditis (which I feel is underreported). Even if these complications are rare, when nine million ESI are performed annually, we are going to see more adverse effects. In my 28 years in practice, I have seen two patients who became quadriplegics after receiving cervical ESI, one MS patient confined to a wheelchair after receiving an epidural, another with vertebral body osteomyelitis when he received an epidural the day after dental surgery, and another with adhesive arachnoiditis following an ESI. Five severe complications from ESI in a lifetime of practice is not very high, but did the perceived benefit of this procedure justify the risk?
Note that I did not even mention the fungal meningitis outbreak that killed and maimed hundreds of patients who received tainted ESI in 2012. [6, 7] That tragic epidemic warrants its own article.
As with any treatment, the perceived benefit should be balanced by the risk, with the right doctor doing the right procedure on the right patient. The perceived benefit for ESI does not substantiate its current level of utilization. A common misconception in referring patients for ESI is that this procedure may reduce the need for surgery. In fact, the science clearly indicates that ESI therapies do not reduce the need for surgery and are only effective in providing temporary short-term pain relief. Are the serious risks worth the short-term benefits?
Hope
As healthcare reimbursement shifts from fee-for-service to reimbursement based on the value of care, we can hope to see the glut of medical procedures come under greater scrutiny and be subject to review and control.
References
Epstein NE.
The risks of epidural and transforaminal steroid injections in the spine: Commentary and a comprehensive review of the literature.
2013; 4(Suppl 2): S74–S93
Methylprednisolone Acetate/DepoMedrol Reformulation/Epidural Use.
Pharmacia Upjohn/Pfizer, New York, NY
Arden NK, Price C, Reading I, Stubbing J, Hazelgrove J, Dunne C, et al.
A multicentre randomized controlled trial of epidural corticosteroid injections for sciatica: The WEST study
Rheumatology (Oxford). 2005 (Nov); 44:1399-406
Carette S, Leclaire R, Marcoux S, Morin F, Blaise GA, St-Pierre A, et al.
Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus
N Engl J Med 1997 (Jun 5); 336 (23): 1634-40
Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B.
Complications of fluoroscopically directed facet joint nerve blocks: a prospective evaluation of 7,500 episodes with 43,000 nerve blocks
Pain Physician 2012 (Mar); 15 (2): E143-50
American Medical Association Morning Rounds, in Affiliation with Bulletin HEALTHCARE, CDC:
25 dead in meningitis outbreak, cases reach 337 in 18 states. Monday, October 29, 2012
More Bad News For Low Back Pain Sufferers: Drug-induced Meningitis
A Chiro.Org Editorial
Dr. Morgan splits his clinical time between a hospital chiropractic clinic and executive health clinics in Washington, D.C. He is adjunct faculty for Uniformed Services University of the Health Sciences and a professor at New York College of Chiropractic. His online courses can be viewed at http://healthpatheducation.com/morgan. He can be reached through his website, www.drmorgan.info

Return to MEDICARE
Return to IATROGENIC INJURY
Since 1-05-2014


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |