

Global, Regional, and National Incidence, Prevalence, and Years
Lived With Disability for 328 Diseases and Injuries for 195 Countries,
1990-2016: A Systematic Analysis for the Global Burden of Disease Study 2016This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Lancet. 2017 (Sep 16); 390 (10100): 1211–1259 ~ FULL TEXT
OPEN ACCESS GBD 2016 Disease and Injury Incidence and Prevalence Collaborators: Amanuel Alemu Abajobir, Kalkidan Hassen Abate, Cristiana Abbafati, Kaja M Abbas, Foad Abd-Allah, Rizwan Suliankatchi Abdulkader, Abdishakur M Abdulle, Teshome Abuka Abebo, Semaw Ferede Abera, Victor Aboyans, et. al.
BACKGROUND: As mortality rates decline, life expectancy increases, and populations age, non-fatal outcomes of diseases and injuries are becoming a larger component of the global burden of disease. The Global Burden of Diseases, Injuries, and Risk Factors Study 2016 (GBD 2016) provides a comprehensive assessment of prevalence, incidence, and years lived with disability (YLDs) for 328 causes in 195 countries and territories from 1990 to 2016.
METHODS: We estimated prevalence and incidence for 328 diseases and injuries and 2982 sequelae, their non-fatal consequences. We used DisMod-MR 2.1, a Bayesian meta-regression tool, as the main method of estimation, ensuring consistency between incidence, prevalence, remission, and cause of death rates for each condition. For some causes, we used alternative modelling strategies if incidence or prevalence needed to be derived from other data. YLDs were estimated as the product of prevalence and a disability weight for all mutually exclusive sequelae, corrected for comorbidity and aggregated to cause level. We updated the Socio-demographic Index (SDI), a summary indicator of income per capita, years of schooling, and total fertility rate. GBD 2016 complies with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER).
FINDINGS: Globally, low back pain, migraine, age-related and other hearing loss, iron-deficiency anaemia, and major depressive disorder were the five leading causes of YLDs in 2016, contributing 57·6 million (95% uncertainty interval [UI] 40·8-75·9 million [7·2%, 6·0-8·3]), 45·1 million (29·0-62·8 million [5·6%, 4·0-7·2]), 36·3 million (25·3-50·9 million [4·5%, 3·8-5·3]), 34·7 million (23·0-49·6 million [4·3%, 3·5-5·2]), and 34·1 million (23·5-46·0 million [4·2%, 3·2-5·3]) of total YLDs, respectively. Age-standardised rates of YLDs for all causes combined decreased between 1990 and 2016 by 2·7% (95% UI 2·3-3·1). Despite mostly stagnant age-standardised rates, the absolute number of YLDs from non-communicable diseases has been growing rapidly across all SDI quintiles, partly because of population growth, but also the ageing of populations. The largest absolute increases in total numbers of YLDs globally were between the ages of 40 and 69 years. Age-standardised YLD rates for all conditions combined were 10·4% (95% UI 9·0-11·8) higher in women than in men. Iron-deficiency anaemia, migraine, Alzheimer's disease and other dementias, major depressive disorder, anxiety, and all musculoskeletal disorders apart from gout were the main conditions contributing to higher YLD rates in women. Men had higher age-standardised rates of substance use disorders, diabetes, cardiovascular diseases, cancers, and all injuries apart from sexual violence. Globally, we noted much less geographical variation in disability than has been documented for premature mortality. In 2016, there was a less than two times difference in age-standardised YLD rates for all causes between the location with the lowest rate (China, 9201 YLDs per 100,000, 95% UI 6862-11943) and highest rate (Yemen, 14,774 YLDs per 100,000, 11,018-19,228).
INTERPRETATION: The decrease in death rates since 1990 for most causes has not been matched by a similar decline in age-standardised YLD rates. For many large causes, YLD rates have either been stagnant or have increased for some causes, such as diabetes. As populations are ageing, and the prevalence of disabling disease generally increases steeply with age, health systems will face increasing demand for services that are generally costlier than the interventions that have led to declines in mortality in childhood or for the major causes of mortality in adults. Up-to-date information about the trends of disease and how this varies between countries is essential to plan for an adequate health-system response.
There is more like this at our
Global Burden of Disease PageFUNDING: Bill & Melinda Gates Foundation, and the National Institute on Aging and the National Institute of Mental Health of the National Institutes of Health.
Research in Context
Evidence before this study
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) produces the only assessment of prevalence, incidence, and years lived with disability (YLDs) for a comprehensive list of diseases and injuries, and for all countries from 1990 to the present. The World Health Organization has published YLD estimates for the years 2000–15 largely based on GBD 2015 results apart from ad hoc changes applied to selected disability weights and the prevalence of a small subset of causes. GBD 2016 is a reassessment of the burden of disease due to non-fatal diseases and injuries and updates the GBD 2015 study results.
Added value of this study
This study adds new knowledge about YLD rates globally and improves upon prior iterations of the GBD study in seven ways. First, new data were incorporated based on 56,356 unique data sources; these were composed mainly of peer-reviewed scientific literature identified by systematic reviews, reports from statistical agencies or ministries of health, household surveys, administrative data systems, claims data, and hospital data. In 2016, we had 14,521 sources from the scientific literature compared with 10,478 such sources used in GBD 2015. Our network of collaborators provided 2,598 data sources for GBD 2016 compared with 968 available for GBD 2015; furthermore, 3,430 sources of survey data were used in GBD 2016. These counts reflect our updated counting criteria for GBD 2016. Large amounts of new data for the main causes of YLDs were identified through our collaboration with the Indian Council of Medical Research and the Public Health Foundation of India. For particular diseases, the volume of available data increased substantially. Examples include Rapid Assessment of Avoidable Blindness surveys and the detailed studies reported in the Global Atlas of Helminth Infection for schistosomiasis and lymphatic filariasis.
Second, we substantially changed the modelling approach for some diseases, such as cancers and tuberculosis. For cancer we improved our analysis of mortality-to-incidence ratios, resulting in considerably higher ratios in lower Socio-demographic Index (SDI) locations and thus lower YLD estimates. We also applied mortality-to-incidence ratios in the analysis of tuberculosis to better predict the gap between true incidence and notified cases—ie, undetected cases. Third, estimation at the subnational level was newly developed for Indonesia, and estimates for England were disaggregated into those for 150 local government areas. Fourth, we have disaggregated several causes to separately estimate drug-sensitive, multidrug-resistant, and extensively drug-resistant tuberculosis; latent tuberculosis infection; alcoholic cardiomyopathy; urogenital, musculoskeletal, and digestive congenital anomalies; and self-harm by firearm, to provide more detail within the GBD cause hierarchy.
Additionally, Guinea worm disease was estimated due to the fact that there is policy interest in eradication, which is feasible in the near future. Sexual violence was added as a non-fatal cause of YLDs because of its relevance to several of the new sustainable development goal (SDG) targets. Fifth, we were able to incorporate inpatient hospital data by cause for 222 more locations and a final total of 3,557 location-years. A separate analysis of total hospital admissions per capita by country, year, age, and sex allowed the use of hospital data sources that previously had been rejected because of incomplete knowledge about catchment populations. We extended our analyses of US medical claims data to impute a ratio of any health service contact for a diagnosis to inpatient episodes for chronic diseases that we applied to hospital inpatient data from elsewhere to predict prevalence. Sixth, we have extended our analyses of GBD results by SDI with new ways of presenting and visualising changes over time and the relationship with development. Seventh, we extended the terminal age group used in our analyses of older than 80 years into 80–84, 85–89, 90–94, and older than 95 years.
Implications of all the available evidence
As countries confront the effects of the epidemiological transition, there will be an increased need for up-to-date assessment of non-fatal health outcomes and exploration of the implications of growing numbers of individuals in need of chronic care as populations age. The GBD study provides opportunities to identify important non-fatal health trends across various locations and levels of development, and to assess the strength of available estimates.
From the FULL TEXT Article:
Introduction
Assessment of death rates by cause has been an essential component of tracking progress in global health. The Millennium Development Goals (MDGs) emphasised child, maternal, and infectious disease mortality and spurred investments that contributed to a rapid decline in mortality from these sources, although these have not been universally achieved at the same level. [1, 2] Progress in reducing the disabling outcomes of disease has been much slower. [3] The Global Burden of Diseases, Injuries, and Risk Factors Study 2015 (GBD 2015) estimated a modest 2.1% reduction in the age-standardised rate of years lived with disability (YLDs) for all causes compared with a 22.7% reduction in age-standardised rates of years of life lost (YLLs) for all causes between 2005 and 2015. [3] The slower progress in addressing non-fatal compared with fatal health outcomes and ageing of populations make YLDs an increasingly important component of global disability-adjusted life-years (DALYs). In some high-income countries with advanced ageing, YLDs already make up more than half of the total burden in DALYs. [4] The GBD Study is the only global effort to quantify non-fatal outcomes using a metric that allows comparisons between fatal and non-fatal outcomes of a comprehensive list of diseases and injuries.
There are several challenges in standardising the estimation of YLDs. For example, case definitions vary; there are diverse data sources and study methods; accessible data sources are sparse for many diseases, with large parts of the world lacking adequate data; and data for severity of outcomes are limited and lack a standardised approach. This annual update of the GBD study provides an opportunity to incorporate new data and improved methods within a standardised framework to enhance the precision and accuracy of estimation.
The extensive GBD network of more than 2518 collaborators from 133 countries and three non-sovereign locations have provided invaluable critiques of methods and helped to identify new data sources. Most of the debates arising from GBD 2015 have come as direct communications from the collaborative network or have been published by collaborators and other researchers. For example, collaborators have addressed omissions in the GBD cause list, [5–10] challenged the GBD hierarchy of causes, [11] or explored the continual debate regarding disability weights. [12] There is also a growing scientific literature on secondary analyses of GBD results — eg, with a focus on chronic kidney disease, [13] oral diseases, [14] or cardiovascular disease among the poorest billion. [15]
The primary objective of the non-fatal component of GBD 2016 was to estimate prevalence, incidence, and YLDs for 328 GBD causes from 1990 to 2016. For each cycle of GBD, the entire time series is re-estimated to incorporate new data and methods; thus, these results supersede previous GBD results. We explore the patterns of non-fatal disease over time and in comparison to expected levels based on an index of sociodemographic development.
Methods
Overview
The GBD study provides a standardised analytical approach for estimating incidence, prevalence, and YLDs by age, sex, cause, year, and location. We aim to use all accessible information on disease occurrence, natural history, and severity that passes minimum inclusion criteria set disease-by-disease (appendix 1 , p 33). Our approach is to optimise the comparability of data collected by varying methods or different case definitions; find a consistent set of estimates between data for prevalence, incidence, and causes of death; and predict estimates for locations with sparse or absent data by borrowing information from other locations and using covariates.
In this study, we use different methods to reflect the available data and specific epidemiology of each disease. Our main approach is to combine all sources of information for a disease using the Bayesian meta-regression tool DisMod-MR 2.1.16 Subsequently, we use data for severity, the occurrence of particular consequences of diseases, or sequelae, to establish the proportion of prevalent cases experiencing each sequela. Several broad classes of alternative approaches are used within the GBD study. First, for injuries, non-fatal estimates must account for the cause of injury (eg, a fall), the nature of injury (eg, a fracture or head injury), the amount of disability arising in the short term, and permanent disability for a subset of cases. Second, cancers were estimated by assessing the association between mortality and incidence, taking into account the effect on survival of access to, and quality of, treatment for the cancer site. Third, we combined the natural history model strategy for HIV/AIDS with the DisMod-MR 2.1 modelling approach for tuberculosis as HIV infection affects outcomes in patients who also have tuberculosis. Fourth, models for malaria, hepatitis, and varicella relied on data of the presence of circulating antibodies or parasites in the blood to predict the incidence of clinical episodes for which we estimate disability. Fifth, neonatal disorders were estimated from birth prevalence data and cohort studies on the risk of death in the first month and the probability of long-term disabling outcomes. Sixth, incidence of rabies, whooping cough, diphtheria, and tetanus was estimated from cause-specific mortality rates and data on the case fatality of acute episodes (appendix 1, p 33).
Below we describe these modelling efforts organised into eight sections; the supplementary methods (appendix 1, p 1) presents a single source for additional detail of inputs, analytical processes, outputs, and methods specific to each cause. This study complies with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) recommendations (appendix 1, p 723). [17]
1. Geographic units and time periods
The GBD 2016 study was based on a geographic hierarchy that includes 195 countries and territories grouped within 21 regions and seven GBD super-regions (appendix 1, p 726). For this publication, we present subnational estimates in figures and only for Brazil, China, India, and the USA. Details of subnational estimates will be reported in separate publications.
Cause-specific estimation in GBD 2016 was done for the years 1990, 1995, 2000, 2006, 2010, and 2016 and interpolated to get a full time series. In view of policy priorities, a subset of results focus on change over the time period 2006–16. Results from GBD 2016 by year and location can be explored further in dynamic data visualisations.
2. GBD cause list
In the GBD Study, causes and their sequelae are collectively exhaustive and mutually exclusive and are organised in a hierarchy with five levels. Level 1 contains three broad cause groups: communicable, maternal, neonatal, and nutritional diseases; non-communicable diseases; and injuries. These are broken down into 21 Level 2 causes with further disaggregation into 163 Level 3 causes and 271 Level 4 causes. Sequelae of these causes are represented at Level 5 of the hierarchy.
For GBD 2016, we expanded the list of causes of non-fatal outcomes from 310 to 328. This involved the refinement of certain Level 3 causes into new Level 4 causes, including disaggregation of tuberculosis and HIV- tuberculosis into drug-susceptible tuberculosis, multidrug-resistant tuberculosis, extensively drug-resistant tuberculosis, and latent tuberculosis infection. Cardiomyopathy and myocarditis were further refined as alcoholic cardiomyopathy, myocarditis, and other cardiomyopathy. Other leukaemia was added as an additional sub-cause at Level 4. Self-harm was separated into self-harm by firearm and self-harm by other means. The previously named cause grouping “collective violence and legal intervention” was divided into two Level 4 causes: executions and police conflict. New causes of non-fatal outcomes added to the GBD hierarchy for 2016 included Zika virus disease; musculoskeletal, urogenital, and digestive congenital anomalies; Guinea worm disease; and sexual violence. Medication overuse headache was removed as a cause and, instead, characterised as a sequela of migraine and tension-type headache.
3. Sources of data
The first step in non-fatal estimation was the compilation of data sources from systematic data and literature searches conducted by cause. This process resulted in 4,043 published studies newly included in GBD 2016, leading to a total of 14,521. Our network of collaborators for GBD 2016 provided 2,598 data sources and studies. These were systematically screened, together with sources suggested by country-level experts, surveys located in multinational survey data catalogues, and Ministry of Health and Central Statistical Office websites. We analysed 18,792 sources of epidemiological surveillance data (country-years of disease reporting), up from 14,081 in 2015. All counts reflect our updated counting criteria for GBD 2016. The supplementary methods provides details of data adjustments, correction factors, and standardisations employed in incorporating these different data types (appendix 1, p 18).
The number of location-years of hospital inpatient data by cause increased from 1176 in GBD 2015 to 3557 in GBD 2016. This increase can be attributed to the addition of new years of data for some locations, as well as newly incorporated data for 16 countries where we had previously lacked clear information about the population covered. To allow their use in GBD, we first collated information from surveys and hospital administrative records to estimate hospital admission rates per capita for all GBD locations by age and sex, from 1990 to 2016, using DisMod-MR 2.1 (appendix 1, p 7). We then used inpatient data by cause from locations with unclear denominators as cause fractions of the all-cause inpatient admission rates. Three adjustment factors were derived from USA health insurance claims data on more than 80 million person-years of coverage. The first factor corrected for multiple inpatient episodes for the same cause in an individual. The second adjustment was to include secondary diagnostic fields. The third adjustment was to include any mention of a cause in inpatient or outpatient episodes of care as opposed to inpatient episodes with a primary diagnosis only. This new method of predicting prevalence or incidence from inpatient data allowed us to use these sources for 16 more causes than in 2015. The supplementary methods provides a detailed description of our process for inpatient data (appendix 1, p 11).
To provide a summary view on data availability, the number of causes at the most detailed level for which we have any prevalence or incidence data from 1980 to 2016 by location is presented in the appendix (appendix 1, p 722). An online search tool is available to view all data sources that were used in the estimation process for each cause.
4. Non-fatal disease models
Non-fatal diseases were modelled using DisMod-MR 2.1, a statistical method that synthesises sparse and heterogeneous epidemiological data for non-fatal outcomes. Estimation occurred at five levels: global, super-region, region, country, and subnational locations, with results from a higher level providing guidance for the analysis at a lower geographical level (appendix 1, p 18).
Custom models were created where DisMod-MR 2.1 does not capture the complexity of the disease, or if incidence and prevalence needed to be calculated from other data. Further details of these custom models can be found in the supplementary methods (appendix 1, p 18). Prevalence was estimated for nine impairments, disorders that are sequelae of multiple diseases and for which there were better data available to estimate the overall occurrence than for each underlying cause: anaemia, intellectual disability, epilepsy, hearing loss, vision loss, heart failure, infertility, pelvic inflammatory disease, and Guillain-Barré syndrome.
The methods for estimating YLDs from a number of diseases changed substantially for GBD 2016. We improved our estimation of mortality-to-incidence ratios for cancers to better reflect lower survival probabilities in low-income and middle-income locations based on each location's Socio-demographic Index (SDI) value. As a consequence, our prevalence and YLD estimates were lower in those locations but did not change much for higher-SDI locations. We made major changes to our modelling of tuberculosis. First, we made explicit estimates of latent tuberculosis infection from tuberculin skin testing data and the risk of developing active tuberculosis by induration size. Second, we predicted mortality-to-incidence ratios in locations with high data-quality ratings (4–star or 5–star using a system developed for the GBD 2016 causes of death estimation) [18] and SDI as a covariate. We anchored the lower end of the SDI scale with a datapoint from an untreated cohort of pulmonary tuberculosis cases in the 1960s, half of whom had died after five years. [18, 19] Third, we estimated incidence from these mortality-to-incidence ratios in all locations except those with higher reported notifications. Fourth, we modelled these incidence estimates as well as the prevalence data from surveys in low-income and middle-income countries and cause-specific mortality rates among the proportion of the population with latent infection in DisMod-MR 2.1. Fifth, we estimated the proportions of tuberculosis cases with multidrug-resistant tuberculosis or extensively drug-resistant tuberculosis from notification and survey data and included an increased risk of multidrug-resistant tuberculosis in HIV/AIDS-infected patients with tuberculosis from a meta-analysis. [20]
In our measles estimation strategy, we included the coverage of measles-containing vaccine second-dose (MCV2) rather than just the coverage of the primary vaccine as a covariate. As relatively few countries in sub-Saharan Africa have introduced MCV2, the estimated incidence for those locations is notably higher compared with previous estimates.
5. Severity distributions and disability weights
For 214 causes at Level 4 of the GBD hierarchy, sequelae were defined in terms of severity, usually graded as mild, moderate, or severe outcomes. We followed the same approach as in GBD 2015. For Zika virus disease, we included sequelae for those with symptomatic acute infection, a small proportion with Guillain-Barré syndrome, and the number of neonates with congenital Zika virus disease as reported to the Pan American Health Organization (PAHO). For sexual violence, we estimated YLDs associated with concurrent physical injuries and the short-term psychological outcomes following sexual violence.
A more substantial change in estimating severity was applied to stroke. A systematic review was done to collect data on modified Rankin scores, a measure of neurological disability. [21] Levels of Rankin score were analysed in DisMod-MR 2.1 and mapped to the existing GBD health state lay descriptions for mild, moderate, and severe motor impairment from stroke, and, separately, the proportion of stroke patients with moderate-to-severe motor impairment who also experienced cognitive impairment. For GBD 2016 we used the same disability weights as in GBD 2013 and GBD 2015; the supplementary methods provides a complete listing of lay descriptions of all 235 health states used in GBD 2016 (appendix 1, p 799).
6. Comorbidity
We estimated comorbidity by simulating 40,000 individuals in every location-age-sex-year combination as exposed to the independent probability, based on the prevalence of the sequelae included in GBD 2016. In simulants with two or more sequelae, we assumed a multiplicative function to combine disability weights and then distributed the reduced combined weight proportionately among all comorbid sequelae. Averaging these adjusted values across all simulants with a particular sequela gave the adjusted value of YLDs. There was no change in the approach compared with GBD 2015.
7. YLD computation
All computations in GBD were done 1000 times, every time drawing from the distribution of the sampling error of data inputs, the uncertainty of data corrections for measurement errors, the uncertainty in coefficients from model fit (eg, in DisMod-MR 2.1), and the uncertainty of severity distributions and disability weights. Uncertainty bounds for a quantity of interest were defined by the 25th and 975th value of the ordered 1000 estimate values. If there was a change in disease estimates between locations or over time that was in the same direction in more than 950 of the 1000 samples we report it as significant. Age-standardised prevalence YLD rates were calculated based on the GBD reference population. [22]
The GBD cause hierarchy is comprehensive and includes 35 residual disease categories to capture YLDs from conditions for which we do not currently make separate estimates. For 22 of these residual categories, we made explicit epidemiological estimates of prevalence and incidence, and define sequelae based on the most common diseases in the Level 2 or 3 cause group and severity distributions from the Medical Expenditure Panel Survey (MEPS). [23] For 13 residual categories, we had no epidemiological data and estimated YLDs from the ratio of YLDs to YLLs from explicitly modelled diseases in the cause category, assuming that relative to each death, the number of YLDs was similar to that of other diseases at the same level of the GBD hierarchy (appendix 1, p 29).
8. SDI and epidemiological transition
SDI is a summary measure that places all GBD locations on a spectrum of socioeconomic development. [24] The SDI was developed for GBD 2015 to provide a comparable metric of overall development. This was achieved by using an equal weighting of lag-distributed income per capita, average years of education in the population over age 15 years, and total fertility rate. [22] For GBD 2016, we modified the estimation of SDI by taking into consideration that SDI scales were subject to change based on increasing geographic units and an extended time period of analysis, affecting the interpretability across GBD iterations. We redefined the values of zero and one for each component of the index: zero now represents the level below which we have not observed GDP per capita or educational attainment or above which we have not observed the total fertility rate in known datasets. Maximum scores for educational attainment and Lagged Distributed Income represent a plateau in the relationship between each of the two components and life expectancy or under–5 mortality rates, suggesting no additional benefit. Analogously, the maximum score for total fertility rate represents the minimum level at which the relationship with the selected health outcomes plateaued. An SDI value was generated for each location and year as the geometric mean of each component score. Five SDI quintiles, high, high-middle, middle, low-middle, and low, were selected based on 2016 values of SDI; additional details are available in the supplementary methods (appendix 1). [22]
A Gaussian process regression was used to evaluate the average relationship for each age-sex-cause group, for cause-specific YLD rates on SDI at Levels 1, 2, and 3 of the GBD cause hierarchy using data from 1990 to 2016. These rates were used as the expected values for cause-specific YLD rates at a given level of SDI. Additional detail on this analysis is available in the supplementary methods (appendix 1, p 30) and in previous GBD publications.18
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or the writing of the report. All authors had full access to the data in the study and had final responsibility for the decision to submit for publication.
Results
Global prevalence and incidence
Global prevalence, incidence, and YLDs for 328 causes and nine impairments, as well as percent change of YLDs and percent change of age-standardised YLD rates from 2006 to 2016 are listed in the table. Cause-specific estimates for each year of the GBD estimation period 1990–2016 by location, age, and sex are available through an online results tool.
Prevalence

Table In 2016, the ten causes with the greatest prevalence were caries of permanent teeth (2·44 billion, 95% UI 2·29 billion to 2·59 billion), latent tuberculosis infection (1·91 billion, 1·79 billion to 2·03 billion), tension-type headache (1·89 billion, 1·71 billion to 2·10 billion), age-related and other hearing loss (1·27 billion, 1·21 billion to 1·34 billion), iron-deficiency anaemia (1·24 billion cases, 1·21 billion to 1·28 billion), migraine (1·04 billion, 1·00 billion to 1·09 billion), glucose-6-phosphate dehydrogenase deficiency (G6PD) trait (866 million, 852 million to 882 million), genital herpes (860 million, 748 million to 992 million), refraction and accommodation disorders (854 million, 822 million to 886 million), and ascariasis (800 million, 738 million to 872 million; table). The vast majority of cases for two of these causes are asymptomatic sequelae that have no YLDs associated with them: genital herpes with no active lesions, and G6PD trait that does not result in anaemia. Similarly, latent tuberculosis infection is a highly prevalent cause but without any associated disability. The leading ten causes of prevalence accounted for 17·5% (95% uncertainty interval [UI] 15·8–19·3) of YLDs globally in 2016.
Incidence
In 2016, the ten causes with the highest incidence wereupper respiratory infections (17·78 billion, 15·85 billion to 19·90 billion),
caries of permanent teeth (7·26 billion, 6·72 billion to 7·84 billion),
diarrhoeal diseases (4·48 billion, 4·25 billion to 4·74 billion),
fungal skin diseases (2·10 billion, 1·88 billion to 2·34 billion),
caries of deciduous teeth (1·76 billion, 1·26 billion to 2·39 billion),
tension-type headache (1·06 billion, 899 million to 1·24 billion),
other sense organ diseases (708 million, 668 million to 754 million),
other skin and subcutaneous diseases (634 million, 617 million to 652 million),
vitamin A deficiency (552 million, 469 million to 671 million), and
pyoderma (474 million, 461 million to 489 million; Table.These ten causes of incidence accounted for 4·4% (3·7–5·6) of all YLDs globally in 2016.
Overall global numbers of YLDs and trends 2006–2016
Globally, communicable, maternal, neonatal, and nutritional deficiency diseases accounted for 12·6% (95% UI 11·3–14·0) of YLDs in 2016 (101·5 million, 72·3 million to 136·9 million), while NCDs accounted for 80·6% (78·2–82·5) or 648·6 million (481·3 million to 836·5 million) of YLDs and injuries accounted for 6·9% (5·6–8·4) or 55·4 million (37·2 million to 78·7 million) of YLDs (table). In 2016, the age-standardised YLD rate for all causes was lowest in China at 9,201 YLDs per 100,000 (95% UI 6862–11 943 per 100,000); Yemen had the highest age-standardised YLD rate at 14,774 YLDs per 100,000 (11 018–19 228 per 100,000).

Figure 1A + B

Figure 1C Fig. 1 Legend Figure 1C shows the change in global YLDs over time in three ways: mean percentage change in number of YLDs, mean percentage change in all-age rates, and mean percentage change in age-standardised YLD rates from 1990 to 2006 and from 2006 to 2016. The mean percentage change in the number of YLDs reflects the combined effects of population growth, population ageing, and epidemiological change. Population ageing and epidemiological change explain the mean percentage change in all-age rates. The mean percent change in age-standardised YLD rates reflects epidemiological change that is not due to ageing or population growth. All top–30 YLD causes increased in the number of YLDs between 1990 and 2016. Alcohol use disorder, major depressive disorder, and refraction and accommodation errors had the largest declines in age-standardised YLD rates from 2006 to 2016 but the change did not exceed 5%. Preterm birth complications had the largest increase in age-standardised YLD rates, 8·5%. Among the top 30 causes of YLDs, the difference between the change in all-age and age-standardised rates between 2006 and 2016 was 10% or greater for age-related and other hearing loss, diabetes, chronic obstructive pulmonary disease (COPD), osteoarthritis, ischaemic stroke, edentulism, and ischaemic heart disease, indicating that these diseases largely affect the elderly and therefore become more prominent causes of YLDs in an ageing global population.
Low back pain and migraine were the leading causes of YLDs in high-income, high-middle-income, and middle-SDI quintile countries, but iron-deficiency anaemia was the leading cause in low-middle-SDI and low-SDI quintiles in 2016 (appendix 2, p 14). Low back pain, migraine, and age-related and other hearing loss were in the top five causes of YLDs in all SDI quintiles. Major depressive disorders appeared in the top five in all quintiles but the middle, where it was displaced by diabetes. Neck pain was a top five cause of YLDs in high-income, high-middle-income, and middle-SDI quintiles. In 2016, 28 of the 30 leading causes of age-standardised YLD rates for high-SDI countries were NCDs, versus 23 out of 30 in low-SDI countries. Between 2006 and 2016, there were large drops in age-standardised rates of YLDs for malaria, HIV/AIDS, onchocerciasis, and schistosomiasis in the low-SDI quintile.
Leading causes of YLDs by age-standardised rates

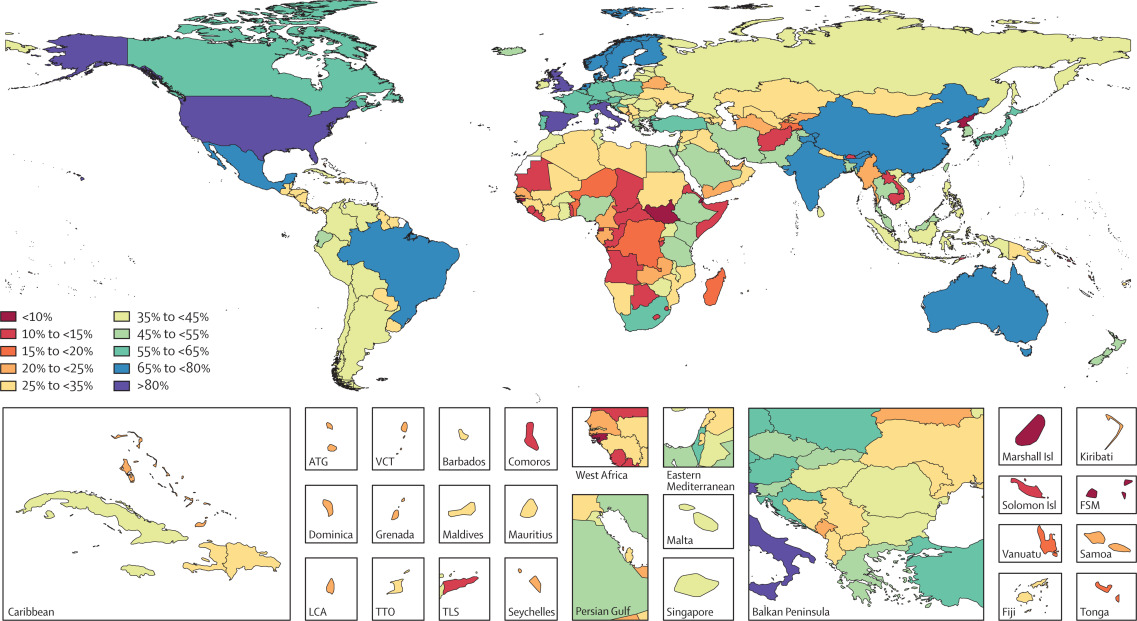
Figure 2A

Figure 2B Fig. 2 Legend For men, the most common leading detailed cause of YLDs in 2016 was low back pain, resulting in the highest age-standardised rates of YLDs in 133 of 195 countries and territories, including every country in the high-income regions, central and eastern Europe, central Asia, Andean and Tropical Latin America, and eastern and central sub-Saharan Africa, as well as most countries in southeast Asia, north Africa and the Middle East, and western sub-Saharan Africa. Diabetes, the second most common leading cause of YLD rates for men, ranked first in 38 countries in Central Latin America, the Caribbean, Oceania, and North Africa and the Middle East. Iron-deficiency anaemia was the leading cause in India, Bhutan, Sudan, Yemen, and Mali. HIV/AIDS was the leading cause in South Africa, Lesotho, Swaziland, Namibia, and Botswana.
In 2016, low back pain was the leading cause of age-standardised YLD rates for women in 104 of the 195 countries and territories (Figure 2B). It was the main cause of YLDs in almost all high-income, central Europe, eastern Europe, North Africa and the Middle East, and Andean and Tropical Latin American countries. Iron-deficiency anaemia was the leading cause for women (35 countries), followed by migraine and diabetes in 24 and 17 countries, respectively. HIV/AIDS was the leading cause in southern sub-Saharan Africa, Zambia, and Malawi.
YLDs over time for countries classified into SDI quintiles in 2016

Figure 3 Trends for the number of YLDs (in millions) and age-standardised YLD rates from 1990 to 2016 at Level 1 of the GBD cause hierarchy are shown by SDI quintile in Figure 3. Generally, there was little or no change in the age-standardised rates of YLDs for NCDs, communicable, maternal, neonatal, and nutritional causes, or injuries, apart from a decrease in communicable, maternal, neonatal, and nutritional YLD rates between 2000 and 2016 in the low-SDI quintile. The large increase in total YLD numbers for NCDs reflects the combined effect of population growth, ageing, and epidemiological change. NCDs contributed the most YLDs at each SDI quintile, followed by communicable, maternal, neonatal, and nutritional causes and injuries, with exceptions for high and high-middle quintiles, where injuries contributed more YLDs than communicable, maternal, neonatal, and nutritional causes in 2016. This was particularly the case at the highest level of SDI, where YLDs from communicable, maternal, neonatal, and nutritional causes and injuries represented only a small fraction of overall YLDs.
YLD pattern by age and sex

Figure 4

Figure 5 Between 1990 and 2016 the number of YLDs for 21 Level 2 causes increased, particularly in the 40–69 year age range (Figure 4). In childhood, other NCDs (skin diseases being the largest contributor in this category), nutritional deficiencies, infectious diseases, and mental and substance use disorders were the main causes of YLDs. After childhood, NCDs were the dominant source of YLDs. Mental and substance use disorders were the largest contributors to disability in young adults, while at older ages, other NCDs (with hearing loss and vision loss being the largest contributors to this category), musculoskeletal disorders, and cardiovascular diseases were the most important causes. YLDs from injuries were largest between ages 20 and 69 years.
YLD rates were higher in males than in females at ages under 10 years and between ages 75 and 94 years (Figure 5). At all other ages, all-cause YLD rates were higher in females. Boys had higher YLD rates for mental disorders (particularly conduct disorder and autism), while girls had higher YLD rates for other non-communicable diseases (most of this difference is explained by higher YLD rates from dermatitis). At ages over 10 years, musculoskeletal disorders contributed most to higher YLD rates in females. The next two cause groups with higher YLD rates in females were neurological disorders (particularly migraine and, at older ages, Alzheimer's disease and other dementias) and nutritional deficiencies (mostly iron-deficiency anaemia). The sex differences in mental and substance use disorders were small, with slightly elevated rates in younger males, and somewhat higher rates in older females. The small overall sex difference masks much higher YLD rates from depressive disorder and anxiety in females and higher YLD rates from injuries, substance use disorders, and autism spectrum disorders in males. Adult males older than 55 years had higher YLD rates from diabetes, urogenital, blood, and endocrine disorders (diabetes and benign prostatic hyperplasia being the main drivers of differences), injuries, chronic respiratory diseases, and cancers.
Rates of YLDs and change in rates of YLDs by cause

Figure 6
Fig. 6 Legend Figure 6 shows the annualised rates of change in age-standardised YLD rates between 2006 and 2016, with Level 3 causes against age-standardised YLD rates presented on a log-scale from right to left. 15 causes significantly increased by more than 1%: six cancers (brain and nervous system, liver, non-Hodgkin lymphoma, testicular, thyroid, and other neoplasms), dengue, gastritis and duodenitis, leishmaniasis, neonatal encephalopathy due to birth asphyxia and trauma, neonatal sepsis and other neonatal infections, other chronic respiratory diseases, other neurological disorders, peptic ulcer disease, and Zika virus disease. Of 31 causes with declines of greater than 1·0% per year, 25 were communicable, maternal, neonatal, and nutritional causes and five were NCD causes. Road injuries was the only cause out of 30 causes with age-standardised rates of YLDs greater than 100 per 100,000 that significantly increased by more than 0·5% annually. There were no large causes with a greater than 0·5% decrease in age-standardised YLD rates.
Leading causes of YLDs and deviations from expected levels based on SDI
Figure 7A
Figure 7B
Figure 7C
Figure 7D
Figure 7E
Figure 7F
Figure 7G
Fig. 7 Legend Age-standardised YLD rates for the top ten most detailed causes are plotted by region and year against SDI in the supplementary results (appendix 2, p 4). The black solid line represents the expected value based on SDI. Two of the top ten causes, iron-deficiency anaemia and age-related and other hearing loss show a large decline in expected values with increasing SDI, while the regional estimates are relatively close to the expected line. The interpretation is that much of the variation in YLD rates for these two causes is linked to SDI. The expected lines for the other top ten conditions show a less clear pattern with SDI while regional estimates are dispersed widely around the line. These graphs show that most of the variation in YLD rates for these leading causes of YLDs depends on factors other than sociodemographic development, unlike the much clearer relationship between SDI and rates of YLLs for the leading causes of death. [18]
Low back pain and migraine ranked in the top ten of YLDs in all 195 countries and territories in 2016. Adult-onset hearing loss was in the top ten in 193 countries and territories. Major depressive disorder ranked in the top ten in all but four countries. Anxiety disorders, iron-deficiency anaemia, neck pain, diabetes, and other musculoskeletal disorders ranked in the top ten of more than half of the countries and territories (Figure 7).
Apart from showing the top ten causes of YLDs by country, Figure 7 also shows for each top ten cause the variation from expected values based on SDI. The cells in dark red have at least twice the expected values and those in dark blue at least 50% lower values. In the high-income super-region, the USA had much higher than expected YLDs from opioid dependence. YLDs due to Alzheimer's disease and other dementia were more than double what was expected in Italy and Japan. Greece had much higher than expected rates of COPD. YLDs from other musculoskeletal disorders were more than twice the expected values in Australia, Canada, Chile, Greenland, and the USA. Many eastern and central European countries had much higher than expected YLDs from falls, alcohol use disorders, and ischaemic stroke. Four countries in central Asia had more than twice the expected rates of iron-deficiency anaemia. In Latin America, YLDs from diabetes were more than twice the expected rate in Barbados, Jamaica, Mexico, Puerto Rico, Saint Vincent and the Grenadines, Trinidad and Tobago, and the Virgin Islands. Venezuela had less than half the expected rate of YLDs from low back pain but more than double the expected rate of YLDs from diarrhoea.
Haiti had higher than expected YLDs from asthma. YLDs from iron-deficiency anaemia were more than double the expected rate in five Caribbean nations. China had more than twice the expected YLD rate of ischaemic stroke, while North Korea had more than double the expected YLD rate for neck pain. In the southeast Asia region, YLD rates of iron-deficiency anaemia were more than twice the expected values in Maldives and Mauritius. Mauritius also had more than twice the expected YLD rates for diabetes and COPD. Thailand and the Seychelles had more than twice the expected rate of COPD. Timor-Leste was the only country in the region where lymphatic filariasis and long-term disability from conflict ranked among the top ten causes of YLDs. Diabetes ranked highly in all island nations of Oceania with much higher YLDs than expected based on SDI. In North Africa and the Middle East, more than twice the expected YLD rates from opioid dependence were found in Afghanistan, Bahrain, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Palestine, Oman, Qatar, and the United Arab Emirates. Afghanistan and Bahrain had more than twice the expected YLD rates of diabetes. Long-term disability from injuries sustained during conflict ranked in the top ten for Afghanistan, Lebanon, Syria, and Iraq.
Iron-deficiency anaemia was much higher than expected in India and Bhutan. India had considerably higher than expected YLDs from COPD. Bangladesh was the only country in 2016 with YLDs from the residual category of other congenital anomalies in the top ten. Bhutan had more than double the expected YLDs from diarrhoea. HIV/AIDS was the leading cause of YLDs in southern sub-Saharan Africa. Malaria ranked in the top ten for YLDs in 14 sub-Saharan African countries. Three neglected tropical diseases, schistosomiasis, lymphatic filariasis, and onchocerciasis, ranked in the top ten of YLDs in six, three, and seven sub-Saharan African countries, respectively. In Madagascar, protein-energy malnutrition ranked in the top ten. Epilepsy was a top ten cause of YLDs in Senegal and São Tomé and Príncipe. Much lower than expected YLDs from iron-deficiency anaemia were found in Burundi, Ethiopia, and Rwanda. The long-term consequences of injuries sustained during the 1994 genocide in Rwanda still ranked among the top ten causes of YLDs in 2016.
Discussion
Summary of main findings
The largest Level 2 disease groups contributing to non-fatal burden in 2016 were mental and substance use disorders (18·7%, 95% UI 15·9–21·0), other NCDs (18·6%, 15·6–22·5), and musculoskeletal disorders (17·1%, 15·3–18·9), together covering more than half of global YLDs. Despite mostly stagnant age-standardised rates, the number of YLDs from NCDs grew rapidly in all the SDI quintiles, due to population growth and ageing. Across all causes of YLDs, age-standardised rates of YLDs decreased between 1990 and 2016 by 2·7% (95% UI 2·3–3·1) in contrast to the 39·1% (37·8–40·2) decrease in YLL rates over the same time period.18 Thus, the relative contribution of YLD to the overall burden of disease in DALYs increased from 21·7% (17·2–26·6) in 1990 to 33·5% (27·4–39·7) in 2016.
Age-standardised YLD rates for all conditions combined were 10·4% (9·0–11·8) higher in women compared to men. Iron-deficiency anaemia, migraine, Alzheimer's disease and other dementias, major depressive disorder, anxiety, and all musculoskeletal disorders apart from gout were the main conditions contributing to higher YLD rates in women. Men had higher age-standardised rates of substance use disorders, diabetes, cardiovascular diseases, cancers, and all injuries apart from sexual violence.
Globally, we found much less geographical variation in disability than has been documented for premature mortality. In 2016, there was a less than two-fold difference in age-standardised YLD rates for all causes between the location with the lowest (China, 9,201 YLDs per 100,000, 95% UI 6,862–11,943 per 100,000) and highest rates (Yemen, 14,774 YLDs per 100,000, 11,018–19,228 per 100,000). By contrast, there was a greater than tenfold range in age-standardised rates of YLLs between countries in GBD 2016. [18] Two other countries with mainly Chinese populations, Singapore and Taiwan (Province of China), were ranked second and fourth lowest in terms of age-standardised YLD rates, respectively. The low YLD rates in China were largely determined by much lower prevalence of headaches, musculoskeletal disorders (in particular low back pain), major depressive disorder, iron-deficiency anaemia, falls, and anxiety. Low rates of reporting chronic pain and low prevalence of depressive disorder and anxiety in China and among Chinese immigrants elsewhere have frequently been reported, but these findings may partly be explained by standard diagnostic tools inadequately detecting cases in the Chinese and cultural differences in the perception and communication of pain. [25–29]
Trends across the causes of YLD were also different. For example, age-standardised YLD rates for NCDs were stagnant between 1990 and 2016 and showed little variation by SDI quintile; YLD rates for communicable, maternal, neonatal, and nutritional diseases were highest at lower SDI quintiles but with a steady drop; and injury YLD rates showed modest declines since 1990. Over the same period, age-standardised YLL rates of communicable, maternal, neonatal, and nutritional diseases rapidly declined, particularly in lower SDI quintiles. The decline in YLL rates from NCDs was slower than the decline in communicable, maternal, neonatal, and nutritional diseases but still substantial. The main causes of YLLs and YLDs were also notably different. Of the top 30 causes of YLLs, only seven appeared in the top 30 causes of YLDs (diabetes, falls, COPD, ischaemic stroke, neonatal preterm birth complication, diarrhoeal diseases, and ischaemic heart disease). At Level 4, 17 of the top 30 causes of YLDs were diseases for which we estimated no YLLs as they are not considered underlying causes of death.
Cross-cutting themes
The availability and quality of epidemiological data the GBD Study draws upon to make non-fatal estimates vary enormously among diseases and by location. A multitude of study methods and preferred case definitions pose challenges to making comparable estimates. A large part of the effort in the GBD study in making non-fatal estimates is to identify and correct for known sources of measurement error. The main classes of data sources each have their own limitations. Surveys can be biased by low response rates or by exclusion of individuals who do not reside in a traditional household, and may be limited in the capacity to properly identify cases within the limited diagnostic means available during a survey. Administrative data on health service encounters include only those seeking and receiving health care and are likely biased toward more severe disease, but may offer more accurate diagnostic variables than available in surveys.
With the development of electronic medical records and advancements in linkage between data sources, non-fatal population health assessments can benefit tremendously if survey and administrative records can be linked. This would help to overcome many of the limitations of individual data sources: administrative records can provide rich diagnostic information, while surveys can provide better information on cases that are not in contact with health services, exposure to risk factors, and health status measures that can provide information on severity. The challenges in low-income and middle-income countries will be to fund the data systems and infrastructure and development of technical expertise, and to provide access to generic rather than proprietary software to manage electronic medical record data and produce the linkages while preserving confidentiality.
In the GBD 2016 companion paper on causes of death [18] we reported a faster decline in age-standardised YLL rates for the top ten causes of YLL (ischaemic heart disease, cerebrovascular disease, lower respiratory infections, diarrhoeal diseases, road injuries, neonatal preterm birth complications, malaria, COPD, HIV/AIDS, and neonatal encephalopathy) than for the rest of causes, globally and in each of the SDI quintiles. We hypothesised that a greater investment in large causes has led to greater improvements. We did not observe an equivalent rapid decline in the age-standardised YLD rates for these top ten causes of YLLs. YLD rates for ischaemic heart disease, stroke, LRI, COPD, and road injuries increased by less than 10% over the last ten years. YLDs for diarrhoeal diseases declined by less than 10%. The only top ten YLL causes with a greater decline in YLD rates were HIV/AIDS and malaria, though at a lesser pace than the change in YLL rates. Antiretroviral treatment greatly reduces the death rate in persons living with HIV but also improves the immune status of survivors.
Thus, while there was a small increase in prevalence, the age-standardised YLD rate dropped by almost a fifth since 2006 as a larger proportion of cases were estimated to be in higher CD4 categories, for which we apply a lower disability weight. YLD rates from preterm birth complications and neonatal encephalopathy increased, while YLL rates dropped by almost a quarter. Improved survival through neonatal intensive care interventions predisposes survivors to the risk of long-term disabling outcomes. In terms of how we measure the burden of disease in DALYs, this means that large gains by prevention of YLLs can be accompanied by a smaller amount of health loss in terms of YLDs in new survivors. Similarly, health interventions that address mortality by reducing the case fatality among causes of disease or injury may in turn lead to an increase in non-fatal outcomes. For example, reducing cardiovascular risks in people with diabetes will increase the prevalence of those with sequelae such as neuropathy or vision loss. Similarly, preventing death from a myocardial infarction by revascularisation improves survival and thus exposes more people to heart failure as a complication.
The MDGs focused health policy on predominant infectious, neonatal, and maternal causes of death. The health-related SDGs have expanded into a number of non-communicable diseases and injuries. However, the focus remains on reducing mortality rather than the main causes of disability. The only goals that correspond with non-fatal outcomes are those related to substance use (goal 3.5) and physical and sexual violence (goals 5.2, 11.7, 16.1, and 16.2). Furthermore, the targets formulated on incidence of HIV, tuberculosis, malaria, and hepatitis were included because of the large number of deaths associated with these infectious diseases rather than presumably out of concern for their non-fatal outcomes. [1] Diabetes and opioid use disorder are the only causes in the top 20 of age-standardised YLD rates at Level 4, globally, that are mentioned in the SDGs. The diabetes target, however, is formulated as an indicator of mortality only. The mental, musculoskeletal, sense organ, and neurological disorders that contribute to more than half of all YLDs are not considered. While this may partially be a bias toward assessing global health in terms of mortality, it may also reflect a perception that there is inadequate knowledge to address these major causes of disability. Indeed, the much smaller gap in YLD rates compared to the large differences in YLL rates between high-SDI and low-SDI countries suggests that the capacity to intervene in non-fatal outcomes is more limited.
Several threats exist that could lead to reversals in global health gains, such as widespread antimicrobial resistance, [30, 31] conflict, [32] climate change, [33, 34] and obesity. [35] Of these, obesity has the more immediately apparent health consequences and has a large effect on non-fatal outcomes such as diabetes, low back pain, and osteoarthritis. The increase in diabetes incidence due to obesity and the improved survival in people with diabetes, largely through prevention of deaths from cardiovascular complications, both contribute to increases in prevalence and a need for intensive long-term management to prevent fatal and disabling complications. Recent conflicts such as those in Libya, South Sudan, Syria, and Yemen are major health threats not only in terms of casualties but also because they lead to long-term physical and mental consequences directly related to the violence as well as the broader health consequences of disrupted health services and declining economic status. [36]
Important changes in GBD 2016 compared with GBD 2015
The intensive collaborations with countries for which we present subnational estimates and the expanding network of GBD collaborators have contributed to a 36·2% increase in data sources for non-fatal outcome estimates compared to GBD 2015, as well as greater scrutiny of our methods and results. In particular, the close collaboration with the Indian Council for Medical Research and the Public Health Foundation of India, and 14 disease expert groups convened by these partners, has greatly enhanced the quality of the estimates for India. There was a 49·9% increase in non-fatal data sources in India, and disease experts provided access to state-level data for causes, while in GBD 2015 we had only access to national aggregates.
Increasingly, the GBD Study is making use of administrative data based on health care encounters. Public access to these data sources at the level of detail required for GBD analyses remains limited, and enormous scope remains to expand access to these valuable sources of health information in many more countries. By estimating total admission rates from both administrative and survey sources, we were able to increase the number of countries with available inpatient data from 26 in 2015 to 41 in 2016. To predict the level of disease under any type of care for other countries with inpatient data available, we applied the ratio of people with a diagnosis during inpatient and outpatient episodes to that of inpatient diagnoses only in US medical claims data. In our analyses for most conditions, the administrative data sources were adjusted to the level of a reference case set for the disease of interest. Thus, we make use of the detailed information on age and sex in these data sources while adjusting for a potential systematic bias compared to data sources with measurements according to the reference case. For instance, our reference case for diabetes prevalence was the proportion of a population with fasting plasma glucose greater than 7 mmol/L or on diabetes treatment in a representative survey. The adjustment of administrative data reflects the proportion of people with diabetes who may be unaware of their condition or who for other reasons have not contacted health services in the year of interest.
To estimate indicators of sexual violence for the SDGs, we added sexual violence as a subcause of interpersonal violence in the GBD hierarchy. The focus of the effort in GBD 2016 has been to estimate the prevalence of people who report sexual violence by intimate partners and other perpetrators in the last 12 months. For non-fatal outcomes, we quantified the immediate concurrent physical injuries and the more immediate mental health consequences. We realise this is a limited scope for estimating all relevant health loss from sexual violence. In future iterations of GBD we intend to include sexual violence as a risk factor for longer-term outcomes such as major depressive disorder, anxiety disorder, and substance use disorders. Going forward, we aim to become more comprehensive in our estimation of violence to include the wider health consequences of physical violence to children and adults as well as bullying.
Although efforts were undertaken to update data for all causes of YLDs in GBD 2016, a number of sources of new data were especially influential in improving estimates for selected causes. A large number of rapid-assessment vision loss surveys [37] contributed to an increase in the number of sources to measure vision loss and its underlying causes from 397 in 2015 to 768 in 2016, with data available in 75 low-SDI and middle-SDI countries. Likewise, the Global Atlas for Helminth Infections Project provided a large amount of new data for schistosomiasis and lymphatic filariasis. [38]
A new approach to fitting ensembles of distributions improved the estimation of anaemia by better representing the tail end of the distributions of haemoglobin that most concerns our estimation of disability than can be derived from a single parametric distribution. This is important because for many surveys for which we rely on academic papers and survey reports we only have data for means and standard deviations.
The change in modelling strategy for tuberculosis was substantial. The new estimates of the prevalence of latent tuberculosis infection is of policy interest, as there are intervention strategies that target treatment of latent tuberculosis in high-risk individuals. [39] It allowed us to model active disease among those with latent infection to improve the search for a consistent fit between cause of death rates, prevalence surveys, and notification of incident disease, the three main sources of epidemiological data on tuberculosis. Next, we estimated the association between SDI and the ratio of mortality to incidence, assuming this measure of case fatality is dependent on development as a proxy for quality of case finding and management. This provided greater alignment of mortality and non-fatal estimates of tuberculosis than we have been able to achieve in past GBD studies.
A substantial new effort on the severity of stroke was the analysis of 18 studies providing Rankin score data on the severity of disability in stroke survivors. Thus, we were able to make estimates by age, sex, year, and location to capture greater nuances in outcomes – for example, reflecting differences in access to rehabilitative services.
Disease-specific considerations
The GBD study is the only source of comprehensive quantification of the disabling outcomes of diseases and injuries. For a number of diseases there are efforts to estimate global disease prevalence or incidence. Where appropriate, in the following sections on major sources of YLDs, comparisons with other global estimates are made; further detail can also be found in the supplementary methods (appendix 1, p 30).
Mental and substance use disorders
GBD 2016 confirms that mental and substance use disorders, led by depressive disorders, are a major cause of non-fatal burden. With age-standardised prevalence and YLD rates for mental and substance use disorders showing less than 10% change between 1990 and 2016, apart from bulimia YLD rates which increased by almost 20%, our findings show no sizeable improvement in population mental health over time at the global level. Interventions can decrease the severity or increase remission for certain disorders and can be effectively administered in low-income, middle-income, and high-income settings. [40] However, these have yet to be brought up to scale in most countries. Because there are no data measuring the severity of mental disorders in a consistent manner, we have been unable to capture treatment effects that alter severity of disease. By imposing severity distributions from two high-income countries only, we are probably underestimating the burden of mental disorders in countries with less access to quality care.
Musculoskeletal disorders
Low back pain and neck pain are the two largest causes of musculoskeletal disability; their measurement is fully dependent on self-report measures. In GBD, we adjust for variations in recall period, anatomical location, minimum duration of episodes, and whether activity-limiting or not. Although less than 40% of low back pain can be attributed to occupational risks or increased BMI, there are no risks in GBD that are linked to neck pain. The lack of predictive covariates raises concern that we might be assigning measurement error as spatial variation and that the two to two-and-a-half-times difference in age-standardised prevalence between locations is overestimating true differences in disease occurrence of these two conditions.
Diabetes
Several factors have contributed to the increase in the prevalence of diabetes. Ageing of populations along with greater exposure to lifestyle-related risk factors, most importantly high BMI, has increased the incidence of diabetes in almost all countries. [41] At the same time, improvements in treatment of diabetes have increased the life expectancy among people with diabetes. The large increase in prevalence imposes a substantial economic burden on health-care systems. In the USA, diabetes was responsible for the largest health-care spending and the greatest increase over the past two decades among 155 health conditions. [42] This highlights the importance of development and implementation of more effective population-level strategies to prevent diabetes.
Dementia
Age-standardised prevalence of dementia varied four-times between countries. Dementia surveys generally have a two-step approach to identifying cases, with an initial screening phase followed by more intensive diagnostic procedures in those who screened positive. We scrutinised all sources of dementia and identified a wide range of screening and diagnostic tools, varying thresholds on these methods, and diagnoses made according to different classification systems. This made it impossible to identify a reference study method or case definition. Thus, it is likely that we are overestimating the variation in prevalence.
Headaches
We changed our strategy to include medication overuse headache as a sequela of migraine and tension-type headache. This led to an increase in their prevalence and YLD estimates, particularly for migraine as more than two-thirds of medication overuse headache occurs in people with migraine as the primary headache. Thus, migraine has become the second largest cause of disability in 2016. As limited surveys are available that report on the frequency and duration of headache episodes, we have not been able to quantify any effect of treatment.
Malaria
Globally, malaria case incidence trends estimated in GBD 2016 followed a very similar pattern to GBD 2015, where there was a gradual rise in cases until 2005 followed by a steady decline. For all years, however, the updated estimates are approximately one-quarter lower than those from GBD 2015, reflecting mainly lower estimates outside Africa and in particular for India. Outside Africa, and for lower-burden countries within Africa, 2016 estimates were produced using a spatiotemporal geostatistical model. Globally, this improved approach led to a reduction in estimated cases of around 75 million (about 26% reduction) of which most (roughly 60 million fewer cases) were in India, with other notable reductions in Myanmar (roughly 11 million fewer), Indonesia (roughly 3 million fewer), and Pakistan (roughly 1 million fewer). In high-burden countries in sub-Saharan Africa, where the methodology remained similar to GBD 2015, changes were relatively modest and reflected the inclusion of newly available cross-sectional parasite rate surveys or updates to data on malaria intervention coverage in recent years.
Tuberculosis
For the first time, we have estimated the prevalence of latent tuberculosis infection. Globally, this disease affects 1·91 billion people (95% UI 1·79 billion to 2·03 billion) who are at risk of developing active disease when the immune system weakens through old age, HIV infection, diabetes, malnutrition, or excessive alcohol use. Globally, we estimate there were 10·4 million (9·37 million to 11·7 million) incident cases of tuberculosis in 2016, which is the same as the 10·4 million cases estimated by WHO for 2015. [43] The separate estimation of 331,000 cases (95% UI 293,000–373,000) of multidrug-resistant and 19,800 incident cases (17,300–22,600) of extensively drug-resistant tuberculosis with or without HIV infections has great policy relevance, as the resources required for treatment of resistant cases are many times greater given that treatment needs to be applied for a longer period and with more expensive drugs. Drug resistance also requires more expensive detection and monitoring methods. [44]
HIV/AIDS
A major change in methods for estimating burden of HIV/AIDS for GBD 2016 was the distribution of antiretroviral therapy coverage by age, sex, and CD4 count. We used two AIDS Indicator Surveys [45, 46] to predict the age-sex-CD4 distribution of antiretroviral therapy coverage. This shifted the coverage distribution to groups with higher CD4 counts and gave a better fit to the data. UNAIDS produces periodic updates to global, regional, and national estimates of HIV/AIDS incidence and prevalence. In their latest assessment there were 36·7 million (30·8 million to 42·9 million) people living with HIV/AIDS in 2016, compared with 36·4 million (34·2 million to 39·1 million) estimated by GBD 2016. [47] Comparisons of prevalence estimates at the country level in 2005 (the estimated peak of the HIV/AIDS epidemic globally) and 2016 show a high level of concordance between GBD 2016 and UNAIDS, with an average intra-class correlation coefficient of 0·992. For estimates of annual new infections, UNAIDS and GBD follow similar patterns, with UNAIDS having slightly lower estimates for years between 1996 and 2002. The estimates are similar between the two for most of the 2000s, with UNAIDS estimates showing a slightly faster rate of decline in annual new infections from 2008 to 2016 at the global level. GBD 2016 estimates about 1·9 million new infections globally in 2016, while UNAIDS estimates about 1.8 million for the same year. [47]
Cancer
Country-specific cancer statistics are published by the International Agency for Research on Cancer for their GLOBOCAN project. [48] Their most recent estimate of incidence for all cancers combined is 14·1 million cases in 2012, compared with GBD estimates of 14·8 million cases in 2010 and 17·2 million cases in 2016. The appendix provides a comparison of incidence by cancer type between GBD and GLOBOCAN (appendix 1, p 255).
Zika virus disease
The large outbreak of Zika virus disease in Latin America in 2016 led WHO to declare it a public health emergency of international concern. [49] There were 7·6 million new infections in 2016, 7·4 million of which occurred in Latin America and the Caribbean. Most of the health loss associated with Zika virus disease was from non-fatal outcomes, including fever and malaise during acute infection and congenital anomalies and Guillain-Barré syndrome as longer-term consequences.
Guinea worm
Guinea worm disease was included as a cause of non-fatal health loss because eradication of the disease is achievable in the near future.50Although not having received much attention in general global health policy debates, a remarkable reduction from an estimated 3·5 million cases in the mid–1980s to just 15 cases in 2016 has been achieved. Guinea worm eradication interventions include the distribution of filter cloths and pipe filters for drinking water, treatment of water sources with larvacide, case detection, containment to prevent further transmission, and health education. [50]
Limitations
The annual updates of GBD allow incremental improvements to methods. However, several measurement challenges in non-fatal estimation remain. The foremost concern is how best to disentangle measurement error from true variation in disease occurrence. We correct for known bias from non-reference methods or case definitions, but often have to rely on sparse information to make those adjustments. Lack of consensus among researchers on how to measure a disease can make it difficult to define a manageable set of alternative methods for which we can make adjustments. An extreme example is dementia: among 234 data sources we identified 228 different methods of screening, diagnostic tools, and diagnostic criteria. When possible, we use predictive covariates in our non-fatal models. For diseases with a lot of information on what drives differences in disease, covariates help to estimate true variation and minimise residual measurement error. However, many of the leading causes of YLDs lack strong predictors as indicated by our risk assessment, which assigned less than 20% of YLDs from mental, musculoskeletal, sense organ, and neurological disorders to the 79 risks evaluated in the GBD study. [51]
Second, many non-fatal models continue to rely on sparse data in some regions or super-regions despite the steady increase in data sources. With the addition of some new data sources, this can lead to large variation with previous GBD estimates. Alcohol dependence is a good example. Our estimate of the global prevalence of alcohol dependence increased by 70% after adding nine new data sources for Brazil, 12 for India, seven for sub-Saharan Africa, and four in eastern and central Europe. Until there is better coverage of data, non-fatal disease models will continue to be prone to estimates varying between GBD iterations.
Third, the adjustments to our hospital admission data for multiple admissions and secondary diagnosis fields reflect all health-care episodes rather than inpatient episodes only. Adjustments derived from a large, though non-representative, source of medical claims data in the USA are assumed to be generalisable. The generalisability of claims data, the validity of assuming diagnoses based on primary diagnosis alone or all diagnostic fields, and the validity of trends in claims data have been challenged. [52–56] Also, there may be considerable inter-country variation in how diseases are treated between inpatient and outpatient settings. Our models attempt to adjust for such potential biases by using a covariate on claims and hospital admission data to correct for systematic error, although in a relatively crude manner, this assumes no geographical variation in the error. Gaining access to claims data from other countries, particularly in low-income and middle-income countries, is a crucial endeavour for future GBD iterations.
Fourth, our estimates of severity distributions for most diseases are based on sparse studies from the literature for diseases with a more established consensus on a measure of severity, or our analyses of three high-income surveys which combine diagnostic information with a general health status measure, the Short Form-12 (SF-12). [40, 57, 58] Disease-specific researchers can provide better data with more routine use of a single established measure of severity in surveys and patient populations. Another potential improvement can be expected from countries that are able to link survey data with a general health assessment instrument like SF-12 and administrative diagnostic information. The latter approach has the advantage that it would allow adjustments for comorbidity, which can affect measures aiming to capture the severity of a single disease.
Fifth, apart from COPD, stroke, and epilepsy, where we have epidemiological data to estimate the geographical variation in the distribution of sequelae, for most diseases we are unable to capture differences in severity that occur due to treatment. As almost all our data sources on severity are from high-income countries, this would underestimate YLDs in low-income and middle-income countries with poorer access to and quality of treatment. If greater geographical information on severity of disease becomes available, we can incorporate a more explicit gradient based on our health-system access and quality index. [58]
Sixth, we have not yet been able to incorporate dependent comorbidity into our simulation methods. We aim for this to take place in GBD 2017 and will require substantial developmental work to make the computational code more efficient.
Seventh, most of the uncertainty in our YLD estimates comes from the disability weights. We have not conducted any new surveys since GBD 2013. With further data collection, we may be able to reduce some of the uncertainty by increasing the volume of data and by removing some of the ambiguities in lay descriptions, but large uncertainty is inherent to health state valuations that rely on perceptions by respondents of brief descriptions of complex health problems.
Eighth, the separate estimation of non-fatal models in DisMod-MR 2.1 for 1990, 1995, 2000, 2006, 2010, and 2016 implies uncertainty of estimates over time is independent. Also, compositional bias can lead to spurious time trends being estimated. DisMod-AT will allow for the more appealing simultaneous estimation over age and time and thus resolve the current limitations. However, as it is a more complex modelling tool, extensive testing and understanding what sensible settings are will need to take place before we can replace the current DisMod-MR approach.
Ninth, scrutiny of the multitude of results generated by GBD is a challenge. Increasingly, we generate visualisation tools to query results and intermediate steps in our analyses to better vet our results. We share our data and modelling tools with our expanding network of over 2,500 collaborators who frequently query data sources and our measurements for particular diseases or locations. Also, by publishing all code and describing the methods used disease-by-disease we encourage scrutiny of every aspect of the GBD study.
Tenth, as our GBD collaborators have raised, the argument of including Guinea worm disease to document pending eradication can be used to justify the inclusion of poliomyelitis in the next round of GBD. There are also a number of large residual categories, particularly other musculoskeletal disorders and other cardiovascular disease, where we could make more detailed estimates in future rounds of GBD.
Eleventh, despite adding estimates of the prevalence of several asymptomatic states of disease that are precursors of disease that can be targeted with preventive interventions (such as latent tuberculosis infection, chronic hepatitis, or stage III chronic kidney disease without anaemia), we are not comprehensive in doing so. As diagnostic capacity increases, more asymptomatic precursor states can be identified and, in GBD, we will aim to include these if they can be measured at the population level and become relevant to policy.
Future directions
We have introduced a quality grading system for cause of death sources for GBD 2016. We want to introduce a similar grading system of non-fatal data sources for GBD 2017. Important elements to capture in a grading system of non-fatal data sources will include the proportion of data sources using the reference method and case definition for a cause, the proportion of data sources representative of a location, and the amount of detail in reporting of age groups, sex, locations, and time periods covered. Unlike the location-specific grading of cause of death data sources, a grading system of non-fatal data sources will need to be location-specific and cause-specific, making it a much larger endeavour that will likely take several years to complete.
A prototype of a new version of a new analytical tool, DisMod-AT, is currently being tested. It has the advantage over DisMod-MR 2.1 in that it solves for the differential equations that govern the relationship between incidence, prevalence, remission, and mortality simultaneously over age and time. This is of great relevance for causes that vary substantially over time, and overcomes the assumption of a steady disease state that underlies previous versions of DisMod. We expect for GBD 2017 to run both the current tool and DisMod-AT in parallel for a number of time-sensitive causes with a view of DisMod-AT becoming the tool of choice from GBD 2018 onward.
We plan to reinstate a web survey facility that will allow derivation of disability weights for new health states; examination of the effect of changes in the wording of lay descriptions of health states on valuations provided by respondents; and creation of health states for combined impairments for which we currently estimate disability weights multiplicatively.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the Bill & Melinda Gates Foundation, the National Institute on Aging of the National Institutes of Health (award P30AG047845), and the National Institute of Mental Health of the National Institutes of Health (award R01MH110163). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Bill & Melinda Gates Foundation or the National Institutes of Health. The Palestinian Central Bureau of Statistics granted the researchers access to relevant data in accordance with license no. SLN2014-3-170, after subjecting data to processing aiming to preserve the confidentiality of individual data in accordance with the General Statistics Law - 2000. The researchers are solely responsible for the conclusions and inferences drawn upon available data. We thank the Russia Longitudinal Monitoring Survey, RLMS-HSE, conducted by the National Research University Higher School of Economics and ZAO “Demoscope” together with Carolina Population Center, University of North Carolina at Chapel Hill and the Institute of Sociology RAS for making these data available. This study has been realized using the data collected by the Swiss Household Panel (SHP), which is based at the Swiss Centre of Expertise in the Social Sciences FORS. The project is financed by the Swiss National Science Foundation. From the Framingham Heart Study of the National Heart Lung and Blood Institute of the National Institutes of Health and Boston University School of Medicine. This work was supported by the National Heart, Lung and Blood Institute's Framingham Heart Study (Contract No.N01-HC-25195). The HRS (Health and Retirement Study) is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan. This research used data from the National Health Survey 2003 and the National Health Survey 2009-2010. The authors are grateful to the Ministry of Health, Survey copyright owner, allowing them to have the database. All results of the study are those of the author and in no way committed to the Ministry. This research uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by a grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Persons interested in obtaining data files from Add Health should contact Add Health, Carolina Population Center, 123 W. Franklin Street, Chapel Hill, NC 27516-2524 (addhealth@unc.edu). No direct support was received from grant P01-HD31921 for this analysis. The data reported here have been supplied by the United States Renal Data System (USRDS). The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the U.S. government. HBSC is an international study carried out in collaboration with WHO/EURO. The International Coordinator of the 1997/98, 2001/02, 2005/06 and 2009/10 surveys was Prof. Candace Currie and the Data Bank Manager for the 1997/98 survey was Prof. Bente Wold, whereas for the following survey Prof. Oddrun Samdal was the Databank Manager. A list of principal investigator in each country can be found at http://www.hbsc.org. Data used in the preparation of this article were obtained from the Pooled Resource Open-Access ALS Clinical Trials (PRO-ACT) Database. In 2011, Prize4Life, in collaboration with the Northeast ALS Consortium, and with funding from the ALS Therapy Alliance, formed the Pooled Resource Open-Access ALS Clinical Trials (PRO-ACT) Consortium. The data available in the PRO-ACT Database has been volunteered by PRO-ACT Consortium members. This paper uses data from SHARE Waves 1, 2, 3 (SHARELIFE), 4, 5 and 6 (DOIs: 10.6103/SHARE.w1.600, 10.6103/SHARE.w2.600, 10.6103/SHARE.w3.600, 10.6103/SHARE.w4.600, 10.6103/SHARE.w5.600, 10.6103/SHARE.w6.600), see Börsch-Supan et al. (2013) for methodological details. (1) The SHARE data collection has been primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812) and FP7 (SHARE-PREP: N°211909, SHARE-LEAP: N°227822, SHARE M4: N°261982). Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C) and from various national funding sources is gratefully acknowledged (see www.share-project.org). This manuscript is based on data collected and shared by the International Vaccine Institute (IVI). This manuscript was not prepared in collaboration with investigators of IVI and does not necessarily reflect the opinions or views of IVI. The data used in this paper come from the 2009-10 Ghana Socioeconomic Panel Study Survey which is a nationally representative survey of over 5,000 households in Ghana. The survey is a joint effort undertaken by the Institute of Statistical, Social and Economic Research (ISSER) at the University of Ghana, and the Economic Growth Centre (EGC) at Yale University. It was funded by the Economic Growth Center. At the same time, ISSER and the EGC are not responsible for the estimations reported by the analyst(s).
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators
Theo Vos, Amanuel Alemu Abajobir, Cristiana Abbafati, Kaja M Abbas, Kalkidan Hassen Abate, Foad Abd-Allah, Abdishakur M Abdulle, Teshome Abuka Abebo, Semaw Ferede Abera, Victor Aboyans, Laith J Abu-Raddad, Ilana N Ackerman, Abdu Abdullahi Adamu, Olatunji Adetokunboh, Mohsen Afarideh, Ashkan Afshin, Sanjay Kumar Agarwal, Rakesh Aggarwal, Anurag Agrawal, Sutapa Agrawal, Aliasghar Ahmad Kiadaliri, Hamid Ahmadieh, Muktar Beshir Ahmed, Amani Nidhal Aichour, Ibtihel Aichour, Miloud Taki Eddine Aichour, Sneha Aiyar, Rufus Olusola Akinyemi, Nadia Akseer, Faris Hasan Al Lami, Fares Alahdab, Ziyad Al-Aly, Khurshid Alam, Noore Alam, Tahiya Alam, Deena Alasfoor, Kefyalew Addis Alene, Raghib Ali, Reza Alizadeh-Navaei, Ala'a Alkerwi, François Alla, Peter Allebeck, Christine Allen, Fatma Al-Maskari, Rajaa Al-Raddadi, Ubai Alsharif, Shirina Alsowaidi, Khalid A Altirkawi, Azmeraw T Amare, Erfan Amini, Walid Ammar, Yaw Ampem Amoako, Hjalte H Andersen, Carl Abelardo T Antonio, Palwasha Anwari, Johan Ärnlöv, Al Artaman, Krishna Kumar Aryal, Hamid Asayesh, Solomon W Asgedom, Reza Assadi, Tesfay Mehari Atey, Niguse Tadele Atnafu, Sachin R Atre, Leticia Avila-Burgos, Euripide Frinel G Arthur Avokpaho, Ashish Awasthi, Beatriz Paulina Ayala Quintanilla, Huda Omer Ba Saleem, Umar Bacha, Alaa Badawi, Kalpana Balakrishnan, Amitava Banerjee, Marlena S Bannick, Aleksandra Barac, Ryan M Barber, Suzanne L Barker-Collo, Till Bärnighausen, Simon Barquera, Lars Barregard, Lope H Barrero, Sanjay Basu, Bob Battista, Katherine E Battle, Bernhard T Baune, Shahrzad Bazargan-Hejazi, Justin Beardsley, Neeraj Bedi, Ettore Beghi, Yannick Béjot, Bayu Begashaw Bekele, Michelle L Bell, Derrick A Bennett, Isabela M Bensenor, Jennifer Benson, Adugnaw Berhane, Derbew Fikadu Berhe, Eduardo Bernabé, Balem Demtsu Betsu, Mircea Beuran, Addisu Shunu Beyene, Neeraj Bhala, Anil Bhansali, Samir Bhatt, Zulfiqar A Bhutta, Sibhatu Biadgilign, Kelly Bienhoff, Boris Bikbov, Charles Birungi, Stan Biryukov, Donal Bisanzio, Habtamu Mellie Bizuayehu, Dube Jara Boneya, Soufiane Boufous, Rupert R A Bourne, Alexandra Brazinova, Traolach S Brugha, Rachelle Buchbinder, Lemma Negesa Bulto Bulto, Blair R Bumgarner, Zahid A Butt, Lucero Cahuana-Hurtado, Ewan Cameron, Mate Car, Hélène Carabin, Jonathan R Carapetis, Rosario Cárdenas, David O Carpenter, Juan Jesus Carrero, Austin Carter, Felix Carvalho, Daniel C Casey, Valeria Caso, Carlos A Castañeda-Orjuela, Chris D Castle, Ferrán Catalá-López, Hsing-Yi Chang, Jung-Chen Chang, Fiona J Charlson, Honglei Chen, Mirriam Chibalabala, Chioma Ezinne Chibueze, Vesper Hichilombwe Chisumpa, Abdulaal A Chitheer, Devasahayam Jesudas Christopher, Liliana G Ciobanu, Massimo Cirillo, Danny Colombara, Cyrus Cooper, Paolo Angelo Cortesi, Michael H Criqui, John A Crump, Abel Fekadu Dadi, Koustuv Dalal, Lalit Dandona, Rakhi Dandona, José das Neves, Dragos V Davitoiu, Barbora de Courten, Diego De Leo, Louisa Degenhardt, Selina Deiparine, Robert P Dellavalle, Kebede Deribe, Don C Des Jarlais, Subhojit Dey, Samath D Dharmaratne, Preet Kaur Dhillon, Daniel Dicker, Eric L Ding, Shirin Djalalinia, Huyen Phuc Do, E Ray Dorsey, Kadine Priscila Bender dos Santos, Dirk Douwes-Schultz, Kerrie E Doyle, Tim R Driscoll, Manisha Dubey, Bruce Bartholow Duncan, Ziad Ziad El-Khatib, Jerisha Ellerstrand, Ahmadali Enayati, Aman Yesuf Endries, Sergey Petrovich Ermakov, Holly E Erskine, Babak Eshrati, Sharareh Eskandarieh, Alireza Esteghamati, Kara Estep, Fanuel Belayneh Bekele Fanuel, Carla Sofia e Sa Farinha, André Faro, Farshad Farzadfar, Mir Sohail Fazeli, Valery L Feigin, Seyed-Mohammad Fereshtehnejad, João C Fernandes, Alize J Ferrari, Tesfaye Regassa Feyissa, Irina Filip, Florian Fischer, Christina Fitzmaurice, Abraham D Flaxman, Luisa Sorio Flor, Nataliya Foigt, Kyle J Foreman, Richard C Franklin, Nancy Fullman, Thomas Fürst, Joao M Furtado, Neal D Futran, Emmanuela Gakidou, Morsaleh Ganji, Alberto L Garcia-Basteiro, Teshome Gebre, Tsegaye Tewelde Gebrehiwot, Ayele Geleto, Bikila Lencha Gemechu, Hailay Abrha Gesesew, Peter W Gething, Alireza Ghajar, Katherine B Gibney, Paramjit Singh Gill, Richard F Gillum, Ibrahim Abdelmageem Mohamed Ginawi, Ababi Zergay Giref, Melkamu Dedefo Gishu, Giorgia Giussani, William W Godwin, Audra L Gold, Ellen M Goldberg, Philimon N Gona, Amador Goodridge, Sameer Vali Gopalani, Atsushi Goto, Alessandra Carvalho Goulart, Max Griswold, Harish Chander Gugnani, Rahul Gupta, Rajeev Gupta, Tanush Gupta, Vipin Gupta, Nima Hafezi-Nejad, Alemayehu Desalegne Hailu, Gessessew Bugssa Hailu, Randah Ribhi Hamadeh, Samer Hamidi, Alexis J Handal, Graeme J Hankey, Yuantao Hao, Hilda L Harb, Habtamu Abera Hareri, Josep Maria Haro, James Harvey, Mohammad Sadegh Hassanvand, Rasmus Havmoeller, Caitlin Hawley, Roderick J Hay, Simon I Hay, Nathaniel J Henry, Ileana Beatriz Heredia-Pi, Pouria Heydarpour, Hans W Hoek, Howard J Hoffman, Nobuyuki Horita, H Dean Hosgood, Sorin Hostiuc, Peter J Hotez, Damian G Hoy, Aung Soe Htet, Guoqing Hu, Hsiang Huang, Chantal Huynh, Kim Moesgaard Iburg, Ehimario Uche Igumbor, Chad Ikeda, Caleb Mackay Salpeter Irvine, Kathryn H Jacobsen, Nader Jahanmehr, Mihajlo B Jakovljevic, Simerjot K Jassal, Mehdi Javanbakht, Sudha P Jayaraman, Panniyammakal Jeemon, Paul N Jensen, Vivekanand Jha, Guohong Jiang, Denny John, Catherine O Johnson, Sarah Charlotte Johnson, Jost B Jonas, Mikk Jürisson, Zubair Kabir, Rajendra Kadel, Amaha Kahsay, Ritul Kamal, Haidong Kan, Nadim E Karam, André Karch, Corine Kakizi Karema, Amir Kasaeian, Getachew Mullu Kassa, Nigussie Assefa Kassaw, Nicholas J Kassebaum, Anshul Kastor, Srinivasa Vittal Katikireddi, Anil Kaul, Norito Kawakami, Peter Njenga Keiyoro, Andre Pascal Kengne, Andre Keren, Yousef Saleh Khader, Ibrahim A Khalil, Ejaz Ahmad Khan, Young-Ho Khang, Ardeshir Khosravi, Jagdish Khubchandani, Christian Kieling, Daniel Kim, Pauline Kim, Yun Jin Kim, Ruth W Kimokoti, Yohannes Kinfu, Adnan Kisa, Katarzyna A Kissimova-Skarbek, Mika Kivimaki, Ann Kristin Knudsen, Yoshihiro Kokubo, Dhaval Kolte, Jacek A Kopec, Soewarta Kosen, Parvaiz A Koul, Ai Koyanagi, Michael Kravchenko, Sanjay Krishnaswami, Kristopher J Krohn, Barthelemy Kuate Defo, Burcu Kucuk Bicer, G Anil Kumar, Pushpendra Kumar, Sanjiv Kumar, Hmwe H Kyu, Dharmesh Kumar Lal, Ratilal Lalloo, Nkurunziza Lambert, Qing Lan, Anders Larsson, Pablo M Lavados, Janet L Leasher, Jong-Tae Lee, Paul H Lee, James Leigh, Cheru Tesema Leshargie, Janni Leung, Ricky Leung, Miriam Levi, Yichong Li, Yongmei Li, Darya Li Kappe, Xiaofeng Liang, Misgan Legesse Liben, Stephen S Lim, Shai Linn, Angela Liu, Patrick Y Liu, Shiwei Liu, Yang Liu, Rakesh Lodha, Giancarlo Logroscino, Stephanie J London, Katharine J Looker, Alan D Lopez, Stefan Lorkowski, Paulo A Lotufo, Nicola Low, Rafael Lozano, Timothy C D Lucas, Erlyn Rachelle King Macarayan, Hassan Magdy Abd El Razek, Mohammed Magdy Abd El Razek, Mahdi Mahdavi, Marek Majdan, Reza Majdzadeh, Azeem Majeed, Reza Malekzadeh, Rajesh Malhotra, Deborah Carvalho Malta, Abdullah A Mamun, Helena Manguerra, Treh Manhertz, Ana Mantilla, Lorenzo G Mantovani, Chabila C Mapoma, Laurie B Marczak, Jose Martinez-Raga, Francisco Rogerlândio Martins-Melo, Ira Martopullo, Winfried März, Manu Raj Mathur, Mohsen Mazidi, Colm McAlinden, Madeline McGaughey, John J McGrath, Martin McKee, Claire McNellan, Suresh Mehata, Man Mohan Mehndiratta, Tefera Chane Mekonnen, Peter Memiah, Ziad A Memish, Walter Mendoza, Mubarek Abera Mengistie, Desalegn Tadese Mengistu, George A Mensah, Atte Meretoja, Tuomo J Meretoja, Haftay Berhane Mezgebe, Renata Micha, Anoushka Millear, Ted R Miller, Edward J Mills, Mojde Mirarefin, Erkin M Mirrakhimov, Awoke Misganaw, Shiva Raj Mishra, Philip B Mitchell, Karzan Abdulmuhsin Mohammad, Alireza Mohammadi, Kedir Endris Mohammed, Shafiu Mohammed, Sanjay K Mohanty, Ali H Mokdad, Sarah K Mollenkopf, Lorenzo Monasta, Julio Montañez Hernandez, Marcella Montico, Maziar Moradi-Lakeh, Paula Moraga, Rintaro Mori, Chloe Morozoff, Shane D Morrison, Mark Moses, Cliff Mountjoy-Venning, Kalayu Birhane Mruts, Ulrich O Mueller, Kate Muller, Michele E Murdoch, Gudlavalleti Venkata Satyanarayana Murthy, Kamarul Imran Musa, Jean B Nachega, Gabriele Nagel, Mohsen Naghavi, Aliya Naheed, Kovin S Naidoo, Luigi Naldi, Vinay Nangia, Gopalakrishnan Natarajan, Dumessa Edessa Negasa, Ionut Negoi, Ruxandra Irina Negoi, Charles R Newton, Josephine Wanjiku Ngunjiri, Cuong Tat Nguyen, Grant Nguyen, Minh Nguyen, Quyen Le Nguyen, Trang Huyen Nguyen, Emma Nichols, Dina Nur Anggraini Ningrum, Sandra Nolte, Vuong Minh Nong, Bo Norrving, Jean Jacques N Noubiap, Martin J O'Donnell, Felix Akpojene Ogbo, In-Hwan Oh, Anselm Okoro, Olanrewaju Oladimeji, Andrew Toyin Olagunju, Tinuke Oluwasefunmi Olagunju, Helen E Olsen, Bolajoko Olubukunola Olusanya, Jacob Olusegun Olusanya, Kanyin Ong, John Nelson Opio, Eyal Oren, Alberto Ortiz, Aaron Osgood-Zimmerman, Majdi Osman, Mayowa O Owolabi, Mahesh PA, Rosana E Pacella, Adrian Pana, Basant Kumar Panda, Christina Papachristou, Eun-Kee Park, Charles D Parry, Mahboubeh Parsaeian, Scott B Patten, George C Patton, Katherine Paulson, Neil Pearce, David M Pereira, Norberto Perico, Konrad Pesudovs, Carrie Beth Peterson, Max Petzold, Michael Robert Phillips, David M Pigott, Julian David Pillay, Christine Pinho, Dietrich Plass, Martin A Pletcher, Svetlana Popova, Richie G Poulton, Farshad Pourmalek, Dorairaj Prabhakaran, Narayan Prasad, Noela M Prasad, Carrie Purcell, Mostafa Qorbani, Reginald Quansah, Rynaz H S Rabiee, Amir Radfar, Anwar Rafay, Kazem Rahimi, Afarin Rahimi-Movaghar, Vafa Rahimi-Movaghar, Mahfuzar Rahman, Mohammad Hifz Ur Rahman, Rajesh Kumar Rai, Sasa Rajsic, Usha Ram, Chhabi Lal Ranabhat, Zane Rankin, Paturi Vishnupriya Rao, Puja C Rao, Salman Rawaf, Sarah E Ray, Robert C Reiner, Nikolas Reinig, Marissa B Reitsma, Giuseppe Remuzzi, Andre M N Renzaho, Serge Resnikoff, Satar Rezaei, Antonio L Ribeiro, Luca Ronfani, Gholamreza Roshandel, Gregory A Roth, Ambuj Roy, Enrico Rubagotti, George Mugambage Ruhago, Soheil Saadat, Nafis Sadat, Mahdi Safdarian, Sare Safi, Saeid Safiri, Rajesh Sagar, Ramesh Sahathevan, Joseph Salama, Joshua A Salomon, Sundeep Santosh Salvi, Abdallah M Samy, Juan R Sanabria, Damian Santomauro, Itamar S Santos, João Vasco Santos, Milena M Santric Milicevic, Benn Sartorius, Maheswar Satpathy, Monika Sawhney, Sonia Saxena, Maria Inês Schmidt, Ione J C Schneider, Ben Schöttker, David C Schwebel, Falk Schwendicke, Soraya Seedat, Sadaf G Sepanlou, Edson E Servan-Mori, Tesfaye Setegn, Katya Anne Shackelford, Amira Shaheen, Masood Ali Shaikh, Mansour Shamsipour, Sheikh Mohammed Shariful Islam, Jayendra Sharma, Rajesh Sharma, Jun She, Peilin Shi, Chloe Shields, Mika Shigematsu, Yukito Shinohara, Rahman Shiri, Reza Shirkoohi, Shreya Shirude, Kawkab Shishani, Mark G Shrime, Abla Mehio Sibai, Inga Dora Sigfusdottir, Diego Augusto Santos Silva, João Pedro Silva, Dayane Gabriele Alves Silveira, Jasvinder A Singh, Narinder Pal Singh, Dhirendra Narain Sinha, Eirini Skiadaresi, Vegard Skirbekk, Erica Leigh Slepak, Amber Sligar, David L Smith, Mari Smith, Badr H A Sobaih, Eugene Sobngwi, Reed J D Sorensen, Tatiane Cristina Moraes Sousa, Luciano A Sposato, Chandrashekhar T Sreeramareddy, Vinay Srinivasan, Jeffrey D Stanaway, Vasiliki Stathopoulou, Nicholas Steel, Dan J Stein, Murray B Stein, Caitlyn Steiner, Timothy J Steiner, Sabine Steinke, Mark Andrew Stokes, Lars Jacob Stovner, Bryan Strub, Michelle Subart, Muawiyyah Babale Sufiyan, Rizwan Suliankatchi Abdulkader, Bruno F Sunguya, Patrick J Sur, Soumya Swaminathan, Bryan L Sykes, Dillon O Sylte, Rafael Tabarés-Seisdedos, Getachew Redae Taffere, Jukka S Takala, Nikhil Tandon, Mohammad Tavakkoli, Nuno Taveira, Hugh R Taylor, Arash Tehrani-Banihashemi, Tesfalidet Tekelab, Girma Temam Shifa, Abdullah Sulieman Terkawi, Dawit Jember Tesfaye, Belay Tesssema, Ornwipa Thamsuwan, Katie E Thomas, Amanda G Thrift, Tenaw Yimer Tiruye, Ruoyan Tobe-Gai, Mette C Tollanes, Marcello Tonelli, Roman Topor-Madry, Miguel Tortajada, Mathilde Touvier, Bach Xuan Tran, Suryakant Tripathi, Christopher Troeger, Thomas Truelsen, Derrick Tsoi, Kald Beshir Tuem, Emin Murat Tuzcu, Stefanos Tyrovolas, Kingsley N Ukwaja, Eduardo A Undurraga, Chigozie Jesse Uneke, Rachel Updike, Olalekan A Uthman, Benjamin S Chudi Uzochukwu, Job F M van Boven, Santosh Varughese, Tommi Vasankari, S Venkatesh, Narayanaswamy Venketasubramanian, Ramesh Vidavalur, Francesco S Violante, Sergey K Vladimirov, Vasiliy Victorovich Vlassov, Stein Emil Vollset, Fiseha Wadilo, Tolassa Wakayo, Yuan-Pang Wang, Marcia Weaver, Scott Weichenthal, Elisabete Weiderpass, Robert G Weintraub, Andrea Werdecker, Ronny Westerman, Harvey A Whiteford, Tissa Wijeratne, Charles Shey Wiysonge, Charles D A Wolfe, Rachel Woodbrook, Anthony D Woolf, Abdulhalik Workicho, Sarah Wulf Hanson, Denis Xavier, Gelin Xu, Simon Yadgir, Mohsen Yaghoubi, Bereket Yakob, Lijing L Yan, Yuichiro Yano, Pengpeng Ye, Hassen Hamid Yimam, Paul Yip, Naohiro Yonemoto, Seok-Jun Yoon, Marcel Yotebieng, Mustafa Z Younis, Zoubida Zaidi, Maysaa El Sayed Zaki, Elias Asfaw Zegeye, Zerihun Menlkalew Zenebe, Xueying Zhang, Maigeng Zhou, Ben Zipkin, Sanjay Zodpey, Liesl Joanna Zuhlke, Christopher J L Murray
Affiliations
Institute for Health Metrics and Evaluation (Prof T Vos PhD, A Afshin MD, S Aiyar, T Alam MPH, C Allen BA, M S Bannick BS, R M Barber BS, J Benson BA, K Bienhoff MA, S Biryukov BS, B R Bumgarner MBA, A Carter BS, D C Casey MPH, C D Castle BA, F J Charlson PhD, D Colombara PhD, Prof L Dandona MD, Prof R Dandona PhD, Prof L Degenhardt PhD, S Deiparine, D Dicker BS, D Douwes-Schultz BS, H E Erskine PhD, K Estep MPA, A J Ferrari PhD, C Fitzmaurice MD, A D Flaxman PhD, K J Foreman PhD, N Fullman MPH, Prof E Gakidou PhD, W W Godwin BS, A L Gold MSc, E M Goldberg BS, M Griswold MA, J Harvey BS, C Hawley MS, Prof S I Hay DSc, N J Henry BS/BA, C Huynh BA, C Ikeda BS, C M S Irvine BA, C O Johnson PhD, S C Johnson MSc, N J Kassebaum MD, I A Khalil MD, P Kim BA, K J Krohn BA, H H Kyu PhD, D Li Kappe MBA, Prof S S Lim PhD, A Liu BS, P Y Liu MPH, R Lozano MD, H Manguerra BS, T Manhertz BA, L B Marczak PhD, I Martopullo MPH, M McGaughey BA, C McNellan BA, A Millear BA, M Mirarefin MPH, A Misganaw PhD, Prof A H Mokdad PhD, S Mollenkopf MPH, C Morozoff MPH, M Moses MHS, C Mountjoy-Venning BA, K Muller MPH, M Naghavi PhD, G Nguyen MPH, M Nguyen BS, E Nichols BA, H E Olsen MA, K Ong PhD, A Osgood-Zimmerman MS, K Paulson BS, D M Pigott DPhil, C Pinho BA, M A Pletcher BS, C Purcell BS, Z Rankin MPH, P C Rao MPH, S E Ray BS, R C Reiner PhD, N Reinig BS, M B Reitsma BS, G A Roth MD, N Sadat MA, J Salama MSc, D Santomauro PhD, K A Shackelford BA, C Shields BS, S Shirude MPH, E L Slepak MLIS, A Sligar MPH, Prof D L Smith PhD, M Smith MPA, R J D Sorensen MPH, V Srinivasan BA, J D Stanaway PhD, C Steiner MPH, B Strub BS, M Subart BA, P J Sur BA, D O Sylte BA, O Thamsuwan PhD, K E Thomas PhD, C Troeger MPH, D Tsoi BS, R Updike AB, Prof S E Vollset DrPH, M Weaver PhD, Prof H A Whiteford PhD, R Woodbrook MLIS, S Wulf Hanson MPH, S Yadgir BS, Prof M Zhou PhD, B Zipkin BS, Prof C J L Murray DPhil), Division of Hematology, Department of Medicine (C Fitzmaurice MD), Center for Health Trends and Forecasts, Institute for Health Metrics and Evaluation (Prof M B Jakovljevic PhD), University of Washington, Seattle, WA, USA (N D Futran MD, P N Jensen PhD, J Leung PhD, S D Morrison MD); School of Public Health (A A Abajobir MPH, F J Charlson PhD, J Ellerstrand MD, H E Erskine PhD, A J Ferrari PhD, J Leung PhD, A Mantilla MHEcon, D Santomauro PhD, Prof H A Whiteford PhD), School of Dentistry (Prof R Lalloo PhD), Queensland Brain Institute (Prof J J McGrath PhD), University of Queensland, Brisbane, QLD, Australia (S R Mishra MPH); La Sapienza University, Rome, Italy (C Abbafati PhD); Virginia Tech, Blacksburg, VA, USA (Prof K M Abbas PhD); Department of Neurology, Cairo University, Cairo, Egypt (Prof F Abd-Allah MD); New York University Abu Dhabi, Abu Dhabi, United Arab Emirates (A M Abdulle PhD); Hawassa University College of Medicine and Health Sciences, Hawassa, Ethiopia (T A Abebo MPH, D J Tesfaye MPH); School of Public Health, College of Health Sciences (S F Abera MSc), School of Pharmacy (D F Berhe MS), College of Health Sciences (D T Mengistu MS, K E Mohammed MPH), School of Public Health (G R Taffere PhD), Mekelle University, Mekelle, Ethiopia (S W Asgedom MS, T M Atey MS, B D Betsu MS, G B Hailu MSc, A Kahsay MPH, H B Mezgebe MS, K B Tuem MS, Z M Zenebe MS); Food Security and Institute for Biological Chemistry and Nutrition, University of Hohenheim, Stuttgart, Germany (S F Abera MSc); Dupuytren University Hospital, Limoges, France (Prof V Aboyans PhD); Infectious Disease Epidemiology Group, Weill Cornell Medical College in Qatar, Doha, Qatar (L J Abu-Raddad PhD); Department of Epidemiology and Preventive Medicine, School of Public Health and Preventive Medicine (I N Ackerman PhD, Prof R Buchbinder PhD), Department of Medicine, School of Clinical Sciences at Monash Health (Prof A G Thrift PhD), Monash University, Melbourne, VIC, Australia (Prof B de Courten PhD); Center for Infectious Diseases Research, Kano, Nigeria (A A Adamu MS); Department of Psychiatry (Prof C D Parry PhD), Stellenbosch University, Cape Town, South Africa (O Adetokunboh MD, Prof J B Nachega PhD, Prof S Seedat PhD, Prof C S Wiysonge PhD); All India Institute of Medical Sciences, New Delhi, India (Prof S K Agarwal MD, R Lodha MD, Prof R Malhotra MS, A Roy DM, R Sagar MD, Prof N Tandon PhD); Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India (Prof R Aggarwal MD); CSIR - Institute of Genomics and Integrative Biology, Delhi, India (A Agrawal PhD); Department of Internal Medicine, Baylor College of Medicine, Houston, TX, USA (A Agrawal PhD); Indian Institute of Public Health (S Dey PhD, Prof G V S Murthy MD), Centre for Control of Chronic Conditions (P Jeemon PhD), Public Health Foundation of India, Gurugram, India (S Agrawal PhD, Prof L Dandona MD, Prof R Dandona PhD, P K Dhillon PhD, G A Kumar PhD, D K Lal MD, M R Mathur PhD, Prof S Zodpey PhD); Department of Clinical Sciences Lund, Orthopedics, Clinical Epidemiology Unit (A Ahmad Kiadaliri PhD), Skane University Hospital, Department of Clinical Sciences Lund, Neurology (Prof B Norrving PhD), Lund University, Lund, Sweden; Ophthalmic Research Center (H Ahmadieh MD), School of Public Health (N Jahanmehr PhD), Ophthalmic Epidemiology Research Center (S Safi MS), Shahid Beheshti University of Medical Sciences, Tehran, Iran; Department of Ophthalmology, Labbafinejad Medical Center, Tehran, Iran (H Ahmadieh MD); Department of Epidemiology, College of Health Sciences (M B Ahmed MPH), Jimma University, Jimma, Ethiopia (T T Gebrehiwot MPH, H A Gesesew MPH, M A Mengistie MS, T Wakayo MS, A Workicho MPH); University Ferhat Abbas of Setif, Setif, Algeria (A N Aichour BS); National Institute of Nursing Education, Setif, Algeria (I Aichour MS); High National School of Veterinary Medicine, Algiers, Algeria (M T Aichour MD); University of Ibadan, Ibadan, Nigeria (R O Akinyemi PhD); Newcastle University, Newcastle upon Tyne, UK (R O Akinyemi PhD); Centre for Global Child Health, The Hospital for Sick Children, Toronto, ON, Canada (N Akseer MSc, Z A Bhutta PhD); Dalla Lana School of Public Health (N Akseer MSc), Department of Nutritional Sciences, Faculty of Medicine (A Badawi PhD), Centre for Addiction and Mental Health (S Popova PhD), University of Toronto, Toronto, ON, Canada; Baghdad College of Medicine, Baghdad, Iraq (F H Al Lami PhD); Mayo Clinic Foundation for Medical Education and Research, Rochester, MN, USA (F Alahdab MD); Syrian American Medical Society, Washington, DC, USA (F Alahdab MD); Washington University in St Louis, St Louis, MO, USA (Z Al-Aly MD); Murdoch Childrens Research Institute (K Alam PhD), Melbourne School of Population and Global Health (Prof A D Lopez PhD), Department of Medicine (A Meretoja PhD), Murdoch Childrens Research Institute, Department of Paediatrics (Prof G C Patton MD), The University of Melbourne, Melbourne, VIC, Australia (K Alam PhD, Prof H R Taylor AC, R G Weintraub MBBS, Prof T Wijeratne MD); Sydney School of Public Health (Prof T R Driscoll PhD), The University of Sydney, Sydney, NSW, Australia (K Alam PhD, J Leigh PhD); Department of Health, Queensland, Brisbane, QLD, Australia (N Alam MAppEpid); Ministry of Health, Al Khuwair, Oman (D Alasfoor MSc); Department of Epidemiology and Biostatistics, Institute of Public Health (K A Alene MPH), College of Medical and Health Sciences (B B Bekele PhD), University of Gondar, Gondar, Ethiopia (Prof A F Dadi MPH, B Tesssema PhD); Department of Global Health, Research School of Population Health (K A Alene MPH), Australian National University, Canberra, ACT, Australia (Prof K E Doyle PhD); Malaria Atlas Project (K E Battle DPhil), Oxford Big Data Institute, Li Ka Shing Centre for Health Information and Discovery (E Cameron PhD, Prof S I Hay DSc, T C D Lucas PhD), Nuffield Department of Population Health (D A Bennett PhD), Nuffield Department of Medicine (D Bisanzio PhD), NIHR Musculoskeletal Biomedical Research Centre (Prof C Cooper FMedSci), Department of Zoology (P W Gething PhD), University of Oxford, Oxford, UK (R Ali MSc, Prof V Jha DM, K Rahimi DM); Gastrointestinal Cancer Research Center, Mazandaran University of Medical Sciences, Sari, Iran (R Alizadeh-Navaei PhD); Luxembourg Institute of Health, Strassen, Luxembourg (A Alkerwi PhD); School of Public Health, University of Lorraine, Nancy, France (Prof F Alla PhD); College of Medicine and Health Sciences, United Arab Emirates University, Al Ain, United Arab Emirates (Prof F Al-Maskari PhD, S Alsowaidi MD); Joint Program of Family and Community Medicine, Jeddah, Saudi Arabia (R Al-Raddadi PhD); Department of Psychosomatic Medicine, Center for Internal Medicine and Dermatology (S Nolte PhD), Charité Universitätsmedizin, Berlin, Germany (U Alsharif MPH); King Saud University, Riyadh, Saudi Arabia (K A Altirkawi MD, B H A Sobaih MD); School of Medicine (A T Amare MPH, Prof B T Baune PhD, L G Ciobanu MS), Discipline of Psychiatry (A T Olagunju MS), University of Adelaide, Adelaide, SA, Australia; College of Medicine and Health Sciences (A T Amare MPH), Bahir Dar University, Bahir Dar, Ethiopia (T Setegn MPH); Uro-Oncology Research Center (E Amini MD), Non-Communicable Diseases Research Center (E Amini MD, F Farzadfar MD, A Khosravi PhD, M Parsaeian PhD), Endocrinology and Metabolism Research Center (M Afarideh MD, A Kasaeian PhD, Prof A Esteghamati MD, N Hafezi-Nejad MD), Department of Internal Medicine (A Ghajar MD), Center for Air Pollution Research, Institute for Environmental Research (M S Hassanvand PhD), Multiple Sclerosis Research Center, Neuroscience Institute (P Heydarpour MD), Hematology-Oncology and Stem Cell Transplantation Research Center (A Kasaeian PhD), Institute of Health Policy and Management (M Mahdavi PhD), Knowledge Utilization Research Center (Prof R Majdzadeh PhD), Digestive Diseases Research Institute (Prof R Malekzadeh MD, G Roshandel PhD, S G Sepanlou PhD), Department of Epidemiology and Biostatistics, School of Public Health (M Parsaeian PhD), Iranian National Center for Addiction Studies (INCAS) (A Rahimi-Movaghar MD), Sina Trauma and Surgery Research Center (Prof V Rahimi-Movaghar MD, S Saadat PhD, M Safdarian MD), Institute for Environmental Research (M Shamsipour PhD), Cancer Research Center (Prof R Shirkoohi PhD), Tehran University of Medical Sciences, Tehran, Iran (M Ganji MD); Ministry of Public Health, Beirut, Lebanon (W Ammar PhD, H L Harb MPH); Department of Medicine, Komfo Anokye Teaching Hospital, Kumasi, Ghana (Y A Amoako MD); Center for Sensory-Motor Interaction, Department of Health Science and Technology, Faculty of Medicine (H H Andersen MSc), Aalborg University, Aalborg Esst, Denmark (C B Peterson PhD); Department of Health Policy and Administration, College of Public Health, University of the Philippines Manila, Manila, Philippines (C A T Antonio MD); Self-employed, Kabul, Afghanistan (P Anwari MS); Department of Neurobiology, Care Sciences and Society Division of Family Medicine and Primary Care (Prof J Ärnlöv PhD, S Fereshtehnejad PhD), Department of Medical Epidemiology and Biostatistics (Prof J J Carrero PhD, E Weiderpass PhD), Department of Public Health Sciences (Prof P Allebeck PhD, Z Z El-Khatib PhD, R H S Rabiee MPH), Karolinska Institutet, Stockholm, Sweden (R Havmoeller PhD); School of Health and Social Studies, Dalarna University, Falun, Sweden (Prof J Ärnlöv PhD); University of Manitoba, Winnipeg, MB, Canada (A Artaman PhD); Nepal Health Research Council, Kathmandu, Nepal (K K Aryal MPH); University of Oslo, Oslo, Norway (K K Aryal MPH, A S Htet MPhil); Department of Medical Emergency, School of Paramedic, Qom University of Medical Sciences, Qom, Iran (H Asayesh MS); Mashhad University of Medical Sciences, Mashhad, Iran (R Assadi PhD); Mizan Tepi University, Mizan Teferi, Ethiopia (N T Atnafu MS, H H Yimam MPH); Centre for Clinical Global Health Education (CCGHE) (S R Atre PhD), Johns Hopkins University, Baltimore, MD, USA (B X Tran PhD); Dr D Y Patil Vidyapeeth Pune, Pune, India (S R Atre PhD); National Institute of Public Health, Cuernavaca, Mexico (L Avila-Burgos PhD, S Barquera PhD, L Cahuana-Hurtado PhD, I B Heredia-Pi PhD, R Lozano MD, J Montañez Hernandez MSc, Prof E E Servan-Mori MSc); Institut de Recherche Clinique du Bénin (IRCB), Cotonou, Benin (E F G A Avokpaho MPH); Laboratoire d'Etudes et de Recherche-Action en Santé (LERAS Afrique), Parakou, Benin (E F G A Avokpaho MPH); Indian Institute of Public Health, Gandhinagar, India (A Awasthi PhD); The Judith Lumley Centre for Mother, Infant and Family Health Research, La Trobe University, Melbourne, VIC, Australia (B P Ayala Quintanilla PhD); Peruvian National Institute of Health, Lima, Peru (B P Ayala Quintanilla PhD); Faculty of Medicine and Health Sciences, Aden University, Aden, Yemen (Prof H O Ba Saleem PhD); School of Health Sciences, University of Management and Technology, Lahore, Pakistan (U Bacha PhD); Public Health Agency of Canada, Toronto, ON, Canada (A Badawi PhD); Department of Environmental Health Engineering, Sri Ramachandra University, Chennai, India (K Balakrishnan PhD); Farr Institute of Health Informatics Research (A Banerjee DPhil), Department of Epidemiology and Public Health (Prof M Kivimaki PhD), University College London, London, UK (C Birungi MS, M R Mathur PhD); Faculty of Medicine (A Barac PhD), Institute of Social Medicine and Centre School of Public Health and Health Management, Faculty of Medicine (M M Santric Milicevic PhD), University of Belgrade, Belgrade, Serbia; School of Psychology, University of Auckland, Auckland, New Zealand (S L Barker-Collo PhD); Department of Global Health and Population, Harvard T H Chan School of Public Health (Prof T Bärnighausen MD, E L Ding ScD, J A Salomon PhD), Ariadne Labs (E R K Macarayan PhD), Harvard University, Boston, MA, USA; Africa Health Research Institute, Mtubatuba, South Africa (Prof T Bärnighausen MD); Institute of Public Health, Heidelberg University, Heidelberg, Germany (Prof T Bärnighausen MD, S Mohammed PhD); Department of Occupational and Environmental Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden (Prof L Barregard MD); Department of Industrial Engineering, School of Engineering, Pontificia Universidad Javeriana, Bogota, Colombia (L H Barrero ScD); Stanford University, Stanford, CA, USA (S Basu PhD); Doctor Evidence, Santa Monica, CA, USA (B Battista MA, M S Fazeli MD); College of Medicine, Charles R Drew University of Medicine and Science, Los Angeles, CA, USA (Prof S Bazargan-Hejazi PhD); David Geffen School of Medicine, University of California at Los Angeles, Los Angeles, CA, USA (Prof S Bazargan-Hejazi PhD); Oxford University, Ho Chi Minh City, Vietnam (J Beardsley MBCHB); College of Public Health and Tropical Medicine, Jazan, Saudi Arabia (N Bedi MD); IRCCS - Istituto di Ricerche Farmacologiche Mario Negri, Milan, Italy (E Beghi MD, G Giussani BiolD); University Hospital and Medical School of Dijon, University of Burgundy, Dijon, France (Prof Y Béjot PhD); Mizan Tepi University, Mizan Aman, Ethiopia (B B Bekele PhD); Yale University, New Haven, CT, USA (Prof M L Bell PhD); Center for Clinical and Epidemiological Research Center, Hospital Universitario (A C Goulart PhD), Internal Medicine Department (Prof I S Santos PhD), University of São Paulo, São Paulo, Brazil (I M Bensenor PhD, Prof P A Lotufo DrPh); College of Health Sciences (A Berhane PhD), Public Health Department, College of Health (K B Mruts MPH), Debre Berhan University, Debre Berhan, Ethiopia; University Medical Center Groningen (D F Berhe MS), Department of Psychiatry, University Medical Center Groningen (Prof H W Hoek MD), University of Groningen, Groningen, Netherlands (J F M van Boven PhD); Division of Health and Social Care Research (Prof C D Wolfe MD), King's College London, London, UK (E Bernabé PhD, Prof R J Hay DM); Carol Davila University of Medicine and Pharmacy, Bucharest, Romania (Prof M Beuran PhD, D V Davitoiu PhD, S Hostiuc PhD, I Negoi PhD, R I Negoi PhD); Emergency Hospital of Bucharest, Bucharest, Romania (Prof M Beuran PhD, I Negoi PhD); College of Health and Medical Sciences (A S Beyene MPH), Haramaya University, Harar, Ethiopia (L N B Bulto MS, A Geleto MPH, M D Gishu MS, D E Negasa MS); Queen Elizabeth Hospital Birmingham, Birmingham, UK (N Bhala DPhil); University of Otago Medical School, Wellington, New Zealand (N Bhala DPhil); Postgraduate Institute of Medical Education and Research, Chandigarh, India (A Bhansali DM); Department of Infectious Disease Epidemiology (S Bhatt DPhil, T Fürst PhD), Department of Primary Care & Public Health (Prof A Majeed MD), Division of Brain Sciences (Prof T J Steiner PhD), Imperial College London, London, UK (M Car PhD, Prof S Rawaf MD, S Saxena MD); Centre of Excellence in Women and Child Health, Aga Khan University, Karachi, Pakistan (Z A Bhutta PhD); Independent Public Health Consultants, Addis Ababa, Ethiopia (S Biadgilign MPH); IRCCS - Istituto di Ricerche Farmacologiche Mario Negri, Bergamo, Italy (B Bikbov MD, N Perico MD, Prof G Remuzzi MD); Department of Public Health (D J Boneya MPH), Debre Markos University, Debre Markos, Ethiopia (H M Bizuayehu MPH, G M Kassa MS, C T Leshargie MPH, T Y Tiruye MPH); Transport and Road Safety (TARS) Research (S Boufous PhD), National Drug and Alcohol Research Centre (Prof L Degenhardt PhD), Brien Holden Vision Institute and School of Optometry and Vision Science (Prof S Resnikoff MD), University of New South Wales, Kensington, NSW, Australia (Prof P B Mitchell MD); Vision & Eye Research Unit, Anglia Ruskin University, Cambridge, UK (Prof R R A Bourne MD); Faculty of Health Sciences and Social Work, Department of Public Health, Faculty of Medicine, Comenius University, Bratislava, Slovakia (A Brazinova MD); University of Leicester, Leicester, UK (Prof T S Brugha MD); Monash Department of Clinical Epidemiology, Cabrini Institute, Melbourne, VIC, Australia (Prof R Buchbinder PhD); Al Shifa Trust Eye Hospital, Rawalpindi, Pakistan (Z A Butt PhD); Ministry of Health of the Republic of Croatia, Zagreb, Croatia (M Car PhD); Department of Biostatistics and Epidemiology, University of Oklahoma Health Sciences Center, Oklahoma City, OK, USA (H Carabin PhD); Telethon Kids Institute, Princess Margaret Hospital for Children, The University of Western Australia, Subiaco, WA, Australia (Prof J R Carapetis PhD); Metropolitan Autonomous University, Mexico City, Mexico (R Cárdenas ScD); University at Albany, Rensselaer, NY, USA (Prof D O Carpenter MD); Faculty of Pharmacy (Prof F Carvalho PhD), i3S - Instituto de Investigação e Inovação em Saúde and INEB - Instituto de Engenharia Biomédica (J das Neves PhD), Faculty of Medicine (J V Santos MD), UCIBIO@REQUIMTE, Toxicology Group, Faculty of Pharmacy (J P Silva PhD), University of Porto, Porto, Portugal; Stroke Unit, University of Perugia, Perugia, Italy (V Caso MD); Colombian National Health Observatory, Instituto Nacional de Salud, Bogota, Colombia (C A Castañeda-Orjuela MSc); Epidemiology and Public Health Evaluation Group, Public Health Department, Universidad Nacional de Colombia, Bogota, Colombia (C A Castañeda-Orjuela MSc); Department of Medicine, University of Valencia, INCLIVA Health Research Institute and CIBERSAM, Valencia, Spain (F Catalá-López PhD, Prof R Tabarés-Seisdedos PhD); Clinical Epidemiology Program, Ottawa Hospital Research Institute, Ottawa, ON, Canada (F Catalá-López PhD); National Health Research Institutes, Zgunan Town, Taiwan (H Chang DrPH); National Yang-Ming University, Taipei, Taiwan (H Chang DrPH); School of Nursing, College of Medicine, National Taiwan University, Taipei, Taiwan (Prof J Chang PhD); The Park Centre for Mental Health (Prof J J McGrath PhD), Queensland Centre for Mental Health Research, Brisbane, QLD, Australia (F J Charlson PhD, H E Erskine PhD, A J Ferrari PhD, D Santomauro PhD, Prof H A Whiteford PhD); Michigan State University, East Lansing, MI, USA (H Chen PhD); Crowd Watch Africa, Lusaka, Zambia (M Chibalabala BS); National Center for Child Health and Development, Setagaya ku, Japan (C E Chibueze PhD); University of Zambia, Lusaka, Zambia (V H Chisumpa MPhil, C C Mapoma PhD); University of Witwatersrand, Johannesburg, South Africa (V H Chisumpa MPhil); Ministry of Health, Baghdad, Iraq (A A Chitheer MD); Christian Medical College, Vellore, India (Prof D J Christopher MD, Prof S Varughese DM); University of Salerno, Baronissi, Italy (Prof M Cirillo MD); MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton, UK (Prof C Cooper FMedSci); NIHR Biomedical Research Centre, University of Southampton and University Hospital Southampton NHS Foundation Trust, Southampton, UK (Prof C Cooper FMedSci); Research Centre on Public Health (CESP), University of Milan-Bicocca, Monza, Italy (P A Cortesi PhD); VA San Diego (S K Jassal MD), University of California, San Diego, La Jolla, CA, USA (M H Criqui MD, M B Stein MD); Centre for International Health, Dunedin School of Medicine (Prof J A Crump MD), University of Otago, Dunedin, New Zealand (Prof R G Poulton PhD); Flinders University, Adelaide, SA, Australia (Prof A F Dadi MPH, H A Gesesew MPH, Prof K Pesudovs PhD); Centre for Injury Prevention and Safety Promotion, School of Health and Medical Sciences, Orebro University, Orebro, Sweden (Prof K Dalal PhD); Griffith University, Brisbane, QLD, Australia (Prof D De Leo DSc); University of Colorado School of Medicine and the Colorado School of Public Health, Aurora, CO, USA (R P Dellavalle MD); Brighton and Sussex Medical School, Brighton, UK (K Deribe MPH); School of Public Health (K Deribe MPH, A D Hailu MPH), Addis Ababa University, Addis Ababa, Ethiopia (A Z Giref PhD, H A Hareri MS, N A Kassaw MPH, G Temam Shifa MPH); Mount Sinai Beth Israel, New York, NY, USA (Prof D C Des Jarlais PhD); Icahn School of Medicine at Mount Sinai, New York, NY, USA (Prof D C Des Jarlais PhD); Department of Community Medicine, Faculty of Medicine, University of Peradeniya, Peradeniya, Sri Lanka (S D Dharmaratne MD); Undersecretary for Research & Technology, Ministry of Health & Medical Education, Tehran, Iran (S Djalalinia PhD); Institute for Global Health Innovations, Duy Tan University, Da Nang, Vietnam (H P Do MSc, C T Nguyen MSc, Q L Nguyen MD, T H Nguyen MSc, V M Nong MSc); University of Rochester Medical Center, Rochester, NY, USA (E R Dorsey MD); Universidade do Estado de Santa Catarina, Florianópolis, Brazil (Prof K P B dos Santos MA); RMIT University, Bundoora, VIC, Australia (Prof K E Doyle PhD); International Institute for Population Sciences, Mumbai, India (M Dubey MPhil, A Kastor MPhil, P Kumar MPhil, Prof S K Mohanty PhD, B K Panda MPhil, M H U Rahman MPhil, Prof U Ram PhD); Federal University of Rio Grande do Sul, Porto Alegre, Brazil (B B Duncan PhD, C Kieling MD, Prof M I Schmidt MD); University of North Carolina, Chapel Hill, NC, USA (B B Duncan PhD); Department of Global Health and Social Medicine, Harvard Medical School, Kigali, Rwanda (Z Z El-Khatib PhD); School of Public Health and Health Sciences Research Center, Sari, Iran (Prof A Enayati PhD); Arba Minch University, Arba Minch, Ethiopia (A Y Endries MPH, G Temam Shifa MPH); The Institute of Social and Economic Studies of Population, Russian Academy of Sciences, Moscow, Russia (Prof S P Ermakov DSc); Federal Research Institute for Health Organization and Informatics, Ministry of Health of the Russian Federation, Moscow, Russia (Prof S P Ermakov DSc); Ministry of Health and Medical Education, Tehran, Iran (B Eshrati PhD); Arak University of Medical Sciences, Arak, Iran (B Eshrati PhD); Multiple Sclerosis Research Center, Tehran, Iran (S Eskandarieh PhD); Hawassa University, Hawassa, Ethiopia (F B B Fanuel MPH); Wolaita Sodo University, Wolaita Sodo, Ethiopia (F B B Fanuel MPH, F Wadilo MS); DGS Directorate General of Health, Lisboa, Portugal (C S E S Farinha MSc); Universidade Aberta, Lisboa, Portugal (C S E S Farinha MSc); Federal University of Sergipe, Aracaju, Brazil (Prof A Faro PhD); National Institute for Stroke and Applied Neurosciences, Auckland University of Technology, Auckland, New Zealand (V L Feigin PhD); CBQF - Center for Biotechnology and Fine Chemistry - Associate Laboratory, Faculty of Biotechnology, Catholic University of Portugal, Porto, Portugal (J C Fernandes PhD); Wollega University, Nekemte, Ethiopia (T R Feyissa MPH, T Tekelab MS); Kaiser Permanente, Fontana, CA, USA (I Filip MD); School of Public Health, Bielefeld University, Bielefeld, Germany (F Fischer PhD); Fred Hutchinson Cancer Research Center, Seattle, WA, USA (C Fitzmaurice MD); Escola Nacional de Saúde Pública Sergio Arouca (ENSP/Fiocruz), Rio de Janeiro, Brazil (L S Flor MPH); Universidade Federal do Espírito Santo, Vitoria, Brazil (L S Flor MPH); Institute of Gerontology, Academy of Medical Science, Kyiv, Ukraine (N Foigt PhD); James Cook University, Townsville, QLD, Australia (R C Franklin PhD); Department of Epidemiology and Public Health (T Fürst PhD), Swiss Tropical and Public Health Institute, Basel, Switzerland (C K Karema MSc); University of Basel, Basel, Switzerland (T Fürst PhD); Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo, Ribeirão Preto, Brazil (J M Furtado MD); Manhiça Health Research Center, Manhiça, Mozambique (A L Garcia-Basteiro MSc); Barcelona Institute for Global Health, Barcelona, Spain (A L Garcia-Basteiro MSc); The Task Force for Global Health, Decatur, GA, USA (T Gebre PhD); University of Newcastle, Newcastle, NSW, Australia (A Geleto MPH, T Tekelab MS); Madda Walabu University, Bale Goba, Ethiopia (B L Gemechu MPH); The Peter Doherty Institute for Infection and Immunity, The University of Melbourne & The Royal Melbourne Hospital, Melbourne, VIC, Australia (K B Gibney MBBS); Warwick Medical School, University of Birmingham, Birmingham, UK (Prof P S Gill DM); Howard University, Washington, DC, USA (R F Gillum MD); College of Medicine, University of Hail, Hail, Saudi Arabia (I A Ginawi MD); Kersa Health and Demographic Surveillance System, Harar, Ethiopia (M D Gishu MS); University of Massachusetts Boston, Boston, MA, USA (Prof P N Gona PhD); Instituto de Investigaciones Cientificas y Servicios de Alta Tecnologia - INDICASAT-AIP, Cuidad del Saber, Panama (A Goodridge PhD); Department of Health and Social Affairs, Government of the Federated States of Micronesia, Palikir, Federated States of Micronesia (S V Gopalani MPH); Division of Epidemiology, Center for Public Health Sciences, National Cancer Center, Tokyo, Japan (A Goto PhD); Center of Check of Hospital Sirio Libanes, São Paulo, Brazil (A C Goulart PhD); Departments of Microbiology and Epidemiology & Biostatistics, Saint James School of Medicine, The Quarter, Anguilla (Prof H C Gugnani PhD); West Virginia Bureau for Public Health, Charleston, WV, USA (R Gupta MD); Eternal Heart Care Centre and Research Institute, Jaipur, India (R Gupta PhD); Montefiore Medical Center, Bronx, NY, USA (T Gupta MD); Albert Einstein College of Medicine, Bronx, NY, USA (T Gupta MD, Prof H D Hosgood PhD); Department of Anthropology, University of Delhi, Delhi, India (V Gupta PhD); Department of Psychosocial Science (A K Knudsen PhD), Department of Global Public Health and Primary Care (Prof S E Vollset DrPH), University of Bergen, Bergen, Norway (A D Hailu MPH, M C Tollanes PhD); Kilte Awlaelo Health and Demographic Surveillance System, Mekelle, Ethiopia (G B Hailu MSc); Arabian Gulf University, Manama, Bahrain (Prof R R Hamadeh DPhil); Hamdan Bin Mohammed Smart University, Dubai, United Arab Emirates (S Hamidi DrPH); University of New Mexico, Albuquerque, NM, USA (A J Handal PhD); School of Medicine and Pharmacology, University of Western Australia, Perth, WA, Australia (Prof G J Hankey MD); Harry Perkins Institute of Medical Research, Nedlands, WA, Australia (Prof G J Hankey MD); Western Australian Neuroscience Research Institute, Nedlands, WA, Australia (Prof G J Hankey MD); School of Public Health, Sun Yat-sen University, Guangzhou, China (Prof Y Hao PhD); Parc Sanitari Sant Joan de Déu - CIBERSAM, Sant Boi de Llobregat (Barcelona), Spain (J M Haro MD); International Foundation for Dermatology, London, UK (Prof R J Hay DM); Department of Epidemiology, Mailman School of Public Health (Prof H W Hoek MD), Columbia University, New York, NY, USA (Prof V Skirbekk PhD); Epidemiology and Statistics Program, National Institute on Deafness and Other Communication Disorders (H J Hoffman MA), Center for Translation Research and Implementation Science, National Heart, Lung, and Blood Institute (G A Mensah MD), National Institutes of Health, Bethesda, MD, USA; Department of Pulmonology, Yokohama City University Graduate School of Medicine, Yokohama, Japan (N Horita MD); College of Medicine, Baylor University, Houston, TX, USA (P J Hotez PhD); Public Health Division, The Pacific Community, Noumea, New Caledonia (D G Hoy PhD); International Relations Division, Ministry of Health, Nay Pyi Taw, Myanmar (A S Htet MPhil); Department of Epidemiology and Health Statistics, School of Public Health, Central South University, Changsha, China (G Hu PhD); Cambridge Health Alliance, Cambridge, MA, USA (H Huang MD); National Centre for Register-Based Research, Aarhus School of Business and Social Sciences (Prof J J McGrath PhD), Aarhus University, Aarhus, Denmark (K M Iburg PhD); US Centers for Disease Control and Prevention, Pretoria, South Africa (Prof E U Igumbor PhD); School of Public Health, University of the Western Cape, Cape Town, South Africa (Prof E U Igumbor PhD); Department of Global and Community Health, George Mason University, Fairfax, VA, USA (K H Jacobsen PhD); Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia (Prof M B Jakovljevic PhD); University of Aberdeen, Aberdeen, UK (M Javanbakht PhD); Department of Surgery, Virginia Commonwealth University, Richmond, VA, USA (S P Jayaraman MD); Centre for Chronic Disease Control, New Delhi, India (P Jeemon PhD, D Prabhakaran DM); The George Institute for Global Health, New Delhi, India (Prof V Jha DM); Tianjin Centers for Disease Control and Prevention, Tianjin, China (G Jiang MD); International Center for Research on Women, New Delhi, India (D John MPH); Department of Ophthalmology, Medical Faculty Mannheim, Ruprecht-Karls-University Heidelberg, Mannheim, Germany (Prof J B Jonas MD); Institute of Family Medicine and Public Health, University of Tartu, Tartu, Estonia (M Jürisson MD); University College Cork, Cork, Ireland (Z Kabir PhD); London School of Economics and Political Science, London, UK (R Kadel MPH); CSIR - Indian Institute of Toxicology Research, Lucknow, India (R Kamal MSc); Department of Pulmonary Medicine, Zhongshan Hospital (J She MD), Fudan University, Shanghai, China (H Kan MD); University of Balamand, Beirut, Lebanon (N E Karam MD); Epidemiological and Statistical Methods Research Group, Helmholtz Centre for Infection Research, Braunschweig, Germany (A Karch MD); Hannover-Braunschweig Site, German Center for Infection Research, Braunschweig, Germany (A Karch MD); Quality and Equity Health Care, Kigali, Rwanda (C K Karema MSc); Department of Anesthesiology & Pain Medicine, Seattle Children's Hospital, Seattle, WA, USA (N J Kassebaum MD); MRC/CSO Social & Public Health Sciences Unit, University of Glasgow, Glasgow, UK (S V Katikireddi PhD); Oklahoma State University, Tulsa, OK, USA (A Kaul MD); School of Public Health, University of Tokyo, Tokyo, Japan (Prof N Kawakami MD); Institute of Tropical and Infectious Diseases, Nairobi, Kenya (P N Keiyoro PhD); School of Continuing and Distance Education, Nairobi, Kenya (P N Keiyoro PhD); UKZN Gastrointestinal Cancer Research Centre (Prof B Sartorius PhD), South African Medical Research Council, Cape Town, South Africa (A P Kengne PhD); Department of Psychiatry (Prof D J Stein PhD), University of Cape Town, Cape Town, South Africa (A P Kengne PhD, J J N Noubiap MD); Assuta Hospitals, Assuta Hashalom, Tel Aviv, Israel (Prof A Keren MD); Department of Community Medicine, Public Health and Family Medicine, Jordan University of Science and Technology, Irbid, Jordan (Prof Y S Khader ScD); Health Services Academy, Islamabad, Pakistan (E A Khan MD); Department of Health Policy and Management, Seoul National University College of Medicine, Seoul, South Korea (Prof Y Khang MD); Institute of Health Policy and Management, Seoul National University Medical Center, Seoul, South Korea (Prof Y Khang MD); Iranian Ministry of Health and Medical Education, Tehran, Iran (A Khosravi PhD); Department of Nutrition and Health Science, Ball State University, Muncie, IN, USA (J Khubchandani PhD); Hospital de Clinicas de Porto Alegre, Porto Alegre, Brazil (C Kieling MD); Department of Health Sciences, Northeastern University, Boston, MA, USA (Prof D Kim DrPH); School of Medicine, Xiamen University Malaysia Campus, Sepang, Malaysia (Y J Kim PhD); Simmons College, Boston, MA, USA (R W Kimokoti MD); Centre for Research and Action in Public Health, University of Canberra, Canberra, ACT, Australia (Y Kinfu PhD); Oslo University, Oslo, Norway (Prof A Kisa PhD); Institute of Public Health, Faculty of Health Sciences (R Topor-Madry PhD), Jagiellonian University Medical College, Krakow, Poland (K A Kissimova-Skarbek PhD); Clinicum (Prof M Kivimaki PhD), Finnish Institute of Occupational Health, Work Organizations, Work Disability Program, Department of Public Health (R Shiri PhD), Faculty of Medicine, University of Helsinki, Helsinki, Finland (T J Meretoja PhD); Center for Disease Burden (A K Knudsen PhD, Prof S E Vollset DrPH), Norwegian Institute of Public Health, Oslo, Norway (Prof V Skirbekk PhD); Department of Preventive Cardiology, National Cerebral and Cardiovascular Center, Suita, Japan (Y Kokubo PhD); Division of Cardiology, Brown University, Providence, RI, USA (D Kolte MD); University of British Columbia, Vancouver, BC, Canada (J A Kopec PhD, F Pourmalek PhD); Center for Community Empowerment, Health Policy and Humanities, National Institute of Health Research & Development, Jakarta, Indonesia (S Kosen MD); Sher-i-Kashmir Institute of Medical Sciences, Srinagar, India (Prof P A Koul MD); Research and Development Unit, Parc Sanitari Sant Joan de Deu (CIBERSAM), Barcelona, Spain (A Koyanagi MD); Research Center of Neurology, Moscow, Russia (M Kravchenko PhD); Oregon Health and Science University, Portland, OR, USA (S Krishnaswami MD); Department of Social and Preventive Medicine, School of Public Health, and Department of Demography and Public Health Research Institute, University of Montreal, Montreal, QC, Canada (Prof B Kuate Defo PhD); Institute of Public Health, Hacettepe University, Ankara, Turkey (B Kucuk Bicer PhD); National Health Systems Resource Centre, New Delhi, India (S Kumar MD); Ministry of Public Health and Fight Against AIDS, Mukaza, Burundi (N Lambert MD); National Cancer Institute, Rockville, MD, USA (Q Lan PhD); Department of Medical Sciences, Uppsala University, Uppsala, Sweden (Prof A Larsson PhD); Servicio de Neurologia, Clinica Alemana, Universidad del Desarrollo, Santiago, Chile (P M Lavados MD); College of Optometry, Nova Southeastern University, Fort Lauderdale, FL, USA (J L Leasher OD); Department of Preventive Medicine, College of Medicine (S Yoon PhD), Korea University, Seoul, South Korea (Prof J Lee PhD); Hong Kong Polytechnic University, Hong Kong, China (P H Lee PhD); State University of New York, Albany, Rensselaer, NY, USA (R Leung PhD); Tuscany Regional Centre for Occupational Injuries and Diseases, Florence, Italy (M Levi PhD); Department of Data Management, Peking University Clinical Research Institute, Beijing, China (Y Li PhD); National Center for Chronic and Noncommunicable Disease Control and Prevention (Y Li PhD, S Liu PhD, P Ye MPH, Prof M Zhou PhD), Chinese Center for Disease Control and Prevention, Beijing, China (Prof X Liang MD); San Francisco VA Medical Center, San Francisco, CA, USA (Y Li PhD); Samara University, Samara, Ethiopia (M L Liben MPH); University of Haifa, Haifa, Israel (Prof S Linn MD); Emory University, Atlanta, GA, USA (Prof Y Liu PhD, Prof M R Phillips MD); University of Bari, Bari, Italy (Prof G Logroscino PhD); Division of Intramural Research, National Institute of Environmental Health Sciences (S J London MD), National Institutes of Health, Research Triangle Park, NC, USA; University of Bristol, Bristol, UK (K J Looker PhD); Institute of Nutrition, Friedrich Schiller University Jena, Jena, Germany (Prof S Lorkowski PhD); Competence Cluster for Nutrition and Cardiovascular Health (nutriCARD) Halle-Jena-Leipzig, Jena, Germany (Prof S Lorkowski PhD); Institute of Social and Preventive Medicine, University of Bern, Bern, Switzerland (Prof N Low MD); Ateneo de Manila University, Manila, Philippines (E R K Macarayan PhD); Mansoura Faculty of Medicine, Mansoura, Egypt (H Magdy Abd El Razek MBBCH); Aswan University Hospital, Aswan Faculty of Medicine, Aswan, Egypt (M Magdy Abd El Razek MBBCH); Erasmus University Rotterdam, Rotterdam, Netherlands (M Mahdavi PhD); Faculty of Health Sciences and Social Work, Department of Public Health, Trnava University, Trnava, Slovakia (M Majdan PhD); National Institute of Health Research, Tehran, Iran (Prof R Majdzadeh PhD); Universidade Federal de Minas Gerais, Belo Horizonte, Brazil (Prof D C Malta PhD); The University of Queensland, Brisbane, QLD, Australia (Prof A A Mamun PhD); University of Milano Bicocca, Monza, Italy (Prof L G Mantovani DSc); Hospital Universitario Doctor Peset, Valencia, Spain (J Martinez-Raga PhD, M Tortajada PhD); CEU Cardinal Herrera University, Moncada, Spain (J Martinez-Raga PhD); Federal Institute of Education, Science and Technology of Ceará, Caucaia, Brazil (F R Martins-Melo PhD); Synlab Academy, Mannheim, Germany (Prof W März MD); Clinical Institute of Medical and Chemical Laboratory Diagnostics, Medical University of Graz, Graz, Austria (Prof W März MD); Key State Laboratory of Molecular Developmental Biology, Institute of Genetics and Developmental Biology, Chinese Academy of Sciences, Beijing, China (M Mazidi PhD); University Hospitals Bristol NHS Foundation Trust, Bristol, UK (C McAlinden PhD); Public Health Wales, Swansea, UK (C McAlinden PhD); London School of Hygiene and Tropical Medicine, London, UK (Prof M McKee DSc, Prof G V S Murthy MD, Prof N Pearce PhD); Ipas Nepal, Kathmandu, Nepal (S Mehata PhD); Janakpuri Superspecialty Hospital, New Delhi, India (Prof M M Mehndiratta DM); Wollo University, Dessie, Ethiopia (T C Mekonnen MPH); University of West Florida, Pensacola, FL, USA (P Memiah PhD); Saudi Ministry of Health, Riyadh, Saudi Arabia (Prof Z A Memish MD); College of Medicine, Alfaisal University, Riyadh, Saudi Arabia (Prof Z A Memish MD); United Nations Population Fund, Lima, Peru (W Mendoza MD); Department of Neurology (A Meretoja PhD), Comprehensive Cancer Center, Breast Surgery Unit (T J Meretoja PhD), Helsinki University Hospital, Helsinki, Finland; Friedman School of Nutrition Science and Policy (R Micha PhD), Tufts University, Boston, MA, USA (P Shi PhD); Pacific Institute for Research & Evaluation, Calverton, MD, USA (T R Miller PhD); Centre for Population Health, Curtin University, Perth, WA, Australia (T R Miller PhD); University of Ottawa, Ottawa, ON, Canada (E J Mills PhD); Hunger Action Los Angeles, Los Angeles, CA, USA (M Mirarefin MPH); Kyrgyz State Medical Academy, Bishkek, Kyrgyzstan (Prof E M Mirrakhimov PhD); National Center of Cardiology and Internal Disease, Bishkek, Kyrgyzstan (Prof E M Mirrakhimov PhD); Nepal Development Society, Chitwan, Nepal (S R Mishra MPH); University of Salahaddin, Erbil, Iraq (K A Mohammad PhD); ISHIK University, Erbil, Iraq (K A Mohammad PhD); Neuroscience Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran (A Mohammadi PhD); Health Systems and Policy Research Unit (S Mohammed PhD), Ahmadu Bello University, Zaria, Nigeria (M B Sufiyan MBA); Institute for Maternal and Child Health, IRCCS “Burlo Garofolo”, Trieste, Italy (L Monasta DSc, M Montico MSc, L Ronfani PhD); Department of Community Medicine (A Tehrani-Banihashemi PhD), Preventive Medicine and Public Health Research Center, Gastrointestinal and Liver Disease Research Center (GILDRC) (M Moradi-Lakeh MD), Preventive Medicine and Public Health Research Center (A Tehrani-Banihashemi PhD), Iran University of Medical Sciences, Tehran, Iran (M Yaghoubi MSc); Lancaster Medical School, Lancaster University, Lancaster, UK (P Moraga PhD); National Center for Child Health and Development, Setagaya, Japan (R Mori PhD); Competence Center Mortality-Follow-Up of the German National Cohort (A Werdecker PhD), Federal Institute for Population Research, Wiesbaden, Germany (Prof U O Mueller PhD, R Westerman PhD); West Herts Hospitals NHS Trust, Watford, United Kingdom (M E Murdoch MD); School of Medical Sciences, University of Science Malaysia, Kubang Kerian, Malaysia (K I Musa MD); Graduate School of Public Health, University of Pittsburgh, Pittsburgh, PA, USA (Prof J B Nachega PhD); Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA (Prof J B Nachega PhD); Ulm University, Ulm, Germany (Prof G Nagel PhD); International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b), Dhaka, Bangladesh (A Naheed PhD, S M Shariful Islam PhD); Public Health Medicine, School of Nursing and Public Health (Prof B Sartorius PhD), Discipline of Public Health Medicine, School of Nursing and Public Health (B Yakob PhD), University of KwaZulu-Natal, Durban, South Africa (Prof K S Naidoo PhD, E A Zegeye MS); Azienda Ospedaliera Papa Giovanni XXIII, Bergamo, Italy (Prof L Naldi MD); Suraj Eye Institute, Nagpur, India (V Nangia MD); Madras Medical College, Chennai, India, India (Prof G Natarajan DM); KEMRI Wellcome Trust, Kilifi, Kenya (Prof C R Newton MD); University of Nairobi, Nairobi, Kenya (J W Ngunjiri PhD); Department of Public Health, Semarang State University, Semarang City, Indonesia (D N A Ningrum MPH); Graduate Institute of Biomedical Informatics, College of Medical Science and Technology, Taipei Medical University, Taipei City, Taiwan (D N A Ningrum MPH); Population Health Strategic Research Centre, School of Health and Social Development (S Nolte PhD), Deakin University, Burwood, VIC, Australia (Prof M A Stokes PhD); Medical Diagnostic Centre, Yaounde, Cameroon (J J N Noubiap MD); National University of Ireland Galway, Galway, Ireland (M J O'Donnell PhD); Centre for Health Research (F A Ogbo MPH), Western Sydney University, Penrith, NSW, Australia (Prof A M N Renzaho PhD); Department of Preventive Medicine, School of Medicine, Kyung Hee University, Seoul, South Korea (Prof I Oh PhD); Society for Family Health, Abuja, Nigeria (A Okoro MPH); Human Sciences Research Council (HSRC), South Africa and University of KwaZulu-Natal, Durban, South Africa (O Oladimeji MS); Department of Psychiatry, College of Medicine, University of Lagos, Lagos, Nigeria (A T Olagunju MS); Department of Psychiatry, Lagos University Teaching Hospital, Lagos, Nigeria (A T Olagunju MS); McMaster University, Hamilton, ON, Canada (T O Olagunju MD); Department of Clinical Neurological Sciences (L A Sposato MD), Western University, London, ON, Canada (T O Olagunju MD); Center for Healthy Start Initiative, Lagos, Nigeria (B O Olusanya PhD, J O Olusanya MBA); Lira District Local Government, Lira Municipal Council, Uganda (J N Opio MPH); University of Arizona, Tucson, AZ, USA (Prof E Oren PhD); IIS-Fundacion Jimenez Diaz-UAM, Madrid, Spain (Prof A Ortiz PhD); YBank, Cambridge, MA, USA (M Osman MD); Department of Medicine, Ibadan, Nigeria (M O Owolabi DrMed); Blossom Specialist Medical Center, Ibadan, Nigeria (M O Owolabi DrMed); JSS Medical College, JSS University, Mysore, India (Prof M PA DNB); Institute of Health and Biomedical Innovation, Queensland University of Technology, Brisbane, QLD, Australia (R E Pacella PhD); Bucharest University of Economic Studies, Bucharest, Romania (A Pana MPH); Charité University Medicine Berlin, Berlin, Germany (C Papachristou PhD); Department of Medical Humanities and Social Medicine, College of Medicine, Kosin University, Busan, South Korea (E Park PhD); Alcohol, Tobacco & Other Drug Research Unit (Prof C D Parry PhD), South African Medical Research Council, Cape Town, South Africa (A P Kengne PhD); Department of Community Health Sciences (Prof S B Patten PhD), University of Calgary, Calgary, AB, Canada (Prof M Tonelli MD); REQUIMTE/LAQV, Laboratório de Farmacognosia, Departamento de Química, Faculdade de Farmácia, Universidade do Porto, Porto, Portugal (Prof D M Pereira PhD); Health Metrics Unit, University of Gothenburg, Gothenburg, Sweden (Prof M Petzold PhD); University of the Witwatersrand, Johannesburg, South Africa (Prof M Petzold PhD); Shanghai Jiao Tong University School of Medicine, Shanghai, China (Prof M R Phillips MD); Durban University of Technology, Durban, South Africa (J D Pillay PhD); Exposure Assessment and Environmental Health Indicators, German Environment Agency, Berlin, Germany (D Plass DrPH); Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India (Prof N Prasad DM); The Fred Hollows Foundation, Sydney, NSW, Australia (N M Prasad DO); Centre for Eye Research Australia, Melbourne, VIC, Australia (N M Prasad DO); Non-Communicable Diseases Research Center, Alborz University of Medical Sciences, Karaj, Iran (M Qorbani PhD); University of Ghana, Accra, Ghana (R Quansah PhD); Noguchi Memorial Institute of Medical Research, Accra, Ghana (R Quansah PhD); A T Still University, Kirksville, MO, USA (A Radfar MD); Contech International Health Consultants, Lahore, Pakistan (A Rafay MS); Contech School of Public Health, Lahore, Pakistan (A Rafay MS); Research and Evaluation Division, BRAC, Dhaka, Bangladesh (M Rahman PhD); Society for Health and Demographic Surveillance, Suri, India (R K Rai MPH); ERAWEB Program, University for Health Sciences, Medical Informatics and Technology, Hall in Tirol, Austria (S Rajsic MD); Department of Preventive Medicine, Wonju College of Medicine, Yonsei University, Wonju, South Korea (C L Ranabhat PhD); Health Science Foundation and Study Center, Kathmandu, Nepal (C L Ranabhat PhD); Diabetes Research Society, Hyderabad, India (Prof P V Rao MD); Diabetes Research Center, Hyderabad, India (Prof P V Rao MD); Azienda Socio-Sanitaria Territoriale, Papa Giovanni XXIII, Bergamo, Italy (Prof G Remuzzi MD); Department of Biomedical and Clinical Sciences “L Sacco”, University of Milan, Milan, Italy (Prof G Remuzzi MD); Research Center for Environmental Determinants of Health, School of Public Health, Kermanshah University of Medical Sciences, Kermanshah, Iran (S Rezaei PhD); Hospital das Clínicas da Universidade Federal de Minas Gerais, Belo Horizonte, Brazil (Prof A L Ribeiro MD); Golestan Research Center of Gastroenterology and Hepatology, Golestan University of Medical Sciences, Gorgan, Iran (G Roshandel PhD); Universidad Tecnica del Norte, Ibarra, Ecuador (E Rubagotti PhD); Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania (G M Ruhago PhD, B F Sunguya PhD); Managerial Epidemiology Research Center, Department of Public Health, School of Nursing and Midwifery, Maragheh University of Medical Sciences, Maragheh, Iran (S Safiri PhD); Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia (R Sahathevan PhD); Ballarat Health Service, Ballarat, VIC, Australia (R Sahathevan PhD); Chest Research Foundation, Pune, India (S S Salvi MD); Faculty of Science, Ain Shams University, Cairo, Egypt (A M Samy PhD); J Edwards School of Medicine, Marshall University, Huntington, WV, USA (J R Sanabria MD, M Sawhney PhD); Case Western Reserve University, Cleveland, OH, USA (J R Sanabria MD); Department of Community Medicine, Information and Health Decision Sciences, Center for Health Technology and Services Research - CINTESIS, Porto, Portugal (J V Santos MD); Centre of Advanced Study in Psychology, Utkal University, Bhubaneswar, India (M Satpathy PhD); Federal University of Santa Catarina, Florianópolis, Brazil (I J C Schneider PhD); Division of Clinical Epidemiology and Ageing Research, German Cancer Research Center, Heidelberg, Germany (B Schöttker MPH); Institute of Health Care and Social Sciences, FOM University, Essen, Germany (B Schöttker MPH); University of Alabama at Birmingham, Birmingham, AL, USA (D C Schwebel PhD, J A Singh MD); Charité Berlin, Berlin, Germany (F Schwendicke PhD); Department of Public Health, An-Najah University, Nablus, Palestine (A Shaheen PhD); Independent Consultant, Karachi, Pakistan (M A Shaikh MD); The George Institute for Global Health, Sydney, NSW, Australia (S M Shariful Islam PhD); Ministry of Health, Thimphu, Bhutan (J Sharma MPH); Indian Institute of Technology Ropar, Rupnagar, India (R Sharma MA); National Institute of Infectious Diseases, Tokyo, Japan (M Shigematsu PhD); Sandia National Laboratories, Albuquerque, NM, USA (M Shigematsu PhD); Tachikawa Hospital, Tokyo, Japan (Y Shinohara PhD); Washington State University, Spokane, WA, USA (K Shishani PhD); Harvard Medical School, Boston, MA, USA (M Osman MD, M G Shrime MD); American University of Beirut, Beirut, Lebanon (Prof A M Sibai PhD); Reykjavik University, Reykjavik, Iceland (I D Sigfusdottir PhD); Federal University of Santa Catarina, Florianopolis, Brazil (D A S Silva PhD); Brasília University, Brasília, Brazil (D G A Silveira MD); Max Hospital, Ghaziabad, India (Prof N P Singh MD); School of Preventive Oncology, Patna, India (D N Sinha PhD); WHO FCTC Global Knowledge Hub on Smokeless Tobacco, National Institute of Cancer Prevention, Noida, India (D N Sinha PhD); Hywel Dda University Health Board, Carmarthen, UK (E Skiadaresi MD); Bristol Eye Hospital, Bristol, UK (E Skiadaresi MD); King Khalid University Hospital, Riyadh, Saudi Arabia (B H A Sobaih MD); University of Yaoundé, Yaoundé, Cameroon (Prof E Sobngwi PhD); Yaoundé Central Hospital, Yaoundé, Cameroon (Prof E Sobngwi PhD); National School of Public Health/Oswaldo Cruz Foundation, Rio de Janeiro, Brazil (Prof T C M Sousa MPH); Department of Community Medicine, International Medical University, Kuala Lumpur, Malaysia (C T Sreeramareddy MD); Attikon University Hospital, Athens, Greece (V Stathopoulou PhD); University of East Anglia, Norwich, UK (Prof N Steel PhD); Public Health England, London, UK (Prof N Steel PhD); South African Medical Research Council Unit on Anxiety & Stress Disorders, Cape Town, South Africa (Prof D J Stein PhD); Department of Neuroscience, Norwegian University of Science and Technology, Trondheim, Norway (Prof T J Steiner PhD, Prof L J Stovner PhD); Department of Dermatology, University Hospital Muenster, Muenster, Germany (S Steinke DrMed); Norwegian Advisory Unit on Headache, St Olavs Hospital, Trondheim, Norway (Prof L J Stovner PhD); Ministry of Health, Kingdom of Saudi Arabia, Riyadh, Saudi Arabia (R Suliankatchi Abdulkader MD); Indian Council of Medical Research, New Delhi, India (S Swaminathan MD); Departments of Criminology, Law & Society, Sociology, and Public Health, University of California, Irvine, Irvine, CA, USA (Prof B L Sykes PhD); WSH Institute, Ministry of Manpower, Singapore, Singapore (J S Takala DSc); Tampere University of Technology, Tampere, Finland (J S Takala DSc); New York Medical Center, Valhalla, NY, USA (M Tavakkoli MD); Instituto Superior de Ciências da Saúde Egas Moniz, Almada, Portugal (Prof N Taveira PhD); Faculty of Pharmacy, Universidade de Lisboa, Lisboa, Portugal (Prof N Taveira PhD); Department of Anesthesiology, University of Virginia, Charlottesville, VA, USA (A S Terkawi MD); Department of Anesthesiology, King Fahad Medical City, Riyadh, Saudi Arabia (A S Terkawi MD); Outcomes Research Consortium (A S Terkawi MD), Cleveland Clinic, Cleveland, OH, USA (Prof E M Tuzcu MD); National Center for Child Health and Development, Tokyo, Japan (R Tobe-Gai PhD); National Institute of Public Health, Bergen, Norway (M C Tollanes PhD); Faculty of Health Sciences, Wroclaw Medical University, Wroclaw, Poland (R Topor-Madry PhD); School of Medicine, University of Valencia, Valencia, Spain (M Tortajada PhD); INSERM (French National Institute for Health and Medical Research), Paris, France (M Touvier PhD); Hanoi Medical University, Hanoi, Vietnam (B X Tran PhD); Department of Neurology, Rigshospitalet, University of Copenhagen, Copenhagen, Denmark (T Truelsen DMSc); Parc Sanitari Sant Joan de Déu, Fundació Sant Joan de Déu, Universitat de Barcelona, CIBERSAM, Barcelona, Spain (S Tyrovolas PhD); Department of Internal Medicine, Federal Teaching Hospital, Abakaliki, Nigeria (K N Ukwaja MD); School of Government, Pontificia Universidad Catolica de Chile, Santiago, Chile (E A Undurraga PhD); Ebonyi State University, Abakaliki, Nigeria (C J Uneke PhD); Warwick Medical School, University of Warwick, Coventry, UK (O A Uthman PhD); University of Nigeria, Nsukka, Enugu Campus, Enugu, Nigeria (Prof B S C Uzochukwu MD); UKK Institute for Health Promotion Research, Tampere, Finland (Prof T Vasankari PhD); National Centre for Disease Control, Delhi, India (S Venkatesh MD); Raffles Neuroscience Centre, Raffles Hospital, Singapore, Singapore (N Venketasubramanian MBBS); Weill Cornell Medical College, New York, NY, USA (R Vidavalur MD); University of Bologna, Bologna, Italy (Prof F S Violante MD); Federal Research Institute for Health Organization and Informatics, Moscow, Russia (S K Vladimirov PhD); National Research University Higher School of Economics, Moscow, Russia (Prof V V Vlassov MD); University of São Paulo Medical School, São Paulo, Brazil (Y Wang PhD); McGill University, Ottawa, ON, Canada (S Weichenthal PhD); Department of Research, Cancer Registry of Norway, Institute of Population-Based Cancer Research, Oslo, Norway (E Weiderpass PhD); Department of Community Medicine, Faculty of Health Sciences, University of Tromsø, The Arctic University of Norway, Tromsø, Norway (E Weiderpass PhD); Genetic Epidemiology Group, Folkhälsan Research Center, Helsinki, Finland (E Weiderpass PhD); Royal Children's Hospital, Melbourne, VIC, Australia (R G Weintraub MBBS); Murdoch Childrens Research Institute, Melbourne, VIC, Australia (R G Weintraub MBBS); German National Cohort Consortium, Heidelberg, Germany (R Westerman PhD); Western Health, Footscray, VIC, Australia (Prof T Wijeratne MD); South African Medical Research Council, Cochrane South Africa, Cape Town, South Africa (Prof C S Wiysonge PhD); National Institute for Health Research Comprehensive Biomedical Research Centre, Guy's & St Thomas' NHS Foundation Trust and King's College London, London, UK (Prof C D Wolfe MD); Royal Cornwall Hospital, Truro, UK (Prof A D Woolf MBBS); Ghent University, Ghent, Belgium (A Workicho MPH); St John's Medical College and Research Institute, Bangalore, India (Prof D Xavier MD); Department of Neurology, Jinling Hospital, Nanjing University School of Medicine, Nanjing, China (Prof G Xu PhD); School of Public Health, University of Saskatchewan, Saskatoon, SK, Canada (M Yaghoubi MSc); Global Health Research Center, Duke Kunshan University, Kunshan, China (Prof L L Yan PhD); Department of Preventive Medicine, Northwestern University, Chicago, IL, USA (Y Yano MD); Social Work and Social Administration Department (Prof P Yip PhD), The Hong Kong Jockey Club Centre for Suicide Research and Prevention (Prof P Yip PhD), University of Hong Kong, Hong Kong, China; Department of Biostatistics, School of Public Health, Kyoto University, Kyoto, Japan (N Yonemoto MPH); The Ohio State University, Columbus, OH, USA (M Yotebieng PhD); School of Public Health, University of Kinshasa, Kinshasa, Democratic Republic of the Congo (M Yotebieng PhD); Jackson State University, Jackson, MS, USA (Prof M Z Younis DrPH); University Hospital of Setif, Setif, Algeria (Prof Z Zaidi DSc); Faculty of Medicine, Mansoura University, Mansoura, Egypt (Prof M E Zaki PhD); Ethiopian Public Health Institute, Addis Ababa, Ethiopia (E A Zegeye MS); University of Texas School of Public Health, Houston, TX, USA (X Zhang MS); MD Anderson Cancer Center, Houston, TX, USA (X Zhang MS); and Red Cross War Memorial Children's Hospital, Cape Town, South Africa (L J Zuhlke PhD).
Contributors
Please see the appendix for more detailed information about individual authors' contributions to the research, divided into the following categories: managing the estimation process; writing the first draft of the manuscript; providing data or critical feedback on data sources; developing methods or computational machinery; applying analytical methods to produce estimates; providing critical feedback on methods or results; drafting the work or revising it critically for important intellectual content; extracting, cleaning, or cataloging data; designing or coding figures and tables; and managing the overall research enterprise.
References:
Nino F.
United Nations Sustainable Development Goals. UNDP.
http://www.undp.org/content/undp/en/home/sustainable-development-goals.html
(accessed March 10, 2017).Lim SS, Allen K, Bhutta ZA.
Measuring the health-related Sustainable Development Goals in 188 countries:
a baseline analysis from the Global Burden of Disease Study 2015.
Lancet. 2016;388:1813–1850GBD 2015 Disease and Injury Incidence and Prevalence Collaborators.
Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 310 Diseases
and Injuries, 1990-2015: a Systematic Analysis for the Global Burden of Disease Study 2015
Lancet. 2016 (Oct 8); 388 (10053): 1545–1602Kassebaum NJ, Arora M, Barber RM.
Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases
and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for
the Global Burden of Disease Study 2015.
Lancet. 2016;388:1603–1658Kissoon N, Uyeki TM.
Sepsis and the Global Burden of Disease in Children.
JAMA Pediatr. 2016;170:107–108Limmathurotsakul D, Golding N, Dance DAB.
Predicted global distribution of Burkholderia pseudomallei and burden of melioidosis.
Nature Microbiology. 2016;1 nmicrobiol20158Vallabhaneni S, Mody RK, Walker T, Chiller T.
The Global Burden of Fungal Diseases.
Infect Dis Clin North Am. 2016;30:1–11Vigo D, Thornicroft G, Atun R.
Estimating the true global burden of mental illness.
Lancet Psychiatry. 2016;3:171–178Holden BA, Fricke TR, Wilson DA.
Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050.
Ophthalmology. 2016;123:1036–1042Jackson T, Thomas S, Stabile V, Shotwell M, Han X, McQueen K.
A Systematic Review and Meta-Analysis of the Global Burden of Chronic Pain Without Clear
Etiology in Low- and Middle-Income Countries: Trends in Heterogeneous Data and a
Proposal for New Assessment Methods.
Anesth Analg. 2016;123:739–748Chavan BS, Aneja J.
Global mental health movement has not helped in reducing global burden of psychiatric disorders.
Indian JSoc Psychiatry. 2016;32:261–266.Neethling I, Jelsma J, Ramma L, Schneider H, Bradshaw D.
Disability weights from a household survey in a low socio-economic setting:
how does it compare to the global burden of disease 2010 study?
Global Health Action. 2016;9:31754Jager KJ, Fraser SDS.
The ascending rank of chronic kidney disease in the global burden of disease study.
Nephrol Dial Transplant. 2017;32:ii121–ii128Jin LJ, Lamster IB, Greenspan JS, Pitts NB, Scully C, Warnakulasuriya S.
Global burden of oral diseases: emerging concepts, management and interplay with systemic health.
Oral Diseases. 2016;22:609–619Kwan GF, Mayosi BM, Mocumbi AO.
Endemic Cardiovascular Diseases of the Poorest Billion.
Circulation. 2016;133:2561–2575Flaxman AD, Vos T, Murray CJL, editors.
An Integrative Metaregression Framework for Descriptive Epidemiology. 1st edn.
University of Washington Press; Seattle: 2015.Stevens GA, Alkema L, Black RE.
Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement.
Lancet. 2016;388:e19–e23GBD 2016 Causes of Death Collaborators Global, regional, and
national age-sex specific mortality for 264 causes of death, 1980–2016:
a systematic analysis for the Global Burden of Disease Study 2016.
Lancet. 2017;390:1151–1210National Tuberculosis Institute Tuberculosis in a rural population
of South India: a five-year epidemiological study.
Bull World Health Organ. 1974;51:473–488Mesfin YM, Hailemariam D, Biadglign S, Kibret KT.
Association between HIV/AIDS and Multi-Drug Resistance Tuberculosis:
A Systematic Review and Meta-Analysis.
PLoS One. 2014;9:e82235Banks JL, Marotta CA.
Outcomes validity and reliability of the modified Rankin scale:
implications for stroke clinical trials: a literature review and synthesis.
Stroke. 2007;38:1091–1096GBD 2016 Mortality Collaborators Global, regional, and national under-5 mortality,
adult mortality, age-specific mortality, and life expectancy, 1970–2016:
a systematic analysis for the Global Burden of Disease Study 2016.
Lancet. 2017;390:1084–1150Agency for Healthcare Research and Quality.
United States Medical Expenditure Panel Survey.
Rockville, USA: Agency for Health Care Research and Quality.McKee S.
Rethinking Development and Health: Findings from the Global Burden of Disease Study.
Institute for Health Metrics and Evaluation;
Seattle, Washington, USA: 2016.
http://www.healthdata.org/sites/default/files/files/policy_report/GBD/2016/
IHME_GBD2015_report.pdf
(accessed June 1, 2017).Tsang A, Von Korff M, Lee S.
Common Chronic Pain Conditions in Developed and Developing Countries:
Gender and Age Differences and Comorbidity With Depression-Anxiety Disorders.
J Pain. 2008;9:883–891Parker G, Cheah Y-C, Roy K.
Do the Chinese somatize depression? A cross-cultural study.
Soc Psychiatry Psychiatr Epidemiol. 2001;36:287–293Tung W-C, Li Z.
Pain Beliefs and Behaviors Among Chinese.
Home Health Care Management & Practice. 2015;27:95–97.Anand A.
Understanding Depression among Older Adults in Six Low-Middle Income Countries
using WHO-SAGE Survey.
http://jghcs.info/index.php/bh/article/view/363
(accessed July 17, 2017).Phillips MR, Zhang J, Shi Q.
Prevalence, treatment, and associated disability of mental disorders in four provinces
in China during 2001–05: an epidemiological survey.
Lancet. 2009;373:2041–2053WHO .
Antimicrobial resistance: global report on surveillance, 2014.
World Health Organization; Geneva, Switzerland: 2014.Spellberg B, Bartlett JG, Gilbert DN.
The Future of Antibiotics and Resistance.
N Engl J Med. 2013;368:299–302Burnham G, Doocy S, Dzeng E, Lafta R, Roberts L.
The Human Cost of the War in Iraq. A Mortality Study, 2002–2006.
Bloomberg School of Public Health, Johns Hopkins University;
School of Medicine, Al Mustansiriya University;
Center for International Studies, Massachusetts Institute of Technology;
Baltimore, MD; Baghdad, Iraq; Cambridge, MA: 2016.McMichael AJ, Woodruff RE, Hales S.
Climate change and human health: present and future risks.
Lancet. 2006;367:859–869Patz JA, Campbell-Lendrum D, Holloway T, Foley JA.
Impact of regional climate change on human health.
Nature. 2005;438:310–317Ramsey R, Giskes K, Turrell G, Gallegos D.
Food insecurity among adults residing in disadvantaged urban areas:
potential health and dietary consequences.
Public Health Nutr. 2012;15:227–237Hassan G, Ventevogel P, Jefee-Bahloul H, Barkil-Oteo A, Kirmayer LJ.
Mental health and psychosocial wellbeing of Syrians affected by armed conflict.
Epidemiol Psychiatr Sci. 2016;25:129–141Rapid Assessment of Avoidable Blideness Repository RAAB Repository.
http://raabdata.info/repository/
(accessed July 17, 2017).Brooker S, Hotez PJ, Bundy DAP.
The Global Atlas of Helminth Infection: Mapping the Way Forward in Neglected Tropical Disease Control.
PLOS Neglected Tropical Diseases. 2010;4:e779WHO .
Guidelines on the management of latent tuberculosis infection.
World Health Organization; Geneva, Switzerland: 2015.
http://www.who.int/tb/publications/latent-tuberculosis-infection/en/
(accessed May 3, 2017).Patel V, Chisholm D, Parikh R.
Addressing the burden of mental, neurological, and substance use disorders:
key messages from Disease Control Priorities, 3rd edition.
Lancet. 2016;387:1672–1685Afshin A, Forouzanfar MH, Reitsma M, Sur P, Estep K, Murray CJ.
Obesity and overweight and their health impact 1990-2015 in 195 countries.
N Engl J Med. 2017;377:13–27Dieleman JL, Baral R, Birger M, et al.
US Spending on Personal Health Care and Public Health, 1996-2013
JAMA 2016 (Dec 27); 316 (24): 2627-2646WHO .
Global Tuberculosis Report 2016.
World Health Organization;
Geneva, Switzerland: 2016.WHO .
Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis.
World Health Organization;
Geneva, Switzerland: 2014National AIDS and STI Control Programme (NASCOP) Kenya AIDS Indicator Survey 2012:
Final Report. NASCOP; Nairobi, Kenya: 2014.Ministry of Health, ICF International,
Centers for Disease Control and Prevention,
U.S. Agency for International Development, and WHO Uganda .
Uganda AIDS Indicator Survey. Ministry of Health; Kampala, Uganda: 2012.UNAIDS Global AIDS update 2016. 2016;
published online May 31.
http://www.unaids.org/en/resources/documents/2016/Global-AIDS-update-2016
(accessed March 10, 2017).International Agency for Research on Cancer .
Globocan 2012: Estimated Cancer Incidence, Mortality, and Prevlance Worldwide in 2012.
World Health Organization; Geneva: 2017.WHO Fifth meeting of the Emergency Committee under the International
Health Regulations (2005) regarding microcephaly, other neurological disorders and Zika virus.
http://www.who.int/mediacentre/news/statements/2016/zika-fifth-ec/en/
(accessed July 6, 2017).Barry M.
The tail end of guinea worm: global eradication without a drug or a vaccine.
N Engl J Med. 2007;356:2561–2564GBD 2016 Risk Factors Collaborators Global, regional, and national
comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic
risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016.
Lancet. 2017;390:1345–1359Jensen ET, Cook SF, Allen JK.
Enrollment factors and bias of disease prevalence estimates in administrative claims data.
Ann Epidemiol. 2015;25:519–525.e2Kottke TE, Baechler CJ, Parker ED.
Accuracy of Heart Disease Prevalence Estimated from Claims Data Compared With an Electronic Health Record.
Prev Chronic Dis. 2012;9 DOI:10.5888/pcd9.120009Rothberg MB, Pekow PS, Priya A, Lindenauer PK.
Variation in Diagnostic Coding of Patients With Pneumonia and Its Association With Hospital
Risk-Standardized Mortality Rates: A Cross-sectional Analysis.
Ann Intern Med. 2014;160:380–388Yeom H, Kang DR, Cho SK, Lee SW, Shin D-H, Kim HC.
Admission route and use of invasive procedures during hospitalization for acute myocardial infarction:
analysis of 2007-2011 National Health Insurance database.
Epidemiol Health. 2015;37:e2015022Ghosh A, McCarthy S, Halcomb E.
Perceptions of primary care staff on a regional data quality intervention in Australian general practice:
a qualitative study.
BMC Fam Pract. 2016;17:50Pooled Resource Open-Access ALS Clinical Trials Database PRO-ACT -
Data Sets.
https://nctu.partners.org/ProACT/Data/Index/
(accessed May 3, 2017).Barber RM, Fullman N, Sorensen RJD.
Healthcare Access and Quality Index based on mortality from causes amenable to personal health care
in 195 countries and territories, 1990–2015: a novel analysis from the Global Burden of Disease Study 2015.
Lancet. 2017;390:231–266

Return to LOW BACK PAIN
Return to GLOBAL BURDEN OF DISEASE
Since 4-09-2018

| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |