

A Meta-analysis of Core Stability Exercise versus
General Exercise for Chronic Low Back PainThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: PLoS One. 2012 (Dec 17); 7 (12): e52082 ~ FULL TEXT
OPEN ACCESS Xue-Qiang Wang, Jie-Jiao Zheng, Zhuo-Wei Yu, 2 Xia Bi, Shu-Jie Lou, Jing Liu, et. al.
Department of Sport Rehabilitation,
Shanghai University of Sport,
Shanghai, China.
OBJECTIVE: To review the effects of core stability exercise or general exercise for patients with chronic low back pain (LBP).
SUMMARY OF BACKGROUND DATA: Exercise therapy appears to be effective at decreasing pain and improving function for patients with chronic LBP in practice guidelines. Core stability exercise is becoming increasingly popular for LBP. However, it is currently unknown whether core stability exercise produces more beneficial effects than general exercise in patients with chronic LBP.
METHODS: Published articles from 1970 to October 2011 were identified using electronic searches. For this meta-analysis, two reviewers independently selected relevant randomized controlled trials (RCTs) investigating core stability exercise versus general exercise for the treatment of patients with chronic LBP. Data were extracted independently by the same two individuals who selected the studies.
RESULTS: From the 28 potentially relevant trials, a total of 5 trials involving 414 participants were included in the current analysis. The pooling revealed that core stability exercise was better than general exercise for reducing pain [mean difference (–1.29); 95% confidence interval (–2.47, –0.11); P = 0.003] and disability [mean difference (–7.14); 95% confidence interval (–11.64, –2.65); P = 0.002] at the time of the short-term follow-up. However, no significant differences were observed between core stability exercise and general exercise in reducing pain at 6 months [mean difference (–0.50); 95% confidence interval (–1.36, 0.36); P = 0.26] and 12 months [mean difference (–0.32); 95% confidence interval (–0.87, 0.23); P = 0.25].
CONCLUSIONS: Compared to general exercise, core stability exercise is more effective in decreasing pain and may improve physical function in patients with chronic LBP in the short term. However, no significant long-term differences in pain severity were observed between patients who engaged in core stability exercise versus those who engaged in general exercise.
From the FULL TEXT Article:
Introduction
Low back pain (LBP) is one of the two most common types of disability affecting individuals in Western countries (the other is mental illness), and the assessment of LBP-related disabilities represents a significant challenge. [1] LBP affects approximately 80% of people at some stage in their lives. [2, 3] In developing countries, the 1–year prevalence of LBP among farmers was 72% in southwest Nigeria [4], 56% in Thailand [5], and 64% in China. [6] The impact of chronic LBP can be severe and profound because chronic LBP often results in lost wages and additional medical expenses and can even increase the risk of incurring other medical conditions. [7, 8] In the United States, the total indirect and direct costs due to LBP are estimated to be greater than $100 billion annually. [9, 10]
Exercise therapy seems to be an effective treatment to relieve the pain and to improve the functional status of patients with chronic LBP in most clinical practice guidelines. [11] Core stability training has become a popular fitness trend that has begun to be applied in rehabilitation programs and in sports medicine. [12] Many studies [13–15] have shown that core stability exercise is an important component of rehabilitation for LBP. Panjabi [16] proposed a well-known model of the spine stability system that consists of three subsystems: the passive subsystem (which includes bone, ligament and joint capsule), the active subsystem (which includes muscle and tendons), and the neural subsystem (which consists of the central nervous system and peripheral nervous system). According to this model, these three subsystems work together to provide stabilization by controlling spinal movement. Thus, an effective core stability exercise should consider the motor and sensory components of the exercise and how they relate to these systems to promote optimal spinal stability. [17] In addition, core stability training includes the exercise associated with the prior activation of the local trunk muscles and should be advanced to include more intricate static, dynamic, and functional exercises that involve the coordinated contraction of local and superficial spinal muscles.
Although there have been four published systematic reviews [18–21] of core stability training, these articles only include a review of the literature published prior to June 2008. Positive effects have been reported with different forms of exercise used by physical therapists. However, it is currently unclear whether core stability training produces more beneficial effects than conventional exercise for patients with chronic LBP.
Core stability training has a powerful theoretical foundation for the prevention and treatment of LBP, as is evidenced by its widespread clinical use. However, there appears to be no consensus agreement that core stability exercise is better than general exercise for chronic LBP. It is important to ensure that the determination of the most effective exercise for LBP is based on scientific evidence so as not to waste staff time and resources and to avoid unnecessary stress for patients with LBP and their families. The purpose of this paper is to conduct a meta-analysis of the effects of core stability exercise compared to general exercise as a treatment for chronic LBP.
Methods
Search Strategy
We identified randomized controlled trials (RCTs) by electronically searching the following databases: China Biology Medicine disc (1970–October 2011), PubMed (1970–October 2011), Embase (1970–October 2011), and the Cochrane Library (1970–October 2011).
A detailed explanation of the full electronic search strategy for PubMed is presented in Appendix S1. Briefly, the following medical subject headings (MeSH) were included: low back pain, sciatica, lumbosacral region, exercise, and chronic pain. The keywords used were RCTs, double-blind method, single-blind method, random allocation, pelvic girdle pain, motor control, exercise therapy, stability, stabilization, general exercise, traditional exercise, conventional exercise, specific exercise, and physical therapy. We removed duplicates that were identified in multiple database searches.
Inclusion Criteria
Types of studies Only RCTs examining the effects of core stability exercise versus general exercise for the treatment of patients with chronic LBP were included. No language or publication date limits were set.
Types of participants We included articles with both female and male subjects (over 18 years of age) who had chronic LBP (longer than 3 months). We excluded articles that included participants with LBP evoked by specific conditions or pathologies.
Types of interventions We included articles that compared a control group, which received general exercise, and a treatment group, which received core stability exercise training. A core stability training program could be described as the reinforcement of the ability to insure stability of the neutral spine position. [22] Core stability exercises were usually performed on labile devices, such as an air-filled disc, a low density mat, a wobble board, or a Swiss ball. [23]
Types of outcome measures The primary outcomes of interest were pain intensity, back-specific functional status, quality of life, and work absenteeism. Outcomes were recorded for three time periods [11]: long term (1 year or more), intermediate (6 months), and short term (less than 3 months).
Selection of Studies
Two reviewers (Wang XQ, Bi X) used the pre-specified criteria to screen for relevant titles, abstracts and full papers. An article was removed if it was determined not to meet the inclusion criteria. If these two reviewers reached different final selection decisions, a third reviewer (Zheng JJ) was consulted.
Data Extraction
We extracted the following data from the included articles: study design, subject information, description of interventions between the control and experimental group, follow-up period, and outcome measures. These data were then compiled into a standard table. The two reviewers who selected the appropriate studies also extracted the data and evaluated the risk of bias. It was necessary to consult an arbiter (Zheng JJ) to reconcile any disagreements.
Assessing the Risk of Bias
We used the Cochrane Collaboration recommendations [24] to assess the risk of bias for all articles. The following information was evaluated: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessments, incomplete outcome data, selective reporting and other bias. Two reviewers (Xu GH, Hua YH) evaluated the methodological quality of all articles examined in the current study. An arbiter was consulted (Chen PJ) to reconcile any disagreements.
Statistical Analysis
Review Manager Software (RevMan5.2) was used for the meta-analysis. Heterogeneity among the studies was evaluated using the I2 statistic and the chi-squared test. The fixed effects model was used if the heterogeneity test did not reveal statistical significance (I2<50%; P>0.1). Otherwise, we adopted the random effects model. We conducted a sensitivity analysis if heterogeneity existed among the studies. All of the variables in the studies included in this meta-analysis were continuous, so we used the mean difference (MD) and 95% confidence interval (CI) to analyze the studies. We considered P values less than 0.05 to be statistically significant.
Systematic review registration:
http://www.crd.york.ac.uk/PROSPERO. PROSPERO registration number: CRD42011001717.
Results
Search Results

Figure 1

Table 1

Table 2

Figure 2

Figure 3 The process of identifying eligible studies was outlined in Figure 1. Six hundred twenty-nine records were initially identified through the Cochrane Library, PubMed, Embase, and China Biology Medicine disc. Of these, 28 potentially eligible articles were included based on their title and abstract. After reviewing these 28 potential articles, only 5 articles [25, 29] fulfilled the inclusion criteria. The remaining 23 articles [30–52] were removed because the trials included participants with diagnoses other than chronic LBP, did not compare core stability exercise with general exercise, or the original data were not available from the authors. The characteristics of each included study are described in Table 1.
Risk of Bias of Included Studies
According to the Cochrane Collaboration recommendations, each article was at a high risk of bias. Thus, the evidence involved in this meta-analysis had a high overall risk of bias. Each article was described as randomized, but the randomization method was unclear for one study. [27] Four articles used the allocation concealment method, but we could not determine the allocation concealment in the Ottar 2010 article. [28] Three of the included articles attempted to blind the participants to the allocated treatment, and outcome assessors were blinded in five trials. Incomplete outcome data were at a low risk of bias in all articles. The risk of bias assessment of all included studies is described in Table 2.
Core Stability Exercise Versus General Exercise on Pain Intensity
In total, four trials assessed pain intensity using a numeric rating scale (NRS) and a visual analog scale (VAS). The data indicated that core stability exercise was better than general exercise for short-term pain relief when the results were combined in a random-effects model [MD (95% CI) = –1.29 (–2.47, –0.11), P = 0.003] [Figure 2(A)]. However, no significant differences were observed between the effects of core stability exercise and general exercise at 6 months [MD (95% CI) = –0.50 (–1.36, 0.36), P = 0.26] [Figure 2(B)] or 12 months [MD (95% CI) = –0.32 (–0.87, 0.23), P = 0.25] [Figure 2(C)].
Core Stability Exercise Versus General Exercise on Disability
Five studies included self-reported back-specific functional status. Of these, one used the Roland Morris Disability Questionnaire (RMDQ), and four used the Oswestry Disability Index (ODI). Compared to general exercise, core stability exercise resulted in a significant improvement in functional status by the random-effects model in the short term [MD (95% CI) = –7.14 (–11.64, –2.65), P = 0.002] (Figure 3).
Discussion
This meta-analysis, which included 414 patients, identified 5 RCTs that compared core stability exercise and general exercise for chronic LBP. The risk of bias was assessed for each article using the Cochrane Collaboration recommendations. In addition, each article contained a high risk of other bias. And it was difficult to evaluate whether the articles described the outcome measures they had originally meant to describe. However, no serious complications were reported in any of the five articles that investigated adverse events. However, the number of included subjects was too small to determine the safety of core stability exercise.
The results of this meta-analysis indicate that core stability exercise is better than general exercise for pain relief and improving back-specific functional status in the short term. However, no significant differences in pain relief were observed in the intermediate- and long-term follow-up periods. The primary results of this review are consistent with the findings of a systematic review [20] of the effects of core stability exercise on nonspecific LBP. The results of the meta-analysis indicated that core stability exercise can be more effective than other types of exercise in improving back-specific functional status in the short term (MD = –5.1points, 95% CI = –8.7 to 1.4). Two other systematic reviews [18, 19] also reported that specific stabilization exercise was better than ordinary medical care and treatment by a general practitioner for reducing pain over the short term and intermediate term.
Compared to the prior reviews, approximately four-fifths of the articles included in the current study were new, and all of the articles in the current analysis considered only patients with chronic LBP (duration of pain >12 weeks). In addition, we conducted a meta-analysis of the effects of core stability exercise compared to general exercise. Because of these characteristics, this meta-analysis is considered to be much more robust.
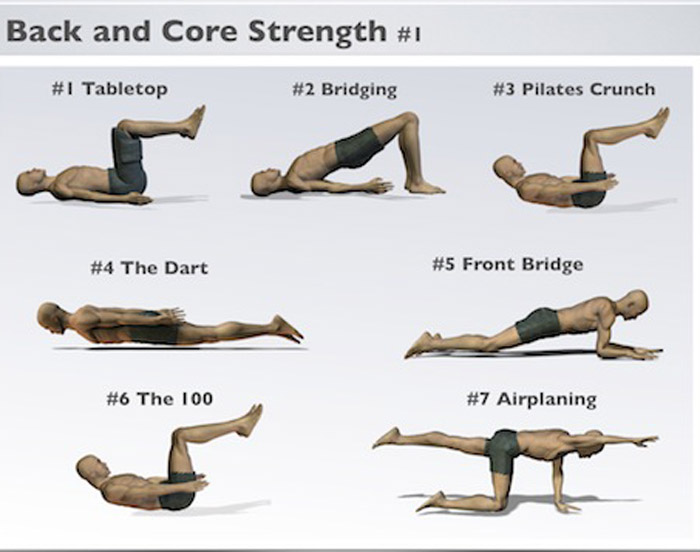
Core stability is the ability to control the position and movement of the central portion of the body. [53] Popular fitness programs, such as Tai Chi, Yoga, and Pilates, are based on core stability exercise principles. There are several different approaches currently in use for core stability exercise for LBP, which could lead to different results. A systematic review and meta-analysis of different core stability exercises for LBP should be conducted to determine the optimal treatment approach.
Limitations
This meta-analysis was characterized by several limitations that should be noted. The first limitation, which is common in many systematic reviews, was that the findings were based on relatively low quality data that had a high risk of bias. Although several of the articles involved in this meta-analysis were published within the last five years, methodologically rigorous articles were still deficient. Second, the total number of subjects involved in the meta-analysis was too small to identify relatively small disparities between the effects of core stability exercise and general exercise. A third limitation was that numerous articles did not contain sufficient information for evaluating the quality and clinical relevance of the data. Another limitation was the probability of publication bias, which we attempted to diminish via a substantial database search. However, unpublished articles were not searched. Finally, it would have been preferable to conduct multiple outcome measures between the compared treatments in this meta-analysis. However, the primary outcome measures evaluated in the majority of articles were pain intensity and back-specific functional status. Relatively few articles had a significant analysis of quality of life, global improvement, and return to work/absenteeism.
Implications for Practice
In comparison to general exercise, core stability exercise may be more effective in relieving pain and improving back-specific function for patients with chronic LBP in the short term. However, no significant differences were observed between core stability exercise and general exercise in pain and functional status in the long term. However, these conclusions are sustained by low-quality data, and more definitive articles are required to confirm these results.
Implications for Research
Articles that were methodologically sound and sufficiently powered are required to confirm the effects of core stability exercise on pain relief and functional improvements in patients with chronic LBP. The types of outcomes in articles should include proprioception, muscle strength and trunk endurance to provide insight into the potential mechanisms of cooperative action. Comparisons of different core stability exercises would be more reasonable. The effects of core stability exercise should be evaluated over the long term. Eventually, theories regarding the mechanisms by which core stability exercise relieves pain in patients with LBP should be explored further.
Supporting Information
MEDLINE search strategy
PRISMA 2009 ChecklistAcknowledgments
We would like to thank American Journal Experts for English language editing.
Funding Statement
This work was supported by the Shanghai Key Lab of Human Performance (SUS) (11DZ2261100); the National Science Foundation for Young Scholars of China (Grant No.81101391); the Science and Technology Foundation Program of Shanghai University of Sport (Grant No. YJSCX201120), and the Science and Technology Development Fund of Shanghai Pudong (Grant No.PKJ2011-Y05. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References:
Katz RT (2001)
Impairment and disability rating in low back pain.
Phys Med Rehabil Clin N Am 12: 681–94Beith ID, Kemp A, Kenyon J, Prout M, Chestnut TJ (2011)
Identifying neuropathic back and leg pain: a cross-sectional study.
Pain 152: 1511–6Andersson GB (1999)
Epidemiological features of chronic low-back pain.
Lancet 354: 581–5Fabunmi AA, Aba SO, Odunaiya NA (2005)
Prevalence of low back pain among peasant farmers in a rural community in South West Nigeria.
Afr J Med Med Sci 34: 259–62Barrero LH, Hsu YH, Terwedow H, Perry MJ, Dennerlein JT, et al. (2006)
Prevalence and physical determinants of low back pain in a rural Chinese population.
Spine (Phila Pa 1976) 31: 2728–34Taechasubamorn P, Nopkesorn T, Pannarunothai S (2011)
Prevalence of low back pain among rice farmers in a rural community in Thailand.
J Med Assoc Thai 94: 616–21Ivanova JI, Birnbaum HG, Schiller M, Kantor E, Johnstone BM, et al. (2011)
Real-world practice patterns, health-care utilization, and costs in patients with
low back pain: the long road to guideline-concordant care.
Spine J 11: 622–32Miller P, Kendrick D, Bentley E, Fielding K (2002)
Cost-effectiveness of lumbar spine radiography in primary care patients
with low back pain.
Spine (Phila Pa 1976) 27: 2291–7Frymoyer JW, Cats-Baril WL (1991)
An overview of the incidences and costs of low back pain.
Orthop Clin North Am 22: 263–71Crow WT, Willis DR (2009)
Estimating cost of care for patients with acute low back pain:
a retrospective review of patient records.
J Am Osteopath Assoc 109: 229–33Hayden JA, van Tulder MW, Malmivaara A, Koes BW (2005)
Exercise therapy for treatment of non-specific low back pain.
Cochrane Database Syst Rev CD000335Akuthota V, Ferreiro A, Moore T, Fredericson M (2008)
Core Stability Exercise Principles.
Curr Sports Med Rep 7: 39–44Desai I, Marshall PW (2010)
Acute effect of labile surfaces during core stability exercises in people with
and without low back pain.
J Electromyogr Kinesiol 20: 1155–62Baerga-Varela L, Abréu Ramos AM (2006)
Core strengthening exercises for low back pain.
Bol Asoc Med P R 98: 56–61Sung PS, Yoon B, Lee DC (2010)
Lumbar spine stability for subjects with and without low back pain during
one-leg standing test.
Spine (Phila Pa 1976) 35: E753–60Panjabi MM (1992)
The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis.
J Spinal Disord 5: 390–6Hodges PW (2003)
Core stability exercise in chronic low back pain.
Orthop Clin North Am 34: 245–54Ferreira PH, Ferreira ML, Maher CG, Herbert RD, Refshauge K (2006)
Specific stabilisation exercise for spinal and pelvic pain:
a systematic review.
Aust J Physiother 52: 79–88Rackwitz B, de Bie R, Limm H, von Garnier K, Ewert T, Stucki G (2006)
Segmental stabilizing exercises and low back pain. What is the evidence?
A systematic review of randomized controlled trials.
Clin Rehabil 20: 553–67Macedo LG, Maher CG, Latimer J, McAuley JH (2009)
Motor control exercise for persistent, nonspecific low back pain:
a systematic review.
Phys Ther 89: 9–25Hauggaard A, Persson A (2007)
Specific spinal stabilisation exercises in patients with low back pain:
a systematic review.
Phys Ther Rev 12: 233–248.Akuthota V, Ferreiro A, Moore T, Fredericson M (2008)
Core Stability Exercise Principles.
Curr Sports Med Rep 7: 39–44Willardson JM (2004)
The effectiveness of resistance exercises performed on unstable equipment.
Strength and Conditioning Journal 26: 70–74.Higgins JPT, Altman DG (2008)
Assessing risk of bias in included studies.
In: Higgins JPT, Green S, eds. Cochrane handbook for systematic reviews of interventions.
Wiley 187–241.Ferreira ML, Ferreira PH, Latimer J, et al.
Comparison of General Exercise, Motor Control Exercise and Spinal Manipulative Therapy
for Chronic Low Back Pain: A Randomized Trial
Pain. 2007 (Sep); 131 (1-2): 31–37Unsgaard-Tøndel M, Fladmark AM, Salvesen Ø, Vasseljen O (2010)
Motor control exercises, sling exercises, and general exercises for patients with
chronic low back pain: a randomized controlled trial with 1-year follow-up.
Phys Ther 90: 1426–40França FR, Burke TN, Hanada ES, Marques AP (2010)
Segmental stabilization and muscular strengthening in chronic low back pain:
a comparative study.
Clinics (Sao Paulo) 65: 1013–7Vasseljen O, Fladmark AM (2010)
Abdominal muscle contraction thickness and function after specific and general exercises:
a randomized controlled trial in chronic low back pain patients.
Man Ther 15: 482–9Tekur P, Singphow C, Nagendra HR, Raghuram N (2008)
Effect of short-term intensive yoga program on pain, functional disability and
spinal flexibility in chronic low back pain: a randomized control study.
J Altern Complement Med. 14: 637–44Koumantakis GA, Watson PJ, Oldham JA (2005)
Trunk muscle stabilization training plus general exercise versus general exercise
only: randomized controlled trial of patients with recurrent low back pain.
Phys Ther 85: 209–25Marshall PW, Murphy BA (2008)
Muscle activation changes after exercise rehabilitation for chronic low back pain.
Arch Phys Med Rehabil 89: 1305–13Kumar S, Sharma VP, Negi MP (2009)
Efficacy of dynamic muscular stabilization techniques (DMST) over conventional
techniques in rehabilitation of chronic low back pain.
J Strength Cond Res 23: 2651–9Cairns MC, Foster NE, Wright C (2006)
Randomized controlled trial of specific spinal stabilization exercises and
conventional physiotherapy for recurrent low back pain.
Spine (Phila Pa 1976) 2006 31: E670–81O'Sullivan PB, Phyty GD, Twomey LT, Allison GT (1997)
Evaluation of specific stabilizing exercise in the treatment of chronic low back pain
with radiologic diagnosis of spondylolysis or spondylolisthesis.
Spine (Phila Pa 1976) 22: 2959–67Stuge B, Laerum E, Kirkesola G, Vøllestad N (2004)
The efficacy of a treatment program focusing on specific stabilizing exercises
for pelvic girdle pain after pregnancy: a randomized controlled trial.
Spine (Phila Pa 1976) 29: 351–9Elden H, Ladfors L, Olsen MF, Ostgaard HC, Hagberg H (2005)
Effects of acupuncture and stabilising exercises as adjunct to standard treatment
in pregnant women with pelvic girdle pain: randomised single blind controlled trial.
BMJ 330: 761Stuge B, Veierød MB, Laerum E, Vøllestad N (2004)
The efficacy of a treatment program focusing on specific stabilizing exercises for
pelvic girdle pain after pregnancy: a two-year follow-up of a randomized clinical trial.
Spine (Phila Pa 1976) 29: E197–203Rasmussen-Barr E, Ang B, Arvidsson I, Nilsson-Wikmar L (2009)
Graded exercise for recurrent low-back pain: a randomized, controlled trial with
6-, 12-, and 36-month follow-ups.
Spine (Phila Pa 1976) 34: 221–8Kumar S, Negi MP, Sharma VP, Shukla R, Dev R, et al. (2009)
Efficacy of two multimodal treatments on physical strength of occupationally
subgrouped male with low back pain.
J Back Musculoskelet Rehabil 22: 179–88Sherman KJ, Cherkin DC, Cook AJ, Hawkes RJ, Deyo RA, et al. (2010)
Comparison of yoga versus stretching for chronic low back pain:
protocol for the Yoga Exercise Self-care (YES) trial.
Trials 11: 36Elden H, Ostgaard HC, Fagevik-Olsen M, Ladfors L, Hagberg H (2008)
Treatments of pelvic girdle pain in pregnant women: adverse effects of standard
treatment, acupuncture and stabilising exercises on the pregnancy, mother,
delivery and the fetus/neonate.
BMC Complement Altern Med 8: 34Macedo LG, Latimer J, Maher CG, Hodges PW, Nicholas M, et al. (2008)
Motor control or graded activity exercises for chronic low back pain?
A randomised controlled trial.
BMC Musculoskelet Disord 9: 65Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA (2005)
Comparing yoga, exercise, and a self-care book for chronic low back pain:
a randomized, controlled trial.
Ann Intern Med 143: 849–56Kluge J, Hall D, Louw Q, Theron G, Grové D (2011)
Specific exercises to treat pregnancy-related low back pain in a South African population.
Int J Gynaecol Obstet 113: 187–91Mohseni-Bandpei MA, Rahmani N, Behtash H, Karimloo M (2011)
The effect of pelvic floor muscle exercise on women with chronic
non-specific low back pain.
J Bodyw Mov Ther 15: 75–81Koumantakis GA, Watson PJ, Oldham JA (2005)
Supplementation of general endurance exercise with stabilisation training versus
general exercise only. Physiological and functional outcomes of a randomised
controlled trial of patients with recurrent low back pain.
Clin Biomech (Bristol, Avon) 20: 474–82Bentsen H, Lindgärde F, Manthorpe R (1997)
The effect of dynamic strength back exercise and/or a home training program in
57-year-old women with chronic low back pain. Results of a prospective
randomized study with a 3-year follow-up period.
Spine (Phila Pa 1976) 22: 1494–500Schenkman ML, Jordan S, Akuthota V, Roman M, Kohrt WM, et al. (2009)
Functional movement training for recurrent low back pain: lessons from a pilot
randomized controlled trial.
PM R 1: 137–46Ewert T, Limm H, Wessels T, Rackwitz B, von Garnier K, et al. (2009)
The comparative effectiveness of a multimodal program versus exercise alone for the
secondary prevention of chronic low back pain and disability.
PM R 1: 798–808Kumar S, Sharma VP, Shukla R, Dev R (2010)
Comparative efficacy of two multimodal treatments on male and female sub-groups
with low back pain (part II)
J Back Musculoskelet Rehabil. 23: 1–9Wang Xueqiang, Zheng Jiejiao, Bi Xia, Liu Jing (2012)
Effect of core stability training on patients with chronic low back pain.
HealthMED 6: 754–759.Guo Xianfeng, Yuan Shuaixiao, Li Xu (2010)
Sling exercise therapy on back pain of adults with idiopathic scoliosis.
Chin J Rehabil Theory Pract 16: 716–719.Omkar SN, Vishwas S, Tech B (2009)
Yoga techniques as a means of core stability training.
J Bodyw Mov Ther 13: 98–103
Return to LOW BACK PAIN
Return to EXERCISE AND CHIROPRACTIC
Since 4-30-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |