

Spinal Manipulative Therapy in Older Adults
with Chronic Low Back Pain: An Individual
Participant Data Meta-analysisThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: European Spine Journal 2022 (Jul); 31 (7): 1821–1845 ~ FULL TEXT
OPEN ACCESS Alan Jenks • Annemarie de Zoete • Maurits van Tulder
Sidney M Rubinstein • International IPD-SMT group
Faculty of Science,
Department of Health Sciences,
Vrije Universiteit,
Gebouw MF, Flexruimte,
Van der Boechorststraat 7,
1081 BT, Amsterdam,
The Netherlands.

Purpose: Many systematic reviews have reported on the effectiveness of spinal manipulative therapy (SMT) for low back pain (LBP) in adults. Much less is known about the older population regarding the effects of SMT.
Objective: To assess the effects of SMT on pain and function in older adults with chronic LBP in an individual participant data (IPD) meta-analysis.
Setting: Electronic databases from 2000 until June 2020, and reference lists of eligible trials and related reviews.
Design and subjects: Randomized controlled trials (RCTs) which examined the effects of SMT in adults with chronic LBP compared to interventions recommended in international LBP guidelines.
Methods: Authors of trials eligible for our IPD meta-analysis were contacted to share data. Two review authors conducted a risk of bias assessment. Primary results were examined in a one-stage mixed model, and a two-stage analysis was conducted in order to confirm findings.
Main outcomes and measures: Pain and functional status examined at 4, 13, 26, and 52 weeks.
Results: 10 studies were retrieved, including 786 individuals, of which 261 were between 65 and 91 years of age. There is moderate-quality evidence that SMT results in similar outcomes at 4 weeks (pain: mean difference [MD] – 2.56, 95% confidence interval [CI] – 5.78 to 0.66; functional status: standardized mean difference [SMD] – 0.18, 95% CI – 0.41 to 0.05). Second-stage and sensitivity analysis confirmed these findings.
Conclusion: Spinal manipulative therapy (SMT) provides similar outcomes to recommended interventions for pain and functional status in the older adult with chronic LBP. SMT should be considered a treatment for this patient population.
Keywords: Individual participant data; Low back pain; Older adult; Spinal manipulative therapy.
From the FULL TEXT Article:
Purpose
Low back pain (LBP) is one of the leading causes of disability and a lower quality of life in older adults. [1] It is one of the top three reasons why this population group visits a general practitioner. [2] The prevalence and burden of LBP increase with age [3], yet little is known about the effectiveness of interventions for LBP in older adults. [1]
Older adults with LBP are underrepresented in randomized controlled trials (RCTs) [4], and LBP remains ubiquitous among older adults in retirement. [5] Studies have demonstrated that LBP in older adults often lasts longer than 3 months [6] and is usually undertreated or mismanaged. [7]
Older adults tend to have more than one illness, and the odds of having LBP are higher in older adults with multiple comorbidities. [8] Therefore, it is important to identify treatment options which are safe and effective for this population. [9] Guidelines advocate non-pharmacological treatments for LBP, such as complementary health approaches. [10] Finding safe and effective treatments for the older adult with LBP should be a priority. One such non-pharmacological approach is spinal manipulative therapy (SMT), which is a technique used worldwide by a variety of healthcare providers, such as chiropractors, osteopaths, and physiotherapists.
Many systematic reviews and meta-analyses have analyzed the effects of SMT. [11] Their results suggest that it is an effective intervention for both the reduction in pain and the improvement in function, two of the core domains in LBP trials. [12] Systematic reviews examining the effectiveness of various non-pharmacological treatments in older adults with LBP [13, 14] identified only three studies that assessed the effect of SMT. Two of the three trials were included in this analysis, and the third trial was excluded due to average age below 55. Therefore, it is difficult to draw valid conclusions for this patient population due to the lack of trials.
Given this, one approach to examine the effectiveness of SMT in older adults with LBP is to perform individual participant data (IPD) meta-analysis. This type of analysis has distinct advantages over traditional aggregate meta-analysis. In an IPD meta-analysis, we can select certain individuals since we have the individual data for each participant. This is more efficient than setting up new trials, particularly if the data are sufficient in order to allow for a meaningful analysis. Additional advantages of IPD include allowing the investigator to analyze the data independently of how the data were reported in the original publication. This is in contrast to the traditional aggregate approach in which meta-analyses extract data at the study level, meaning that the author(s) of the review must rely on how the data were analyzed and presented originally. Additionally, IPD makes it possible to correct for baseline covariates which may influence the results, enabling a more precise, and thereby potentially more valid, calculation of the effect estimates. [15]
In short, LBP is a common cause of disability in the older adult [16], and our current knowledge of LBP in this patient group is limited. [17] The objective of this IPD meta-analysis is to assess the effectiveness of SMT versus interventions recommended by the guidelines at 1–, 3–, 6– and 12–month follow-up in older adults with chronic LBP.
Methods
This study was conducted according to the Preferred Reporting Items of Systematic Reviews and Meta-Analyses for IPD (PRISMA-IPD) guidelines [18] (Appendix 1).
IPD database
A detailed description of the IPD database design and the procedures followed was published previously. [19] The protocol [19] for the original study upon which this analysis is based was registered with PROSPERO (https://www.crd.york.ac.uk/prospero/25714). The database includes the raw data from 21 RCTs, which were published between 2000 and April 2018 [11], examining the effects of SMT on chronic LBP. This study used the IPD database defined above and represents a secondary analysis as defined a priori in PROSPERO. We updated the search from April 2018 to June 2020 identifying one trial that met our inclusion criteria. [20]
Study selection
Trials examining the effects of SMT versus recommended therapies in the older age-group with chronic low back pain were included.
Inclusion criteria: Patients with chronic LBP with or without leg pain, defined as LBP of > 12 weeks of duration and not attributable to a recognizable, known specific pathology (e.g., infection, fracture, tumor, radicular syndrome, or herniation) were included. Additionally, trials from primary or secondary care settings were included. When a mixed population was involved (e.g., subacute and chronic), only those participants with > 12 weeks of LBP were included. For this IPD meta-analysis, we selected only those trials that had included participants aged 55 and older.
Exclusion criteria: Studies were excluded if they: (1) used an inadequate randomization procedure (e.g., alternate allocation, allocation based on birth date); (2) included patients with LBP and other conditions, such as pregnancy or postoperative patients; (3) tested the immediate effect of a single treatment only; (4) compared the effects of a multimodal therapy including SMT to another therapy or any other study design whereby the contribution of SMT could not be isolated; and (5) included patients where there was a contraindication to SMT.
Types of interventions
Experimental intervention: Spinal manipulation (i.e., high-velocity low-amplitude [HVLA] techniques) and mobilization (i.e., low-velocity low-amplitude [LVLA] techniques) were defined as SMT.
Comparison: We addressed the effects on pain and functional status of SMT versus interventions (e.g., exercise therapy, usual care) that are consistently recommended in international guidelines [21–24], while SMT is not. [25] The determination for recommended therapy was based on Rubinstein et al. [11] We categorized an intervention into ‘recommended’ when this was consistently stated in at least two of the guidelines.
Types of outcome measures
Primary outcomes were pain and back-specific functional status, as recommended in the core set of outcome measurements in LBP. [12]
Data extraction and quality assessmentRisk of bias assessment The 13 risks of bias criteria recommended by the Cochrane Back and Neck group were used [26] (Appendix 2). These 13 criteria are used to identify selection bias, performance bias, attrition bias, detection bias, and selective outcome reporting bias.
Data extracted were study characteristics, patient characteristics, types of outcomes, duration of follow-up, and descriptions of experimental and control interventions.
Preparing data for analyses The original data were compared with the published data to check for completeness. All variables were then harmonized in a data harmonization platform developed for a previous IPD analysis. [27]
All outcomes were pooled following a decision rule (Appendix 3). All pain scores were converted to a pain scale (range 0–100 where a higher score indicates more pain) following a decision rule. To allow pooling of different functional status measures, we recoded the individual scores into Z-scores for each separate time point using pooled standard deviations as the nominator
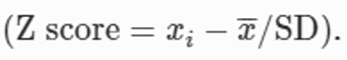
Analyzing these Z-scores resulted in standardized mean differences (SMDs). To ease interpretation of SMDs, we converted these to a mean difference (MD) for the 24–point Roland Morris Disability Questionnaire (RMDQ), by multiplying the SMD with the population standard deviation (SD) of the studies measuring
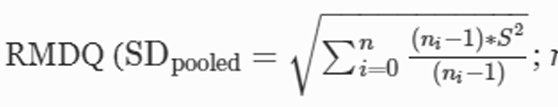
ni = sample size for each trial;
S = standard deviation for each trial).
Data analysis and synthesis All analyses were based on the intention-to-treat principle. Our primary analyses consisted of one-stage IPD meta-analysis at 4, 13, 26, and 52 weeks of follow-up. We chose these specific intervals as they are standard follow-up moments in the treatment of LBP. [11] We did not examine the effects of SMT post-intervention as there were large inter-study variations in the number and frequency of treatments and, consequently, the duration of therapies and follow-up data for the period immediately following the end of treatment. Lastly, longitudinal analyses were not performed as the models are too complex and do not converge.
Analyses were conducted using a random-effects model that was adjusted for baseline using the restricted maximum likelihood (REML) method, where a separate intercept and a separate residual variance for each study are specified. However, in most analyses, these models did not demonstrate convergence. Instead, we present the results adjusted for baseline and with a random intercept and common residual variance. [28]
The pooled treatment effects of SMT were estimated with a mean difference or Z-score for continuous outcomes, including the 95% confidence interval (CI).
Sensitivity and subgroup analyses In order to examine whether the RCTs included in this IPD meta-analysis were a representative sample of all RCTs assessing the effects of SMT in older adult patients, we conducted a two-stage sensitivity analysis wherein we examined the effect sizes of RCTs both included in this IPD meta-analysis and those which were eligible for inclusion, but for which no IPD were available. For the latter, we used published aggregate data of those eligible trials that had an average age above 55.
A post hoc sensitivity analysis was performed as the one-stage and two-stage estimates at 4 weeks for the outcome pain were not similar.
Lastly, we performed a moderator analysis for age. Age was dichotomized into 55–64 and 65 years and older. This moderator was analyzed using a one-stage random-effect IPD meta-analysis or get rid of ‘a’ before one-stage. The baseline outcome, treatment, age, and interaction between treatment and age were included as fixed effects. Study-specific intercepts were also included as fixed effects. Random treatment and interaction effects were added to the model. We performed these analyses for each time point and age separately to facilitate convergence of models. Centering the patient-level covariates about their study-specific means enabled us to separate the within- and across-study interactions. [28] The within-study interaction explained the patient-level variation in treatment response, while the across-study interaction represented the age effect on study level. We present the within-study interactions. A negative interaction coefficient indicates a more positive or less negative estimate of the intervention effects of SMT vs comparison for the group 65 years and older compared to 55–64 years old.
We refrained from presenting stratified results for subgroups of moderator variables, because these included a combination of within- and across-study information due to differences in proportions of persons within the separate subgroups between studies.
Synthesis of evidence The overall quality of the evidence for each outcome was evaluated using the GRADE approach [29] (Appendix 4), and assessment of clinical relevance was defined as small, medium, or large effect. [26, 30] Results from meta-epidemiological studies suggest that selection bias (i.e., randomization) and performance bias (i.e., blinding) are perhaps the more important forms of bias which influence treatment effects [31]; therefore, we focused on these two aspects when considering ‘limitations’ as part of the GRADE process.
Results

Tables &
FiguresIn total, of the 21 trials in the IPD database, ten RCTs met the inclusion criteria, all of which provided data for the primary analysis [32–41] (Table 1) (Figure 1). One trial [42] that did not provide data and had an average age above 55 was used in the second-stage analysis. In total, 786 participants aged ≥ 55 years were examined (403 were randomized to the spinal manipulative therapy (SMT) group and 383 were randomized to the comparison group) (Table 2). Two studies [20, 42] fit the inclusion criteria but did not provide individual data. (Table 3) Their aggregate published results were used in the two-stage analyses (Table 4) as they had an average age above 55. We identified 261 participants (from a total 786) older than 65 years of age originating from seven studies [32–37, 40], representing a third of all cases. Of the 261 patients, three quarters of them came from three studies [33, 34, 36] and were evenly distributed between treatment arms.
Description of studies
Of the ten RCTs, nine compared SMT to exercise therapy [32–39, 41] and one evaluated the effects of SMT compared to standard medical care [40] (consisting of drug and non-drug therapies). The included trials varied with respect to recruitment method, type of SMT technique, number and duration of treatments, and type of practitioner (Table 1).
Sample sizes ranged from 5 to 220 (median = 78.6; interquartile range [IQR] = 16–132). It should be noted that some trials had multiple arms, and some included non-chronic LBP patients; therefore, the sample size for a given comparison should be considered to be smaller.
The patient characteristics at baseline for SMT versus recommended interventions are presented in Table 2. The average age of all participants was 63 years (standard deviation [SD] 6.7), and slightly more than half (58.4%) were women.
Risk of bias
Approximately 80% of the studies (n = 8/10) reported an adequate random sequence generation and allocation concealment. [32, 33, 35, 36, 38, 40, 41] Two trials provided an adequate overview of withdrawals or dropouts and were able to keep these to a minimum for the subsequent follow-up measurements. [34, 40]
Missing data for primary outcomes ranged from 12% at 4 weeks to 21% at 52 weeks.
Effects of SMT vs recommended interventions Pain and function improved by the end of treatment, and this improvement was sustained up to 12 months after randomization for all groups (Table 3).
One-stage analysisPain There is moderate quality evidence that SMT has similar benefits to recommended interventions at all time points for pain (Table 3). The mean difference (MD) for SMT compared to recommended interventions is – 2.56 (95% CI – 5.78 to 0.66; scale 0–100) after 1 month, and these effects appear similar over the subsequent 12 months (Table 4). Further analysis on the group of patients 65 and older showed similar effects – 2.46 (95% CI – 7.41 to 2.48; scale 0–100) after 1 month and appear similar over the subsequent 12 months (Appendix 5).
Functional status There is moderate quality evidence that SMT has similar benefits to recommended interventions at all time points for functional status (Table 3). The comparison of SMT and recommended interventions for functional status outcome demonstrated a SMD of – 0.18 (95% CI – 0.41. to 0.05; scale 0–100) (– 0.85 on RMDQ 24–point scale) after 1 month and remained similar over the subsequent 12 months (SMD – 0.15; 95% CI – 0.38 to 0.08; scale 0–100) (– 0.76 on RMDQ 24–point scale) (Table 3). Further analysis on the group of patients 65 and older showed similar effects – 0.32 (95% CI – 0.57 to – 0.08; scale 0–100) (– 0.79 on RMDQ 24–point scale) after 1 month and appear similar over the subsequent 12 months – 0.40 (95% CI – 0.77 to – 0.02) (– 0.73 on RMDQ 24–point scale) (Appendix 5).
Sensitivity analyses and subgroup analysis We identified two trials to be included in the two-stage analysis, one from the original systematic review [42] and the other from our updated search. [20] We included the aggregate results of these studies in the second-stage analysis after going through a risk of bias assessment. The two-stage analysis showed a MD similar to the one-stage analysis except for pain at 4 weeks (Table 4). The difference at 4 weeks was a result of two studies that included 5 patients, yet had a large effect on recommended therapies. The second-stage analysis confirmed the results of the one-stage analysis at all time points, showing robustness of the effect in both analyses (Appendix 5). A subgroup analysis using age as a moderator showed similar results to a previous IPD [43], that age does moderate any effect of the treatment (Appendix 5) (Tables 5 and 6).
Discussion
These results suggest that spinal manipulative therapy (SMT) has similar effects to recommended interventions, mainly exercise therapy, at the short, intermediate, and long term. This is the first IPD meta-analysis to examine the effects of SMT in older adults with LBP, although admittedly, the majority of subjects (two-thirds) were between 55 and 65 years of age; therefore, these results should perhaps be interpreted with caution. However, if there were big differences in effects, this might have become intuitively obvious from this subgroup analysis. [43, 44] Using age as a moderator also did not change the effects at all time points. The importance of these findings cannot be sufficiently underscored. Given the growing aging population and the burden of LBP, there is a need to provide safe, conservative treatments. These data provide support for the use of SMT in this population.
These findings have important implications. The recent Lancet series [45] suggests that SMT should be considered a second treatment option, following the more commonly recommended treatments for chronic LBP (e.g., exercise). Our results suggest that SMT produces similar effects to other commonly recommended interventions for older patients with LBP. This is particularly pertinent because prior to this analysis, these effects were unclear. However, a note of caution is perhaps necessary because we did not examine adverse reactions in detail. These data were not registered in any systematic way in the individual studies and were not directly available; therefore, uncommon and potentially serious adverse reactions cannot be ruled out.
Importantly, our results appear consistent with recent systematic reviews using aggregate data on the effects of SMT for adults with LBP [11] as well as older adults. [13, 14] An important difference of our IPD analysis compared to traditional aggregate meta-analyses is that we could adjust for the baseline pain and functional status and were not dependent upon how these data were reported in the original publications. This adjustment increased the precision of our estimates compared to aggregate data meta-analyses, but did not lead to a different conclusion for the main effects.
Adverse events were often not reported by trial authors, and when reported there was no uniformity in how this was done, particularly for older patients; therefore, these data do not provide more information than the adverse events described in our systematic review of aggregate data. [11] The adverse events which were reported are likely to be more serious events for which reporting was required, or were unrelated to SMT. [20] Nevertheless, there may be a theoretically increased risk with SMT which would need to be examined in future studies and compared to recommendations like exercise therapy (e.g., osteoporosis). In short, the risk of (major) adverse events is likely to be very low and may reflect adaptation by the therapist for this patient population.
Strengths and weaknesses
These results should be interpreted in light of a few strengths and limitations. The most important strength is that we included 786 patients from ten trials in our analysis. Furthermore, these patients came from 10 of the 11 trials that could have provided data, which minimized selection bias. Additionally, all trials provided data for pain and functional status for all the time points analyzed; lastly, the one-stage estimates were confirmed by the two-stage analysis, suggesting that our effects estimates were robust.
Study limitations
There are, however, some important limitations. Inclusion bias cannot be ruled out. We may have missed some important studies published after 2018. In order to determine whether this might be the case, we performed a cursory search of the literature in PubMed (up to June 2020). We identified 18 potential articles. Upon further analysis, 17 were excluded for various reasons, including younger age, lack of randomization, a protocol, or other type of comparison (e.g., SMT as adjuvant therapy). In short, only one study fulfilled the inclusion criteria which could have been included in an update. We analyzed that trial [20] in the two-stage analysis, and those results were consistent with the one-stage analysis.
Additionally, selection bias cannot be ruled out; 11 of the 21 studies identified in the search did not provide IPD data. Of those, three included patients older than 55 [46–48], but relatively few subjects would have been included because the average age was under 55 (SDs ranged from 12 to 15). One [42] trial included subjects with an average age over 55 and was examined in our second-stage analysis. Again, those results were consistent with our one-stage analysis. This suggests that our analysis is representative of all subjects that could have been included and, therefore, robust.
Implications for clinicians
SMT appears to be similarly effective to recommended therapies for reducing pain and improving function in older patients with chronic LBP, meaning SMT may be delivered as a stand-alone therapy. Future research should focus on identifying which older adults are best suited for SMT, taking lifestyle factors, comorbidities, and level of physical activity into account.
Conclusion
Spinal manipulative therapy (SMT) is equally as effective as recommended interventions for the treatment of chronic low back pain in the older adult. Over three quarters of the data came from adults aged 55–64, yet sensitivity analysis in the second stage and using age as a moderator showed results were similar across all age-groups. Therefore, SMT should be considered a treatment option in this patient population.
Appendices
Acknowledgements
We thank Jen Walraven and Anne Jenks-Coupland for their advice in writing the article and correcting the English.
International IPD-SMT group: Bronfort G, Cecchi F, Ferreira ML, Gudavalli MR, Hidalgo B, Hondras MA, Hsieh CJ, Petersen T, Rasmussen-Barr E, Skillgate E, UK Beam Trial Team.
Funding
This individual patient data analysis was funded by a grant from the European Centre for Chiropractic Research Excellence. European Chiropractic Union Research Fund Contract No A.14.03. Systematic review registration: prospero-25714.
Contributions
SMR, MVT, and ADZ are members of the steering committee of LBP consortium. These authors contributed to the concept and design of the study. SMR, ADZ, and AJ gathered, pooled, and analyzed the data and drafted the manuscript. CF, BG, FML, GMR, HMA, HCJ, PT, R-E, SE, and Underwood are principal investigators of the randomized clinical trials from which the data are pooled for the current study, and have consequently contributed to the study concept, design, and conduct of the trial that they were responsible for. All authors critically reviewed the manuscript. All authors read and approved the final manuscript.
Conflict of interest
SMR, ADJ, and AdeZ work in clinical practice as chiropractors and treat older adults with chronic low back pain. SMR reports grants from European Chiropractor’s Union, grants from Netherlands Chiropractic Association, grants from Centre for Chiropractic Research Excellence, and grants from Belgian Chiropractic Association, during the conduct of the study.
Ethical approval
The study protocol was approved by the Scientific Review Board of the coordinating institution Vrije Universiteit Amsterdam and by the Ethical Committee of the VU University Medical Center Amsterdam. (Projectnr. 2015.544). Risk of bias assessment: Evaluation of the risk of bias was conducted by two independent reviewers (SMR, AdeZ). To adjudicate disagreement, a third reviewer (ADJ) was contacted.
References:
Wong AY, Karppinen J, Samartzis D (2017)
Low back pain in older adults: risk factors, management options and future directions.
Scoliosis Spinal Disord 12:14.
https://doi.org/10.1186/s13013-017-0121-3St Sauver JL, Warner DO, Yawn BP, Jacobson DJ, McGree ME, Pankratz JJ, et al (2013)
Why patients visit their doctors: assessing the most prevalent conditions in a defined American population.
Mayo Clin Proc 88:56–67.
https://doi.org/10.1016/j.mayocp.2012.08.020James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, et al (2018)
Global, regional, and national incidence, prevalence, and years lived with disability
for 354 diseases and injuries for 195 countries and territories, 1990–2017:
a systematic analysis for the Global Burden of Disease Study 2017.
Lancet 392:1789–1858.
https://doi.org/10.1016/s0140-6736(18)32279-7Paeck T, Ferreira ML, Sun C, Lin CW, Tiedemann A, Maher CG (2014)
Are older adults missing from low back pain clinical trials?
A systematic review and meta-analysis.
Arthritis Care Res (Hoboken) 66:1220–1226.
https://doi.org/10.1002/acr.22261Palacios-Cena D, Alonso-Blanco C, Hernandez-Barrera V, Carrasco-Garrido P (2015)
Prevalence of neck and low back pain in community-dwelling adults in Spain:
an updated population-based national study (2009/10-2011/12).
Eur Spine J 24:482–492.
https://doi.org/10.1007/s00586-014-3567-5Hartvigsen J, Frederiksen H, Christensen K (2006)
Back and Neck Pain in Seniors-Prevalence and Impact
European Spine Journal 2006 (Jun); 15 (6): 802–806American Geriatrics Society Panel on Pharmacological Management of Persistent Pain in Older Persons?
why is this repeated and where are the authors? (2009)
Pharmacological management of persistent pain in older persons.
J Am Geriatr Soc 57:1331–1346.
https://doi.org/10.1111/j.1532-5415.2009.02376.xStewart Williams J, Ng N, Peltzer K, Yawson A, Biritwum R, Maximova T (2015)
Risk factors and disability associated with low back pain in older adults
in low- and middle-income countries. Results from the WHO study on Global
AGEing and Adult Health (SAGE).
PLoS ONE 10:e0127880.
https://doi.org/10.1371/journal.pone.0127880Pohontsch NJ, Heser K, Loffler A, Haenisch B, Parker D, Luck T (2017)
General practitioners’ views on (long-term) prescription and use of problematic
and potentially inappropriate medication for oldest-old patients—
a qualitative interview study with GPs (CIM-TRIAD study).
BMC Fam Pract 18:22.
https://doi.org/10.1186/s12875-017-0595-3Sibbritt DWAJ (2010)
Back pain amongst 8910 young Australian women: a longitudinal analysis of the use
of conventional providers, complementary and alternative medicine (CAM)
practitioners and self-prescribed CAM.
Clin rheumatol. https://doi.org/10.1007/s10067-009-1299-4Rubinstein SM, De Zoete A, Van Middelkoop M, Assendelft WJJ, De Boer MR, Van Tulder MW.
Benefits and Harms of Spinal Manipulative Therapy for the Treatment of
Chronic Low Back Pain: Systematic Review and Meta-analysis
of Randomised Controlled Trials
British Medical Journal 2019 (Mar 13); 364: l689Chiarotto A, Deyo RA, Terwee CB, Boers M, Buchbinder R, Corbin TP, Costa LO (2015)
Core outcome domains for clinical trials in non-specific low back pain.
Eur Spine J 24:1127–1142.
https://doi.org/10.1007/s00586-015-3892-3Nascimento P, Costa LOP, Araujo AC, Poitras S, Bilodeau M (2019)
Effectiveness of interventions for non-specific low back pain in older adults.
A systematic review and meta-analysis.
Physiotherapy 105:147–162.
https://doi.org/10.1016/j.physio.2018.11.004Amaral LKB, Souza MB, Campos MGM, Mendonca VA, Bastone A, Pereira LSM (2020)
Efficacy of conservative therapy in older people with nonspecific low back pain:
a systematic review with meta-analysis and GRADE recommendations.
Arch Gerontol Geriatr 90:104177.
https://doi.org/10.1016/j.archger.2020.104177Tierney JF, Vale C, Riley R, Smith CT, Stewart L, Clarke M, Rovers M (2015)
Individual participant data (IPD) meta-analyses of randomised controlled trials:
guidance on their use.
PLoS Med 12:e1001855.
https://doi.org/10.1371/journal.pmed.1001855Prince MJ, Wu F, Guo Y, Gutierrez Robledo LM, O’Donnell M, Sullivan R (2015)
The Burden of Disease in Older People and Implications
for Health Policy and Practice
Lancet 2015 (Feb 7); 385 (9967): 549–562Jenks AD, Hoekstra T, Axen I, de Luca K, Field J, Newell D, Hartvigsen J (2020)
Back Complaints in the Elders - Chiropractic (BACE-C):
Protocol of an International Cohort Study of Older
Adults with Low Back Pain Seeking Chiropractic Care
Chiropractic & Manual Therapies 2020 (Apr 1); 28 (1): 17Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, Stewart G (2015)
Preferred reporting items for systematic review and meta-analyses
of individual participant data: the PRISMA-IPD statement.
JAMA 313:1657–1665.
https://doi.org/10.1001/jama.2015.3656de Zoete A, de Boer MR, van Tulder MW, Rubinstein SM, Underwood M, Hayden JA (2017)
Rationale and design of an individual participant data meta-analysis of
spinal manipulative therapy for chronic low back pain-a protocol.
Syst Rev 6:21.
https://doi.org/10.1186/s13643-017-0413-ySchulz C, Evans R, Maiers M, Schulz K, Leininger B, Bronfort G (2019)
Spinal Manipulative Therapy and Exercise for Older Adults
with Chronic Low Back Pain: A Randomized Clinical Trial
Chiropractic & Manual Therapies 2019 (May 15); 27: 21Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Bernstein IA, Malik Q, Carville S, Ward S (2017)
Low back pain and sciatica: summary of NICE guidance.
BMJ 356:i6748.
https://doi.org/10.1136/bmj.i6748Bons SCS, Borg MAJP, Van den Donk M, Koes BW, Kuijpers T, Ostelo RWJG (2017)
NHG-Standaard Aspecifieke lagerugpijn.
Huisarts Wet 60(2):54–84Cost B (2006)
European guidelines for the management of low back pain.
Eur Spine J 15:s125–s127.
https://doi.org/10.1007/s00586-006-1066-zFoster NE, Anema JR, Cherkin D, Chou R, Cohen SP, et al.
Prevention and Treatment of Low Back Pain:
Evidence, Challenges, and Promising Directions
Lancet. 2018 (Jun 9); 391 (10137): 2368–2383
This is the third of 4 articles in the remarkable Lancet Series on Low Back PainFurlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, Bronfort G (2015)
2015 Updated method guideline for systematic reviews in the Cochrane back and neck group.
Spine 40:1660–1673.
https://doi.org/10.1097/BRS.0000000000001061Kalter J, Sweegers MG, Verdonck-de Leeuw IM, Brug J, Buffart LM (2019)
Development and use of a flexible data harmonization platform to facilitate the
harmonization of individual patient data for meta-analyses.
BMC Res Notes 12:164.
https://doi.org/10.1186/s13104-019-4210-7Riley RD, Lambert PC, Abo-Zaid G (2010)
Meta-analysis of individual participant data: rationale, conduct, and reporting.
BMJ 340:c221.
https://doi.org/10.1136/bmj.c221Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2019)
Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019).
CochraneJ. C (1988)
Statistical power analysis for the behavioral sciences.
https://doi.org/10.4324/9780203771587Savovic J, Turner RM, Mawdsley D, Jones HE, Beynon R, Higgins JPT (2018)
Association between risk-of-bias assessments and results of randomized trials
in cochrane reviews: the ROBES meta-epidemiologic study.
Am J Epidemiol 187:1113–1122.
https://doi.org/10.1093/aje/kwx344Bronfort G, Maiers MJ, Evans RL, Schulz CA, Bracha Y, Svendsen KH (2011)
Supervised Exercise, Spinal Manipulation, and Home Exercise
for Chronic Low Back Pain: A Randomized Clinical Trial
Spine J. 2011 (Jul); 11 (7): 585–598Cecchi, F., Molino-Lova, R., Chiti, M. et al.
Spinal Manipulation Compared with Back School and with Individually Delivered
Physiotherapy for the Treatment of Chronic Low Back Pain:
A Randomized Trial with One-year Follow-up
Clinical Rehabilitation 2010 (Jan); 24 (1): 26–36Ferreira ML, Ferreira PH, Latimer J, Herbert RD, Hodges PW, Jennings MD (2007)
Comparison of general exercise, motor control exercise and spinal manipulative therapy
for chronic low back pain: a randomized trial.
Pain 131:31–37.
https://doi.org/10.1016/j.pain.2006.12.008Gudavalli MR, Cambron JA, McGregor M, Jedlicka J, Keenum M, Ghanayem AJ (2006)
A randomized clinical trial and subgroup analysis to compare flexion-distraction
with active exercise for chronic low back pain.
Eur Spine J 15:1070–1082.
https://doi.org/10.1007/s00586-005-0021-8Hondras MA, Long CR, Cao Y, et al.
A Randomized Controlled Trial Comparing 2 Types of Spinal Manipulation
and Minimal Conservative Medical Care for Adults 55 Years and Older
With Subacute or Chronic Low Back Pain
J Manipulative Physiol Ther. 2009 (Jun); 32 (5): 330–343Hsieh CY, Adams AH, Tobis J, Hong CZ, Danielson C, Platt K, Hoehler F, Reinsch S, Rubel A (2002)
Effectiveness of four conservative treatments for subacute low back pain:
a randomized clinical trial.
Spine 27:1142–1148Petersen T, Larsen K, Nordsteen J, Olsen S, Fournier G, Jacobsen S.
The McKenzie Method Compared with Manipulation When Used
Adjunctive to Information and Advice in Low Back Pain Patients
Presenting with Centralization or Peripheralization:
A Randomized Controlled Trial
Spine (Phila Pa 1976) 2011 (Nov 15); 36 (24): 1999-2010Rasmussen-Barr E, Nilsson-Wikmar L, Arvidsson I (2003)
Stabilizing training compared with manual treatment in sub-acute and chronic low-back pain.
Man Ther 8:233–241.
https://doi.org/10.1016/s1356-689x(03)00053-5Skillgate E, Vingard E, Alfredsson L (2007)
Naprapathic manual therapy or evidence-based care for back and neck pain:
a randomized, controlled trial.
Clin J Pain 23:431–439.
https://doi.org/10.1097/AJP.0b013e31805593d8Underwood M, UK BEAM Trial Team.
United Kingdom Back Pain Exercise and Manipulation (UK BEAM) Randomized Trial:
Effectiveness of Physical Treatments for Back Pain in Primary Care
British Medical Journal 2004 (Dec 11); 329 (7479): 1377–1384Dougherty PE, Karuza J, Dunn AS, Savino D, Katz P (2014)
Spinal Manipulative Therapy for Chronic Lower Back Pain in Older Veterans:
A Prospective, Randomized, Placebo-Controlled Trial
Geriatric Orthopaedic Surgery and Rehab. 2014 (Dec); 5 (4): 54–164de Zoete A, Rubinstein SM, de Boer MR, Ostelo R, Underwood M, Hayden JA (2021)
The Effect of Spinal Manipulative Therapy on Pain Relief and Function
in Patients with Chronic Low Back Pain: An Individual
Participant Data Meta-analysis
Physiotherapy 2021 (Mar 17); 112: 121–134Hee SW, Mistry D, Friede T, Lamb SE, Stallard N, Underwood M, Patel S (2021)
Identification of subgroup effect with an individual participant data meta-analysis
of randomised controlled trials of three different types of therapist-delivered care in low back pain.
BMC Musculoskelet Disord 22:191.
https://doi.org/10.1186/s12891-021-04028-8Buchbinder R, Underwood M, Hartvigsen J, Maher CG (2020)
The Lancet Series Call to Action to Reduce Low Value Care
for Low Back Pain: An Update
Pain. 2020 (Sep); 161 (1): S57–S64Cook CLK, Showalter C, Kabbaz V, O’Halloran B (2013)
Early use of thrust manipulation versus non-thrust manipulation: a randomized clinical trial.
Man Ther 18:191–198.
https://doi.org/10.1016/j.math.2012.08.005Wilkey AGM, Byfield D, McCarthy PW (2008)
A Comparison Between Chiropractic Management and Pain Clinic Management
for Chronic Low-back Pain in a National Health Service Outpatient Clinic
J Alternative and Complementary Med 2008 (Jun); 14 (5): 465–473Hidalgo BPL, Hall T, Detrembleur C, Nielens H (2015)
Short-term effects of Mulligan mobilization with movement on pain, disability,
and kinematic spinal movements in patients with nonspecific low back pain:
a randomized placebo-controlled trial.
J Manip Physiol Ther 38:365–374. https://doi.org/10.1016/j.jmpt.2015.06.013

Return to MEDICARE
Return to LOW BACK PAIN
Since 6-02-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |