Stability: From Biomechanical Concept to Chiropractic Practice This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Can Chiropr Assoc 1999 (Jun); 43 (2): 75–88 ~ FULL TEXT
OPEN ACCESS Stuart M McGill, PhD
Faculty of Applied Health Sciences,
Department of Kinesiology,
University of Waterloo,
Waterloo, Ontario, Canada N2L 3G1.
This paper formalizes stability in a clinician-friendly way and then discusses waysfor chiropractors to ensure stability ofspinaljoints that may have their stability compromized from manipulation.
KEY WORDS: lumbar stability, chiropractic, exercise, manipulation.
From the FULL TEXT Article:
Introduction
The purpose of this paper is to develop a scientific foundation and formalize the notion of stability as it pertains to the spine, and then discuss some implications of stability for advancing spine rehabilitation and clinical practice. The intention was to write a reader-friendly synthesis where only minimal references were provided. This invited review will complement my last review written for this journal 10 years ago. Over the intervening time we have established the UW-CMCC Chiropractic Research Clinic and have been conducting research with CMCC researchers. While we have been investigating the biomechanical effects of manipulation, we will need to perform additional experiments to provide a synthesis of sufficient utility for chiropractic practice. Look forward to this report in another couple of years.
A major theme developed here pertains to the stability of spinal joints which are directly affected by chiropractic treatment. Can chiropractors be more effective at stabilizing a joint with exercise after they have decreased its stability with manipulation - and if so, how?
On stability: the foundation
Ask ten different clinicians to define stability and chances are there will be ten different responses. Much progress has been made recently on the formulation and operationalization of stability in musculoskeletal linkages and joints. These concepts are now being employed in the clinic and have resulted in enhanced rehabilitation outcome together with more biomechanically justifiable injury prevention strategies. This section shall formalize the notion of stability from a spine perspective.
During the late 1980's, Anders Bergmark, a professor of solid mechanics at the University of Lund in Sweden, very elegantly formalized stability in a muscular system using a very simplistic model of the spine. [1] With an extremely simplified linkage, and only a few muscles, he was able to formalize mathematically, the concepts of "energy wells", stiffness, stability and instability. For the most part, this classic work went unrecognized largely because the engineers who understood the mechanics did not have the biological - clinical perspective, while the clinicians were unable to interpret the engineering-mechanics. This pioneering work, together with embellishment by several others will be synthesized here. The following forms a brief tutorial for clinicians to understand the mechanical formulation, and implications of stability for musculoskeletal examples.
First, one must understand the concept of potential energy, which for the purposes here, comprise two basic forms. In the first form, objects have potential energy by virtue of their height above a datum. An apple has potential energy while still on the tree since this energy will be transformed into kinetic energy if it were to fall.PE = m*g*h

Figure 1 In the second form, elastic bodies may possess potential energy by virtue of their elastic deformation under load, storing potential energy which is then recovered when the load is removed - such as what would happen when loading and unloading any elastic band. Let's begin with the first form of potential energy to describe the notions of energy wells and minimum potential energy. If we place the ball into a bowl it is stable. We know this because if one were to apply a force to the ball (or a perturbation) the ball will rise up the side of the bowl but then come to rest again in the position of least potential energy - or the bottom of the bowl. We can make this system more stable by deepening the bowl and/or by increasing the steepness of the sides of the bowl (see Figure 1). Conversely, a ball placed on a flat surface or at the top of hill (an upside down bowl) is unstable since any perturbation would cause the ball to roll away. So one can see that the objective in creating stability with this analogy is to create a bowl shaped potential energy surface or an energy well. The ball will seek the position ofminimum potential energy (or mass times gravity times height - height being the variable to minimize). This corresponds to a stable situation. Thus, the notion of stability requires the specification of the unperturbed state of a system followed by study of the system following perturbation, which in turn indicates the stability of the perturbed state.
The previous analogy is a two dimensional example. This would be analogous to a hinged skeletal joint that only has the capacity for flexion/extension. Some ball and socket joints can rotate in three planes requiring a 4 dimensional bowl. Obviously, this is a theoretical bowl since a real bowl has only 3 dimensions - mathematics allows us to examine a 15 dimensional bowl. If one were to decrease the height of the bowl in any one of these 15 dimensions, the ball would roll out. In clinical terms, a single muscle force having an inappropriate magnitude will cause instability.
Having understood these analogies incorporating potential energy by virtue of height, we can now consider potential energy as a function of stiffness and storage of the elastic energy, which is much more useful for musculoskeletal application. Elastic potential energy can be calculated from the formula:PE = 1/2*k*x2

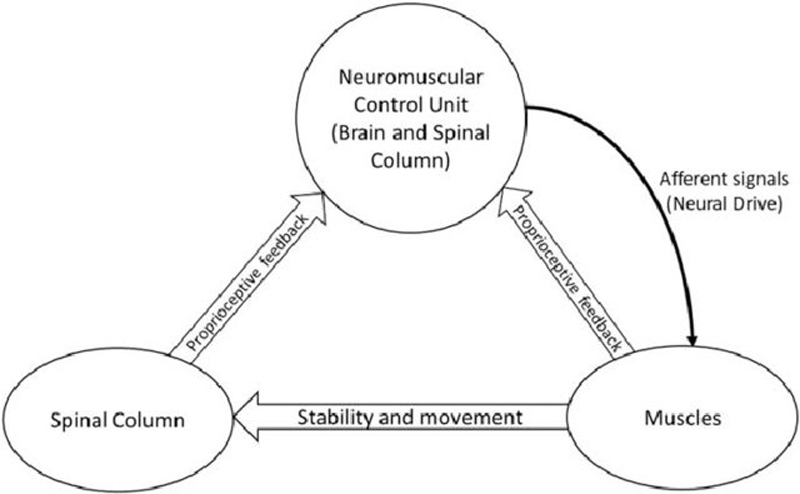
Figure 2 In other words the greater the stiffness (k) the greater the steepness of the sides of the bowl (from the previous analogy), and the more stable the structure. Thus stiffness creates stability (see Figure 2). Active muscle, produces a stiff member and in fact the greater the activation of the muscle the greater this stiffness. Furthermore, joints possess inherent joint stiffness, ligaments contribute stiffness in different ranges of motion. Nonetheless the motor control system is able to control stability of the joints through intentional muscle activation and to a lesser degree by placing joints in positions which modulate passive stiffness contribution. A faulty motor control system leads to inappropriate magnitudes of muscle force, and stiffness, allowing a "valley" for the "ball to roll out" or, for ajoint to buckle or undergo shear translation.
In a complex system such as the lumbar spine one must analyze the bowl which will have many dimensions - 6 dimensions or degrees of freedom per joint (3 rotational and 3 translational) multiplied by the number of joints chosen for the analysis. This is done by forming a matrix where each dimension is represented by a number (or eiganvalue) and the magnitude of that number represents its contribution to forming the height of the bowl in that particular dimension. One then simply scans the matrix for eigenvalues less than zero indicating instability, and furthermore, by observing the eigenvector can then identify the mode in which the instability occurred.

Figure 3 The next concept that clinicians must understand is the link between muscle activation and stiffness. Activating a muscle increases stiffness, both within the muscle and to the joint(s). Activating a group of muscle synergists and antagonists in the optimal way now becomes a critical issue. From a motor control point of view, we often use the analogy of an orchestra - we must get the orchestra to play together, or in clinical terms we must get the full complement of the stabilizing musculature to work together to achieve stability. One instrument out of tune ruins the sound - one muscle with inappropriate activation amplitude can produce instability, or at least unstable behaviour will result at lower applied loads. Figure 3 shows a few of the stabilizers of the spine which we appreciate to be very architecturally complex.
Clinicians are very aware of patients who co-contract in order to stabilize a joint - this type of behavior makes sense and in fact it is the only way to stabilize a joint. However the clinical question then becomes how much stability is necessary - obviously insufficient stiffness will not achieve the necessary stability for the joint but on the other hand too much stiffness and co-activation imposes massive load penalties on the joints and skeletal system. We must now develop the concept of "sufficient stability".
In order for a joint to bear larger loads, more stability is required. However, in most situations only a modest amount of stability is required to stabilize the joint. Too much stiffness from muscle activation imposes a severe load penalty on the joint, and would over-stiffen the joint impeding motion. In normal joints, with fit motor control systems, appropriate stability is achieved. Individual joints have passive stiffness. If the joint is not at the end range and passive tissues cannot create a mechanical stop to motion, the joint will most likely be unstable without additional muscular stiffness. The role of the motor system is to add stiffness required to make the joint stable. Post injury, the motor system has been documented to loose its fitness and it chooses abnormal muscle activation sequences. Furthermore, the passive stiffnesses are disturbed decreasing the force required for unrestricted rotations and translations. The Biomechanist's contribution is to quantify the loss of passive tissue stiffness and determine how much muscular stiffness is necessary for stability. Once this amount of stability is determined, the clinician will then wish to add a modest amount of extra stability to form a margin of safety, and this is known as "sufficient stability".
The stability concept is revolutionizing rehabilitation. New insight into the pathogenesis of injury is obtained - we are now able to explain how people can sustain a back injury picking up a pencil. In this situation, the general demand of the task is relatively low, muscular forces are low, and stiffness is low. If the motor system committed a small error in activation sequence and/or muscle magnitudes resulting in a temporary loss of stiffness, in a single mode from a single muscle, instability could result. [2] In other words, the ball would roll through the side of the bowl formed by the contributions of the particular muscle stiffness (bowl sides are created by systems of muscles, not only single muscles that contribute to the particular direction of joint motion). The resulting rotation and/or translation at the joint overloads a passive tissue to the point of damage. In fact we observed such an instability on videoflouroscope records in a single spine motion segment that resulted in injury. [3] We are also beginning to provide clinicians with specific target levels of activation in order to achieve sufficient stability.
Interestingly enough, large muscular forces are rarely required. Rather low levels of activation are required for long periods of time. In our recent paper, [4] stabilization exercises were quantified and ranked for muscle activation magnitudes together with the resultant spine load. Furthermore, Cholewicki and McGill, [5] and Cholewicki et al. [6] have demonstrated that sufficient stability of the lumbar spine is achieved, for a neutral spine, in most people with modest levels of coactivation of the abdominal wall. This means that a patient must be able to maintain sufficient stability getting on off the toilet, in and out of the car, up and downstairs etc. The amount of "Sufficient stability" over these types of tasks depends on the health of the joints and their passive stiffness profiles.
This argument suggests that the margin of safety when performing tasks, particularly the tasks of daily living, is not compromised by insufficient strength but rather insufficient endurance. We are now beginning to understand the mechanistic pathway of those studies showing the efficacy of endurance training vs. strength for the muscles that stabilize the spine. Having strong abdominals do not provide the prophylactic effect that had been hoped for - but recent work suggests that endurable muscles reduce the risk of future back troubles (e.g. [7]).
Joint stability and chiropractic practice
Stiffness, and stability, of a spinal motion segment is due to both muscle stiffness and the inherent passive stiffness of the joint. Chiropractors attempt to identify spinal segments that are not moving correctly, or are "blocked" or "stiff'. Interestingly enough, stiffjoints are, by definition, quite stable or would require a very large perturbation to become unstable. The goal of manipulation is to restore more normal motion, but more motion means less joint stiffness and stability. This may increase the need for more stability from muscular sources. Furthermore, there may be a peril in overmanipulation producing too much motion, which compromises stability and can produce another set of concerns.
In my opinion, some chiropractors are lagging in the practice and prescription of stabilization exercises for their patients. While some progressive chiropractors have employed stabilization programs for their patients, many manipulate without due consideration of enhancing spine stability through exercises specifically designed to increase the effectiveness of the motor control system to activate the stiffening muscular "guy wires". The next section is designed to assist the chiropractor in prescribing optimal stabilizing exercises.
Exercise for the low back: general concepts
A lot of the notions that clinicians consider to be principles for exercise prescription may not be as well supported with data as one may think. For example, we have all heard to perform sit ups with bent knees. Why? Further, many clinicians emphasize performing a pelvic tilt when performing many types of low back exercise. What is the scientific evidence for such a recommendation? An examination of the literature will reveal that the scientific foundation upon which many exercise notions are based is extremely thin. Rather "clinical wisdom" appears to prevail and, in fact, dominates the decision process when choosing the most appropriate exercise for an individual situation. This observation is not intended to belittle clinical wisdom but rather to emphasize that choosing an optimal exercise challenge requires the blend of "clinical art" and "science". The foundation for specific exercises will be briefly developed here. Chiropractors interested in more detail should consult the American College of Sports Medicine textbook [8] in which I was asked to develop a program emphasizing enhancement of stabilizing motor patterns and muscle endurance performance.
The traditional objective of most exercise prescription is to stress both damaged tissue and other healthy supporting tissues to foster tissue repair, while avoiding further excessive loading which can exacerbate an existing structural weakness. However, a relatively recent development is to meet these objectives, while also enhancing the ability of the motor control system to optimize stability. Furthermore, certain types of low back injuries are characterized by very specific tissue damage which may require quite different exercise rehabilitation programs for different people. For example, the posterior herniated disc would do well to avoid full spine flexion manoeuvres, particularly with concomitant muscle activity causing significant compressive loading since this is a potent way to herniate the annulus. Yet this spine posture is often unknowingly adopted by patients or consciously advocated by clinicians who demand a full pelvic tilt! Consider an example that addresses the- mechanically unstable spine which may be associated with a musculature and motor control system that is very "unfit" whereby the individual makes all sorts of inappropriate muscle activation sequences (cf. [9]).
It is well documented that, following injury, the motor system loses its ability to optimally sequence motor patterns to muscles. These motor control "errors" appear to lead to brief spine buckling situations and a high risk of injury. [5] It is imperative that clinicians understand what are the stabilizers of the spine - and what is the safest, and most effective way to train them. While an entire textbook could be written to describe ideal exercise programs for the entire population including chronic low back pain sufferers, children, men and women of all ages, through to elite athletes, the focus of the exercises discussed here is on developing the safest exercise for enhancing stability and the daily maintenance of low back health that is of utility for the chiropractic office.
Instability as a cause of injury
The ability of the joints of the lumbar spine to bend in any direction is accomplished with large amounts of muscle cocontraction. Such coactivation patterns are counterproductive to generating the torque necessary to support the applied load in a way that minimizes the load penalty imposed on the spine from muscle cocontraction. In fact a ligamentous spine will fail under compressive loading at about 20 Newtons in a buckling mode. [10] From the first section of this paper, the reader understands that muscle activity around the spine acts like the rigging on a ship's mast, and while the spine ultimately experiences more compression it is able to bear a much higher compressive load as it stiffens and becomes more resistant to buckling. A number of years ago we were investigating the mechanics of powerlifter spines while they lifted extremely heavy loads using video fluoroscopy viewing the sagittal plane. We happened to film and record one injury. The view of the powerlifter spines was calibrated for full flexion by first asking them to flex at the waist and hang the upper body against gravity with no load in the hands.
During their lifts, even though they outwardly appeared to fully flex their spines in fact their spines were two to three degrees per joint from full flexion, thus explaining how they could lift magnificent loads without sustaining injury which we suspect is linked with full flexion. However, one lifter dropped the weight and complained about pain (apparently injured). Upon examination of the video fluoroscopy records a local instability was noted: specifically only at L3 /L4 where this joint approached the full flexion calibrated angle and exceeded it by one-half a degree, while all other joints maintained their static positions. [3] This is the first observation reported in the scientific literature documenting the presence of a local instability occurring at a single lumbar joint that we know of. This motivated the work of my former graduate student Dr. Jacek Cholewicki, now a professor at Yale University, to first define mathematically lumbar stability and then continuously quantify stability of the lumbar spine throughout a reasonably wide variety of loading tasks.
Generally speaking it appears that the spine is most prone to instability failure when the loading demands are low and the major muscles are not activated to high levels. (In the case of the powerlifter the loading was extreme). Nonetheless it appears that the chance of the motor control error which results in a short and temporary reduction in activation, to one of the intersegmental muscles would cause rotation of just a single joint to a point where passive or other tissues become irritated or possibly injured. In fact at this point it is interesting to discuss the very small intersegmental muscles, the rotators and intransversarri. There is evidence to suggest that these muscles are highly rich in muscle spindles (at least four to seven times higher than multifidus). [11] It would seem that these organs are not functioning to produce force given their minimal cross sectional area, but are rather position transducers for each lumbar joint enabling the motor control system to control overall lumbar posture and avoid injury. Once again these findings are relevant to those responsible for injury management and exercise prescription - spine stability and motor control issues appear to be important considerations.
Toward developing the stabilization program - more evidence
Choosing the best exercise requires evidence on tissue loading and on the knowledge of how injury occurs to specific tissues (described in [12-14]). The ideal exercise will challenge muscle, impose minimal joint loads to spare the spine, and do this in a way that enhances joint stability in a neutral posture, and that requires additional elements of whole body stabilization. The following section addresses certain selected exercise issues beginning with an example to illustrate the need for quantitative analysis for evaluating the safety of certain exercises.
Situps with bent knees?
We have all been aware of the principle to perform situps and other flexion exercises with the knees and hips flexed. Several hypotheses have suggested that this disables the psoas and/or changes the line of action of psoas to reduce the low back compressive load. Recent MRI based data [15] demonstrated that the psoas line of action does not change due to lumbar or hip posture (except at L5/S 1) as the psoas laminae attach to each vertebrae and "follow" the changing orientation of spine, not of the hip or knees. There is no doubt that psoas is shortened with the flexed hip, modulating force production. But the question remains, is there a reduction in spine load with the legs bent? Recently McGill [16] examined 12 young men, with the laboratory technique described previously, and observed no major difference in lumbar load as the result of bending the knees (average moment of 65 Nm in both straight and bent knees, Compression: 3230N-straight legs, 3410N-bent knees; Shear: 260N-straight legs, 300N-bent knees). Compressive loads in excess of 3000N certainly raises questions of safety for some patients. This type of quantitative analysis is necessary to demonstrate that the issue of performing situps using bent knees or straight legs is probably not as important as the issue of whether to prescribe situps at all!
The pelvic tilt
Many clinicians universally recommend performing a pelvic tilt when prescribing exercise. One what evidence? Flexing the spine consistent with the "pelvic tilt", preloads the annulus and posterior ligaments [17] which appears to be associated with an increase in the risk of injury. Therefore a "neutral" spine (neutral lordosis) is emphasized to reduce the risk of injury while the spine is under load - neither hyperlordotic or hypolordotic. A general rule of thumb is to preserve the normal low back curve (similar to that of upright standing) or some variation of this posture that minimizes pain. While in the past performing a "pelvic tilt" when exercising has been recommended, this is not justified as the "pelvic tilt" increases spine tissue loading as the spine is no longer in staticelastic equilibrium, in fact the "pelvic tilt" preloads the spine - it would appear to be unwise to recommend the "pelvic tilt" when challenging the spine.
Issues of flexibility
The amount of emphasis on spine flexibility depends on the person's injury history, exercise goal, etc. Generally, for the back injured, spine flexibility should not be emphasized until the spine has stabilized and has undergone strength and endurance conditioning - some may never reach this stage! Despite the notion held by some, there is little quantitative data to support a major emphasis on trunk flexibility to improve back health and lessen the risk of injury. In fact some exercise programs that have included loading of the torso throughout the range of motion (in flexion-extension, lateral bend, or axial twist) have had negative results (cf [18, 19]) and greater spine mobility has been, in some cases, associated with low back trouble (cf [20, 21]). Furthermore spine flexibility has been shown to have little predictive value for future low back trouble. [20, 22] The most successful programs appear to emphasize trunk stabilization through exercise with a neutral spine (e.g. [23]) but emphasize mobility at the hips and knees (Bridger et al. [24] demonstrate mobility advantages for sitting and standing while McGill and Norman [25] outline advantages for lifting).
Issues ofstrength and endurance
While it is well documented that those with previous back injuries have lower muscle strength and endurance performance, very few studies (longitudinal) have linked reduced strength and endurance with the risk of a subsequent first time low back injury. The few studies available suggest that endurance has a much greater prophylactic value than strength. [7] Furthermore, it would appear that emphasis placed on endurance should precede specific strengthening exercise in a gradual progressive exercise program (i.e., longer duration, lower effort exercises).
Aerobic exercise
The mounting evidence supporting the role of aerobic exercise in both reducing the incidence of low back injury [26] and also in the treatment of low back patients [27] is compelling. Recent investigation into loads sustained by the low back tissues during walking [28] confirm very low levels of supporting passive tissue load coupled with mild, but prolonged, activation of the supporting musculature. Epidemiological evidence also sheds light on the effects of aerobic exercise. A large study [29] examined age related changes to the lumbar spines of elderly people as a function of life long activity level, those who were runners had no differences in spine changes measured from MRI images while weight lifters and soccer players were characterized with more disc degeneration and bulges.
The abdominals (anterior and lateral)
First, there is no single abdominal exercise that challenges all of the abdominal musculature - requiring the prescription of more than one single exercise. Calibrated intramuscular and surface EMG evidence [12, 14] suggests that the various types of curl-ups challenge mainly rectus abdominis as psoas and abdominal wall (internal and external oblique, transverse abdominis) activity is low. Situps (both straight-leg and bent-knee) are characterized by higher psoas activation and higher low back compression while leg raises cause even higher activation and also spine compression (the interested reader is directed to reference [14] for actual data).

Table 1 Several relevant observations were made regarding abdominal exercises in our investigations. The challenge to psoas is lowest during curl-ups, followed by higher levels during the horizontal isometric side support, while bent knee situps were characterized by larger psoas activation than straight leg situps, through to the highest psoas activity observed during leg raises and hand-on-knee flexor isometric exertions. It is interesting to note that the "pressheels" sit-up which has been hypothesized to activate hamstrings and neurally inhibit psoas, [30] actually increased psoas activation. Normalized electromyographic data in Table 1 is provided for comparative purposes. (We note here that some clinicans intentionally wish to train psoas and will find this data informative). One exercise not often performed, but that appears to have merit is the horizontal side support as it challenges the lateral obliques without high lumbar compressive loading. [14]
In addition this exercise produces high activation levels in quadratus lumborum which appears to be a significant stabilizer of the spine. [31] Graded activity in rectus abdominis and each of the components of the abdominal wall changes with each of these exercises demonstrating that there is no single best task for the collective "abdominals". Clearly, curl-ups excel at activating the rectus abdominis but produce relatively lower oblique activity. A very wise choice for abdominal exercises, in the early stages of training or rehabilitation, would consist of several variations of curl-ups for rectus abdominis and isometric horizontal side support (or side bridge), with the body supported by the knees and upper body supported by one elbow on the floor to challenge the abdominal wall in a way that imposes minimal compressive penalty to the spine. The level of challenge with the isometric, horizontal side support can be increased by supporting the body with the feet rather than the knees.
Quadratus lumborum and spine stabilization
Several other clinically relevant findings from these two data sets include notions that: psoas activation is really determined by hip flexion demands and that psoas activity is not consistent with either lumbar sagittal moment or spine compression demands - we question the often cited notion that psoas is a lumber spine stabilizer; quadratus lumborum activity is consistent with lumbar sagittal moment and compression demands suggesting a larger role in stabilization; in fact when compression is applied to the spine, in an upright posture with no bending moments, quadratus lumborum is the muscle whose activation is most closely related to the increasing need for stability more than any other torso muscle; [31] and psoas activation is relatively high (greater than 25% MVC) during pushups suggesting cautious prescription of this exercise for the low back injured. As noted in the previous section, the horizontal side support appears to be a wise choice of exercise for training quadratus lumborum for enhancing spine stability.
The back extensors

Table 2 Most traditional extensor exercises are characterized with high spine loads which result from externally applied compressive and shear forces (either from free weights or resistance machines). We have been searching for methods to activate the extensors with minimal spine loading. [13] It appears that the single leg extension hold, while on the hands and knees minimizes external loads on the spine but produces spine extensor moment (and small isometric twisting moments) which activates the extensors. Activation is sufficiently high on one side of the extensors to facilitate training but the total spine load is reduced since the contralateral extensors are producing lower forces (lumbar compression is less than 2500N) (see Table 2). Switching legs trains both sides of the extensors (one side of lumbar approximately 18% of MVC).
Simultaneous leg extension with contralateral arm raise ("birddog") increases the unilateral extensor muscle challenge (approximately 27% MVC in one side of lumbar extensors and 45% MVC in other side of thoracic extensors) but also increases lumbar compression to well over 3000N. The often performed exercise of laying prone on the floor and raising the upper body and legs off the floor is contraindicated for anyone at risk of low back injury - or re-injury. In this task the lumbar region pays a high compression penalty to a hyperextended spine (approximately 4000N) which transfers load to the facets and crushes the interspinous ligament (noted earlier as an injury mechanism). Once again, these data are provided for the exercise professional who must design programs for a wide range of objectives.
The beginner's program for stabilization

Figure 4

Figure 5
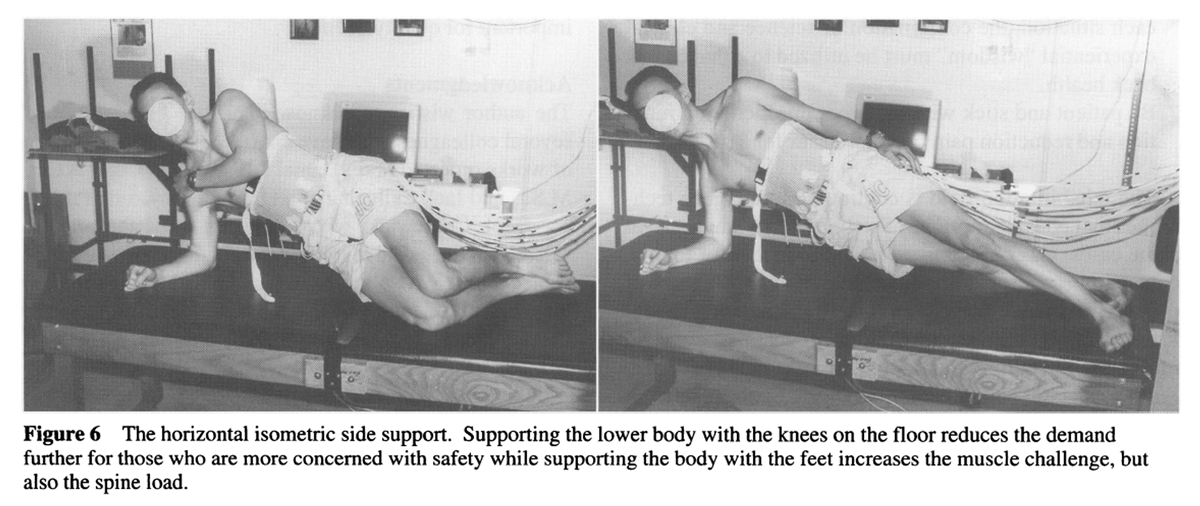
Figure 6

Figure 7 Specific recommended low back exercises have been shown. We recommend that the program begin with the flexion-extension cycles (Figure 4) to reduce spine viscosity, followed by hip and knee mobility exercises. We have found that 5-6 cycles is often sufficient to reduce most viscous stresses. This is followed by anterior abdominal exercises, in this case the curl-up with the hands under the lumbar spine to preserve a neutral spine posture (Figure 5) and one knee flexed but with the other leg straight to lock the pelvis-lumbar spine. Then, lateral musculature exercises are performed - namely isometric side support, or side bridge, for quadratus lumborum and the obliques of the abdominal wall for optimal stability (Figure 6). The upper leg-foot is placed in front of the lower leg-foot to facilitate longitudinal "rolling" of the torso to challenge both anterior and posterior portions of the wall. The extensor program consists of leg extensions and the "birddog" (Figure 7).
We have recently established "normal" ratios of endurance times for the torso flexors relative to the extensors (0.98) And for the lateral musculature relative to the extensors (0.73) [32] to assist clinicians to identify endurance deficits. Finally, as patients progress with these isometric stabilization exercises, we recommend conscious simultaneous contraction of the abdominals (hollowing - drawing the navel towards the spine) to enhance motor control and stability using the deeper abdominal wall (transverse abdominis and internal oblique) after Richardson et al. [33]
Some general caveats
While there is a common belief among some "experts" that exercise sessions should be performed at least 3 times per week, it appears low back exercises have the most beneficial effect when performed daily. [34]
The "no pain-no gain" axiom does not apply when exercising the low back, scientific and clinical wisdom would suggest the opposite is true.
While specific low back exercises have been rationalized in this chapter, general exercise programs that also combine cardiovascular components (like walking) have been shown to be more effective in both rehabilitation and for injury prevention. [27] The exercises shown here only focus on the stabilization component of the total program.
Diurnal variation in the fluid level of the intervertebral discs (discs are more hydrated early in the morning after rising from bed), changes the stresses on the disc throughout the day. It would be very unwise to perform full range spine motion while under load, shortly after rising from bed (e.g. 17).
Low back exercises performed for maintenance of health need not emphasize strength, with high-load low repetition tasks, rather more repetitions of less demanding exercises will assist in the enhancement of endurance and strength. There is no doubt that back injury can occur during seemingly low level demands (such as picking up a pencil) and that the risk of injury from motor control error can occur. While it appears that the chance of motor control errors, resulting in inappropriate muscle forces, increase with fatigue there is also evidence documenting the changes in passive tissue loading with fatiguing lifting. [35] Given that endurance has more protective value than strength, [7] strength gains should not be overemphasized at the expense of endurance.
There is no such thing as an ideal set of exercises for all individuals. For the specific case of chiropractors who wish to enhance spine stability following a manipulative regimen, we recommend the "Big 3" described here (in Figures 5, 6 and 7). In other situations, an individuals' training objectives must be identified, (be they rehabilitation, specifically to reduce the risk of injury, optimize general health and fitness, or maximize athletic performance), and the most appropriate exercises chosen. While science cannot evaluate the optimal exercises for each situation, the combination of science and clinical experiential "wisdom" must be utilized to enhance low back health.
Be patient and stick with the program. Increased function and reduction pain may not occur for 3 months. [36]
The rehabilitation field is continuing to embrace techniques that consider notions of stability. Past emphasis, in some cases, was on issues such the production of torque, enhancing range of motion etc. Fortunately, the laws of physics, and techniques of engineering, are being recognized by clinicians who can then ensure that first a system must be stable before presented with a physical challenge. Furthermore of particular importance to chiropractic, is the need to consider the role of stabilizing exercise when joint stability may be altered from treatment. We will continue our work to understand the contributions to stability of various components of the anatomy at particular joints - and the ideal ways to enhance their contribution; to understand what magnitudes of muscle activation are required to achieve sufficient stability; to identify the best methods to re-educate faulty motor control systems to both achieve sufficient stability and reduce the risk of inappropriate motor patters occurring in the future. Our challenge for the future, as clinicians like yourselves and scientists like myself, is to tackle in a collaborative and scientifically substantiated way, the pain and mobility problems that are so important for quality of life.
Acknowledgments
The author wishes to acknowledge the contributions of several colleagues who have contributed to the collection of works reported here: Daniel Juker, M.D., Craig Axler, M.Sc., and Jack Callaghan, Ph.D. and in particular Professor Jacek Cholewicki who I consider to be the premier scientist in the world regarding the engineering analysis of spine stability. Also the continual financial support from the Natural Science and Engineering Research Council, Canada has made this series of work possible.
References:
Bergmark A.
Stability of the lumbar spine: A study in mechanical engineering.
Acta Orthop Scand 1989; 60:3-53.2McGill SM.
Biomechanics of low back injury: Implications on current practice and the clinic.
J Biomech 1997; 30:465-475.Cholewicki J, McGill SM.
Lumbar posterior ligament involvement during extremely heavy lifts estimated from fluoroscopic measurements.
J Biomech 1992; 25(1): 17-28.McGill SM.
Low Back Exercises: Evidence for improving exercise regimens.
Physical Therapy, 78:754-765.Cholewicki J, McGill SM.
Mechanical stability of the in vivo lumbar spine: Implications for injury and chronic low back pain.
Clin Biomech 1996; 11(1):1-15.Cholewicki J, Panjabi MM, Khachatryan A.
Stabilizing function of trunk flexor-extensor muscles around a neutral spine posture.
Spine 1997; 22(19):2207-2212.Luoto S, Heliovaara M, Hurri H, Alaranta M.
Static back endurance and the risk of low back pain.
Clin Biomech 1995; 10(6):323-324.McGill SM.
Low back exercises: Prescription for the healthy back and when recovering from injury.
In: Resource manual for guidelines for exercise testing and prescription,
American College of Sports Medicine. 3rd ed.
Baltimore, Williams and Wilkins, 1998.McGill SM, Sharratt MT, Sequin JP.
Loads on spinal tissues during simultaneous lifting and ventilatory challenge.
Ergonomics 1995; 38:1772-1792.Lucas D, Bresler B.
Stability of the ligamentous spine.
Technical Report number 40, Biomechanics Laboratory,
San Francisco, University of California.Nitz AJ, Peck D.
Comparison of muscle spindle concentrations in large and small human epaxial muscles acting in parallel combinations.
The American Surgeon 1986; 12:273-277.Juker D, McGill SM, Kropf P, Steffen T.
Quantitative intramuscular myoelectric activity of lumbar portions of psoas and the abdominal wall during a wide variety of tasks. (In press)
Med Sci Sports Ex.Callaghan JP, Gunning JL, McGill SM.
Relationship between lumbar spine load and muscle activity during extensor exercises.
Physical Therapy 1998, 78:8-18.Axler CT, McGill SM.
Low back loads over a variety of abdominal exercises: Searching for the safest abdominal challenge.
Med Sci Sports and Exerc 1997; 29:804-811.Santaguida L, McGill SM.
The psoas major muscle: a three dimensional mechanical modelling study with respect to the spine based on MRI measurement.
J Biomech 1995; 128(3):339-345.McGill SM.
The mechanics of torso flexion: situps and standing dynamic flexion manoeuvres.
Clinical Biomechanics 1995; 10(4):184-192.Adams MA, Dolan P.
Recent advances in lumbar spine mechanics and their clinical significance.
Clin Biomech 1995; 10(1):3-19.Malmivaara A, Hakkinen U, Aro T, Heinrichs M, Koskenniemi L, Kuosma E, Lappi S, Hernberg S.
The treatment of acute low back pain - bed rest, exercises, or ordinary activity?
N Eng J Med 1995; 332:35 1.Nachemson A.
Newest knowledge of low back pain: a critical look.
Clin Orthop Rel Res 1992; 279:8-20.Biering-Sorensen F.
Physical measurements as risk indicators for low back trouble over a one year period.
Spine 1884; 9:106-119.Burton AK, Tillotson KM, Troup JDG.
Variation in lumbar sagittal mobility with low back trouble.
Spine 1989; 14(6):584-590.Battie MC, Bigos SJ, Fischer LD, Spengler DM, Hansson TH, Nachemson AL, Wortley MD.
The role of spinal flexibility in back pain complaints within industry: a prospective study.
Spine 1990; 15(8):768-773.Saal JA, Saal JS.
Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy: An Outcome Study.
Journal Missing 1989; 14(4):431-437.Bridger RS, Orkin-D, Henneberg M.
A quantitative investigation of lumbar and pelvic postures in standing and sitting: interrelationships with body position and hip muscle length.
Int J Ind Ergonomics 1992; 9:235-244.McGill SM, Norman RW.
Partitioning of the L4/L5 dynamic moment into disc, ligamentous, and muscular components during lifting.
Spine 1986; 11:666-667.Cady LD, Bischoff DP, O'Connel ER, Thomas PC, Allan JH.
Strength and fitness and subsequent back injuries in firefighters.
J Occup Med 1979; 21(4):269-272.Nutter P.
Aerobic exercise in the treatment and prevention of low back pain.
State Art Rev Occup Med 1988; 3:137-145.Callaghan JP, Patla A, McGill SM.
Low back three dimensional joint forces, kinematics and kinetics during walking.
Clin Biomech. 1999; in press.Videman T, Sarna S, Crites-Battie M, Koskinen S, Gill K, Paananen H, Gibbons L.
The long term effects of physical loading and exercise lifestyles on back-related symptoms, disability, and spinal pathology among men.
Spine 1995; 20(b):669-709.Spring H.
Kraft-Theorie und praxis.
1990. Thieme, Stuttgardt.McGill SM, Juker D, Kropf P.
Quantitative intramuscular myoelectric activity of quadratus lumborum during a wide variety of tasks.
Clin Biomech 1996; 11(3):170-172.McGill SM, Childs A, Leibenson C.
Endurance times for stabilization exercises: clinical targets for testing and training from a normal database.
Arch Phys Med Rehab 1999.Richardson C, Jull G, Toppenberg R, Comerford M.
Techniques for active lumbar stabilization for spinal protection: a pilot study
Australian Physiotherapy; 38(2): 105-112.Mayer TG, Gatchel RJ, Kishino N, Keeley J, Capra P, Mayer H, Barnett J, Mooney V.
Objective assessment of spine function following industrial injury: a prospective study with comparison group and one-year follow up.
Spine 1985; 10(6):482-493.Potvin JR, Norman RW. Can fatigue compromise lifting safety?
Proc. NACOB II, The Second North American Congress on Biomechanics, 1992;
August 24-28, pp.513-514.Manniche C, Hesselsoe G, Bentzen L, Christensen I, Lundberg E.
Clinical trial of intensive muscle training for chronic low back pain.
Lancet 1988; Dec. 24-31, pp.1473-1476.
Return to LOW BACK PAIN
Since 11-17-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |