

Long-Term Medicare Costs Associated with Opioid
Analgesic Therapy vs Spinal Manipulative Therapy
for Chronic Low Back Pain in a Cohort of Older AdultsThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2021 (Sep); 44 (7): 519-526 ~ FULL TEXT
James M. Whedon, DC, MSm Anupama Kizhakkeveettil, PhD Andrew Toler, MS,
Todd A. MacKenzie, PhD Jon D. Lurie, MD, MS Serena Bezdjian, PhD,
Scott Haldeman, DC, MD, PhD Eric Hurwitz, DC, PhD Ian Coulter, PhD
Health Services Research,
Southern California University of Health Sciences,
Whittier, California.
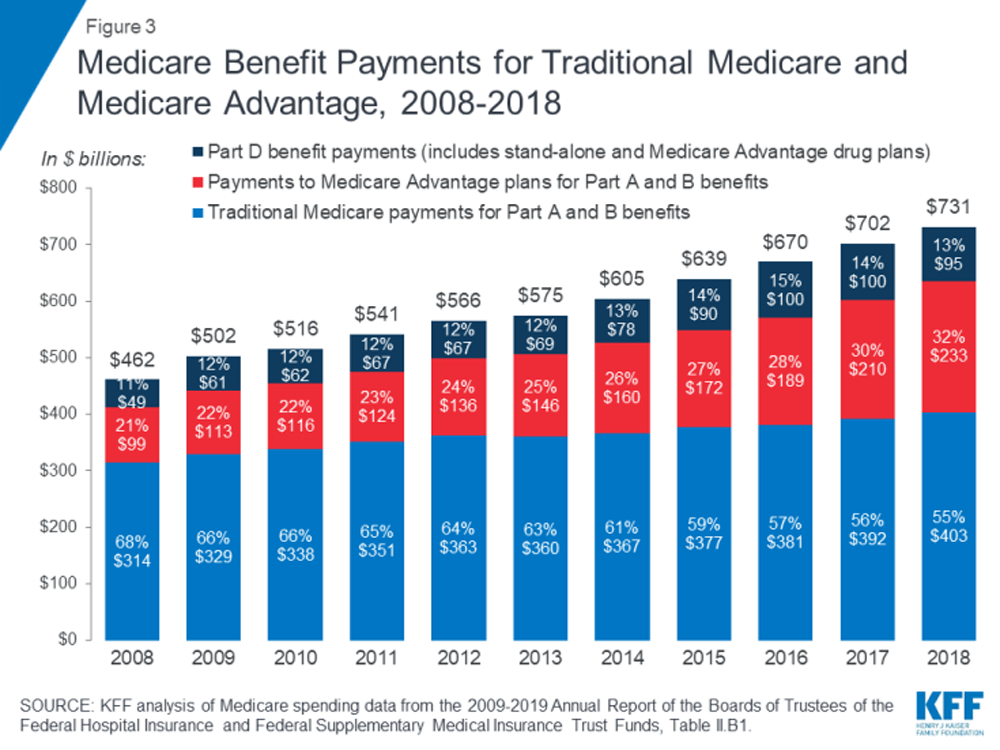
FROM: The Facts on Medicare Spending (2019)Objectives: The purpose of this study was to compare Medicare healthcare expenditures for patients who received long-term treatment of chronic low back pain (cLBP) with either opioid analgesic therapy (OAT) or spinal manipulative therapy (SMT).
Methods: We conducted a retrospective observational study using a cohort design for analysis of Medicare claims data. The study population included Medicare beneficiaries enrolled under Medicare Parts A, B, and D from 2012 through 2016. We assembled cohorts of patients who received long-term management of cLBP with OAT or SMT (such as delivered by chiropractic or osteopathic practitioners) and evaluated the comparative effect of OAT vs SMT upon expenditures, using multivariable regression to control for beneficiary characteristics and measures of health status, and propensity score weighting and binning to account for selection bias.
Results: The study sample totaled 28,160 participants, of whom 77% initiated long-term care of cLBP with OAT, and 23% initiated care with SMT. For care of low back pain specifically, average long-term costs for patients who initiated care with OAT were 58% lower than those who initiated care with SMT. However, overall long-term healthcare expenditures under Medicare were 1.87 times higher for patients who initiated care via OAT compared with those initiated care with SMT (95% CI 1.65-2.11; P < .0001).
Conclusions: Adults aged 65 to 84 who initiated long-term treatment for chronic low back pain (cLBP) via opioid analgesic therapy (OAT) incurred lower long-term costs for low back pain but higher long-term total healthcare costs under Medicare compared with patients who initiated long-term treatment with spinal manipulative therapy (SMT).
Keywords: Aged; Analgesics, Opioid; Costs and Cost Analysis; Low Back Pain; Manipulation, Spinal; Medicare.
From the FULL TEXT Article:
Introduction
Burden of Low Back Pain Among Older Adults
The crisis of opioid prescribing in the Unites States reflects in part a failure in the management of low back pain (LBP). Low back pain is highly prevalent in the United States and is the most common condition for which opioid analgesics are prescribed. [1] Low back pain is also one of the most common reasons for a physician visit in general, [2] and for older US adults in particular. [3] The point prevalence of nonspecific back pain among older adults is approximately 30%. [4] Older adults often have recurrent episodes of LBP. [5] Between 2000 and 2007, the total number of US adults with chronic low back pain (cLBP) increased by 64%. [6] Spinal pain is the most costly of all medical conditions. [7] A systematic review of LBP cost of illness studies that included 27 studies published between 1997 and 2007 found that direct costs ranged from $12 to $90 billion annually, and indirect costs ranged from $7 to $28 billion annually. [8] Because spine care in the Unites States has shown a decline in positive outcomes despite these rising costs, [9] it is important to assess the comparative value of treatments for cLBP.
Opioid Analgesic Therapy for LBP
Evidence-based management of LBP for older adults often includes prescription analgesics, including opioids. [10] A recent examination of health claims data found that 31% of patients with LBP received prescriptions for opioid analgesics within the first 6 months of initial diagnosis; within 3 years the percentage increased to 42%. [11] However, although opioid prescribing for LBP is often prolonged, [12] 3 systematic reviews concluded that the long-term effectiveness of opioid therapy for cLBP is unknown. [1315] The hazards of opioid analgesics are well known, however: the use and misuse of opioid analgesic therapy (OAT) has led to 3.8% of patients developing opioid use disorder, [16] and up to 26% of prescribed patients reporting opioid dependence. [17] In 2018, nearly 70% of US drug overdose deaths involved an opioid, and 46,802 people (128 per day on average) died from opioid-related overdoses. [18] In 2013, the cost of prescription opioid misuse totaled more than $78 billion, and among 6,917 Medicare patients, the additional annual per patient cost associated with diagnosis of opioid abuse or dependence was over $17,000. [19] Furthermore, among patients with a chronic disabling musculoskeletal disorder, higher dosing of opioids correlates with higher pain severity, greater disability, and higher levels of depression. [20] Recent studies suggest that OAT should be used sparingly and with caution for patients with cLBP owing to the risk of adverse effects. [11, 21]
Spinal Manipulative Therapy for LBP
Nonpharmacological management of spinal pain is associated with decreased use of opioids, [2225] and the National Academy of Medicine and the Joint Commission on Accreditation of Healthcare Organizations have recommended the use of nonpharmacological therapies as effective alternatives to pharmacotherapy for management of pain. [26, 27] Recent systematic reviews have found spinal manipulative therapy (SMT) to be an effective treatment for cLBP, [2830] and current clinical guidelines recommend nonpharmacological therapies, including SMT, as a first-line approach to management of LBP. [31]
Chiropractic management of LBP, which often involves treatment with SMT, may offer a safer alternative to analgesic medication: an observational study of adults with LBP found that the likelihood of adverse drug events was significantly lower for recipients of chiropractic care compared with nonrecipients. [20] Among older Medicare beneficiaries with an office visit risk for a neuromusculoskeletal problem, the adjusted risk of injury to the head, neck, or trunk among recipients of SMT was 76% lower compared with recipients of primary care. [32] More recently, a systematic review on the benefits and harms of SMT for treatment of cLBP found limited evidence regarding adverse events. [33]
Thus, there is little cause for concern about the safety of SMT for LBP, but for long-term treatment of cLBP, the overall value of SMT remains uncertain. A series of US government reports based upon medical record reviews found that chiropractors (who provide more than 97% of all SMT services under Medicare [34]) frequently provide excessive and unnecessary SMT, particularly as maintenance care, which is provided on an ongoing long-term basis, ostensibly to prevent spinal problems from recurring or worsening. [3537]
However, the government reports did not follow standardized review methods and failed to consider the value of chiropractic services. [38] It is also uncertain whether SMT offers a cost advantage for management of cLBP. A rigorously designed study that modelled the 1year cost-effectiveness of adding nonpharmacologic interventions for cLBP to usual care analyzed data from randomized trials of nonpharmacologic therapies, and found that 15 of 17 therapies were cost-effective from the payer perspective, but the results for chiropractic care were less favorable for patients with high-impact chronic pain than for a typical mix of patients. [39]
A study of Medicare claims data found that patients with multiple comorbidities who only used SMT for cLBP had significantly lower costs, [40] and in a quasi-experimental study of over 84,000 older Medicare beneficiaries, Davis et al. found that increased access to chiropractic spinal manipulation was correlated with reduced spine-related costs. [41] However, the comparative value of SMT for older adults with cLBP remains uncertain.
Cost of Care for cLBP Under Medicare
Owing to the high-cost burden imposed upon the Medicare system by care of patients with cLBP, it is critically important to identify high-value approaches to the treatment of cLBP. Until now, the long-term costs associated with OAT and SMT have not been rigorously compared. Therefore, the purpose of this study was to compare Medicare expenditures for cLBP among recipients of OAT versus SMT. We hypothesized that among older Medicare beneficiaries receiving long-term care for cLBP, initiation of treatment via OAT would be associated with higher costs compared with SMT.
References:
Hudson TJ Edlund MJ Steffick DE Tripathi SP Sullivan MD.
Epidemiology of regular prescribed opioid use:
results from a national, population-based survey.
J Pain Symptom Manage. 2008; 36: 280-288Kim LH Vail D Azad TD et al.
Expenditures and Health Care Utilization Among Adults
with Newly Diagnosed Low Back and Lower Extremity Pain
JAMA Network Open 2019 (May 3); 2 (5): e193676Hart LG Deyo RA Cherkin DC.
Physician office visits for low back pain. Frequency, clinical evaluation,
and treatment patterns from a U.S. national survey.
Spine. 1995; 20: 11-19Docking RE Fleming J Brayne C Zhao J Macfarlane GJ Jones GT.
Epidemiology of back pain in older adults:
prevalence and risk factors for back pain onset.
Rheumatology. 2011; 50: 1645-1653Dunn KM, Hestbaek L, Cassidy JD.
Low Back Pain Across the Life Course
Best Pract Res Clin Rheumatol 2013 (Oct); 27 (5): 591-600Smith, M, Davis, MA, Stano, M, and Whedon, JM.
Aging Baby Boomers and the Rising Cost of Chronic Back Pain:
Secular Trend Analysis of Longitudinal Medical Expenditures
Panel Survey Data for Years 2000 to 2007
J Manipulative Physiol Ther. 2013 (Jan); 36 (1): 211Dieleman JL, Cao J, Chapin A, et al.
US Health Care Spending by Payer and Health Condition, 1996-2016
JAMA 2020 (Mar 3); 323 (9): 863884Dagenais S, Caro J, Haldeman S.
A Systematic Review of Low Back Pain Cost of Illness Studies
in the United States and Internationally
Spine J 2008 (Jan); 8 (1): 820Martin BI, Turner JA, Mirza SK, et al.
Trends in Health Care Expenditures, Utilization, and Health Status Among
US Adults With Spine Problems, 1997-2006
Spine (Phila Pa 1976). 2009 (Sep 1); 34 (19): 20772084Jones MR Ehrhardt KP Ripoll JG et al.
Pain in the elderly.
Curr Pain Headache Rep. 2016; 20: 23Ong KL Stoner KE Yun BM Lau E Edidin AA.
Baseline and postfusion opioid burden for patients with low back pain.
Am J Manag Care. 2018; 24: e234-e240Cifuentes M Webster B Genevay S Pransky G.
The course of opioid prescribing for a new episode of disabling
low back pain: opioid features and dose escalation.
Pain. 2010; 151: 22-29Abdel Shaheed C Maher CG Williams KA Day R McLachlan AJ
Efficacy, tolerability, and dose-dependent effects of opioid analgesics
for low back pain: a systematic review and meta-analysis.
JAMA Intern Med. 2016; 176: 958-968Chaparro LE Furlan AD Deshpande A Mailis-Gagnon A Atlas S Turk DC.
Opioids compared with placebo or other treatments for chronic
low back pain: an update of the Cochrane Review.
Spine (Phila Pa). 2014; 39: 556-563Chou R Turner JA Devine EB et al.
The effectiveness and risks of long-term opioid therapy for
chronic pain: a systematic review for a National Institutes
of Health Pathways to Prevention Workshop.
Ann Intern Med. 2015; 162: 276-286Fleming MF Balousek SL Klessig CL Mundt MP Brown DD.
Substance use disorders in a primary care sample receiving daily opioid therapy.
J Pain. 2007; 8: 573-582Boscarino JA Rukstalis M Hoffman SN et al.
Risk factors for drug dependence among out-patients on opioid therapy
in a large US health-care system.
Addiction. 2010; 105: 1776-1782Centers for Disease Control. 2019 (Available at)
https://www.cdc.gov/drugoverdose/data/statedeaths.html
(Accessed Nov 5, 2020)Florence CS Zhou C Luo F Xu L.
The economic burden of prescription opioid overdose, abuse,
and dependence in the United States, 2013.
Med Care. 2016; 54: 901-906Kidner CL Mayer TG Gatchel RJ.
Higher opioid doses predict poorer functional outcome in patients
with chronic disabling occupational musculoskeletal disorders.
J Bone Joint Surg Am. 2009; 91: 919-927Tucker HR Scaff K McCloud T et al.
Harms and benefits of opioids for management of non-surgical
acute and chronic low back pain: a systematic review.
Br J Sports Med. 2020; 54: 664Whedon JM, Toler AWJ, Goehl JM, Kazal LA.
Association Between Utilization of Chiropractic Services for
Treatment of Low-Back Pain and Use of Prescription Opioids
J Altern Complement Med. 2018 (Jun); 24 (6): 552556Corcoran KL, Bastian LA, Gunderson CG, et al.
Association Between Chiropractic Use and Opioid Receipt Among
Patients with Spinal Pain: A Systematic Review and Meta-analysis
Pain Medicine 2020 (Feb 1); 21 (2): e139e145Kazis LE, Ameli O, Rothendler J, et al.
Observational Retrospective Study of the Association of Initial Healthcare Provider
for New-onset Low Back Pain with Early and Long-term Opioid Use
BMJ Open. 2019 (Sep 20); 9 (9): e028633
There are more like this at our INITIAL PROVIDER/FIRST CONTACT PageWhedon JM, Toler AWJ, Kazal LA, Bezdjian S, Goehl JM, Greenstein J.
Impact of Chiropractic Care on Use of
Prescription Opioids in Patients with Spinal Pain
Pain Medicine 2020 (Dec 25); 21 (12): 35673573
There are more like this at our SPINAL PAIN MANAGEMENT PageInstitute of Medicine (IOM)
Relieving Pain in America: A Blueprint for Transforming Prevention,
Care, Education, and Research
Washington, DC: The National Academies Press, 2011.Revisions to pain management standard effective January 1, 2015. Available at:
http://www.jointcommission.org/assets/1/23/jconline_november_12_14.pdf
Accessed May 28, 2015.Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al.
Nonpharmacologic Therapies for Low Back Pain: A Systematic Review
for an American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 493505Coulter ID, Crawford C, Hurwitz EL, Vernon H, Khorsan R, Suttorp Booth M, Herman PM.
Manipulation and Mobilization for Treating Chronic Low Back Pain:
A Systematic Review and Meta-analysis
Spine J. 2018 (May); 18 (5): 866879Rubinstein SM, de Zoete A, van Middelkoop M, et al.
Benefits and Harms of Spinal Manipulative Therapy for the Treatment
of Chronic Low Back Pain: Systematic Review and Meta-analysis
of Randomised Controlled Trials
British Medical Journal 2019 (Mar 13); 364: l689Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514530Whedon, JM, Mackenzie, TA, Phillips, RB, and Lurie, JD.
Risk of Traumatic Injury Associated with Chiropractic Spinal Manipulation
in Medicare Part B Beneficiaries Aged 66-99
Spine (Phila Pa 1976) 2015 (Feb 15); 40 (4): 264270Rubinstein SM, de Zoete A, van Middelkoop M, et al.
Benefits and Harms of Spinal Manipulative Therapy for the Treatment
of Chronic Low Back Pain: Systematic Review and Meta-analysis
of Randomised Controlled Trials
British Medical Journal 2019 (Mar 13); 364: l689Whedon JM Haldeman S Petersen C Schoellkopf W MacKenzie T Lurie J.
Temporal trends and geographic variations in the supply of clinicians
who provide spinal manipulation to Medicare beneficiaries: a serial cross-sectional study.
J Manipulative Physiol Ther. 2021; 44: 177-185Office of Inspector General Chiropractic services in the Medicare Program:
patient vulnerability analysis.
Office of Inspector General, Department of Health and Human Services,
Washington, DC2005Office of Inspector General
Inappropriate Medicare payments for chiropractic services.
Office of Inspector General, Department of Health and Human Services,
Washington, DC2009Office of Inspector General
Hundreds of millions in Medicare payments for chiropractic services did not comply with Medicare requirements.
2016Whedon JM, Goertz CM, Lurie JD, Stason WB.
Beyond Spinal Manipulation: Should Medicare Expand Coverage for Chiropractic Services?
A Review and Commentary on the Challenges for Policy Makers
Journal of Chiropractic Humanities 2013 (Aug 28); 20 (1): 918Herman PM Lavelle TA Sorbero ME Hurwitz EL Coulter ID.
Are nonpharmacologic interventions for chronic low back pain
more cost effective than usual care? Proof of concept results from a Markov model.
Spine. 2019; 44: 1456-1464Weeks, WB, Leininger, B, Whedon, JM et al.
The Association Between Use of Chiropractic Care and Costs of Care Among Older
Medicare Patients With Chronic Low Back Pain and Multiple Comorbidities
J Manipulative Physiol Ther. 2016 (Feb); 39 (2): 6375Davis AY, O, Liu H, Tootoo J, Titler MG, Bynum JPW.
Access to Chiropractic Care and the Cost of Spine Conditions Among Older Adults
American J Managed Care 2019 (Aug); 25 (8): e230e236R.A. Deyo, S.F. Dworkin, D. Amtmann, G. Andersson, et al.,
Report of the NIH Task Force on Research Standards for Chronic Low Back Pain
Journal of Pain 2014 (Jun); 15 (6): 569585National Drug Codes List -
The complete repository of National Drug Codes Information.
NDC List, 2020. Available at
https://ndclist.com/
Accessed June 20, 2020.Morden NE Munson JC Colla CH et al.
Prescription opioid use among disabled Medicare beneficiaries:
intensity, trends, and regional variation.
Med Care. 2014; 52: 852-859Keeney BJ, Fulton-Kehoe D, Turner JA, Wickizer TM, Chan KC, Franklin GM.
Early Predictors of Lumbar Spine Surgery After Occupational Back Injury:
Results From a Prospective Study of Workers in Washington State
Spine (Phila Pa 1976). 2013 (May 15); 38 (11): 953964Liliedahl RL, Finch MD, Axene DV, Goertz CM.
Cost of Care for Common Back Pain Conditions Initiated with
Chiropractic Doctor vs Medical Doctor/Doctor of Osteopathy
as First Physician: Experience of One Tennessee-Based
General Health Insurer
J Manipulative Physiol Ther 2010 (Nov); 33 (9): 640643
Return to MEDICARE
Return to COST-EFFECTIVENESS
Since 12-14-2021


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |