Association Between Chiropractic Use and Opioid Receipt Among
Patients with Spinal Pain: A Systematic Review and Meta-analysisThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Pain Medicine 2020 (Feb 1); 21 (2): e139–e145 ~ FULL TEXT
OPEN ACCESS Kelsey L Corcoran, DC, Lori A Bastian, MD, Craig G Gunderson, MD,
Catherine Steffens, Alexandria Brackett, MA, MLIS, Anthony J Lisi, DC
Kelsey L. Corcoran, DC,
Yale Center for Medical Informatics,
300 George St., Suite 501,
New Haven, CT 06511, USA.
kelsey.corcoran@yale.edu
OBJECTIVE: To investigate the current evidence to determine if there is an association between chiropractic use and opioid receipt.
DESIGN: Systematic review and meta-analysis.
METHODS: The protocol for this review was registered on PROSPERO (CRD42018095128). The MEDLINE, PubMed, EMBASE, AMED, CINAHL, and Web of Science databases were searched for relevant articles from database inception through April 18, 2018. Controlled studies, cohort studies, and case-control studies including adults with noncancer pain were eligible for inclusion. Studies reporting opioid receipt for both subjects who used chiropractic care and nonusers were included. Data extraction and risk of bias assessment were completed independently by pairs of reviewers. Meta-analysis was performed and presented as an odds ratio with 95% confidence interval.
RESULTS: In all, 874 articles were identified. After detailed selection, 26 articles were reviewed in full, and six met the inclusion criteria. Five studies focused on back pain and one on neck pain. The prevalence of chiropractic care among patients with spinal pain varied between 11.3% and 51.3%. The proportion of patients receiving an opioid prescription was lower for chiropractic users (range = 12.3–57.6%) than nonusers (range = 31.2–65.9%). In a random-effects analysis, chiropractic users had a 64% lower odds of receiving an opioid prescription than nonusers (odds ratio = 0.36, 95% confidence interval = 0.30–0.43, P < 0.001, I2 = 92.8%).
There are more articles like this @ our: SPINAL PAIN MANAGEMENT Page
CONCLUSIONS: This review demonstrated an inverse association between chiropractic use and opioid receipt among patients with spinal pain. Further research is warranted to assess this association and the implications it may have for case management strategies to decrease opioid use.
KEYWORDS: Analgesic; Chiropractic; Low Back Pain; Meta-analysis; Neck Pain; Opioid; Systematic Review

Chiropractic Care For Back Pain Tied To Lower Odds Of Opioid Use
By Lisa Rapaport ~ October 24, 2019
(Reuters Health) – People with chronic back and neck pain who receive chiropractic care may be less likely to use opioid painkillers, a research review suggests.
Researchers examined data from six previously-published smaller studies with a total of more than 62,000 participants with spinal pain. Across all of the studies, 11% to 51% of the patients used chiropractic care.
People who saw a chiropractor were 64% less likely to use opioids than people who didn’t, researchers report in the journal Pain Medicine.
“Patients with spinal pain who visit a chiropractor may receive treatments such as spinal manipulation, massage, acupuncture, exercises and education as appropriate,” said lead author Kelsey Corcoran of Yale School of Medicine in New Haven, Connecticut.
“These therapies may lead to decreased pain, improved range of motion and increased function,” Corcoran said by email. “If a patient’s pain is well controlled by the treatment they received from a chiropractor, they may subsequently need less pain medications or even none at all.”
Read the rest of this Full Text article now!
From the Full-Text Article:
Introduction
Since the release of the Centers of Disease Control and Prevention’s guidelines for prescribing opioids for chronic pain in 2016, certain opioid prescribing rates have declined. [1, 2] This includes the rates of highdosage prescriptions (≥90 morphine equivalent milligrams per day) and overall opioid prescribing. [1] Although this trend is favorable, preventing opioid addiction and overdose still remain a significant public health priority. [3] In 2017 alone, an average 115 Americans died daily from opioid overdose. [4]
Overdose deaths from opioids are correlated with prescribing patterns and legal sales. [5–8] Therefore, one component of addressing the opioid epidemic is the effective utilization of nonpharmacological therapies as frontline treatment options to avoid the prescription of opioids and the potential harms associated with their use. [2] Current clinical practice guidelines for the management of low back pain (LBP), neck pain, and osteoarthritis of the hip, knee, and hand recommend specific nonpharmacological treatments as initial considerations ahead of pharmacological treatment. [9–12]
Chiropractors provide many of the nonpharmacological treatments recommended by clinical practice guidelines for spinal pain, including spinal manipulation, patient education, exercise, acupuncture, and massage. [13–15] Chiropractors do not prescribe opioids; therefore, patients would never receive opioid prescriptions as part of a chiropractic treatment plan. Yet it is unknown whether patients who receive chiropractic care are less likely to receive an opioid prescription from any provider for a given complaint. Recent work from the Veterans Health Administration (VHA) demonstrated that veterans who utilized VHA chiropractic services had a decreased likelihood of receiving an opioid after an initial chiropractic visit than before the visit. [16]
This project was a systematic review and meta-analysis to investigate the current evidence and determine if there is an association between chiropractic use and opioid receipt. To date, no review has assessed for such an association.
Methods
Search Strategy
Before commencing the review, a protocol was registered on PROSPERO (CRD42018095128). A clinical librarian (AB) developed the literature search strategy using the protocol as a framework. The search strategy used both key words and controlled vocabulary combining the terms for “chiropractic” and “opioids.” The OVID Medline, OVID Embase, OVID AMED, Web of Science, PubMed, and CINAHL databases were searched from database inception to April 18, 2018. The year of inception of the included databases was 1946 for OVID Medline, 1974 for OVID Embase, 1985 for OVID AMED, 1946 for PubMed, and 1937 for CINAHL, and Web of Science’s earliest record was 1900. The OVID Medline search strategy is included in Supplement 1. The search results were exported into EndNote (Clarivate Analytics, Philadelphia, Pennsylvania), deduplicated, and then uploaded to Covidence (Veritas Health Innovation, Melbourne, Australia) for screening. Additional articles were identified by examining included articles’ bibliographies and other sources. Gray literature was considered by searching the Cochrane library, ongoing registered clinical trials, and as part of the main search strategy, as gray literature is included in both OVID Embase and OVID AMED.
Inclusion Criteria
To be included in this review, studies had to include only adults (≥18 years of age) with noncancer pain and quantitatively report on opioid receipt for both a group of chiropractic users and nonusers. Chiropractic users were defined as individuals who received care from a Doctor of Chiropractic. Controlled studies, cohort studies, and case–control studies were eligible for inclusion.
Exclusion Criteria
Studies including children (<18 years of age), cancer pain, and animals were excluded. Studies that evaluated chiropractic care as part of a combined, multidisciplinary approach were excluded unless the chiropractic care portion was assessed separately. Studies that evaluated spinal manipulation delivered by providers other than chiropractors were also excluded, unless the chiropractic care was assessed separately.
Selecting Manuscripts for Full-Text Review
Two co-authors (KC, AL) used inclusion and exclusion criteria to assess titles and abstracts. Eligibility decisions and disagreements were reconciled through discussion or by a third reviewer (LB). Full-text articles included by two reviewers underwent further evaluation.
Data Extraction and Quality Assessment
Two co-authors (CS, LB) extracted data from published reports into evidence tables. An additional co-author over-read the evidence tables (KC). In instances where there were questions about the study data of included manuscripts, the corresponding author of the manuscript was contacted. For included studies, data were extracted on study characteristics, study sample, quality, prevalence of chiropractic use and observation period assessed, proportion of opioid receipt for chiropractic users and nonusers, and length of follow-up. If studies reported on more than one follow-up duration for opioid receipt, the longer follow-up period was chosen for data extraction.
Two co-authors (KC, CS) independently rated quality at the study level using key criteria described in the Newcastle-Ottawa Quality Assessment Scale for Cohort Studies and assigned a numerical score out of a possible nine points. [17] The Newcastle Ottawa Scale (NOS) is an evaluation tool for cohort studies has demonstrated content validity and inter-rater reliability. [17] Higher scores on the NOS represent a lower risk of bias, and the NOS uses three main categories to assess risk of bias: selection of the cohort, comparability of the exposed and nonexposed cohort, and assessment of outcomes. [18] Disagreements in NOS scoring were adjudicated by obtaining a third co-author’s (LB) opinion.
Statistical Analysis
The proportion of patients receiving opioids was calculated for each individual study for the group receiving chiropractic care and compared with the group that was not receiving chiropractic care. The difference in proportions between these groups was expressed as an odds ratio. Individual study odds ratios were plotted using a forest plot, and the pooled odds ratio was calculated using random effects meta-analysis. Between-study heterogeneity was estimated using the I2 statistic. [19] Statistical significance was set at a P value of <0.05. Statistical analysis was performed using Stata/MP, version 15.1 (StataCorp, College Station, TX, USA).
Results
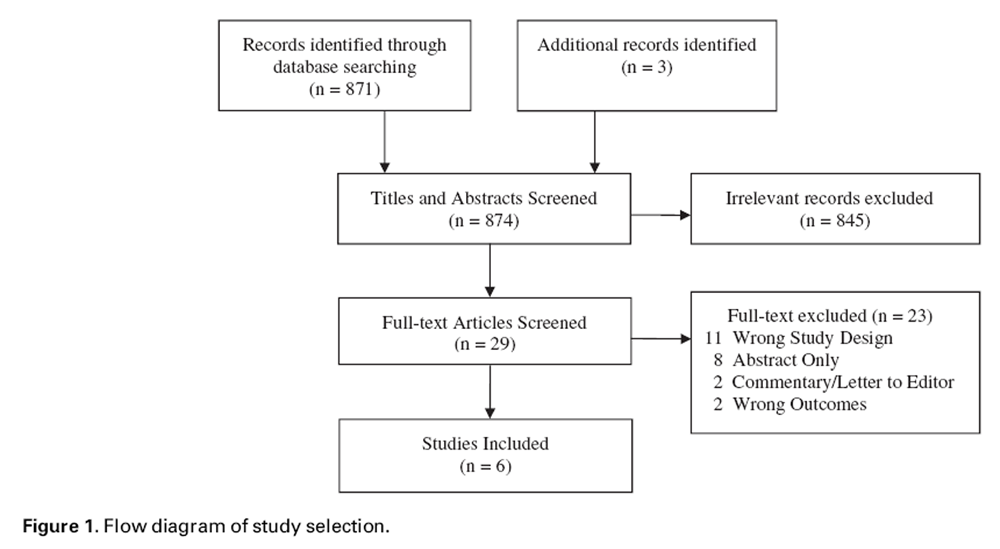
Figure 1

Table 1

Table 2

Table 3
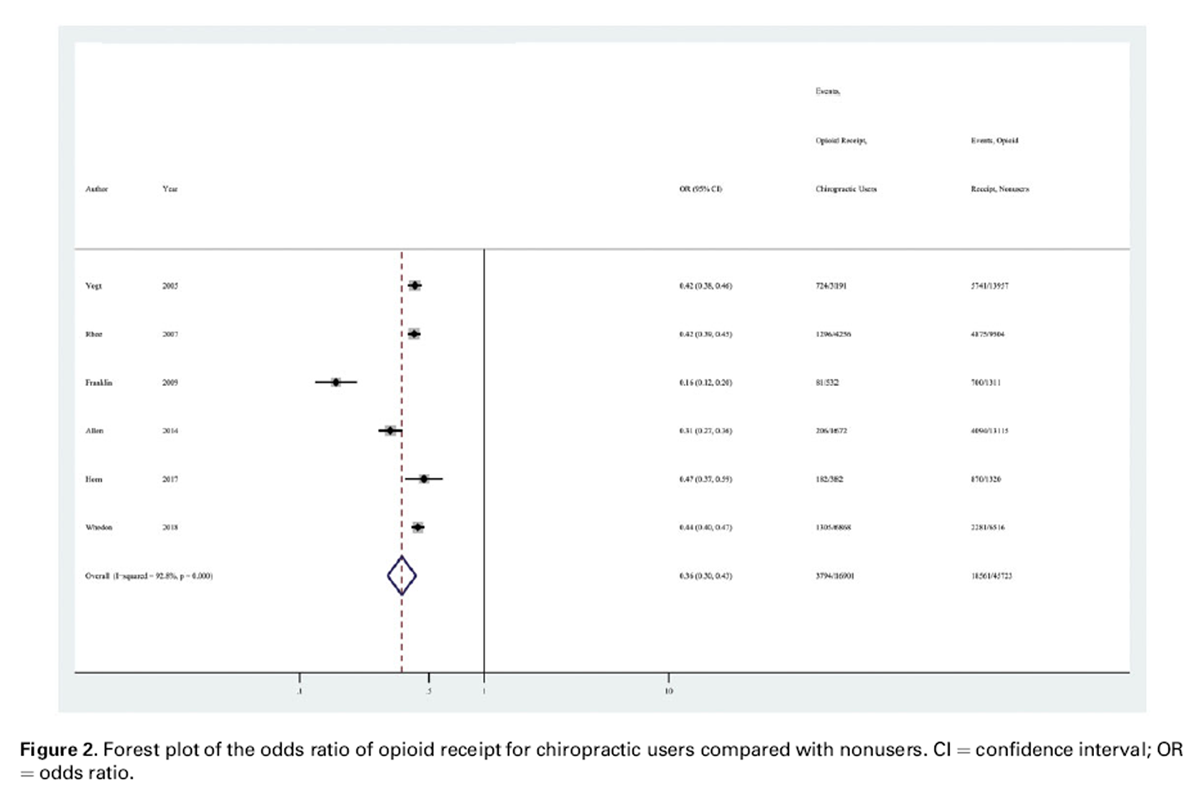
Figure 2 The electronic literature search identified a total of 1,051 records with 871 original articles. Three additional articles were identified by the co-authors. After detailed selection, 26 articles were reviewed in full, and six met study inclusion criteria (Figure 1). [20–25] During title and abstract screening, the majority of excluded manuscripts were reviews or case reports (53%). Additional manuscripts were excluded at this stage because they did not examine chiropractic care or did not have outcome data on opioid use. Very few studies (<5%) were excluded because they included children or examined cancer pain. Additional data were requested and received by investigators from one of the included studies. [23] The gray literature search yielded no additional literature pertinent to this review.
All included studies were cohort studies with a low risk of bias (Tables 1 and 2). The prevalence of chiropractic care varied between 11.3% and 51.3%. Chiropractic users had a lower percentage of opioid receipt than nonusers in all studies included (Table 3, Figure 2).
All six studies (62,624 patients) provided sufficient data and were judged similar enough to be pooled for meta-analysis. In a random-effects analysis, chiropractic users had a 64% lower odds of receiving an opioid prescription than nonusers (odds ratio = 0.36, 95% confidence interval = 0.30–0.43, P<0.001, I2 = 92.8%).
Discussion
The main finding of the review was that all included studies demonstrated a negative association between use of chiropractic care and opioid prescription receipt. The current study adds to the small but increasing body of evidence demonstrating that access to and utilization of chiropractic services are negatively associated with opioid use, and thus may warrant further investigation to determine if chiropractic care may be an effective component of opioid prescription reduction strategies. [16, 26, 27] It is noteworthy that the negative association found in this review encompasses all providers that patients may have seen for their care, not just the chiropractors, who would never prescribe opioids based on their scope of practice.
Chiropractors predominantly manage spinal conditions, with back conditions being the most common reason to seek chiropractic care. [13, 28] All studies included in this review evaluated patient populations with spinal pain, with the majority focusing on back pain and one study addressing neck pain patients. Back pain is also responsible for a considerable amount of worldwide disability and social costs, including an estimated cost of >$100 billion per year in the United States alone. [29, 30] It is logical that the majority of the current literature existing on the topic of chiropractic care and opioid receipt predominantly focuses on back pain.
In four of the six studies included, chiropractors were either the first provider seen or part of the initial treatment strategy. Ideally, nonpharmacological therapies including multimodal chiropractic care are utilized as frontline treatments to ultimately avoid the prescription of opioids, which are associated with poor outcomes for low back pain and chronic pain. [7, 31] For patients who are already receiving opioid therapy, the effectiveness of chiropractic care on pain and function is not well understood. All studies included in this review did not assess for prior opioid use; therefore, no conclusions can be drawn as to whether an association between chiropractic care and opioid receipt exists in opioid-naive patient populations and/or populations that have used opioid therapy. A VHA study evaluating the implementation of a stepped-care model of pain management for long-term opioid users demonstrated that referrals to chiropractic services and physical therapy increased, whereas highdose opioid prescribing was successfully decreased, during a four-year study period. [27] It is possible that chiropractic care may be a reasonable component of a pain management plan during an opioid taper, though this has not been sufficiently studied.
Only one of the included studies graded LBP severity and incorporated severity into a regression model. [23] This study demonstrated that long-term opioid use (one or more years) was significantly lower for those who saw a chiropractor as the first provider for LBP compared with individuals who initially saw other provider types after adjusting for LBP severity, baseline pain, and function. [23] An additional study by Whedon et al. used propensity scoring and determined that the chiropractic users were healthier than the nonusers studied. [24] However, the authors reported that the difference in opioid receipt for chiropractic users and nonusers was minimally affected by propensity score adjustments. [24] These two studies preliminarily suggest that the negative association between chiropractic use and opioid receipt may persist despite potential differences in disease severity and the general health of the individuals utilizing chiropractic care. However, more research is needed, particularly controlled trials to account for potential selection bias.
None of the included studies identified the specific treatments that patients received from the chiropractors. Therefore, we cannot comment on if specific treatment components of multimodal chiropractic care contributed more than others to the inverse association between chiropractic use and opioid receipt. It is also unknown whether this association is unique to chiropractic care or similar to clinical management from other nonpharmacological health care providers such as physical therapists and acupuncturists. Of the studies included in this review, four reported on the likelihood of opioid receipt for physical therapy patients, and none reported on other traditionally nonpharmacological health care provider types. [20–22, 25] The one study on neck pain demonstrated that patients seen by physical therapists also had a decreased odds of opioid receipt. [25] For the included studies of low back pain that referred to physical therapy, the results were mixed. Rhee et al. found that physical therapy users were more likely to receive an opioid prescription than to not receive one, whereas Vogt et al. similarly reported that patients with an opioid claim were more likely to use physical therapy than those without an opioid claim. [20, 21]
In contrast, Allen et al. demonstrated that patients who were treated by a physical therapist were less likely to receive opioids than to not receive them during the first four weeks of low back pain. [22] This sampling of the literature is not comprehensive enough to determine the potential association between physical therapy and opioid receipt, but it does demonstrate that for included studies there were instances where the inverse association between chiropractic use and opioid receipt was similar to the relationship between physical therapy and opioid receipt and instances where the relationship between physical therapy and opioid receipt was different. Further research is needed to determine if the inverse association demonstrated in this review between chiropractic care and opioid receipt is unique to chiropractic care or consistent with the relationship between opioid receipt and other nonpharmacological health care specialties.
Further research is warranted given that effective strategies to decrease opioid prescribing are a public health and research priority. [3, 32, 33] Developing a better understanding of the relationship between chiropractic care and opioid use has the potential to impact clinical decisions and health care policy, especially concerning access to chiropractic services within health care systems and sequencing with other therapies. Although the results of this review are promising, more research is needed to understand which components of multimodal chiropractic care may be inversely associated with opioid use and if this association is unique to chiropractic management or consistent with other nonpharmacological therapies. Future research on the relationship between chiropractic use and opioid receipt should also include randomized controlled trials, as there were none available for inclusion in this review. This could inform how to best operationalize chiropractic services to support improvement in rates of opioid use.
Limitations
No conclusion of causation can be made from the association presented in this study, nor can it be concluded that the negative association between chiropractic care and opioid receipt is unique to chiropractic care and not consistent with other therapies.
There are several limitations inherent in this study. There was a small quantity of available research that met the inclusion criteria. The included studies had significant heterogeneity of their results. In all but one study, the severity of spinal disease was not reported. Therefore, we cannot comment on whether differences in disease severity existed between chiropractic users and nonusers, which may have influenced the pooled odds ratio of opioid receipt. We also cannot conclude if there were other differences between the chiropractic users and nonusers that may have resulted from the self-selection of chiropractic services in these cohort studies. For instance, patients who chose to undergo chiropractic care may have been inherently opposed to opioid medications, which could explain some of the inverse association we found. Details regarding chiropractic management, such as dose and therapies utilized, were also not reported and may have influenced study results. It is likely that the available research on the topic of chiropractic use and opioid receipt is subject to both publication bias and selective reporting. Although all included studies had a low risk of bias at the study level, the risk of bias for the outcomes reported in this paper was not evaluated. It is likely that there is more bias at the outcome level than at the study level, as none of the included studies accounted for opioid receipt before the study period.
Conclusions
This systematic review demonstrated an inverse association between chiropractic use and opioid receipt among patients with spinal pain. Overall, chiropractic users had a 64% lower odds of receiving an opioid prescription than nonusers. Further research is warranted to assess this association and the implications it may have for case management strategies to decrease opioid use.
Acknowledgments
The study authors would like to thank Gary M. Franklin, MD, MPH, and Deborah Fulton-Kehoe, PhD, MPH, from the University of Washington for supplying additional study data and Khadija El-Hazimy and Vermetha Polite of the Cushing/Whitney Medical Library at Yale University for administrative support.
Funding sources:
This material is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, and Health Services Research and Development IIR 12-118, CIN 13-407; by the NCMIC Foundation; and with resources from and the use of facilities at the VA Connecticut Healthcare System.
Conflict of interest:
The authors have no conflicts of interest to report.
References:
Bohnert ASB, Guy GP Jr, Losby JL.
Opioid prescribing in the United States before and after the Centers for Disease Control
and Prevention’s 2016 opioid guideline.
Ann InternMed 2018;169(6):367–75.Dowell D, Haegerich TM, Chou R.
CDC Guideline for Prescribing Opioids for Chronic Pain: United States, 2016
Morbidity and Mortality Weekly Report
Recommendations and Reports Vol. 65 No. 1 March 18, 2016Alexander LM, Keahey D, Dixon K.
Opioid use disorder: A public health emergency.
JAAPA 2018;31 (10):47–52.Centers for Disease Control and Prevention.
Wide-Ranging Online Data for Epidemiologic Research (WONDER).
Atlanta, GA: National Center for Health Statistics; 2017.Bohnert AS, Valenstein M, BairMJ, et al.
Association between opioid prescribing patterns and opioid overdose-related deaths.
JAMA 2011;305 (13):1315–21.Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN.
Opioid dose and drug-related mortality in patients with nonmalignant pain.
Arch Intern Med 2011;171(7):686–91.Dunn KM, Saunders KW, Rutter CM, et al.
Opioid prescriptions for chronic pain and overdose: A cohort study.
Ann InternMed 2010;152(2):85–92.Centers for Disease Control and Prevention.
Vital Signs: Overdoses of Prescription Opioid Pain Relievers—United States, 1999–2008.
Atlanta: Centers for Disease Control and Prevention; 2011. Available at:
https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6043a4.htm? s_cid = mm6043a4_w%20-%20fig2
(accessed January 17, 2019).Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Cote P, Wong JJ, Sutton D, et al.
Management of Neck Pain and Associated Disorders: A Clinical Practice Guideline
from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration
European Spine Journal 2016 (Jul); 25 (7): 2000–2022Bruyere O, Cooper C, Pelletier JP, et al.
An algorithm recommendation for the management of knee osteoarthritis in Europe and internationally:
A report from a task force of the European Society for Clinical and Economic Aspects of
Osteoporosis and Osteoarthritis (ESCEO).
Semin Arthritis Rheum2014;44(3):253–63.Hochberg MC, Altman RD, April KT, et al.
American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic
therapies in osteoarthritis of the hand, hip, and knee.
Arthritis Care Res (Hoboken) 2012;64(4):465–74.Lisi AJ, Brandt CA.
Trends in the Use and Characteristics of Chiropractic Services
in the Department of Veterans Affairs
J Manipulative Physiol Ther. 2016 (Jun); 39 (5): 381–386Mootz RD, Cherkin DC, Odegard CE, Eisenberg DM, Barassi JP, Deyo RA.
Characteristics of Chiropractic Practitioners, Patients, and Encounters in Massachusetts and Arizona
J Manipulative Physiol Ther. 2005 (Nov); 28 (9): 645–653Coulter ID, Shekelle PG.
Chiropractic in North America: A descriptive analysis.
J Manipulative Physiol Ther 2005;28(2):83–9.Lisi AJ, Corcoran KL, DeRycke EC, et al.
Opioid Use Among Veterans of Recent Wars Receiving
Veterans Affairs Chiropractic Care
Pain Med. 2018 (Sep 1); 19 (suppl_1): S54–S60Wells GS, Shea B, O’Connell D, et al.
The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses.
Ottawa, Canada: Ottawa Hospital Research Institute; 2013. Available at:
http://www. ohri.ca/programs/clinical_epidemiology/oxford.asp
(accessed January 17, 2019).Baldacchino A, Balfour DJ, Matthews K.
Impulsivity and opioid drugs: Differential effects of heroin, methadone and prescribed analgesic medication.
Psychol Med 2015;45(6):1167–79.Higgins JP, Thompson SG, Deeks JJ, Altman DG.
Measuring inconsistency in meta-analyses.
BMJ 2003;327(7414):557–60.Rhee Y, Taitel MS, Walker DR, Lau DT.
Narcotic drug use among patients with lower back pain in employer health plans:
A retrospective analysis of risk factors and health care services.
Clin Ther 2007; 29(Suppl):2603–12.Vogt MT, Kwoh CK, Cope DK, Osial TA, Culyba M, Starz TW.
Analgesic usage for low back pain: Impact on health care costs and service use.
Spine (Phila Pa 1976) 2005;30(9):1075–81.Allen, H, Wright, M, Craig, T et al.
Tracking Low Back Problems in a Major Self-Insured Workforce:
Toward Improvement in the Patient's Journey
J Occup Environ Med. 2014 (Jun); 56 (6): 604-620Franklin GM, Rahman EA, Turner JA, Daniell WE, Fulton-Kehoe D.
Opioid use for chronic low back pain: A prospective, population-based study among injured workers
in Washington State, 2002-2005.
Clin J Pain 2009;25(9):743–51.Whedon JM, Toler AWJ, Goehl JM, Kazal LA.
Association Between Utilization of Chiropractic Services for Treatment of Low-Back Pain
and Use of Prescription Opioids
J Altern Complement Med. 2018 (Jun); 24 (6): 552–556Horn ME, George SZ, Fritz JM.
Influence of Initial Provider on Health Care Utilization in Patients Seeking Care for Neck Pain
Mayo Clin Proc Innov Qual Outcomes. 2017 (Oct 19); 1 (3): 226–233Weeks WB, Goertz CM.
Cross-Sectional Analysis of Per Capita Supply of Doctors of Chiropractic
and Opioid Use in Younger Medicare Beneficiaries
J Manipulative Physiol Ther 2016 (May); 39 (4): 263–266Dorflinger L, Moore B, Goulet J, et al.
A partnered approach to opioid management, guideline concordant care and the stepped care model of pain management.
J Gen Intern Med 2014;29(Suppl 4): 870–6.Adams J, Peng W, Cramer H, et al.
The Prevalence, Patterns, and Predictors of Chiropractic Use Among US Adults:
Results From the 2012 National Health Interview Survey
Spine (Phila Pa 1976). 2017 (Dec 1); 42 (23): 1810–1816Vos T, Flaxman AD, Naghavi M, et al.
Years Lived with Disability (YLDs) for 1160 Sequelae of 289 Diseases and Injuries
1990-2010: A Systematic Analysis for the Global Burden of Disease Study 2010
Lancet. 2012 (Dec 15); 380 (9859): 2163–2196Katz JN.
Lumbar disc disorders and low-back pain: Socioeconomic factors and consequences.
J Bone Joint Surg Am 2006;88(Suppl 2):21–4.Ashworth J, Green DJ, Dunn KM, Jordan KP.
Opioid use among low back pain patients in primary care:
Is opioid prescription associated with disability at 6-month follow-up?
Pain 2013;154 (7):1038–44.Department of Health and Human Services.
NIHDoD-VA Pain Management Collaboratory - Pragmatic Clinical Trials Demonstration Projects (UG3/UH3).
Washington, DC: Department of Health and Human Services,
Department of Defense, Department of Veterans Affairs; 2016. Available at:
https://grants.nih.gov/grants/guide/rfa-files/RFA-AT-17-001.html
(accessed January 17, 2019).Kligler B, Bair MJ, Banerjea R, et al.
Clinical Policy Recommendations from the VHA State-of-the-Art Conference
on Non-Pharmacological Approaches to Chronic Musculoskeletal Pain
J Gen Intern Med 2018 (May); 33 (Suppl 1): 16–23
Return to OPIOID EPIDEMIC
Return to SPINAL PAIN MANAGEMENT
Return NON-PHARMACOLOGIC THERAPY
Since 9-29-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |