Integrating a Multidisciplinary Pain Team and Chiropractic Care
in a Community Health Center: An Observational Study
of Managing Chronic Spinal PainThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Primary Care & Community Health 2020 (Sep 10) ~ FULL TEXT
OPEN ACCESS Christopher Prater, Melissa Tepe, Patrick Battaglia
Washington University School of Medicine,
St. Louis, MO, USA.Background: Chronic spinal pain is one of the most common diseases in the United States. Underserved patients are most affected, and disproportionately may use opioid medications as they lack access to other therapies. It is therefore important to develop systems to treat spinal pain within the primary medical home.
Methods: We designed a prospective observational pilot study at a community health center to measure the effectiveness of two interventions among an underserved population: a multidisciplinary pain team and chiropractic care. Study outcomes were pain and functional disability measured by the Pain Disability Questionnaire (PDQ), and reduction of opioid dose at baseline and 6–12 months. Multivariate linear regression was used to determine associating factors for change in PDQ scores.
Results: Thirty-five individuals completed baseline and follow-up PDQs from August 2018 to May 2020. Overall, the mean baseline PDQ was 92.4 +/– 6.1 and the mean follow-up PDQ was 81.9 +/– 7.7, resulting in a mean improvement of 10.6 (95% CI 1.2 - –22.3, P = .08). Participants in the chiropractic team (mean change –25.0, P = .01) and those completing the study before COVID-19 (mean change = –22.6, P < .01) were found to have significantly greater improvement at follow-up.
Conclusion: This observational study within a community health center resulted in improvement in spinal pain and disability with chiropractic care versus a multidisciplinary pain team. Offering similar services in primary care may help to address pain and disability, and hopefully limit external referrals, advanced imaging, and opioid prescriptions.
Keywords: integrated care; pain mangement; primary care; spinal pain; underserved communities.
From the FULL TEXT Article:
Introduction
In the United States, 20.4% (50.0 million) adults suffer from chronic pain, and 8.0% (19.6 million) of U.S. adults have high-impact chronic pain (chronic pain limiting life and work activities). [1] Spinal pain is common and impactful, as low back pain is the first and neck pain is the fourth most common cause of years lived with disability globally, according to the Global Burden of Disease Study in 2010. [2, 3] Chronic pain is a biopsychosocial condition, and those medically underserved are at greater risk. Using the nationally-represented Health and Retirement Study, investigators determined that 17% of those living in the lowest wealth quartile suffer from high-impact chronic pain compared to 8% of the total study population. [4] Recent regional publications indicate 50%–60% of patients within Federally Qualified Health Centers (FQHCs) in the Midwest suffer from chronic pain. [5, 6] Furthermore, psychosocial variables such as depression, anxiety, and distress, which are common in underserved patients, mediate the transition from acute to chronic pain, and amplify existing pain complaints. [7, 8]
Patients with high-impact chronic spinal pain use opioids at a rate almost four times that of those with low-impact pain, and on average use over five times the morphine equivalent dose (MED). [9] The opioid epidemic has necessitated integrating safe, effective, and evidence-based treatments into chronic pain management, as prescription opioids have lacked efficacy and contributed to adverse effects and deaths. [10–12 ]American College of Physicians guidelines recommend non-pharmacologic (e.g. therapies routinely provided by chiropractors and physical therapists) and non-opioid pharmacologic treatment for low back pain, but high out-of-pocket expenses create access barriers to these evidence-based therapies for many low-income patients. [13–15 ] Average out-of-pocket expenses for one episode of low back pain can range between $150–720 for chiropractic or physical therapy with commercial healthcare insurance, and much greater without insurance. [14] In contrast, a one-month supply of generic opioids costs $10–15. [13]
Treatments provided by chiropractors are safe and effective in managing spinal pain, resulting in lower pain scores and increased patient satisfaction with minimal adverse events. [5, 21–25 ] Integrating chiropractic care in a low-income, urban clinic in Winnipeg, Canada not only reduced spinal and extremity pain, but also decreased opioid use. [20] There is also a foundation for on-site integration for pain management at the primary care level within the community health center (CHC), with proven feasibility and patient satisfaction, and opportunity for inter-professional collaboration. [5, 21–25 ] However, there are few quantitative studies of pain management integration into CHCs.
Our study site had recently implemented a multidisciplinary chronic pain team and chiropractic care to improve pain management and offer patients non-opioid treatments. Thus, we designed an observational study at a CHC with two distinct chronic pain interventions to determine the impact on treatment of chronic spinal pain and disability.
Methods
Design
This was a prospective observational pilot study with the primary objective of quantifying a change in pain scores after 6–12 months of two separate interventions within the study site (pain team and chiropractic team). Anticipated enrollment was 30 participants per intervention. The primary outcome was a change from baseline of the Pain Disability Questionnaire (PDQ), the study tool. Secondary outcomes were reduction of opioid dose by MED. Analysis was performed on additional patient variables to determine potential associations with PDQ scores.
Study Tool
The PDQ is a validated instrument to assess function and disability as affected by pain. Scores on the PDQ correlate stronger to many physical and psychosocial measures of human function (e.g. depression, pain intensity) and work disability than more commonly used low back pain outcome instruments, [27] The PDQ includes 15 questions across functional and psychosocial domains. Scores are divided into five distinct categories: no disability (score of 0); mild (scores 1–70); moderate (scores 71–100); severe (scores 101–130); and extreme (scores 131–150). Strengths of the PDQ include the effect of psychosocial factors on pain assessment as well as the proven linear relationship between scores and return to work and work retention. [26, 27]
Participants and Study site
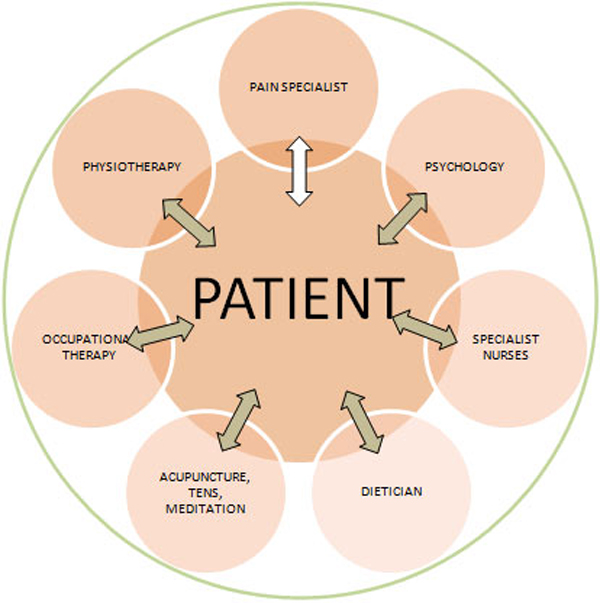
Affinia Healthcare (AHC) is a FQHC treating an underserved population in St. Louis, MO with five clinical sites that serves more than 40,000 individuals annually. At the time of the study, AHC had integrated two distinct interventions to address chronic pain: multidisciplinary chronic pain team and chiropractic care. The pain team consisted of a primary care physician (PCP), behavioral health consultant, clinical nurse, and clinical pharmacist. The chiropractic team consisted of faculty professors and students from Logan University in Chesterfield, MO; on-site chiropractic care was made feasible via an academic affiliation agreement.
Patients were referred internally by providers to either or both interventions based on patient and provider preference. The goal of the pain team was to improve chronic pain, increase psychosocial support, and decrease or wean opioid use for pain. Chiropractic care consisted of patient education, rehabilitation exercises and other home care advice, and manual therapy consisting of low or high-velocity-low-amplitude spinal manipulation and myofascial treatment. Treatment selection for each patient was at the discretion of the attending chiropractor and patient preference.
The pain team provided a reimbursable service covered by private and public insurances with copayments comparable to primary care visits. Patients paid a sliding fee for chiropractic consultations and follow-ups ($12–22 per visit). At the time of study, chiropractic was not a covered service by Missouri Medicaid.
When research staff were available, participants were consented and enrolled at the time of first appointment to either intervention. Inclusion criteria were patients with chronic spinal pain (back and neck) as diagnosed by PCP who were referred to either intervention. The only exclusion criteria was an active cancer diagnosis. This study was approved by the Logan University IRB.
Data collection
Following consent and enrollment, participants completed a baseline PDQ prior to the intervention. Participants continued to see the intervention group (pain team, chiropractic, or both), PCP, and other medical providers as determined by their health providers independent of this study’s protocol. Another PDQ was collected at an intended 6 – 12 months later, after which participants were given a $20 gift card.
Demographic information was collected by manual chart review in the electronic medical record NextGen (NextGen EHR, Nextgen Healthcare, Inc. Irvine, CA, USA). Variables collected included age, sex, race, BMI, insurance type, preferred language, presence of another pain diagnosis (e.g. knee pain), active mental health diagnosis (including substance abuse), diagnosis of hypertension or diabetes, and MED; one post-hoc variable was recorded: timing of follow-up survey in relation to the 2019 coronavirus (COVID-19) pandemic, defined as before/after March 1, 2020, when cases and awareness in the United States started increasing. Intervention type was analyzed as an independent variable since the study was not designed as a comparison of interventions.
Data Analysis
Stata 16.0 (StataCorp, LLC, College Station, TX, USA) was used for statistical analysis. PDQ scores at baseline and follow-up were tested for statistical significance using paired t-tests. Univariate analysis was performed on individual categorical variables and change in PDQ using two-sample t-tests. Multivariate linear regression was used to determine associations of these factors to the outcome. Variables were excluded from regression models if there was a subgroup size of six or less.
Results

Table 1

Table 2 From August 2018 – September 2019, 42 participants with chronic spinal pain were enrolled across all clinical sites at AHC. This included 12 of the 71 new patients seen by the pain team and 20 of the 779 new patients with spinal pain seen by the chiropractic team. Data is not available to distinguish how many of these 779 were eligible for enrollment with chronic spine pain versus acute back or neck pain. Enrollment ended before the targeted number due to elapsed time. Thirty-five individuals (35/42, 83%) completed the follow-up PDQ and were included for analysis; twenty were seen by the chiropractic team, 12 were seen by the pain team, and three saw both. Mean follow-up occurred at 11 months after the baseline assessment (range 6 – 21 months). Demographic information of these participants is included in Table 1.
Mean PDQ scores of selected participants and subgroups are presented in Table 2. The mean baseline PDQ score was 92.4 +/– 6.1 and the mean follow-up PDQ was 81.9 +/– 7.7, resulting in a mean change from baseline of –10.6 (95% CI 1.2 - –22.3, P = .08), where a negative value indicates an improved pain score. On univariate analysis, participation in the chiropractic team (P < .01), absence of another pain diagnosis (P = .02), and completion of the follow-up survey before COVID-19 (P < .01) were statistically significant predictors of better improvements in PDQ scores. However, after adjusting for all variables using multivariate linear regression, only COVID-19 and intervention type remained significant predictors of the outcome; specifically, completing the follow-up survey before COVID-19 (P < .01) and enrollment in the chiropractic team (P = .01) were associated with a larger improvement in PDQ after intervention. Regression coefficients (b) and p-values are listed in Table 2.
Only three participants of the initial 42 had an active opioid prescription, and two of these participants (2/35, 6%) completed both surveys. Both of the participants had been weaned completely from opioids at follow-up, with an increase (ie, worsening) in PDQ of 2 and 31 (mean = 16.5).
Discussion
This pilot study demonstrates efficacy in improving chronic spinal pain and disability utilizing a unique two-intervention approach within one CHC in a sample of 35 individuals. Both interventions are highly utilized by PCPs at the study site, and are generalizable programs that could be adopted by other health centers or practices. Integrating chronic pain care within the CHC offers the advantage of accessible and trustworthy options for services that would otherwise be left to the PCP or externally referred. Although cost of care was not a study outcome, integrating contemporaneous back pain management at the primary care level has demonstrated per patient and downstream societal cost savings, along with improved health outcomes. [28–31] Most (89%) of the enrolled patients had private or public insurance. Therefore, these results may inform decision-making to expand coverage options for the management of chronic pain within the medical home.
The study did not include a qualitative assessment, but both interventions continue to be a long-term plan of the organization. Thus, this is an observational study of a CHC-academic partnership thriving by providing on-site chiropractic services. While this may not be generalizable to some private and/or small practices, this model is a feasible option for larger health centers or medical homes where there may be local academic institutional support. This type of partnership streamlines evidence-based practice to the CHC and its patients while providing a unique but reliable environment for academic endeavors.
Although this was an observational study with no intent of randomization, there was an association with a larger score decrease (improvement) with those in the chiropractic group compared to those in the pain team. The purpose of the study was to analyze the health center’s approach to chronic pain as opposed to determine which intervention is more effective. In this manner, the study site’s system is effective at reducing pain scores, and those scores remained lower at a mean follow-up of 11 months. Despite the primary outcome not achieving statistical significance (mean change in PDQ –10.6, P = .08), those in the chiropractic group had a significant decrease in PDQ scores (P = .01), with a mean score in the range of severe disability (71–100) changing to a score in mild/moderate disability (less than 70). This is important, as the validation studies of the PDQ found improved work retention and return to work in this mild/moderate disability category. [26, 27]
Discovering the post-hoc effect of COVID-19 on PDQ scores has two important implications. First, the mean change in PDQ for both interventions prior to COVID was much greater than the aggregate, likely blunting the true effectiveness of this pain management system. Second, the pandemic has a negative association on the perception of pain in a small group of individuals, with a mean decrease in PDQ of 22.6 prior to COVID compared to a mean increase of 12.4 post-COVID (P < .01). Recent work suggests the COVID-19 pandemic correlates with lower psychological well-being and more anxiety and depression. [32] Unsurprisingly, this new stressor had a significant influence on pain, and subsequently, patient outcomes.
This study has limitations. The small sample size (n = 35) limits implications of both the primary outcome and secondary analyses. Multivariate analysis is particularly limited, and inferences about subgroups are subject to type I error. The study is limited by selection bias, as PCPs referred to the intervention they thought most appropriate for their patients. A small percentage of patients in each intervention gave consent for the study. One reason for this is lack of research staff support and time in this real-world setting. However, participant mistrust, indifference, and/or misunderstanding of research is possible. Future studies could analyze reasons for low participation of CHC/FQHC patients, and improve enrollment.
Randomized studies could be considered to determine true comparisons of different pain interventions, but was not an option at the study site. There was not a comparison group, and thus, the data relies only on measurements of the interventions. Furthermore, a relatively small percentage of patients on opioids enrolled, so the secondary outcome could not be assessed. Regardless, both participants on chronic opioids successfully weaned and discontinued their medication by the end of the study.
While there was minimal crossover among patients enrolled in the study (3/35 utilized both chiropractic care and pain team), it is likely that patients from both groups accessed similar services at the CHC such as PCPs, nurse educators, pharmacists, and social workers. This overlap of services might be different among the intervention groups, but was not studied. This represents a real-world challenge of designing clinical trials at CHCs where patient populations are accustomed to choosing their services rather than being allocated to them.
Finally, the patient population is representative of one FQHC, with a large population of low-income and uninsured patients. While this is the target population of the study site and one of the purposes of this study, it does limit external validity.
Conclusion
Integrating chronic pain interventions within the medical home was effective in treating chronic pain, improving disability, and reducing opioid prescriptions in a small sample of patients. Partnering with academic universities provides access to services such as on-site chiropractic care. This study offers important data for one potential solution in the future of chronic pain management within CHCs.Acknowledgments
The authors would like to acknowledge all participants in the study, the study site, Affinia Healthcare, and the funding source, Logan University.
Author Contributions:
All authors participated in the design and writing of the manuscript. PB and CP were responsible for data collection and analysis.
Declaration of Conflicting Interests:
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding:
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Logan University has funded this study, specifically through a small grant for participant incentives.
References:
Dahlhamer J, Lucas J, Zelaya C, et –al.
Prevalence of Chronic Pain and High-Impact Chronic Pain
Among Adults - United States, 2016
MMWR Morb Mortal Wkly Rep. 2018 (Sep 14); 67 (36): 1001-1006Hoy D, March L, Brooks P, et al.
The Global Burden of Low Back Pain: Estimates from the Global Burden of Disease 2010 study
Ann Rheum Dis. 2014 (Jun); 73 (6): 968–974Hoy D, March L, Woolf A, et al.
The Global Burden of Neck Pain: Estimates From the Global Burden of Disease 2010 Study.
Ann Rheum Dis. 2014 (Jul); 73 (7): 1309–1315Janevic MR, McLaughlin SJ, Heapy AA, Thacker C, Piette JD.
Racial and socioeconomic disparities in disabling chronic pain: findings from the health and retirement study.
J Pain. 2017;18:1459-1467Smith LJ, Johnson-Lawrence V, Andrews M, Parker S.
Opportunity for interprofessional collaborative care-findings from a sample of federally qualified
health center patients in the Midwest.
Public Health. 2017;151:131-136St. Louis Regional Health Commission.
Chronic Pain Prevention and Treatment Policy Paper.
St. Louis, MO; 2019Meints SM, Edwards RR.
Evaluating psychosocial contributions to chronic pain outcomes.
Prog Neuropsychopharmacol Biol Psychiatry. 2018;87:168-182Lee H, Hübscher M, Moseley GL, et al.
How does pain lead to disability A systematic review and meta-analysis of mediation studies in people
with back and neck pain. Pain. 2015;156:988-997Herman PM, Broten N, Lavelle TA, Sorbero ME, Coulter ID.
Health care costs and opioid use associated with high-impact chronic spinal pain in the United States.
Spine. 2019;44:1154-1161Kuehn BM.
AHRQ: little evidence for opioids in managing long-term chronic pain.
JAMA. 2014;312:1185Dowell D, Haegerich TM, Chou R.
CDC Guideline for Prescribing Opioids for Chronic Pain: United States, 2016
Morbidity and Mortality Weekly Report
Recommendations and Reports Vol. 65 No. 1 March 18, 2016Centers for Disease Control and Prevention.
Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008.
MMWR Morb Mortal Wkly Rep. 2011;60:1487-1492Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Goertz CM, George SZ.
Insurer Coverage of Nonpharmacological Treatments for Low Back Pain-Time for a Change
JAMA Netw Open. 2018 (Oct 5); 1 (6): e183037Sandstrom R.
Utilization of ambulatory physical therapy and occupational therapy by the United States population, 2009-2013.
J Allied Health. 2017;46:225-231Goertz CM, Salsbury SA, Long CR, et al.
Patient-centered Professional Practice Models for Managing Low Back Pain in Older Adults:
A Pilot Randomized Controlled Trial
BMC Geriatr. 2017 (Oct 13); 17 (1): 235Walker, BF, Hebert, JJ, Stomski, NJ et al.
Outcomes of Usual Chiropractic.
The OUCH Randomized Controlled Trial of Adverse Events
Spine (Phila Pa 1976). 2013 (Sep 15); 38 (20): 1723–1729Johnson C.
Poverty and human development: contributions from and callings to the chiropractic profession.
J Manipulative Physiol Ther. 2007;30:551-556Davis MA, Mackenzie TA, Coulter ID, Whedon JM, Weeks WB.
The United States Chiropractic Workforce: an alternative or complement to primary care .
Chiropr Man Therap. 2012;20:35Passmore S, Manansala C, Malone Q, Toth EA, Olin GM.
Opioid usage patterns, patient characteristics, and the role of chiropractic services in a publicly
funded inner city health care facility.
Spine J. 2019;19:S78-S79Hurstak E, Chao MT, Leonoudakis-Watts K, Pace J, Walcer B, Wismer B.
Design, implementation, and evaluation of an integrative pain management program in a primary care safety-net clinic.
J Altern Complement Med. 2019;25:S78-S85Dorflinger LM, Ruser C, Sellinger J, Edens EL, Kerns RD, Becker WC.
Integrating interdisciplinary pain management into primary care: development and implementation of a novel clinical program.
Pain Med. 2014;15:2046-2054.Wiedemer NL, Harden PS, Arndt IO, Gallagher RM.
The opioid renewal clinic: a primary care, managed approach to opioid therapy in chronic pain patients at risk for substance abuse.
Pain Med. 2007;8:573-584.Purcell N, Zamora K, Tighe J, Li Y, Douraghi M, Seal K.
The integrated pain team: a mixed-methods evaluation of the impact of an embedded interdisciplinary pain
care intervention on primary care team satisfaction, confidence, and perceptions of care effectiveness.
Pain Med. 2018;19:1748-1763.Kennedy LC, Binswanger IA, Mueller SR, et al.
Those conversations in my experience don’t go well: a qualitative study of primary care provider experiences
tapering long-term opioid medications.
Pain Med. 2018;19:2201-2211.Gatchel RJ, Mayer TG, Theodore BR.
The pain disability questionnaire: relationship to one-year functional and psychosocial rehabilitation outcomes.
J Occup Rehabil. 2006;16:75-94.Anagnostis C, Gatchel RJ, Mayer TG.
The pain disability questionnaire: a new psychometrically sound measure for chronic musculoskeletal disorders.
Spine. 2004;29:2290-2303Hill JC, Whitehurst DGT, Lewis M, et al.
Comparison of Stratified Primary Care Management For Low Back Pain With Current
Best Practice (STarT Back): A Randomised Controlled Trial
Lancet. 2011 (Oct 29); 378 (9802): 1560–1571Foster NE, Mullis R, Hill JC, et al.
Effect of stratified care for low back pain in family practice (IMPaCT Back):
a prospective population-based sequential comparison.
Ann Fam Med. 2014;12:102-111.Whitehurst DG, Bryan S, Lewis M, Hay EM, Mullis R, Foster NE.
Implementing stratified primary care management for low back pain: cost-utility analysis alongside a prospective,
population-based, sequential comparison study.
Spine. 2015;40:405-414.Wayne PM, Buring JE, Eisenberg DM, et al.
Cost-effectiveness of a team-based integrative medicine approach to the treatment of back pain.
J Altern Complement Med. 2019;25(suppl 1):S138-S146.Vindegaard N, Eriksen Benros M.
COVID-19 pandemic and mental health consequences: systematic review of the current evidence [published online May 30, 2020].
Brain Behav Immun. doi:10.1016/j.bbi.2020.05.048
Return to SPINAL PAIN MANAGEMENT
Return to INTEGRATED HEALTH CARE
Return NON-PHARMACOLOGIC THERAPY
Since 10-24-2020


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |