

Vascular Ultrasound Measurements After Atlas Orthogonal
Chiropractic Care in a Patient With Bow Hunter SyndromeThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Chiropractic Medicine 2018 (Dec); 17 (4): 231–236 ~ FULL TEXT
OPEN ACCESS Robert J. Rectenwald, DC, Carolyn M. DeSimone, DC, and Roy W. Sweat, DC
Clinic System,
College of Chiropractic,
Life University,
Marietta, Georgia.OBJECTIVE: This case report describes chiropractic treatment for a patient diagnosed with bow hunter syndrome with transient vision loss (TVL).
CLINICAL FEATURES: A 39-year-old woman presented to a chiropractic clinic with hand and arm numbness that began after she was injured in a motor vehicle collision 18 months earlier. The primary symptom was transient vision loss (TVL) that began 3 days after the motor vehicle collision. At that time, she had been diagnosed with bow hunter syndrome using dynamic angiography findings. She had previously declined surgery recommended by her attending neurosurgeon at a local hospital.
INTERVENTION AND OUTCOME: The patient was treated using atlas orthogonal chiropractic technique for 8 visits over a 6-week period. Examination before and the after the initial treatment included cervical radiographic analysis and vascular ultrasound measurement of the right and the left vertebral artery (VA). After the initial spinal manipulation, there was an improvement in blood flow volume of 8.2% in the left VA and 22.2% in the right VA. There was improvement of the symptom of TVL and a measured reduction of rotational misalignment of the first and second cervical vertebra on the radiographic views. After 6 weeks, the patient's perception of TVL was absent.
CONCLUSION: A patient with transient vision loss (TVL) improved under chiropractic care using atlas orthogonal technique.
KEYWORDS: Chiropractic; Ultrasonography; Vertebrobasilar Insufficiency
From the FULL TEXT Article:
Introduction
Bow hunter syndrome (BHS) is also known as bow hunter stroke and rotational vertebral artery syndrome. Bow hunter syndrome is a rare cause of vertebrobasilar insufficiency; the mechanism was first postulated in cadaveric studies of the early to mid–20th century. [1, 2] Sorensen coined the term in 1978 based on the symptoms occurring with the activity of archery. [3] Bow hunter syndrome is most commonly a result of a mechanical compression of the vertebral artery (VA), except for rare cases where compression results from intrinsic vascular problems such as atherosclerosis. [4] The resultant occlusion or stenosis of the VA occurs with head rotation and typically in the dominant VA. Because the occlusion is dynamic, the symptoms are typically transient, dependent on head position. The most commonly reported symptoms are syncope, near-syncope, drop attack, vertigo, dizziness, and impaired vision. Other less commonly reported symptoms include dysarthria, dysphasia, diplopia, nystagmus, numbness, paresthesia, nausea, headache, neck pain, arm pain, tinnitus, and ataxia. [4–6] Transient vision loss (TVL) and blindness have also been reported in some cases. [4, 5, 7–9] Bow hunter syndrome studies are limited to case studies and case series. The largest overview of BHS to date was published by Jost and Daily [7] in 2015, in which 126 cases were described and categorized and in which a variety of causes, sites of stenosis, and treatment regimens are described. The condition can result in permanent neurologic deficit if left undiagnosed. [10]
Testing methods used in diagnosis and assessment include dynamic computed tomography imaging, single photon emission computed tomography, and transcranial Doppler ultrasonography. [11–13] Dynamic range-of-motion angiography is considered the gold standard for diagnosis. [11] The various physical findings reported as causes of BHS symptoms include osteophytes within the transverse foramina, suboccipital osseous prominences, accessory ossicles, herniated disc, uncovertebral joint instability, spondylolisthesis, thickening of the atlanto-occipital membrane, fibrous bands, neck muscle hypertrophy, and joint subluxation. In a sizeable percentage of cases, the site of occlusion is at C2 and above. [4, 6, 12] Because of the anatomic location, the VA is affected by head motion, especially rotation. Consequently it is vulnerable to space-occupying structural changes in the cervical spine, which occurs commonly in the transverse foramen. The anatomic relationship of VA to the cervical vertebrae is that the VA typically ascends through the vertebral transverse foramina of C6– C1, then bends posteromedially to run over the C1 posterior arch through the groove of the VA of C1, and finally bends superiorly to enter the cranial cavity through the foramen magnum.
Bow hunter syndrome is considered a rare pathologic condition, and as such, guidelines for treatment have not yet been established. [13, 14] Surgery is the most common treatment method reported in the literature. Common among the surgical procedures are decompression of the VA by transversectomy, vertebral fusion, and removal of osteophytes or other offending hard or soft tissue structures. Some cases have been successfully treated using endovascular stent placement. [11] Conservative treatment methods reported include neck bracing to limit the degree of head rotation and halter traction. In some cases, aspirin and other anticoagulant drugs are used. [4]
The purpose of this case study is to describe the change in VA blood flow and patient perception of improvement of TVL after a chiropractic care in a patient diagnosed with BHS. The possible relationship between rotational misalignment of the first and second cervical vertebrae (C1, C2) and VA blood flow is also discussed.
Case Presentation
A 39–year-old woman presented to a chiropractic clinic seeking treatment for constant arm and hand numbness (without pain), with concomitant prior BHS diagnosis and vision symptoms, which were disclosed during the history taking. The episodes of vision loss with head rotation and constant arm and hand numbness had persisted for 18 months.
The onset of the complaints and the diagnosis of BHS was a result of a motor vehicle collision 18 months earlier. She presented at that time for a medical evaluation with complaints of neck pain and bilateral arm numbness that began immediately after her vehicle was stuck from behind by a truck estimated to be traveling at 40 mph. The patient was examined at a hospital emergency department, given prescriptions for pain medication and a nonsteroidal anti-inflammatory agent, and then released. Within 3 days of the accident, she began experiencing episodes of vision loss that occurred whenever she turned her head to the right or left. Subsequently she reported to a second medical center for evaluation of the vision loss, which included radiographs, computed tomography scans, and vascular studies. Dynamic angiography findings indicated stenosis of the right VA at the level of the first and second cervical vertebrae, leading to the diagnosis of BHS. A surgical procedure was recommended as the treatment option. No other treatment options were offered. The patient declined the surgery because of the stated risk, which included possible paralysis.
At the chiropractic clinic, examination revealed that cervical rotation was limited by cervical pain. Cervical range of motion (CROM) was performed using a goniometer. Right rotation was measured at 32° (±5°) and left rotation at 28° (±5°). During the CROM, a gradual loss of vision was also perceived by the patient after 4 seconds, timed with a stopwatch. After the head was rotated to neutral position, the patient reported her vision gradually returned to normal within 10 seconds as timed with a stopwatch. Neurologic testing was unremarkable except for hypoesthesia on the right C5 and T1 dermatomes and motor deficit (4/5) of the deltoid muscles bilaterally. Palpation of the posterior cervical superficial soft tissue over the region of the C1 posterior arch elicited sharp pain bilaterally below the base of the skull. Palpation over the facet joints of C4–C6 and T1–T4 also elicited sharp pain bilaterally in the midcervical region. Postural abnormalities were identified using a postural spinal analysis machine, known as S.A.M., (MeyerDC, Hudson, Ohio). Measured abnormalities included right head tilt (8 mm), left head rotation (5°), and anterior head translation (12 mm from neutral). Functional leg length inequality (fLLI) at 12 mm on the right was measured using a leg length analysis measurement grid attached to the table-mounted atlas orthogonal (AO) adjusting instrument (Hardy Manufacturing, Atlanta, Georgia).

Figure 1 The adjustment (method of chiropractic spinal manipulative therapy) was based on radiographic analysis according to the AO technique. [15] The patient was informed that the type of chiropractic care to be performed was based on an established technique using a percussive thrust over the first vertebra with no manual rotational manipulation of the neck. The patient would be in a stable, unstressed position (Figure 1). The goals of care and possible benefits expected were improved CROM with reduced arm and hand numbness. In addition, the vascular flow measurement was planned to be performed before and after the first treatment. After a question and answer session, the patient consented to proceed with the treatment.
Preadjustment Radiographic Analysis [15]
A cervical radiographic examination was performed, consisting of neutral lateral, anteroposterior open mouth (APOM), and anteroposterior lower cervical views for a general assessment. The nasium and vertex views were also taken. A chiropractic radiologist reported all cervical views to be negative for degenerative changes or anomalies.
The nasium, vertex, and APOM were analyzed by computer program (Atlas Orthogonal Radiographic Analysis Software 2008, Sweat Institute, Atlanta, Georgia). The analysis yields factors that determine adjusting vectors and patient positioning for AO chiropractic adjustment. The radiographic analysis suggested misalignment of osseous structures in the frontal and horizontal planes.
Factors from the radiographic computer analysis of C1 included the following:
The nasium line-drawing analysis was used to measure atlas displacement in relation to the cranium (cephalic), which is considered the Z plane of the patient’s body (right-handed Cartesian coordinate system).
The vertex line-drawing analysis was used to measure rotational component of the atlas displacement in relation to the cranium which is considered the Y plane.
The APOM line-drawing analysis was used to measure rotational component of the C2 in relation to C1.
Preadjustment Vascular Assessment

Table 1 Vascular testing was performed at the chiropractic clinic by a registered vascular technician sonographer, using ultrasound with a high-frequency linear transducer (Fuji Film/SonoSite, Bothell, Washington). Vascular volume and rate in right VA and left VA were assessed with the head in the neutral position. The study revealed the left VA speed measurement to be 27.6 cm/s, and the volume to be 159 mL/min. The right VA measurement for speed was 29.8 cm/s and for volume was 162 mL/min (Table 1). Vertebral artery flow volume of >200 mL/min were normal values as reported in 2005. [16]
Intervention and Outcome
The treatment plan consisted of chiropractic adjustment (method of chiropractic spinal manipulative therapy) to the C1 vertebra.15
Preadjustment ProtocolLeg Length Observation The fLLI measurement was performed with the patient in the supine position on the adjusting table with the measurement grid.
Palpation of the superficial soft tissue overlying the area of the C1 posterior arch was performed with the patient seated. Palpation elicited sharp pain bilaterally below the base of the skull. Palpation over the facet joints of C4–C6 and T1–T4 also elicited sharp pain bilaterally in the midcervical region.
Chiropractic Procedure
The patient was placed in the side-lying position on the adjusting table. The table mounted AO adjusting instrument was set to a degree angle on the Z axis and to a degree angle on the Y axis dependent on the radiographic measurements, and the stylus of the instrument was positioned over the transverse process of the atlas. The instrument delivered a compressional energy wave or impulse using a stylus that was solenoid powered. At the patient-stylus interface, a portion of this wave energy is transmitted through the superficial tissues to the atlas vertebra. The expected result was a positive change in relative alignment of the cervical vertebra and the cranium.
The adjusting instrument delivered a 6.13–lb percussion force without producing excursion into the neck. [15]
Postadjustment Protocol
After the treatment, the examination procedure was repeated. The expected result was correction of fLLI and resolution or reduction of pain and tenderness with palpation. After the first adjustment only, the nasium and vertex and APOM views were repeated and analyzed to determine whether there was a change in the misalignment. Based on the results of the measurements, modifications to the adjusting instrument setup were made if necessary. The modified measurements were used for all subsequent adjusting.
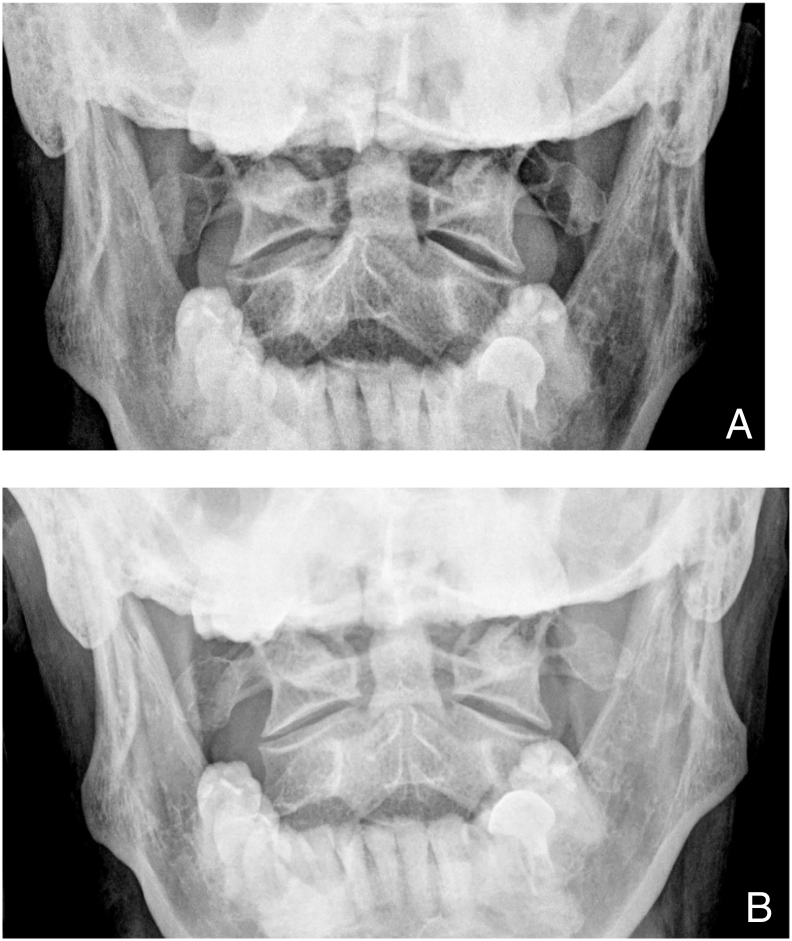
Figure 2 After the first treatment, cervical radiographs were taken and analyzed, and CROM and vascular ultrasound examinations were repeated. Cervical range of motion rotation was improved and measured with a goniometer at 40° (±5°) degrees bilaterally. The onset of patient perceived vision disturbance occurred after 9 seconds in both the right and left rotated position as measured using a stopwatch. Analysis of the APOM radiographic view indicated that misalignment of C1 and C2 in the horizontal plane, relative to rotation, was reduced from 3° to 1° (Figure 2).
Postadjustment Vascular Assessment
The vascular measurements indicated improvement in blood flow volume of 8.2% in the left VA and 22.2% in the right VA (Table 1).
Subsequent Treatment
The patient was evaluated 8 times over a 6–week period with decreasing frequency from 2 times a week for 3 weeks to 1 time a week for 3 weeks. Adjustments were performed on 6 visits when the positive indicators of fLLI and palpatory pain and tenderness were present. After 6 weeks of treatment, CROM was repeated and measured at 42° (±5°) of rotation using a goniometer. The rotated position did not result in any patient-perceived vision abnormality. The patient reported that her arm numbness was improved and occurred infrequently in 10–minute episodes after waking up in the morning. She remained asymptomatic for perceived visual abnormality over the following 3 weeks, at which time she was released from active care. The patient was seen on follow-up visits at 3, 6, and 12 months. The patient reported no symptoms of TVL or numbness and no adverse reactions. The patient provided consent for the publication of this study.
Discussion
Of the BHS cases reported in the literature as of 2015, 36% indicated the site of the stenosis to be at the C1–C2 level. In 34% of those cases with C1–C2 stenosis, a degree of vision impairment was reported. [7] Cases with similarities to this one have been reported in the literature. In one study the patient was a 28–year-old woman with symptoms of arm numbness and vision loss. [6] Another study reported symptoms of episodic bilateral blindness with head rotation. The cause was identified as stenosis caused by hyper-rotation apophyseal joint subluxation. [9] Missori et al [17] reported on a case of atlantoaxial rotatory subluxation resulting in transient blindness after a neck injury. A limited number of published studies cite ultrasonography as a valuable assessment tool. [10, 17]
For the patient in our study, we hypothesize that the rotational component of the vertebral misalignment, as measured by radiographic analysis at the C1–C2 level, may have resulted in pressure and subsequent occlusion of the VA-like findings of Lee, [6] Jost and Dailey, [7] Kawaguchi, [10] and Missori. [17] This occlusion may have been increased with the position of head rotation similar to the study reported by Kawaguchi. [10] The resultant ischemia from blood flow impairment to the visual system may have resulted in the patient-perceived TVL. It is hypothesized that the reduction of rotational misalignment after treatment may have improved VA blood flow with the head in a neutral position. The reduction of rotational misalignment may have also improved VA blood flow with the head in a rotated position, which then may explain the reduction of the patient-perceived TVL. The continued treatment may have been able to further reduce the occlusion and improve VA volume, resulting in resolution of the TVL.
Limitations
Limitations of this study include the absence of dynamic angiography testing after the chiropractic treatment plan was completed. The comparison of pre- and post-treatment angiography results would have provided stronger evidence in support of this postulate. Because we are reporting the findings for only one patient, the results of the treatment that this patient experienced may not necessarily be reproducible for other patients with BHS. Thus this is a case report and is not generalizable to a larger population. More research is needed to determine the association between the osseous alignment of the cervical-occipital area and VA hemodynamics.
Conclusion
A patient with transient vision loss (TVL) improved under chiropractic care using AO technique.
Practical Applications
This study describes one patient’s response to chiropractic care.
Diagnostic ultrasonography may be useful in diagnosis and outcome assessment
in some cases of vertebrobasilar insufficiency.Acknowledgments
The authors thank Kathryn Hoiriis, DC, who reviewed the manuscript and made suggestions for improvement.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): R.J.R., R.W.S.
Design (planned the methods to generate the results): R.J.R., R.W.S.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): R.J.R.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): R.J.R.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): R.J.R., R.W.S.
Literature search (performed the literature search): R.J.R., C.M.D.
Writing (responsible for writing a substantive part of the manuscript): R.J.R., C.M.D.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): R.J.R., C.M.D.
References:
Ford FR.
Syncope, vertigo, and disturbances of vision resulting from intermittent obstruction of vertebral arteries
due to defect in odontoid process and excessive mobility of second cervical vertebra.
Bull Johns Hopkins Hosp. 1952;91(3):168–173Tissington Tatlow WF, Bammer HG.
Syndrome of vertebral artery compression.
Neurology. 1957;7(5):331–340Sorensen BF.
Bow hunter’s stroke.
Neurosurgery. 1978;2(3):259–264Guangxin D, Jiaping X, Jijun S, Yongjun C.
Advances in the pathogenesis, diagnosis and treatment of bow hunter's syndrome:
a comprehensive review of the literature.
Neurol Med Chir (Tokyo) 2016;56(9):580–583Motiei-Langroudi R, Griessenauer CJ, Alturki A, Adeeb N, Thomas AJ, Ogilvy CS.
Bow hunter's syndrome from a tortuous V1 segment vertebral artery treated with stent placement.
World Neurosurg. 2017;98:878.e11–878.e878Lee V, Riles TS, Stableford J, Berguer R.
Two case presentations and surgical management of bow hunter's syndrome associated with bony abnormalities
of the C7 vertebra.
J Vasc Surg. 2011;53(5):1381–1385Jost GF, Dailey AT.
Bow hunter's syndrome revisited: 2 new cases and literature review of 124 cases.
Neurosurg Focus. 2015;38(4):E7Cornelius J, George B, Oka DN, Spiriev T, Steiger H, Hanggi D.
Bow hunter’s syndrome caused by dynamic vertebral artery stenosis at the cranio-cervical junction—
a management algorithm based on a systematic review and clinical series.
Neurosurg Rev. 2012;35(1):127–135Kageyama H, Yoshimura S, Lida T.
Juvenile cerebral infarction caused by bow hunter's syndrome during sport: two case reports.
Department of Neurosurgery, Hyogo College of Medicine.
Neurol Med Chir (Tokyo) 2016;56(9):580–583Kawaguchi T, Fujita S, Hosoda K, Shibata Y, Iwakura M, Tamaki N.
Rotational occlusion of the vertebral artery caused by transverse process hyperrotation and unilateral
apophyseal joint subluxation. Case report.
J Neurosurg. 1997;86(6):1031–1035Yeh J, Lin Y, Po H.
A case of bow hunter’s stroke caused by non-dominant vertebral artery.
Acta Neurol Taiwanica. 2005;14(2):69–73Rastogi V, Rawls A, Moore O.
Rare etiology of bow hunter’s syndrome and systematic review of literature.
J Vasc Interv Neurol. 2015;8(3):7–16Iguchi Y, Kimura K, Shibazaki K, Iwanaga T, Ueno Y, Inoue T.
Transcranial Doppler and carotid duplex ultrasonography findings in Bow hunter's syndrome.
J Neuroimaging. 2006;16(3):278–280Darkhabani M, Thompson M, Lazzaro M, Taqi M, Zaidat O.
Vertebral artery stenting for the treatment of bow hunter’s syndrome: report of 4 cases.
J Stroke Cerebrovasc Dis. 2012;21(8):908-e1–908-e5Sweat R, Sweat M. 11th ed.
Sweat Institute; Atlanta, GA: 2016.
Atlas Orthogonal Chiropractic ProgramAcar M, Degirmenci B, Yucel A, Albayrak R, Haktanir A, Yaman M.
Comparison of vertebral artery velocity and flow volume measurements for diagnosis of vertebrobasilar
insufficiency using color duplex sonography.
Eur J Radiol. 2005;54(2):221–224Missori P, Marruzzo D, Peschillo S, Domenicucci M.
Clinical remarks on acute post-traumatic atlanto-axial rotatory subluxation in pediatric-aged patients.
World Neurosurg. 2014;82(5):e645–e648
Return to BOW HUNTER'S STROKE
Return to CHIROPRACTIC TECHNIQUE
Since 1-17-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |