FROM:
J Electromyo and Kinesio 2012 (Oct); 22 (5): 740–746 ~ FULL TEXT
Walter Herzog, PhD, Tim Leonard, PhD, Symons B, Conrad Tang, DC, Wuest S.
Faculty of Kinesiology,
University of Calgary,
Calgary, Canada.
walter@kin.ucalgary.ca.
FROM:
J Electromyogr Kinesiol 2012
Spinal manipulative therapy (SMT) has been recognized as an effective treatment modality for many back, neck and musculoskeletal problems. One of the major issues of the use of SMT is its safety, especially with regards to neck manipulation and the risk of stroke. The vast majority of these accidents involve the vertebro-basilar system, specifically the vertebral artery (VA) between C2/C1. However, the mechanics of this region of the VA during SMT are unexplored. Here, we present first ever data on the mechanics of this region during cervical SMT performed by clinicians. VA strains obtained during SMT are significantly smaller than those obtained during diagnostic and range of motion testing, and are much smaller than failure strains. We conclude from this work that cervical SMT performed by trained clinicians does not appear to place undue strain on VA, and thus does not seem to be a factor in vertebro-basilar injuries.
From the FULL TEXT Article:
Introduction
Spinal manipulative therapy (SMT) has been recognized as an
effective treatment modality for many back, neck and musculoskeletal
problems (Haldeman, 1986; Herzog, 2000a). It has received
wide-spread acceptance in a variety of disciplines including chiropractic,
physiotherapy, nursing, and mainstream health care. However,
despite its surge in popularity as a cost-effective treatment
modality, there is little basic research as to the beneficial mechanisms
underlying SMT (Herzog, 2010).
Spinal manipulative therapy typically consists of a high-speed,
low-amplitude thrust delivered by a practitioner to a specific landmark
on a patient’s body. We and others, have quantified the force–
time histories of SMTs in a variety of settings and for a variety of
clinical problems (Conway et al., 1993; Downie et al., 2010; Forand
et al., 2004; Herzog, 2000a; Hessel et al., 1990; Triano, 2000). Several
results have emerged from these studies:
(i) the forces applied
by a given clinician are fairly consistent, but they vary dramatically
across clinicians and location of application with peak forces ranging
from approximately
200 N (44 lbs) to values of up to 1400 N
(308 lbs);
(ii) the speed of the treatment thrust is consistent (within
about 100–200 ms for
experienced clinicians) (Herzog, 2000a); and
(iii) the forces applied by male and female clinicians are similar
(Forand et al., 2004),
as are the forces applied to patients or non-patients
subjects in a laboratory setting
(Symons et al., in Press), but
the forces applied on cadaveric specimens (which
have been used
to study the potential injurious effects of SMTs) are significantly
greater and are applied significantly faster than the forces applied
to patients and non-patient control subjects (Symons et al., in
Press).
Forces applied during SMT have been shown to elicit a variety of
mechanical, biological and physiological responses including relative
movements of the intervertebral joints (Gál et al., 1997a,b),
muscle reflex responses (Dishman and Bulbulian, 2000; Dishman
and Burke, 2003; Floman et al., 1997; Gibbons et al., 2000; Herzog,
2000b, 2010; Herzog et al., 1999; Lehman et al., 2001; Suter et al.,
2005, 2009), changes to the blood biochemistry (Brennan et al.,
1991; Triano et al., 1991), and cavitation of joints (Cascioli et al.,
2003; Conway et al., 1993).
Although the total forces during SMTs can be very high, these
forces are typically distributed across a large contact area which
increases with increasing forces because of the soft tissue contacts
between patient and clinician (Herzog et al., 2001), thereby reducing
the local forces to 5–10 N (1–2 lbs) for typical thoracic manipulations.
Nevertheless, there has been increased interest over the
past three decades to elucidate the possible damaging effects of
SMT forces on internal tissues (Cote et al., 1994; Haldeman et al.,
2001; Haldeman and Rubinstein, 1992a,b; Ianuzzi and Khalsa,
2005; Paciaroni and Bogousslavsky, 2009; Powell et al., 1993;
Rubinstein, 2008; Rubinstein and Haldeman, 2001; Terrett and
Kleynhans, 1980). One of the major issues of the use of SMT is its
safety, especially with regards to neck manipulation and the risk
of stroke (Lee et al., 1995; Paciaroni and Bogousslavsky, 2009;
Rubinstein, 2008; Wuest et al., 2010). Although the estimates of
stroke associated (but not necessarily caused) by SMT is small –
about one in a million (Hurwitz et al., 1996) – the severity and
irreversible nature of such accidents makes this a material risk
(Herzog and Symons, 2002; Symons et al., 2002).
The vast majority of these accidents involves the vertebro-basilar
system, specifically the vertebral artery (VA) between C2/C1
and the cephalad/ distal loop as the VA exits the C1 foramen transversarium
and travels to the foramen magnum (Haldeman et al.,
1999). Because of the specific anatomy of the VA in that region,
it has been assumed that the VA experiences considerable stretch
during extension and rotation of the neck, which may lead to
hemodynamic occlusions and damage to the VA, predisposing the
patient to stroke (Herzog and Symons, 2002; Symons et al.,
2002). However, recent evidence suggests that such damage
appears unlikely in the distal extra-cranial loop of the VA (between
C1 and the foramen magnum) and the proximal/caudal loop
between C6 and VA’s origin from the subclavian artery (Austin
et al., 2010; Herzog and Symons, 2002; Symons et al., 2002), but
the regions between C1 and C6 remain unexplored, except for
some preliminary data (Wuest et al., 2010).
Here, we review the results of existing studies on human VA
strains during high-speed, low-amplitude SMTs administered by
qualified clinicians and compare them to the strains encountered
during full range of motion (ROM) tests, and furthermore, add
the summarized results of unpublished works from strains
measured from all sections of 8 VAs using data from 3 clinicians,
resulting in a total of 3034 segment strains obtained during SMTs
and 2380 segment strains obtained during full ROM testing.
Methods
Subjects
 Table 1
Table 1
|
Tests were performed on a total of 12 human cadavers. Two embalmed
cadavers were initially used for pilot testing and evaluation
of all measurements (not included in the results), and 10 fresh,
unembalmed human cadavers were used for measurements of
strains in 16 VAs. Five of these specimens and 6 VAs were used for
measurements of the extra-cranial loop of the VA (from C1 to the
foramen magnum and the proximal/caudal loop (from C6 to the subclavian
artery) (Herzog and Symons, 2002; Symons et al., 2002)
(Cadavers 1–5; Table 1), and four of the cadavers and corresponding
8 VAs were used for measurements throughout the VA (from the
foramen magnum to the origin of VA at the subclavian artery)
(Cadavers 6–9; Table 1). One specimen and corresponding arteries
were excluded from analysis (as were some individual segments)
when strain measurements could not be obtained for technical reasons.
The details of the cadaveric specimens are given in Table 1.
VA dissection
The VA was approached by blunt dissection using an anterolateral
approach as described previously (Symons et al., 2002). Care
was taken to leave all structures intact while exposing the VA.
Specifically, no ligaments, muscles or bones were cut to preserve
the in situ mechanical behavior of the VAs as much as possible.
Range of motion (ROM) testing and spinal manipulative treatments
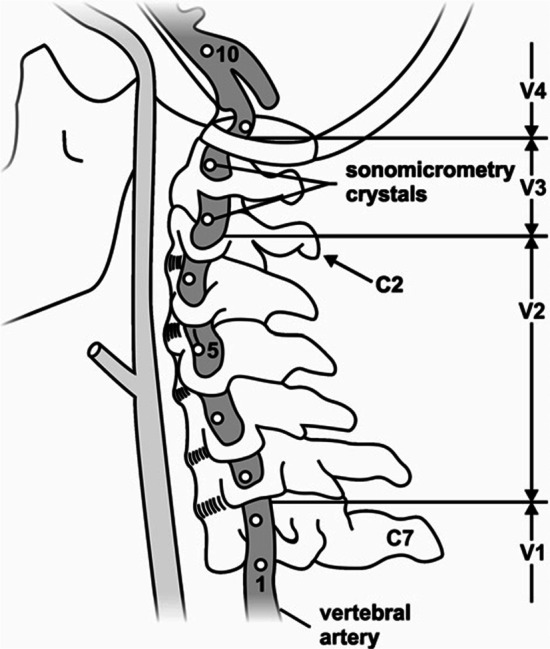
 Figure 1
Figure 1
 Figure 2
Figure 2
|
ROM testing was performed in flexion, extension, rotation and
lateral bending (Figure 1). ROM was established by moving the head
passively from the neutral position (head and neck aligned
straight; Figure 1A) to the point where no further movement was possible
(Figure 1B – end range of rotational movement). Following that,
a Houle’s vertebro basilar insufficiency test was performed by placing
the head in a rotated/extended position. All asymmetric tests
were performed bilaterally (i.e. rotation to the left and right). The
SMTs consisted of a diversified lateral/rotary manipulation with a
second metacarpal contact specifically against the articular pillar
with the cadaver supine, and also a pure lateral manipulation with
the force applied in an essentially lateral direction to the neck
(Figure 1C). These SMTs were delivered at levels C1/C2, C3/C4, and
C6/C7 while measuring strains in all segments that were instrumented
on the side of manipulation and the contralateral side.
All ROM testing was repeated three times and was performed
bilaterally; all SMTs were repeated three times, on all levels and
both sides of the neck. Therefore, for a cadaver instrumented as
shown in Figure (2 – markers 2–9) up to 7 strain measurements
could be made for each test, for a total of 252 strain measurements
(3 repeat tests 3 locations 2 treatment techniques 2 sides of
treatments 7 vertebral segments) for the SMTs alone and a single
clinician working on a single VA. Testing of the first 6 VAs was performed
by a single clinician (Symons et al., 2002), while measurements
on the last 8 VAs were performed by 3 clinicians. For the last
8 VAs tested, strain measurements were accompanied by measurements
of the contact forces, and the VAs were injected with
ultrasound gel to maximize the strain signals (through sonomicrometry)
and to restore the VAs to a natural, fluid filled shape (Wuest
et al., 2010).
All ROM and SMT testing was performed by three licensed chiropractors.
Two of the clinicians were male with 2 and 13 years of
experience, and one was female with 5 years of experience.
VA Strain measurements
Strain measurements were made using sonomicrometry, as
explained in detail in our earlier works (Herzog and Symons,
2002; Symons et al., 2002; Wuest et al., 2010). Briefly, sonomicrometry
crystals (Sonometrics Corporation, London, Ontario, Canada)
of 0.5–1.0 mm diameter were inserted into the wall of the
VA at defined locations (4 crystals and 2 segments for the initial
6 VA tests (Figure 2 markers 1–2 and 9–10) and 8 crystals and 7
segments typically for the 8 final VA tests) (Figure 2 markers 2–9).
Crystals were placed in the lumen of the artery and then sutured
to the VA wall so that they could not move relative to the VA. Each
crystal served as a receiver and a transmitter of short (400 ns)
ultrasound pulses. Knowing the time required for traveling from
one crystal to the next with the head and neck in the neutral position
(Figure 1A; defined as the 0% strain position), strains during ROM
and SMT testing were calculated by the increase or decrease in
time it took to cover the distance from one crystal (transmitter)
to the neighboring crystal (receiver). This approach has the advantage
that the strains are independent of the actual speed of sound
transmission, and that strains can be measured continuously
(2000 Hz) during testing. The detailed calculations and the measurements
of accuracy and resolution (0.016 mm) can be found
in our previous works (Herzog and Symons, 2002; Symons et al.,
2002; Wuest et al., 2010). Percentages of strain (elongations were
defined as positive) were then calculated for each ROM and each
SMT test from the neutral position to the position of maximal VA
strain. For example, a strain of 3.4% would indicate that the VA
was stretched by 3.4% from its original length at neutral, while a
strain of ÿ2.1% would indicate a shortening of the VA of 2.1% from
its neutral length.
Strain results were calculated for each segment, chiropractor,
and ROM/SMT test, but will be given here as summary results
across four identified regions of the VA designated as V1, V2, V3
and V4 (Figure 2). Strains for V1 segments are calculated using markers
1 and 2 (markers are labeled consecutively from inferior to
superior as shown in Figure 1), for V2 segments markers 3–6, V3
markers 7 and 8, and V4 markers 9 and 10.
Force measurements
Forces applied by the clinicians on the neck of the specimens
during SMTs were measured using a thin flexible pressure pad as described before by our group (Conway et al., 1993; Forand et al.,
2004; Herzog, 1991, 2010; Hessel et al., 1990; Wuest et al.,
2010). Briefly, the pressure pad (Novel Inc, Munich, Germany)
was sealed for moisture proofing and then held against the neck
of the specimen over the target site. The clinician then contacted
the pressure pad with her/his 2nd metacarpal, applied a preload
force on the target site, and then executed the treatment thrust.
Analysis of these forces revealed that treatments on the cadaver
specimens, in general, were performed with greater peak forces
and higher rates of load application than found in patient and
non-patient subjects, as illustrated in this special issue of JEK
(Symons et al., in Press). Thus, if anything at all, the strains during
SMTs measured here are likely greater than those one would
obtain in a patient.
Results
 Table 2
Table 2
|
Mean strains (and minimal and maximal strains) for the V1, and
V4 segments for the ROM testing in our initial study (Symons et al.,
2002) were 3.2% (2.0–4.9%), and 5.9% (1.2–12.5%), respectively,
while the corresponding values for the SMT testing were 6.2%
(4.5–8.0%) and 2.1% (1.4–2.7%) (Table 2). Note that the ipsilateral
values for the SMT testing were not used in this analysis as they
had been shown to be affected by direct contact of the clinician
with the sonomicrometry markers, and were found unreliable.
However, ipsilateral values were considered for the ROM testing
as contact with the VA embedded markers was avoided. For example,
VA strains for the left VA would have been used for left and
right rotations of the head and neck, while strains for the left VA
would only have been considered for manipulations on the right
side of the neck, which would create the greatest strains (Symons
et al., 2002).
In our more recent study (Table 1, cadavers 6–9) using three clinicians
and 8 VAs that were anatomically restored by filling them
with ultrasound gel, the mean strains (minimal and maximal
strains) for the V1, V2, and V3 segments for the ROM testing were
3.3% (1.0–14.5%), 4.9% (1.3–12.7%), and 12.2% (3.6–22.9%). The corresponding
values for the SMT testing were 0.9% (0–4.3%), 1.4% (0–
4.6%), and 3.8% (0–12.6%) (Table 2).
Mean failure strains of VAs have been reported previously to be
58%, on average (Symons et al., 2002).
 Figure 3
Figure 3
|
An example of raw data of VA length changes (V4 segment) for a
full flexion range of motion test (Figure 3; gray trace) and a diversified
lateral/rotational SMT (Figure 3; black trace) from the same subject
illustrates many typically observed results:
(i) The length change
of the VA during SMT (indicated by the two arrows) is much smaller
than that observed during the range of motion testing;
(ii) the
length of the VA throughout the entire SMT is smaller than the
length in the neutral
head and neck position (about 15.4 mm –
as seen at the very beginning of the range of
motion test which started at the neutral length); and
(iii) the rate of change in VA
length (given by the slope of the distance-time traces), is similar
for the SMT and range of motion testing, even though the range
of motion testing was
performed very slowly (a full cycle took
approximately 4s, while the displayed SMT took 150 ms).
Discussion
Vertebro basilar accidents associated with high-speed, lowamplitude
spinal manipulative treatments have been a concern
for clinicians and patients alike. The primary argument for such
accidents has been that SMTs stretch vertebral artery segments
to such a degree that there is an occlusion of blood flow, and
possible stretch-induced damage to the VA. Since the thrust phase
of neck SMTs lasts 100–150 ms (Herzog and Symons, 2001; Triano,
2000), any occlusion would likely have little to no effect on blood
flow to the brain. Therefore, we focused on the stretches that occur
during SMTs to the neck by measuring directly the strains of VAs
during SMTs applied by clinicians certified in manipulative treatments
and compared these strains to those one would expect to
occur during normal head and neck movements in everyday life
(passive range of motion).
The average failure strain of human VAs has been found to be
58% (Symons et al., 2002), with failure defined as the first softening
of the VA in a stretch experiment. All values shown in Table 1 are
clearly below the mechanical failure strains of VAs with the largest
measured value of 22.9% for ROM testing in the V3 region representing
about 39% of the failure strain. However, failure strain
might be considered a rude estimate of damage in VAs and it might
be argued that micro-structural failures could occur in the absence
of gross mechanical failure of the tissue. Furthermore, repeat treatments,
as may occur in clinical practice, might cause micro-structural
damage that is not visible following a single SMT.
In order to investigate the structural behavior and integrity of
arterial tissues exposed to repeat loading cycles, we subjected rabbit
descending aortas (which are of similar size to human VAs) to
1000 repeat stretch cycles of 0% strain (controls), 6% strain and
30% strain. Following mechanical loading, the arteries were fixed,
embedded and analyzed histologically for microstructural damage
by a pathologist blinded to the strain grouping. Exposure to 1000
cycles of 6% strain did not result in increased microstructural damage
compared to control tissues, but 1000 cycles of 30% strain
caused significant increases in microstructural damage of the arterial
tissue (Austin et al., 2010). Mean strains across all SMTs, all clinicians
and neck segments ranged from 0.9–6.2%, suggesting that
even 1000 cycles of exposure in a 20 min period (as done in the
study by Austin et al. (2010) would not result in micro-structural
damage of the VA.
Another way of estimating if SMTs might produce harmful
stretches of the VA is to compare the maximal strain values obtained
across all clinicians and all manipulations to the maximal
strain values obtained for ROM testing, as the ROM tests indicate
the range of head and neck movements that a person can perform
in everyday life, assuming that everyday life head/neck rotations,
extensions, and bending are safe. We have done that by calculating
the ratio of the maximal strains obtained by SMT and ROM testing,
where values of less than 100% indicate that the SMT strain was
smaller than the strain during ROM testing, and thus would be considered
safe. For the V1 segment, this ratio is 55% (8%/14.5%). The
corresponding values for V2, V3, and V4 are 36%, 55%, and 22%,
respectively. In summary, the maximal strain values for the ROM
testing at each segmental level were always greater than the corresponding
strain values for the SMTs, suggesting that neck SMTs
impose less stretch than turning your head, or extending your neck
while looking up at the sky.
Limitations
The results of this study suggest that neck SMTs impose
stretches on the VA that are maximally 55% of the passive range
of motion achieved with normal movements of the head and neck
and are maximally 22% of the observed mean mechanical failure
strain of human VAs. Therefore, based on the mechanical tests performed
here, one should be able to conclude that stretching of VA
during neck SMTs does not cause any damage of the VAs. However,
these results must be considered in view of experimental and technical
limitations, and ultimate proof of the safety regarding stretch
of VAs needs to come from live human experiments performed
during actual SMTs in patients with accurate strain measurements
of the VA, but such experiments are not possible at present and our
approach is currently the best to provide information on VA
mechanics during neck SMTs.
All measurements were performed on human cadavers. It has
been argued in the past that strain measurements in cadaveric
specimens might differ from live subjects, however that is rather
unlikely. The strains of the VA (and for that matter of any tissue)
only depend on the distance between origin and insertion points
of the specimen (VA in our case), and the proper shape of the test
specimen. There is no reason why a specific head/neck position
should cause the origin/insertion points to be at a different location
in a live compared to a dead subject. In fact, strain measurements
in other tissues, such as skeletal muscles, have been used for decades
as indications of strains in the live body (Crowninshield et al.,
1978; Wickiewicz et al., 1983). After all, geometrical considerations
dictate that the strain only depends on the joint configuration
(relative location of the vertebral bodies in our case) and the
moment arm around the centre of rotation of the joint (two adjacent
vertebral bodies, respectively). Thus, there is no a priori reason
why strains in the VA should differ between a person that is
alive and the same person right after death. However, in our initial
study on VA strains, we did not perfuse the VAs and that might
have resulted in a systematic error in our strain measurements
(Symons et al., 2002). This potential error was rectified in our
second study (Table 2) by restoring the proper VA shape by filling
the arteries with ultrasound gel. Giving the VAs their in vivo shape
resulted in smaller mean strains during SMT application (0.9%
strain vs. 6.2% strain), but the ROM strains remained unchanged
(3.3% vs. 3.2%).
Another limitation that has been put forward in the past is the
idea of failure strains obtained from ‘‘old’’ cadaveric specimens and
their applicability to the average patient. The average failure strain
observed in our cadaveric specimens was 58%. However, this is
likely an underestimation of the true value, as the age of the specimens,
the placing of the piezoelectric markers into the lumen of
the VA, the dissection of the neck, and the isolation and clamping
of the VA in the materials testing machine, all would have (if anything
at all) compromised VA strength, and therefore given failure
strains less than those of the intact, in vivo VA. Thus, although failure
testing is difficult, compromising the VAs strength as done in
our testing would tend to reduce the failure values, thus working
against the argument that neck SMTs produce safe VA strains.
Engineering strain of a material is typically defined from a reference
length at which stress is just zero, and a small stretch will
produce force and thereby stress in the material. Here, the reference
length (0% strain) was defined as the length of the VA segments
when the head and neck were in a neutral position. We
do not know if that is already a strained position. However, in
our initial(Herzog and Symons, 2002; Symons et al., 2002) studies,
we found that first force in the VA was measured at approximately
12% of strain, which for the segments tested, was approximately
the maximal strain achieved in the ROM testing. Therefore, it appears
that there is no ‘‘real’’ strain in the VA until the head and
neck are moved to the end range of motion, and any elongation
prior to that (that is all the elongations during SMTs) would be
within a strain free region (Herzog and Symons, 2002). This would
mean that the VA is never really strained during spinal manipulative
treatments but that the VA is merely taking up slack as the
neck and head are moved during SMT, but that there is no stress
and thus no possibility for microstructural damage. Qualitative
observation of the VAs in many specimens seem to support the notion
that at least some segments in some specimens are slack, and
do not reach a length of ‘‘engineering strain’’ even at the longest
lengths during SMT and ROM testing. However, in order to confirm
this assertion, careful tests need to be done where individual segments
of the VA are removed from the neck in the neutral position,
and sensitive force–elongation testing is then performed in these
specimens. Such data have not been published to date for human
VAs.
Another limitation that has been mentioned in the past is the
idea that SMT forces applied to cadaveric specimens are not the
same as those applied in patient or non-patient, live human subjects.
Force measurements during neck SMTs in cadavers and live
subjects are the topic of another paper in this special issue of JEK
(Symons et al., in Press). Without taking all the thunder from that
publication, it can be stated here that, on average, SMTs performed
by the same clinicians on cadaveric specimens were statistically
significantly more powerful: that is, the peak forces were greater
and the rate of force application higher in the cadaveric specimens
than the human patient and non-patient subjects. The possible reasons
for this are discussed in the accompanying paper, but the
implications of these results are that, if anything at all, the VA
strains obtained from the cadaveric subjects reported here, would
likely be greater than those obtained in actual patients.
Finally, it has been argued that the rate of stretch of the VA is
more important than the actual stretch (strain) magnitude, and
that ‘‘safe’’ strain magnitudes during neck SMTs might still be
harmful because of the exceptional rate of strain application. The
VA is a visco-elastic structure (Austin et al., 2010), and thus stress
would be greater for a given amount of strain when the VA is
stretched at a high compared to a low rate. However, the mean
peak strain during SMT was 6.2% and occurred over an average
time of about 150 ms for a strain rate of about 41% strain/s. Considering
the largest ROM strain observed in our study (22.9%), the
head movement for that strain (rotation) would produce a similar
strain rate if the rotation occurred in about 560 ms, which seems a
perfectly achievable movement. Similar considerations could be
made for the mean strains during SMT and the peak strains during
ROM, and it would become clear that strain rates for the largest
head/neck movements are within similar rates of strain application
than neck SMTs (e.g. Figure 3). Of course, actual head and neck movements
are slower than what they are during neck SMTs, but the
peak strains are also much larger, thus producing rates of strain
that are actually quite comparable. Nevertheless, in order to determine
the rate dependence of stress in VAs, careful stress–strain
testing should be performed at different rates of stretch. To our
best knowledge, such data are currently not available for human
VAs.
Conclusion
The results from this study demonstrate that average and maximal
VA strains during high-speed low-amplitude cervical spinal
manipulation are substantially less than the strains that can be
achieved during ROM testing for all vertebral artery segments.
Furthermore, VA strains obtained during SMT and ROM testing
are substantially smaller than average failure strains. Therefore,
we conclude that cervical spinal manipulations, as tested here,
are safe from a mechanical point of view for normal, healthy VA.
Acknowledgements
The Canadian Chiropractic Protective Agency, the Canadian
Chiropractic Research Foundation, and the Alberta College and
Association of Chiropractors.
References:
Austin, N, DiFrancesco, LM, and Herzog, W.
Microstructural Damage in Arterial Tissue Exposed to Repeated Tensile Strains
J Manipulative Physiol Ther 2010 (Jan); 33 (1): 14–19
Brennan PC, Kokjohn K, Kaltinger CJ, et al.
Enhanced Phagocytic Cell Respiratory Burst Induced by Spinal Manipulation:
Potential Role of Substance P
J Manipulative Physiol Ther 1991 (Sep); 14 (7): 399–408
Cascioli V, Corr P, Till Ag AG.
An investigation into the production of intra-articular gas bubbles and increase in joint space in the zygapophyseal joints of the cervical spine in asymptomatic subjects after spinal manipulation.
J Manipulative Physiol Ther 2003;26(6):356–64.
Conway PJW, Herzog W, Zhang Y, Hasler EM, Ladly K.
Forces required to cause cavitation during spinal manipulation of the thoracic spine.
Clin Biomech 1993;8:210–4.
Cote P, Mior SA, Vernon H.
The short-term effect of a spinal manipulation on pain/
pressure threshold in patients with chronic mechanical low back pain.
J Manipulative Physiol Ther 1994;17(6):364–8.
Crowninshield RD, Johnston RC, Andrews JG, Brand RA.
A biomechanical investigation of the human hip.
J Biomech 1978;11:75–85.
Dishman JD, Bulbulian R.
Spinal reflex attenuation associated with spinal manipulation.
Spine 2000;25(19):2519–25.
Dishman JD, Burke J.
Spinal reflex excitability changes after cervical and lumbar spinal manipulation: a comparative study.
Spine J 2003;3(3):204–12.
Downie AS, Vemulpad S, Bull PW:
Quantifying the High-velocity, Low-amplitude Spinal Manipulative Thrust: A Systematic Review
J Manipulative Physiol Ther. 2010 (Sep); 33 (7): 542-53
Floman Y, Liram N, Gilai AN.
Spinal manipulation results in immediate H-reflex changes in patients with unilateral disc herniation.
Eur Spine J 1997;6:398–401.
Forand D, Drover J, Suleman Z, Symons B, Herzog W.
The forces applied by female and male chiropractors during thoracic spinal manipulation.
J Manipulative Physiol Ther 2004;27:49–56.
Gál JM, Herzog W, Kawchuk GN, Conway PJW, Zhang Y.
Movements of vertebrae during manipulative thrusts to unembalmed human cadavers.
J Manipulative Physiol Ther 1997a;20:30–40.
Gál JM, Herzog W, Kawchuk GN, Conway PJW, Zhang YT.
Measurements of vertebral translations using bone pins, surface markers and accelerometers.
Clin Biomech 1997b;12(5):337–40.
Gibbons PF, Gosling CM, Holmes M.
Short-term effects of cervical manipulation on edge light pupil cycle time: a pilot study.
J Manipulative Physiol Ther 2000;23(7):465–9.
Haldeman S.
Spinal manipulative therapy in sports medicine.
Clin Sports Med 1986;5:277–93.
Haldeman S, Carey P, Townsend M, Papadopoulos C.
Arterial Dissections Following Cervical Manipulation: The Chiropractic Experience
Canadian Medical Association Journal (CMAJ) 2001 2001 (Oct 2); 165: 905–906
Haldeman S, Kohlbeck FJ, McGregor M.
Risk Factors and Precipitating Neck Movements Causing Vertebrobasilar Artery Dissection
After Cervical Trauma and Spinal Manipulation
Spine (Phila Pa 1976) 1999 (Apr 15); 24 (8): 785–794
Haldeman S, Rubinstein SM.
Cauda equina syndrome in patients undergoing manipulation of the lumbar spine.
Spine 1992a;17(12):1469–73.
Haldeman S, Rubinstein SM.
Compression fractures in patients undergoing spinal manipulative therapy.
J Manipulative Physiol Ther 1992b;15(7):450–4.
Herzog W.
Biomechanical studies of spinal manipulative therapy.
The Journal of the CCA 1991;35:156–64.
Herzog W.
Clinical biomechanics of spinal manipulation.
Philadelphia: Churchill Livingstone; 2000a.
Herzog W.
The mechanical, neuromuscular, and physiologic effects produced by spinal manipulation.
In: Herzog W, editor.
Clinical biomechanics of spinal manipulation.
Philadelphia: Churchill Livingstone; 2000b. p. 191–207.
Herzog W:
The Biomechanics of Spinal Manipulation
J Bodyw Mov Ther. 2010 (Jul); 14 (3): 280–286
Herzog W, Kats M, Symons B.
The effective forces transmitted by high-speed, lowamplitude thoracic manipulation.
Spine 2001;26(19):2105–10.
Herzog W, Scheele D, Conway PJW.
Electromyographic responses of back and limb muscles associated with spinal manipulative therapy.
Spine 1999;24(2):146–52.
Herzog W, Symons B.
The biomechanics of spinal manipulation.
Crit Rev Phys Rehabil Med 2001;13(2&3):191–216.
Herzog, W., Symons, B.,2002.
The Mechanics of Neck Manipulation With Special Consideration of the Vertebral Artery
J Can Chiropr Assoc. 2002 (Sep); 46 (3): 134–136
Hessel BW, Herzog W, Conway PJW, McEwen MC.
Experimental measurement of the force exerted during spinal manipulation using the Thompson technique.
J Manipulative Physiol Ther 1990;13:448–53.
Hurwitz EL, Aker PD, Adams AH, Meeker WC, Shekelle P.
Manipulation and Mobilization of the Cervical Spine:
A Systematic Review of the Literature
SPINE (Phila Pa 1976) 1996 (Aug 1); 21 (15): 1746–1760
Ianuzzi A, Khalsa PS.
Comparison of human lumbar facet joint capsule strains during simulated high-velocity, low-amplitude spinal manipulation versus physiological motions.
Spine J 2005;5(3):277–90.
Lee KP, Carlini WG, McCormick GF, Albers GW.
Neurologic complications following chiropractic manipulation: a survey of California neurologists.
Neurology 1995;45(6):1213–5.
Lehman GJ, Vernon H, McGill SM.
Effects of a mechanical pain stimulus on erector spinae activity before and after a spinal manipulation in patients with back pain: a preliminary investigation.
J Manipulative Physiol Ther 2001;24(6):402–6.
Paciaroni M, Bogousslavsky J.
Cerebrovascular complications of neck manipulation.
Eur Neurol 2009;61(2):112–8.
Powell FC, Hanigan WC, Olivero WC.
A risk/benefit analysis of spinal manipulation therapy for relief of lumbar or cervical pain.
Neurosurgery 1993;33(1):73–9.
Rubinstein, S.M.
Adverse Events Following Chiropractic Care for Subjects With Neck or Low-Back Pain:
Do The Benefits Outweigh the Risks?
J. Manip. Physiol. Ther. 2008, 31, 461–464.
Rubinstein SM, Haldeman S.
Cervical manipulation to a patient with a history of traumatically induced dissection of the internal carotid artery: a case report and review of the literature on recurrent dissections.
J Manipulative Physiol Ther 2001;24(8):520–5.
Suter E, McMorland G, Herzog W.
Short-term effects of spinal manipulation on Hreflex amplitude in healthy and symptomatic subjects.
In: Huijing PA, Hollander P, Findley TW, Schleip R, editors.
Fascia research II – basic science and implications for conventional and complementary health
care.
Munich: Elsevier; 2009. p. 270–5.
Suter E, McMorland GM, Herzog W.
Short-term effects of spinal manipulation on Hreflex amplitude in healthy and symptomatic subjects.
J Manipulative Physiol Ther 2005;28:667–72.
Symons, B., Leonard, T.R., Herzog, W., 2002.
Internal Forces Sustained by the Vertebral Artery
During Spinal Manipulative Therapy
J Manipulative Physiol Ther 2002 (Oct); 25 (8): 504–510
Symons B, Wuest S, Leornard T, Herzog W.
Biomechanical characterization of cervical spinal manipulation in living subjects and cadavers.
J Electromyogr Kinesiol. 2012 Oct;22(5):747-51
Terrett AGJ, Kleynhans AM.
Cerebrovascular complications of manipulation.
In: Haldeman S, editor.
Principles and practice of chiropractic.
Connecticut: Appleton
& Lange; 1980. p. 579–98.
Triano JJ. The mechanics of spinal manipulation.
In: Herzog W, editor.
Clinical biomechanics of spinal manipulation.
Philadelphia, PA: Churchill-Livingstone; 2000. p. 92–190.
Triano JJ, Brennan PC, McGregor M.
A study of threshold response to thoracic manipulation.
Proc 3rd Int Conf Spinal Manip 1991;3:150–2.
Wickiewicz TL, Roy RR, Powell PL, Edgerton VR.
Muscle architecture of the human lower limb.
Clin Orthop 1983;179:275–83.
Wuest, S, Symons, B, Leonard, T, and Herzog, W.
Preliminary Report: Biomechanics of Vertebral Artery
Segments C1-C6 During Cervical Spinal Manipulation
J Manipulative Physiol Ther. 2010 (May); 33 (4): 273–278

Return to STROKE AND CHIROPRACTIC
Since 11-15-2012
|











