

Differential Compliance Instrument in
the Treatment of Infantile Colic:
A Report of Two CasesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2002 (Jan); 25 (1): 58–62 ~ FULL TEXT
Robert A. Leach
Private Practice of Chiropractic,
Postgraduate Faculty,
National University of Health Sciences, USA.
rl@drleach.comOBJECTIVE: To report on the novel use of a computer-assisted adjusting device as a potentially safe method for treatment of infantile colic.
CLINICAL FEATURES: Two infants were diagnosed by their pediatrician as having infantile colic, which was characterized by signs of distress, uncontrollable crying, and brief episodes of screaming. Both children had normal growth (despite low birth weight in the second) and no other abnormalities.
INTERVENTION AND OUTCOME: A PulStar Function Recording and Analysis System (PulStar FRAS, Sense Technology, Inc, Pittsburgh, Penn) device was used to administer light impulses (approximately 1.7 joules, which produced a 3 to 4 lb force) at each segmental level throughout the dorsal spine, with probe tips spaced 2 cm apart straddling the spinous processes. Crying was reduced by 50% after a single session of instrumental adjusting in a 6-week old girl and after 4 sessions in a 9-week old boy, according to colic diaries kept by the mothers. Average hours of uninterrupted daily sleep increased from 3.5 to 6.5 hours after a single session. Within 10 days (5 and 8 sessions, respectively), colicky behavior disappeared and average total daily sleep improved to 14.5 hours (an average increase of 4.5 hours). Results continued over a 30-day follow-up.
CONCLUSION: The PulStar mechanical adjusting device appears to have been well tolerated and beneficial in 2 cases of infantile colic. Further research is necessary to determine whether this device can enhance the safety and effectiveness of chiropractic treatment in infants with colic.
From the Full-Text Article:
Introduction
This article proposes a theory to explain the clinical observation of structural change of the spinal system as a result of manipulation.1-5 The function of the skeletal structure is to provide support and mobility to the body.6 Each joint transmits supportive loads through the joint and, depending on the location of the joint in the structure, enables the structure to move about one or more axes. Fixations of spinal joints that reduce the mobility of the system lead to spinal dysfunction and may produce structural changes in the spine that correlate with patient symptoms such as muscle pain.
General considerations of complex systems result in the formulation of a theory of spinal positioning based on the spine achieving mechanical equilibrium (the equivalent to achieving a minimum internal energy state) with the loads imposed on it. Structural and/or mechanical changes that perturb the conformation of the spine are assumed to be fixations that result from inflammatory changes, along with associated muscle spasm, ligament shortening or thickening, facet locking, and ultimately, degeneration.
A common clinical example of this process is seen in cervical hypolordosis, or cervical kyphosis, in which a lateral cervical spine film shows loss or reversal, respectively, of the normal cervical lordotic curvature.7 This loss of normal curvature is often associated with whiplash disorder and is a requirement for the diagnosis of cervicogenic headache. [8] It is hypothesized that loss of the normal curvature is associated with muscle spasms or more permanent changes in the joint, and there is some evidence that this promotes degenerative changes, although this remains to be proven. [9, 10]
Evidence for the new hypothesis includes previous work in which a patient with radiographically demonstrable cervical hypolordosis had complete resolution of the fixation (measured both radiographically and with computerized measures of tissue compliance) after analysis and treatment with a PulStarFRAS (Sense Technology, Pittsburgh, Penn) computerized adjusting device, which uses multiple highvelocity, low-amplitude impulse percussive therapy for treatment. [4] The results of this and other investigations with “lighter” techniques, including “mirror image” postural retraining and cervical extension distraction, challenge the concept of adjustment as a method of aligning individual spinal segments on the basis of deviations observed on static x-ray film. An alternative hypothesis is presented here to further explore the concept that the spine can reposition itself in space to a more optimal position if the constraints (fixations) that prevent the spine from achieving this position are reduced or removed.
Case report
Case 1
A 6-week-old female infant weighing 10 lb, 6 oz was brought for care after crying almost continuously since birth. The crying, which the mother described as often “violent screaming,” had steadily gotten worse since birth and was uninterrupted except for brief periods of sleep at night (up to 3 hours), 15 minutes of rest 3 or 4 times per day, or brief periods of feeding or riding in a car. The infant was growing at a normal rate and was otherwise healthy, and the mother reported no unusual complications of labor or delivery. Her pediatrician diagnosed the infant with infantile colic, and the mother brought the infant for chiropractic evaluation after a nurse suggested that adjustments might help.

Figure 1 A complete history was taken, including completion of a colic diary for the previous 24-hour period. After obtaining parental consent, a brief physical examination of vital signs and observation of the child’s movements were followed by palpation of the spine. This revealed only some possible stiffness to rotational end feel in the upper cervical and stiffness with posterior to anterior mid dorsal spine massage-type palpation. It seemed the upper cervical end feel restriction may have been nonpain-induced guarding by the infant, but the mid dorsal stiff feel to palpation was seemingly reproducible. The initial working diagnosis of infantile colic and T8 segmental dysfunction was made on the basis of the mother’s statements and observation of the child’s behaviors since entering the clinic (flexion of the thighs to the chest and extension of the spine with violent crying; Figure 1).
Both verbal and written consent to treat was obtained after a thorough discussion of medical, chiropractic, and no-treatment options, including potential benefits as well as known risks. In addition, the mother gave consent for the novel approach of delivering steady, light treatment to the child with the computerized mechanical PulStar device. We demonstrated the device on the mother’s hand before its use over her child’s spine. We told her that it was possible that lighter instrumental thrusts might be better regulated than manual treatment and, if successful, might lead to safer treatments.
Four consecutive sweeps of the entire dorsal spine were made with the PulStar device set in the analysis mode; this produced light impulses that stopped when resistance reached a certain threshold (1.7 joules typically produced a response rate of 30 to 40, or roughly a 3-4 lb force). [24, 25] Each segmental level throughout the dorsal spine was treated in this manner, with probe tips spaced 2 cm apart and placed equidistant from the spinous processes. At each treatment session the baby seemed to express discomfort by the third and fourth sweeps, and some temporary erythema overlying the paraspinal muscles was observed. Given this response, it seemed prudent to discontinue treatment at this point in the sessions. It was unknown whether more or less treatment would be needed to diminish colicky behaviors as effectively as had been observed in previous investigations. [4, 8] After the first treatment, just as with other subsequent sessions, the infant’s discomfort was easily quelled by attention from the mother within a few minutes (and later, even seconds) after discontinuing treatment. Other than this temporary discomfort, the treatment was well tolerated by the baby. (This was not so apparent on the first and second visits because the baby was already crying continuously; however, during later visits when the infant was no longer crying in the office, treatment with PulStar did not trigger any crying.)
As an outcome measure, the mother was asked to complete a daily colic diary that recorded rhythm (resting, awake, crying), stools (small, medium, large), and feeding (breast, formula, water/other) on an hourly basis. [4, 5] Center and Leach [25] discussed the need and rationale for establishing a pretreatment baseline in case studies and quasi-experimental research designs, and the colic diary was used by a number of prior investigators and found to be adequate for measuring these important colic-related outcomes. [4] Although a longer pretreatment baseline would better establish whether posttreatment changes were the result of chance or chiropractic intervention, a shorter 24-hour baseline was chosen because of the high drop-out rate observed during the baseline phase of a recent prior investigation. [4]

Figure 2 After a single adjustment session with the PulStar unit, the child rested for 11 hours during the following 24-hour period, (compared with 4 hours the day before the treatment) and slept for 9 uninterrupted hours during the night. The infant awakened smiling and laughing, which had not before been observed by the parents (Figure 2). [For the first time since birth, the same infant awakened smiling and laughing the day after beginning chiropractic computer-assisted adjustments with the PulStarFRAS device and 2 days before confounding co-intervention with Levsin drops. Photograph taken by mother.]
In addition, there were only 5 hours of crying in that same 24-hour period (a decrease from 13 hours the day before the first adjustment session). The infant rested another 8 hours the following night, and this improvement in rest continued through the first 2 weeks of care and throughout a 30-day follow-up period.
Nevertheless, another caregiver kept the child during the fourth day from onset of care and was disturbed by 4 hours of crying, so the infant was returned to the pediatrician, who prescribed Levsin (Schwarz Pharm, Milwaukee, Wis) drops (0.125 mg hyoscyamine sulfate United States Pharmacopeia (USP) per mL with 5% alcohol, dyes, flavor, glycerin, water, sodium citrate, sorbitol, and sucrose). This anticholinergic agent may cause drowsiness, dizziness, or blurred vision, and may decrease sweat gland activity. The usual dose for a 5-kg infant is about 5 drops. The first use of the drops at 7 PM did not abate a 3-hour crying spell. Although the infant’s crying had reduced to brief periods (1-3 hours) for no more than 4 hours in a 24-hour period, the mother administered the Levsin drops once per day over the next 3 days.
The third adjustment was administered on the sixth day after onset of care. The mother had administered drops once that day, at 2 PM, before the adjustment. The infant cried only 2 hours that day. On the seventh day of chiropractic intervention, the child slept 16 hours and did not cry at all for the first time since her birth 7 weeks before. Only 2 more adjustments were administered over the next 3 days; by that time (10 days, 5 sessions), colicky behavior had disappeared, and the infant was sleeping 12 to 17 hours daily.
At this point there was a break in the data because the mother and child left for a 2-week vacation, and the mother did not continue daily record keeping of colicky behaviors. Nonetheless, on returning 2 weeks later, she was emphatic in stating that the child was still basically cured and that she had only used the drops once per day on 4 different days. We reconstructed the 11th through 27th days of crying spell data together in the office on that visit.
The infant was seen for 4 additional weekly treatment sessions, and the mother discontinued use of the Levsin medication because the baby no longer exhibited “colicky” behavior. In addition, during this 30-day follow-up period, crying was brief and easily quelled by normal parenting activity such as changing a diaper or feeding. The infant continued sleeping 12 to 15 hours per day.

Case 2
A 9-week-old male infant had infantile colic. The mother had been taking Lorazepam (Wyeth-Ayerst Lab, Philadelphia, PA), Paxil (SmithKline Beecham Pharm, Philadelphia, Pa), Zyprexa (Eli Lilly, Indianapolis, Ind), and Wellbutrin (Burroughs Wellcome, Research Triangle Park, NC) for the first 4 months of her pregnancy until she discovered she was pregnant. At that time she discontinued all medications except Zyprexa, which she continued throughout her pregnancy. The infant had a low birth weight of only 5 lb, 14 oz and was born a month early after a difficult 17-hour (3 hours of hard pushing) labor. He was diagnosed with acid reflux as a result of crying day and night; this was unrelieved by normal parenting behaviors, and Zantac (Glaxo Pharm, Research Triangle Park, NC) was prescribed.
The crying seemed to have abated somewhat when, at the age of 4 weeks, his baby seat fell while he was attended by his mother in the kitchen. She caught him with the seat on top of him before he hit the floor; however, both parents agreed that the crying spells became progressively worse over the next 2 weeks. At that time, a pediatrician diagnosed infantile colic on the basis of the infant’s behaviors, which included perceived abdominal tension, frequent passing of gas, and crying up to 8 hours per day. Metoclopramide (Biocraft, Fair Lawn, NJ) 5 mg/mL stp mort 120/mL (0.3 mL every 6-8 hours) as well as Benadryl (Parke-Davis, Morris Plains, NJ) (hydramine) 12.5/5 mL ( teaspoon every 4 hours) was prescribed along with Mylicon (Johnson & Johnson Merck Consumer, Fort Washington, Pa) infant drops to be taken as needed (when the caregiver noted abdominal tightening and passing of gas). The infant was to continue on Zantac.
On entrance to our office 3 weeks later, the parents stated the crying had progressed to about 14 hours per day in spite of these interventions. Consent was obtained from the parents to examine the child, who was now 9 weeks of age.
Physical examination revealed palpable muscle splinting throughout the dorsal erector spinae muscles. The infant’s crying continued throughout the entire first visit, easing only when the infant was on his stomach on his mother’s lap (not when lying against her shoulder or in any other posture). The baby often clenched his fists and tightened his abdomen. Cervical passive range of motion was fluid and without guarding or excessive crying. Unlike the more responsive nature of the female infant in the first case, the male infant was nonresponsive to the snapping of fingers next to his ear and did not turn his head to look at external stimuli applied to his arm, such as a gentle sweep by the examiner’s finger.
Similar to the first case, consent to treat was obtained and a daily colic diary begun. Treatment commenced throughout the dorsal spine with the PulStarFRAS unit used in the first case. After 4 consecutive daily treatment sessions, crying was reduced to 7 hours (a decrease from 15 hours on the day before beginning care and 14 hours on the first day of care), uninterrupted sleep increased to 5 hours (from 3 hours before care), and total sleep in a 24-hour period increased to 13 hours (from 5 hours before care).
After a total of 9 treatment sessions over 2 weeks, the infant was crying an average of only 2 hours per day; he was sleeping an average of 5 hours per night and averaging 14 hours of total sleep per day. The baby seemed more alert and responded by turning his head quickly toward snapping fingers. Both parents agreed that colicky behaviors had seemed to abate after the first week of instrumental adjustments. The baby no longer screamed but smiled and remained awake without crying for long periods and responded appropriately to normal parenting efforts. On subsequent consultation with the pediatrician, all medications were discontinued except Benadryl, to be taken as needed; however, the mother occasionally provided the infant with Mylicon as well (once every few days on average) throughout a subsequent 30-day follow-up. Colicky behaviors, such as unconsolable crying and clenching of fists, did not return.
Discussion
There is now promising initial evidence that chiropractic may help infantile colic, and these cases present a novel approach to treatment with a computerized mechanical adjusting device that appears to be safe. Although the first case was confounded by co-treatment with Levsin drops, medications had not changed for 3 weeks before the onset of chiropractic intervention in the second case. This is certainly not a critical issue because a case, or even a series of cases, cannot validate a treatment approach. A second problem with the first case was that when the mother was away on vacation, she discontinued use of the colic diary temporarily.

Figure 3
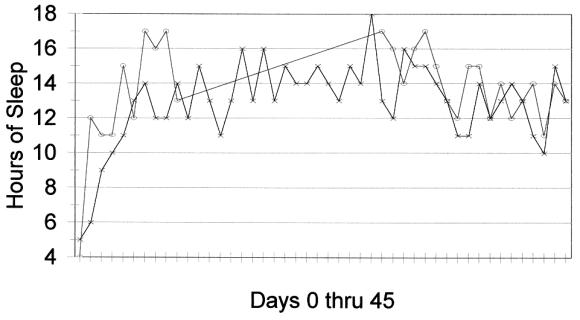
Figure 4 [Figure 3 Hours of crying per 24 hour period. Circle, Case 1; X, Case 2. Day 0 is day before first chiropractic adjustment (case 1 diary data for days 10 to 27 reconstructed at office visit on 27th day after infant’s first adjustment).]
[Figure 4 Hours of uninterrupted sleep per 24 hour period. Circle, Case 1; X, Case 2. Day 0 is the day before the first chiropractic adjustment (break in data for case 1 unrestored—see text).]
Nevertheless, the dramatic improvement seen immediately after the first instrumental adjustment in the first case (administered 2 days before the use of medication in a 6-week old infant), and the significant reduction in crying (Figure 3) and increase in total sleep (Figure 4) within 1 week of the onset of chiropractic care in both cases do lend support to prior investigations that suggest that the use of chiropractic may be an effective treatment for infantile colic. [4, 8] Natural remission seems an unlikely explanation in these cases, given the young age of the infants at the onset of chiropractic (6 and 9 weeks, respectively; natural remissions occur at 3-9 months) and the speed with which the postadjustment remissions occurred. Indeed, the ages of these 2 infants at onset of chiropractic intervention matched the ages of infants selected for research in the published literature to lessen the risk of natural remission as an explanation for improved outcomes. [4, 8]
Doctors should be aware that mothers of infants with colic may be desperate to try any and all measures to obtain relief. Despite little evidence of effectiveness, pediatricians may feel compelled to prescribe medications when family members report that the infant is being treated by a chiropractor. However, it is important to keep pediatricians and other physicians fully informed of all care when consent for this can be obtained from the caregiver.
The most exciting aspect of these cases is that chiropractors may be able to use more controlled adjustive methods in which force, amplitude, and depth are precisely regulated by computer-driven mechanical instruments. [24] The PulStar unit is the only computer-assisted adjusting device holding a US Patent at the time of this writing. It was developed by Joseph M. Evans, PhD, a bioengineer, in conjunction with the late technique developer and chiropractic pioneer, W.V. Pierce. When set in the analysis mode, the device produces a thrust that stops when increasing resistance is met (ie, measured as force in pounds × 10), as measured by transducers in the adjusting head. Set at a force rate of 15 lb force, increased resistance will typically be met in an adult spine at a range of 80 to 150, or an 8 to 15 lb force. Previous published reports outline preliminary reliability and technical aspects of this device. [24, 26] Other noncomputerized mechanical adjusting devices are available and in popular use, including the Activator (Activator Methods, Phoenix, Ariz) instrument; these instruments, used at lower force settings, produce similar thrusts that may not be as precisely controlled by the clinician. In addition, these instruments do not provide the clinician with hard copy data regarding treatment applied to the patient.
Whether the device gently relieved fixations or segmental dysfunction in the dorsal spine [26] or merely exerted some nonspecific vertebral mobilization that had some somatoautonomic or other effect [27] is, of course, speculation and of no consequence anyway. The important issues are whether adjustments can relieve infantile colic and whether they can do it safely. It is incumbent on chiropractors to determine the answer to both these questions, and these cases merely demonstrate a novel approach in that regard. Further research is certainly warranted and necessary to determine whether this instrument or other similar ones can enhance the effectiveness and safety of chiropractic treatment of infants.
Conclusion
The PulStar computer-assisted mechanical adjusting device set to the lowest force setting appears to have been well tolerated by both a 6-week-old female infant and a 9-week-old male infant with colic. Significant improvement in colicky behavior was observed, including apparent remissions within 10 days and 5 to 8 treatment sessions. These gains continued for a 30-day follow-up period in both cases. Although no claims can be made on the basis of individual cases, these findings are supportive of chiropractic intervention for infantile colic. Further research is warranted and necessary to determine whether computer-assisted devices can enhance the effectiveness and safety of chiropractic treatment of infants with colic.
References:
Hensyl WR, editor.
Stedman’s medical dictionary, 25th ed.
Baltimore: Williams & Wilkins; 1990.Wiberg JMM, Nilsson N.
Infants with colic may have had a faster delivery:
a short, preliminary report.
J Manipulative Physiol Ther 2000;23:208-10.Matheson I.
Infantile colic—what will help?
Tidsskr Nor Laegeforen 1995;115:2386-9.Wiberg, JM, Nordsteen, J, and Nilsson, N.
The Short-term Effect of Spinal Manipulation in the Treatment of Infantile Colic:
A Randomized Controlled Clinical Trial with a Blinded Observer
J Manipulative Physiol Ther 1999 (Oct); 22 (8): 517–522Killinger LZ, Azad A.
Chiropractic Care of Infantile Colic:
A Case Study
J Clinical Chiropractic Pediatrics 1999; 3 (1): 203-206Loon MV.
Colic with projectile vomiting: a case study.
J Clin Chiropr Ped 1998;3:207-10.Sheader WE.
Chiropractic Management of an Infant Experiencing
Breastfeeding Difficulties and Colic: A Case Study
J Clinical Chiropractic Pediatrics 2000; 4 (1): 245-247Klougart N, Nilsson N, Jacobsen J.
Infantile Colic Treated by Chiropractors:
A Prospective Study of 316 Cases
J Manipulative Physiol Ther 1989 (Aug); 12 (4): 281–288Greenhill LL.
The use of psychotropic medication in preschoolers:
indications, safety, and efficacy.
Can J Psychiatry 1998;43:576-81.O’Neill A.
Danger and safety in medicines.
Soc Sci Med 1994;38:497-507.O’Neill RT.
Statistical concepts in the planning and evaluation of drug safety
from clinical trials in drug development: issues of international harmonization.
Stat Med 1995;14:117-27.Serabian MA, Pilaro AM.
Safety assessment of biotechnology-derived pharmaceuticals:
ICH and beyond.
Toxicol Pathol 1999;27:27-31.Pistolese, RA.
Risk Assessment of Neurological and/or Vertebrobasilar Complications
in the Pediatric Chiropractic Patient
J Vertebral Subluxation Research 1998; 2 (2): 73–78Shafrir Y, Kaufman BA.
Quadriplegia after chiropractic manipulation in an infant with
congenital torticollis caused by a spinal cord astrocytoma.
J Pediatr 1992;120:266-9.Sperry K, Pfalzgraf R.
Inadvertent clavicular fractures caused by “chiropractic” manipulations
in an infant: an unusual form of pseudoabuse.
J Forensic Sci 1990;35:1211-6.Spigelblatt L, Laine-Ammara G, Pless IB, Guyver A.
The use of alternative medicine by children.
Pediatrics 1994;94:811-4.Giesen JM, Center DB, Leach RA.
An Evaluation of Chiropractic Manipulation as a Treatment
of Hyperactivity in Children
J Manipulative Physiol Ther 1989 (Oct); 12 (5): 353–363Graham RL, Pistolese RA.
An impairment rating analysis of asthmatic children under chiropractic care.
J Vertebral Subluxation Res 1997;1:41-8.Balon J, et al.
A Comparison of Active and Simulated Chiropractic Manipulation
as Adjunctive Treatment for Childhood Asthma
New England Journal of Medicine 1998; 339(15): 1013-1020Danbert RJ.
Scoliosis: biomechanics and rationale for manipulative treatment.
J Manipulative Physiol Ther 1989;12:38-45.Froehle RM.
Ear Infection: A Retrospective Study Examining Improvement From
Chiropractic Care and Analyzing Influencing Factors
J Manipulative Physiol Ther 1996 (Mar); 19 (3): 169–177Cote P, Mierau D.
Chiropractic management of primary nocturnal enuresis [letter; comment].
J Manipulative Physiol Ther 1995;18:184-5.Keating JC.
Chiropractic management of primary nocturnal enuresis.
J Manipulative Physiol Ther 1995;18:638-41.Evans JM.
Differential compliance measured by the function recording and
analysis system in the assessment of vertebral subluxation.
J Vertebral Subluxation Res 1998;2:15-21.Center DB, Leach RA.
The multiple baseline across subjects design: proposed use in research.
J Manipulative Physiol Ther 1984;7:231-6.Evans JM, Collins DL.
The clinical application of differential compliance methodology to
joint fixation identification and resolution using the PulStarFRAS.
J Vertebral Subluxation Res 1998;2:131-6.Leach RA.
The chiropractic theories: principles with clinical applications, 3rd ed.
Baltimore: Williams & Wilkins; 1994.
Return to COLIC
Return to CASE STUDIES
Return to INSTRUMENT ADJUSTING
Return to CHIROPRACTIC TECHNIQUE
Since 8-16-2000


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |