

Is Exercise Effective for the Management of Neck Pain
and Associated Disorders or Whiplash-associated
Disorders? A Systematic Review by the Ontario
Protocol for Traffic Injury Management
(OPTIMa) CollaborationThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Spine J 2016 (Dec); 16 (12): 15031523 ~ FULL TEXT
OPEN ACCESS Danielle Southerst, BScH, DC, FCCS(C), Margareta C. Nordin, MedSci,
Pierre Cote, DC, PhDa, Heather M. Shearer, DC, MSc, FCCS(C),
Sharanya Varatharajan, BSc, MSc, Hainan Yu, MBBS, MSc, et. al
UOIT-CMCC Centre for the Study of Disability Prevention
and Rehabilitation, University of Ontario Institute of
Technology (UOIT) and Canadian Memorial Chiropractic
College (CMCC),
6100 Leslie St,
Toronto, Ontario, Canada, M2H 3J1.
BACKGROUND CONTEXT: In 2008, the Neck Pain Task Force (NPTF) recommended exercise for the management of neck pain and whiplash-associated disorders (WAD). However, no evidence was available on the effectiveness of exercise for Grade III neck pain or WAD. Moreover, limited evidence was available to contrast the effectiveness of various types of exercises.
Purpose: To update the findings of the NPTF on the effectiveness of exercise for the management of neck pain and WAD grades I to III.
Study design/setting: Systematic review and best evidence synthesis.
Sample: Studies comparing the effectiveness of exercise to other conservative interventions or no intervention.
Outcome measures: Outcomes of interest included self-rated recovery, functional recovery, pain intensity, health-related quality of life, psychological outcomes, and/or adverse events.
Methods: We searched eight electronic databases from 2000 to 2013. Eligible studies were critically appraised using the Scottish Intercollegiate Guidelines Network criteria. The results of scientifically admissible studies were synthesized following best-evidence synthesis principles.
Results: We retrieved 4,761 articles, and 21 randomized controlled trials (RCTs) were critically appraised. Ten RCTs were scientifically admissible: nine investigated neck pain and one addressed WAD. For the management of recent neck pain Grade I/II, unsupervised range-of-motion exercises, nonsteroidal anti-inflammatory drugs and acetaminophen, or manual therapy lead to similar outcomes. For recent neck pain Grade III, supervised graded strengthening is more effective than advice but leads to similar short-term outcomes as a cervical collar. For persistent neck pain and WAD Grade I/II, supervised qigong and combined strengthening, range-of-motion, and flexibility exercises are more effective than wait list. Additionally, supervised Iyengar yoga is more effective than home exercise. Finally, supervised high-dose strengthening is not superior to home exercises or advice.
Conclusions: We found evidence that supervised qigong, Iyengar yoga, and combined programs including strengthening, range of motion, and flexibility are effective for the management of persistent neck pain. We did not find evidence that one supervised exercise program is superior to another. Overall, most studies reported small effect sizes suggesting that a small clinical effect can be expected with the use of exercise alone.
Keywords: Exercise; Neck pain; Rehabilitation; Systematic review; Treatment; Whiplash-associated disorders.
The FULL TEXT Article:
Introduction
Neck pain is common in the general population with 30% to 50% of adults experiencing neck pain annually. [1] In the United States, neck pain is the fourth leading cause of morbidity and chronic disability. [2] In 2008, The 2000 to 2010 Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders (NPTF) reported that 50% to 75% of individuals with neck pain report pain 1 to 5 years later. [3] The episodic nature of neck pain also poses a clinical management challenge as few interventions have been identified as effective and treatment effects are often small and short lived. [3, 4]
Clinical practice guidelines promote exercise for the management of neck pain and associated disorders (herein referred to as neck pain) and whiplash-associated disorders (WAD) [5, 6] (Jessica J. Wong, Pierre Cote, Heather M. Shearer, et al. unpublished data, 2013). Moreover, evidence from population-based surveys suggests that it is commonly prescribed by health-care providers. [7] However, guidelines lack consistency in the type, intensity (frequency, duration), and mode of delivery of recommended exercises.
In 2008, the NPTF synthesized evidence on the effectiveness of exercise for the management of neck pain and WAD. Two trials focused on persistent Grade I/II neck pain and compared exercise interventions with other conservative interventions. One trial [8, 9] demonstrated that exercise (aerobic exercise, stretching, progressive upper body strengthening, and dynamic resistance exercises for the neck) with or without spinal manipulative therapy resulted in greater long-term improvements in pain and disability than spinal manipulative therapy alone. In another trial by Chiu et al. [10, 11], both exercise (activation of deep neck flexors and progressive dynamic flexion/extension resistance training) and Transcutaneous electrical nerve stimulation (TENS) led to similar outcomes in patients with persistent neck pain. Both interventions resulted in greater reductions in neck pain and disability compared with infrared irradiation.
The NPTF found three trials that focused on female office workers with persistent neck pain. Two trials [1214] demonstrated that strengthening and endurance exercises for the neck flexors and upper extremities, either alone or when added to a multimodal physical therapy program, yield similar outcomes with respect to pain and disability. In one trial [15], group exercises (dynamic resistance training for the neck and shoulder) resulted in similar long-term clinical outcomes as groupbased relaxation training or advice to continue usual activities. The Task Force found only one trial on exercise for the management of WAD. In a trial by Rosenfeld et al. [16], home-based range-of-motion exercises resulted in greater pain reduction and diminished need for sick leave compared with written information and advice for patients recently exposed to whiplash trauma. The NPTF did not find evidence related to exercise for the management of Grade III neck pain or WAD.
Since the publication of the NPTF, three systematic reviews have commented on the effectiveness of exercise for the management of neck pain. [1719] However, all reviews had important limitations. First, their synthesis of results included both high- and low-quality studies. [1719] Second, two of the three reviews only commented on the statistical significance of results, without reference to clinical significance. [18, 19] These methodological limitations may have led to biased recommendations. Moreover, the reviews had a limited scope. Two reviews focused on the subpopulations: workers [18] and those injured in motor vehicle collisions. [19] In the third review, studies that compared exercise with alternative nonexercise interventions were excluded. [17] This limits our ability to understand the comparative effectiveness of exercise interventions for the management of neck pain.
The purpose of our systematic review is to update the work of the NPTF on the effectiveness of exercise compared with other interventions, placebo/sham interventions, or no intervention for the management of adults or children with Grade I, II, or III neck pain or WAD.
Methods
Registration
This review protocol was registered with the International Prospective Register of Systematic Reviews on January 23, 2013 (CRD42013003717).
Eligibility criteria
Population

Table 2

Table 1 Our review targeted studies of adults or children with neck pain Grade I, II, or III or WAD Grade I, II, or III. We excluded studies of neck pain caused by major structural pathology (eg, fractures, dislocations, spinal cord injury, infection, neoplasms, or systemic disease). We defined neck pain according to the definition proposed by the NPTF (Table 1). [20] We used the Quebec Task Force classification to define WAD (Table 2). [21]
Interventions
We restricted our review to studies that tested the effectiveness of exercise. We defined exercise as any series of movements with the aim of training or developing the body by routine practice or as physical training to promote good physical health. [22] We chose a broad definition of exercise therapy to be inclusive of a wide variety of techniques common in the treatment and rehabilitation of neck pain and WAD. Exercise interventions could include any prescribed movements with the intent of affecting clinical outcomes with respect to neck pain and WAD. We excluded studies where the intervention was advice or education only, for example, advice to engage in physical activity.
Comparison groups
We included studies that compared exercise interventions with other modes of nonsurgical care, wait-list, or no intervention.
Outcomes
To be eligible, studies had to include one of the following outcomes: self-rated recovery; functional recovery (eg, disability, return to activities, work, or school); pain intensity; health-related quality of life; psychological outcomes such as depression or fear; or adverse events.
Study characteristics
Eligible studies met the following criteria: English language; studies published between January 1, 2000 and January 23, 2013 that had not been reviewed by the NPTF; randomized controlled trials (RCTs), cohort studies, or case-control studies; and included an inception cohort of a minimum of 30 participants per treatment arm with the specified condition for RCTs or 100 participants per group with the specified condition in cohort or case-control studies. We excluded studies with the following characteristics: letters, editorials, commentaries, unpublished manuscripts, dissertations, government reports, books and book chapters, conference proceedings, meeting abstracts, lectures and addresses, consensus development statements, or guideline statements; pilot studies, cross-sectional studies, case reports, case series, qualitative studies, narrative reviews, systematic reviews, clinical practice guidelines, biomechanical studies, or laboratory studies; or cadaveric or animal studies.
Information sources
We developed our search strategy with a health sciences librarian (Supplementary data). A second librarian reviewed the search strategy for completeness and accuracy using the Peer Review of Electronic Search Strategies Checklist. [23, 24] We searched the following databases: MEDLINE, EMBASE, CINAHL, PsycINFO, the Cochrane Central Register of Controlled Trials, the Database of Abstracts of Reviews of Effects, PubMed, and the Index to Chiropractic Literature. Although our search aimed to update the NPTF search (that ended in 2006), we searched all bibliographic databases from January 1, 2000 to January 23, 2013. This ensured that any relevant studies published before 2006 and missed by the NPTF would be captured in our review.
The search strategy was first developed in MEDLINE and subsequently adapted to the other bibliographic databases. The search terms included subject headings (eg, MeSH) specific to each database and free-text words relevant to exercise and neck pain (neck pain grades IIII and WAD grades IIII).We used EndNote X6 to create a bibliographic database to manage the search results. All citations were exported from EndNote X6 into Excel for screening.
Study selection
We used a two-phase screening process to select eligible studies. In Phase 1, random pairs of independent reviewers screened citation titles and abstracts to determine the eligibility of studies. Phase 1 screening resulted in studies being classified as relevant, possibly relevant or irrelevant. In Phase 2, the same pairs of reviewers independently screened the possibly relevant studies to determine eligibility. Reviewers met to resolve disagreements and reach consensus on the eligibility of studies. We involved a third reviewer if consensus could not be reached.
Assessment of risk of bias
Random pairs of independent reviewers critically appraised the internal validity of eligible studies using the Scottish Intercollegiate Guidelines Network (SIGN) criteria. [25] The SIGN criteria were used to qualitatively evaluate the presence and impact of selection bias and information bias and confound on the results of a study. We did not use a quantitative score or a cutoff point to determine the internal validity of studies. [26] Rather, the SIGN criteria were used to assist reviewers make an informed overall judgment on the internal validity of studies. This methodology has been previously described. [21, 2731]
Specifically, we critically appraised the following methodological aspects of a study: clarity of the research question; randomization method; concealment of treatment allocation; blinding of treatment and outcomes; similarity of baseline characteristics between/among treatment arms; co-intervention contamination; validity and reliability of outcome measures; follow-up rates; analysis according to intention-to-treat principles; and comparability of results across study sites (where applicable). Reviewers reached consensus through discussion. An independent third reviewer was used to resolve disagreements if consensus could not be reached. We contacted authors when additional information was needed to complete the critical appraisal. Studies with adequate internal validity had a low risk of bias and were included in our evidence synthesis. [32]
Data extraction and synthesis of results
We computed agreements among reviewers for the screening of articles and reported the kappa statistic (k) and 95% confidence interval (CI). [33] We computed differences in mean changes between groups (with 95% CI) where data were available. The computation of CIs assumed an r=0.80 between baseline and follow-up outcome values. [34, 35]
The lead author extracted data from scientifically admissible studies into a Microsoft Access database, which was then used to build evidence tables. A second reviewer independently checked the extracted data. Meta-analysis was not performed because of heterogeneity of scientifically admissible studies with respect to patient populations, interventions, comparators, and outcomes. We performed a qualitative synthesis of findings from scientifically admissible studies to develop evidence statements according to principles of best-evidence synthesis. [32] We used standardized cutoff values to determine if clinically significant changes were reached in each trial for common outcome measures. These include a between-group 2/10 difference on the Numeric Rating Scale [36], 10/100 mm or 10% difference on the visual analog scale (VAS) [37], and 5/50 difference on the neck disability index (NDI). [3739] We stratified our results according to the type (neck pain vs. WAD), severity (Grade I/II vs. Grade III neck pain and WAD), and duration: recent (symptoms lasting!3 months) versus persistent (symptoms lasting $3 months).
Reporting
The systematic review was organized and reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. [40]
Results
Study selection
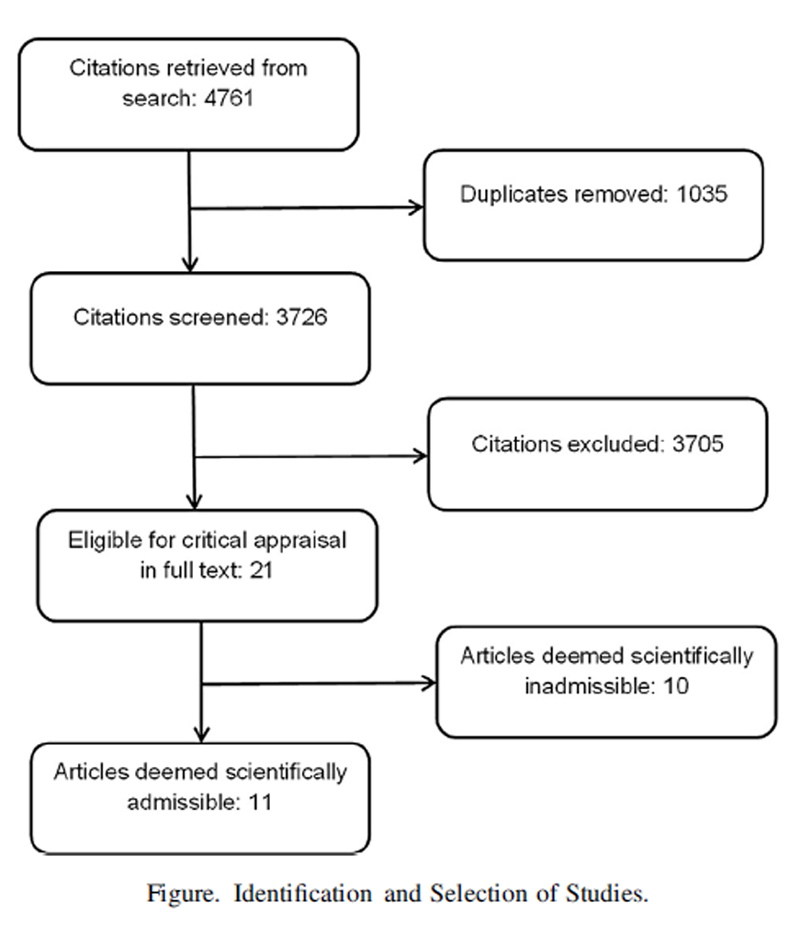
Figure 1 Our search retrieved 4,761 articles. We removed 1,035 duplicates and screened 3,726 articles for eligibility (Figure). After screening, 3,705 articles did not meet our selection criteria, whereas 21 studies were critically appraised. The interrater agreement for the screening of articles was k50.92 (95% CI 0.880.97). We accepted 11 articles as scientifically admissible. One of the scientifically admissible articles [41] was a secondary analysis of another admissible study. [42]
Study characteristics
All 10 scientifically admissible studies were RCTs. Of those, eight assessed the effectiveness of exercise interventions for patients with recent or persistent neck pain Grade I/II. [4149] One RCT [50] addressed recent neck pain Grade III and one RCT [51] included subjects with persistent WAD Grade I/II.

Table 3 The exercise programs varied across studies (Table 3).We identified seven different types of exercises: craniocervical flexion exercises [44, 50], cervical range-of-motion exercises [43, 44, 4648], cervical isometric strengthening exercises [4143, 46, 47], cervical dynamic resistance strengthening exercises [45, 49], shoulder range-of-motion or strengthening exercises [41, 42, 45, 4750], stretching [4143, 46, 47], and general exercise programs [43, 46, 47, 51] (Table 3). The majority (8/10) of RCTs combined different types of exercises within one exercise program. [4147, 49, 50]
Seven RCTs included supervised exercises. [4143, 46, 47, 4951] Most supervised programs were supplemented with home exercise, with the exception of one study. [49] Five RCTs included an unsupervised or home-based exercise intervention arm. [41, 42, 44, 4749] All unsupervised programs were accompanied by written materials, and most provided at least one instructional session. [41, 42, 44, 48, 49] One study provided mixed supervised and unsupervised sessions in the workplace with two formal instructional sessions. [45] Exercise interventions were delivered to groups of participants in five studies. [4143, 4547] Delivery was one-on-one clinician/patient in the remaining studies. [44, 4851] The exercise interventions in most studies (9/10) were provided in clinics. In one study, exercise was delivered in the workplace. [45]
The frequency of unsupervised exercise varied from three times per week in two studies [41, 42, 47] to daily in four RCTs. [44, 4850] Supervised sessions were provided once per week in three RCTs [41, 42, 46, 47] and twice per week in four RCTs. [43, 4951] Mixed supervised and unsupervised sessions were provided at a frequency of three times per week in one study. [45] exercise programs that progressively increased in intensity. [45, 49, 51] The duration of the exercise programs ranged from 6 weeks [48, 51] to 12 months. [41, 42]
Risk of bias within studies
We critically appraised 21 studies; of those, 10 studies (48%) had poor internal validity. [5261] The methodological weakness of the excluded studies included failure to describe or inadequate methods for randomization (three trials) [58, 60, 61]], concealment (six trials) [5255, 57, 60, 61], or blinding (five trials). [5255, 58] Clinically important differences in baseline characteristics among treatment arms were present in seven studies [5257, 60, and co-interventions were not adequately described or accounted for in eight trials. [5254, 5658, 60, 61] Five trials reported high attrition or differential attrition among treatment arms. [5254, 5658] Intention-to-treat analyses could not be confirmed in five trials]. [5558, 60]

Table 4+5 The methodological quality of the scientifically admissible studies is presented in Table 4. Most studies (9/10) used appropriate methods of randomization with the exception of one study where details were not described. [51] All but one study adequately described the method used to conceal treatment allocation. [43] The follow-up rate was greater than 80% in 6/10 studies [41, 42, 44, 46, 4951] and greater than 70% in 8/10 [44, 48] studies. All studies used intention-to-treat analyses.
Summary of evidence
Recent Grade I/II neck pain and associated disorders Home exercises.
Evidence from one RCT suggests that a home exercise program, nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen, or multimodal manual therapy lead to similar outcomes for patients with recent Grade I/II neck pain [48] (Table 5). This trial by Bronfort et al. [48] compared the effectiveness of an exercise program, multimodal manual therapy, and medication in participants with recent neck pain Grade I/II. Participants in the exercise group were allocated to a 12week home exercise program consisting of daily cervical range-of-motion exercises, education, and advice regarding daily activities. Participants randomized to manual therapy received 12 weeks of manipulation, mobilization, soft-tissue massage, assisted stretching, hot and cold packs, and advice to stay active or modify activities as needed. The medication group received NSAIDs, acetaminophen, and advice to stay active or modify activities. At 26 weeks, the home exercise group reported lower pain and disability scores than the medication group. However, these differences did not reach clinical significance (difference in mean change from baseline: numeric rating scale 0.69 [95% CI 0.101.28]; NDI 2.95 [95% CI 0.375.53]). There were no clinically significant differences in pain or disability between the home exercise group and the manual therapy group at all follow-up intervals.
Recent Grade III neck pain and associated disorders Supervised graded strengthening exercises.
For recent Grade III neck pain, the evidence suggests that a supervised graded strengthening exercise program is more effective than advice but leads to similar outcomes as a semi-hard cervical collar with prescribed rest [50] (Table 5). In an RCT by Kuijper et al. [50], participants with cervical radiculopathy of less than 1month duration were randomized to one of the three groups: 6 weeks of supervised graded strengthening exercises for the shoulder and advice, advice to continue activities, or semi-hard cervical collar and rest. Participants in the graded activity group reported greater reduction in arm and neck pain than the advice group at 6week follow-up. This difference in reduction of both arm and neck pain was clinically important (difference in mean change from baseline: arm VAS 13.9 mm [95% CI 7.3320.47]; neck VAS 21.0 mm [95% CI 14.3827.62]). There were no clinically significant differences between these two groups at 6month follow-up. There were no clinically significant differences in neck pain and disability between the exercise group and those randomized to wear a semi-hard cervical collar and rest. However, a higher proportion of participants in the exercise group (45%) remained on partial or complete sick leave after completing the 6week intervention compared those treated with a collar (29%) and those in the control group (38%) (Table 5).
Persistent Grade I/II neck pain and associated disorders
Qigong. Qigong is a gentle focused exercise for the mind and body that aims to increase and restore the flow of qi energy and encourage healing. [62] Evidence from two RCTs suggests that supervised qigong exercise is more effective than wait-listing in reducing neck pain and disability for persistent neck pain Grade I/II [43, 46] (Table 5). Rendant et al. [46] found that 18 group sessions over a 6month period of supervised Nei Yang Gong qigong (ie, a silent and slow form of qigong incorporating neck, shoulder, and breathing exercises) were associated with greater improvements in neck pain compared with wait-list in the short term. The differences in neck pain reduction among groups were clinically important after the 6month intervention (difference in mean change from baseline VAS 18.6 mm [95% CI 13.324.0]). There were no clinically significant differences among participants in the qigong group and those randomized to 18 supervised exercise sessions combining cervical range-of-motion, strengthening, and flexibility exercises. [46] Another RCT found that 24 group sessions of supervised Dantian qigong (ie, a seated form of qigong incorporating breathing and imaginative elements with slow controlled movements) over a 3month period were associated with clinically important reductions in neck pain compared with a wait list after the 6month intervention period (difference in mean change from baseline VAS 13.3 mm [95% CI 5.521.1]. [43] There were also no clinically important differences between the qigong group and a group receiving 24 supervised exercise sessions combining cervical range-of-motion, isometric strengthening, and flexibility exercises [43].
Yoga. Evidence from one RCT suggests that supervised yoga is more effective than education and home exercise for short-term improvement in neck pain and disability [47, 49] (Table 5). Michalsen et al. [47] randomized adults with chronic neck pain to nine weekly supervised Iyengar yoga classes or to an unsupervised home strengthening and mobility program for the neck and shoulders. In Iyengar yoga, a range of classical yoga poses are adapted to patients with neck pain with the use of supportive props. The home exercise program included 12 seated exercises for the neck and shoulder with emphasis on muscle strengthening, stretching, joint mobility, and proper posture. After the intervention, the yoga group reported greater improvements in pain intensity, symptom bothersomeness, disability, health-related quality of life, and depression than the control group. Clinically important between-group differences (mean change) at 1 week postintervention included VAS at rest 23.8 mm (95% CI 17.8 to 29.8), VAS at motion 21.5 mm (95% CI 15.627.4), VAS bothersomeness 18.3 mm (95% CI 12.624.0), NDI 5.7 (95% CI 4.27.3), Short-Form (36) Health Survey 7.4 (95% CI 9.3 to 5.5), and depression 10.2 (95% CI 7.313.1).
Supervised strengthening exercises. The evidence suggests that supervised strengthening exercises alone are not superior to home range-of-motion or stretching exercises (Table 5). [41, 42, 49] In a three-arm RCT, Evans et al. [49] compared the effectiveness of supervised high-dose dynamic resistance strengthening exercises for the neck and upper body; supervised high-dose strengthening (as in Group 1) with multimodal manual therapy including cervical and thoracic spinal manipulation and light massage; and advice regarding posture and daily activities and home-based range-of-motion exercises for the neck and shoulder. No clinically important differences in neck pain intensity or disability were found among groups at short (12 weeks), intermediate (26 weeks), or long (52 weeks) term follow-up points. Another RCT found that adding supervised isometric neck exercises and dynamic resistance shoulder/upper extremity exercises to home-based stretching provided no added benefit to patients with chronic neck pain. [41, 42] Therefore, the evidence indicates that supervised strengthening exercises alone or with multimodal manual therapy are not superior to home range-of-motion or stretching exercises or multimodal manual therapy for the management of persistent neck pain.
Combined supervised strengthening, range-of-motion, and flexibility exercises. Consistent evidence from two RCTs suggests that combined strengthening, range-of-motion, and flexibility exercises are superior to wait list in reducing pain and disability for persistent neck pain Grade I/II [43, 46] (Table 5). Rendant et al. [46] found that participants randomized to 18 supervised sessions of exercise therapy (combining strengthening exercises with cervical range-of-motion and flexibility exercises) reported greater pain reduction than those randomized to a wait list after the 6month intervention period. Differences in pain reduction among groups were clinically important (difference in mean change from baseline VAS 17.7 mm [95% CI 12.522.9]). Similarly, von Trott et al. [43] randomized patients to receive 18 supervised exercise sessions (including isometric strengthening, cervical range-of-motion, and flexibility exercises) followed by 3 months of home exercise or a wait list. Participants in the exercise therapy group reported greater improvement in neck pain and disability after the supervised (3 months) and unsupervised (6 months) components of the intervention. The differences in improvement in neck pain and disability were clinically important after the 6month intervention period (neck pain and disability scale 12.7% [95% CI 6.019.4]). Therefore, the evidence suggests that combining supervised strengthening, range-of-motion, and flexibility exercises is effective in reducing pain and disability in patients with persistent neck pain.
Unsupervised strengthening exercises. Evidence from one RCT suggests that unsupervised, specific, isometric neck and range-of-motion exercises lead to similar outcomes in patients with persistent neck pain. In their RCT, Griffiths et al. [44] tested the effectiveness of unsupervised, specific, isometric neck stabilization exercises by randomizing patients to two groups. The control group received unsupervised active range-of-motion exercises and postural correction techniques. The intervention group received unsupervised active range-of-motion exercises and postural correction techniques supplemented by isometric neck stabilization exercises. The addition of isometric exercises did not result in added benefits in terms of pain or disability reduction or improvement in health-related quality of life.
Persistent Grade I/II WAD
Supervised general exercise. We found evidence that supervised general exercise and advice or advice alone leads to similar short-term pain reduction in adults with persistent WAD Grade I/II [51] (Table 5). In their RCT, Stewart et al. [51] randomized participants with chronic WAD Grade I/II to receive advice (education regarding prognosis, reassurance, and encouragement to resume light activity) or advice supplemented with 6 weeks of supervised general exercise (including stretching, aerobic, strengthening, coordination, and functional activity exercises). The supervised general exercise group reported a greater short-term (6 weeks) reduction in pain intensity compared with the advice group. However, this difference was not clinically important (difference in mean change from baseline NRS 1.0 [95% CI 0.51.5]). There were no clinically significant differences among groups in symptom bothersomeness or disability. Additionally, there were no clinically significant differences among groups at 1year follow-up. Therefore, this study indicates that a general exercise program is not more effective than structured advice alone in patients with persistent WAD Grade I/II.
Neck pain and associated disorders in workers Workplace-based exercise. We found evidence that a workplace exercise program and advice provided in the workplace led to similar outcomes for the management of neck pain in workers [45] (Table 5). Zebis et al. [45] compared a 20week workplace exercise program to advice to stay active in industrial workers with neck pain of unspecified duration. Mixed supervised and unsupervised high-intensity strength training for the neck and shoulder led to a similar reduction in neck/shoulder pain compared with advice.
Adverse events
Eight of the 10 admissible RCTs addressed adverse events. [4143, 4549, 51] None of these studies reported serious adverse events. The rate of minor adverse events associated with exercise therapy varied among studies. Transient nonserious events included worsening of presenting symptoms, neck pain, headache, muscle ache, muscle tension, and nausea.
The frequency of these events rangedfrom 2% in participants performing home stretching exercises [41, 42]
to 45% and 41% in those randomized to supervised qigong and combined exercise, respectively [45],
and 97% in those receiving supervised high dose neck and upper body strengthening exercises. [49]
Discussion
Summary of evidence
Our systematic review suggests that patients with recent neck pain Grade I/II have similar outcomes whether they are managed with home exercises, multimodal manual therapy, or medication (ie, NSAIDs or acetaminophen). However, the risk of mild transient adverse events is higher for those who receive NSAIDs or acetaminophen. [48] We also found evidence that supervised graded strengthening exercises are more effective than advice to continue daily activities but lead to similar outcomes as a semi-hard cervical collar with rest for neck pain Grade III. [50] However, short-term sick leave may be higher among those receiving supervised graded strengthening exercise. We found that supervised qigong exercises, yoga, and combined range-of-motion, strengthening, and flexibility exercises may provide benefit for patients with persistent neck pain. [43, 46, 47]
We found evidence that supervised high-dose strengthening exercises with or without multimodal manual therapy and home range-of-motion exercises lead to similar clinical outcomes in patients with persistent neck pain Grade I/II. [49] Similarly, the evidence suggests that supervised strengthening exercises with home stretching provide no additional benefit over home stretching exercises alone for the management of persistent neck pain. [41, 42, 49]
Finally, a supervised general exercise program with advice and advice alone provide similar reductions in neck pain intensity in patients with persistent WAD Grade I/II. [51] The rate of transient nonserious events is highest in patients receiving high-dose supervised strengthening exercises and lowest in those receiving home-based stretching exercises.
In summary, the evidence does not suggest a clearly superior exercise intervention. Thus, we recommend that clinicians and health policy makers use patient preferences and cost-effectiveness data and consider the risk for transient nonserious events when determining which exercise intervention to recommend for the management of patients with neck pain.
Update of the Bone and Joint Decade 2000 to 2010
Task Force on Neck Pain and Its Associated Disorders
Our review updated the NPTF methodology and results on effectiveness of exercise therapy for the management of neck pain and WAD. In their review, the NPTF included several studies where exercise was a component of a multimodal intervention. Therefore, it was difficult to conclude if the effect of the intervention was specific to exercise or to the other interventions included in the multimodal care. Nonetheless, the NPTF concluded that exercise was more beneficial than manual therapy, TENS, neck collar, or simple advice for the management of persistent neck pain. [4]
We restricted our review to studies designed to isolate the effectiveness of exercise and found evidence that supervised exercise programs including qigong, Iyengar yoga, and combined range-of-motion, strengthening, and flexibility exercises were more effective than advice or wait list. [43, 46, 47]
The NPTF did not find evidence that strengthening exercises were more effective than endurance exercises. [4] Our review supports and expands on this finding. The recent evidence suggests that supervised strengthening exercises are equivalent to home exercises for the management of persistent neck pain. [41, 42, 44, 49] Moreover, qigong exercise programs were equally effective to programs combining strengthening, range-of-motion, and flexibility exercises. [43, 46] Therefore, we did not find evidence of superiority of one type of exercise intervention over another.
The NPTF did not find any evidence on exercise for the management of recent neck pain grade I/II. We updated this finding and found that for recent neck pain grade I/II, home exercise, multimodal manual therapy, or medication leads to similar outcomes. [48]
Our results suggest that a general exercise program provides minimal short-lived benefits over advice alone for the management of persistent WAD Grade I/II. [51] Finally, our update adds to the evidence of the NPTF; our review includes one trial suggesting that patients with Grade III neck pain treated with supervised graded strengthening exercises experience similar outcomes as those treated with a semi-rigid collar and rest. [50]
Other systematic reviews
Our results add to the results of reviews conducted because of the publication of the NPTF report in 2008. Kay et al. [17] conducted a focused review in 2012 and found evidence favoring neck stretching and strengthening exercises for the management of persistent neck pain. They also concluded that upper extremity stretching and strengthening and general exercise programs were ineffective for the management of neck pain. [17] However, their review was restricted to studies comparing exercise with sham, placebo or no treatment, or with studies comparing exercise and another intervention versus that same intervention. Therefore, they excluded studies that inform the discussion on comparative effectiveness. Another review by Sihawong et al. [18] included studies conducted only in populations of office workers with neck pain. The authors found evidence that strengthening and endurance training were superior to stretching or general exercise. Our review does not support this finding. We found that a workplace high-intensity strength-training program and advice to stay active provide similar outcomes in workers with neck and shoulder pain. [45] Conclusions from other reviews may be systematically different from our own considering that they were derived from a synthesis of evidence from both high- and low-quality trials.
Strengths and limitations
Our study has strengths. First, we developed a sensitive search strategy that was checked through peer review. Second, we defined an explicit set of inclusion and exclusion criteria to identify all possibly relevant citations from the searched literature. Third, we used two independent reviewers for screening and critical appraisal to minimize error and bias. Fourth, we used a well-accepted and valid set of criteria (SIGN) for critical appraisal. In addition, we performed a best-evidence synthesis using only internally valid studies to minimize bias in the reported results. Finally, our methodology was standardized, and all reviewers were trained in critical appraisal before commencing the systematic review.
Our review has limitations. First, we restricted our search to studies published in the English language, which may have resulted in the exclusion of some relevant studies. However, previous reviews have found that the restriction of systematic reviews to English language studies has not led to a bias in the reported results. [63] Second, critical appraisal requires scientific judgment that may vary among reviewers. This potential bias was minimized by training reviewers to use a standardized critical appraisal tool and using a consensus process among reviewers to reach decisions regarding scientific admissibility. Third, our search may not have retrieved all relevant studies, despite our efforts to create a sensitive search strategy. Fourth, we searched the literature from 2000 onward. Clinically relevant studies published before 2000 would have been excluded from this review but were likely captured by the NPTF.
Conclusions
Since 2008, new published evidence is available to inform the debate on the comparative effectiveness of exercise for the management of neck pain and WAD. We found evidence from two RCTs that supervised qigong, and combined programs including strengthening, range-of-motion, and flexibility exercises are effective for the management of persistent neck pain. Similarly, we found evidence from one trial supporting the effectiveness of Iyengar yoga. Evidence from three RCTs indicates that supervised or unsupervised strengthening exercises alone are not more effective than home exercises (stretching or range of motion). Overall, the evidence suggests that supervised exercise interventions (including graded activity, qigong, and combined strengthening, range of motion, and flexibility) are more effective than wait list or advice to stay active in patients with persistent neck pain. However, there is evidence from one RCT that supervised strengthening exercises and home range-of-motion exercises lead to similar outcomes as other conservative interventions (ie, manual therapy, NSAIDs, and acetaminophen) for the management of recent neck pain. Finally, we did not find evidence that one supervised exercise program is superior to another. Overall, most studies reported small effect sizes suggesting that a small clinical effect can be expected with the use of exercise alone.
Acknowledgment
This research was undertaken, in part, thanks to funding from the Canada Research Chairs program. The authors acknowledge the invaluable contributions to this review from Angela Verven, Arthur Ameis, Carlo Ammendolia, David Cassidy, Doug Gross, Gail Lindsay, John Stapleton, Maja Stupar, Mike Paulden, Murray Krahn, Patrick Loisel, Poonam Cardoso, and Roger Salhany. The authors also thank Trish Johns-Wilson at the University of Ontario Institute of Technology for her review of the search strategy.
Author disclosures:
DS: Consulting: Appraisal of guidelines for the Ontario Chiropractic Association. The appraisals were used to prepare a report to be submitted for consideration by the Workplace Safety and Insurance Board, Canada (A, estimated).
MCN: Support for travel to meetings for the study or other purposes (B); Royalties: Wolters Kluwer (B); Speaking/Teaching Arrangements: EuroSpine (B); Trips/Travel: (B); Scientific Advisory Board/Other Office: Palladian Healthcare (B).
PC: Grant: Ontario Ministry of FinanceFinance Services Commission of Ontario (I CDN, Paid directly to institution).
HMS: Nothing to disclose. SV: Nothing to disclose. HY: Nothing to disclose.
JJW: Nothing to disclose.
DAS: Nothing to disclose.
KAR: Nothing to disclose.
GMvdV: Nothing to disclose.
SAM: Consulting fee or honorarium: Member of the Guideline Expert Panel; MIG Project (B).
LJC: Support for travel to meetings for the study or other purposes: Guideline Expert Panel Meetings (A, Paid directly to institution); Consulting: Government of Alberta Department of Finance (Insurance Branch) (A); Grants: WCB Manitoba Scientific Research Competition endMS Research and Training Network (F, Paid directly to institution), Eurospine (D, Paid directly to institution), WCB Manitoba Scientific Research Competition (F, Paid directly to institution), CIHR (E, Paid directly to institution).
CLJ: Nothing to disclose.
Funding:
This study was funded by the Ontario Ministry of Finance and the Financial Services Commission of Ontario (RFP#: No.: OSS_00267175). The funding agency was not involved in the collection of data, data analysis, interpretation of the data, or drafting of the article.
REFERENCES
Hogg-Johnson, S., van der Velde, G., Carroll, L. J. et al (2008).
The Burden and Determinants of Neck Pain in the General Population:
Results of the Bone and Joint Decade 20002010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S3951Murray CJ, Abraham J, Ali MK, et al.
The State of US Health, 1990-2010:
Burden of Diseases, Injuries, and Risk Factors
JAMA 2013 (Aug 14); 310 (6): 591608Carroll, LJ, Hogg-Johnson, S, van der Velde, G et al.
Course and Prognostic Factors for Neck Pain in the General Population:
Results of the Bone and Joint Decade 20002010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S7582Hurwitz, EL, Carragee, EJ, van der Velde, G et al.
Treatment of Neck Pain: Noninvasive Interventions: Results of the
Bone and Joint Decade 20002010 Task Force on Neck Pain
and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123152Childs JD, Cleland JA, Elliott JM, et al.
Neck pain: clinical practice guidelines linked to the
international classification of functioning, disability,
and health from the Orthopedic Section of the
American Physical Therapy Association.
J Orthop Sports Phys Ther 2008;38: A134.Anderson-Peacock, E, Blouin, JS, Bryans, R et al.
Chiropractic Clinical Practice Guideline: Evidence-based Treatment
of Adult Neck Pain Not Due to Whiplash
J Canadian Chiro Assoc 2005 (Sep); 49 (3): 158209Freburger JK, Carey TS, Holmes GM, et al.
Exercise prescription for chronic back or neck pain
who prescribes it? Who gets it? What is prescribed?
Arthritis Rheum 2009;61:192200.Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon HT.
A Randomized Clinical Trial of Exercise and Spinal
Manipulation for Patients with Chronic Neck Pain
Spine (Phila Pa 1976) 2001 (Apr 1); 26 (7): 788797Evans R, Bronfort G, Nelson B, Goldsmith CH.
Two-year Follow-up of a Randomized Clinical Trial of Spinal Manipulation
and Two Types of Exercise Patients With Chronic Neck Pain
Spine (Phila Pa 1976) 2002 (Nov 1); 27 (21): 23832389Chiu TT, Hui-Chan CW, Chein G.
A randomized clinical trial of TENS and exercise
for patients with chronic neck pain.
Clin Rehabil 2005;19:85060.Chiu TT, Lam TH, Hedley AJ.
A randomized controlled trial on the efficacy of exercise
for patients with chronic neck pain.
Spine 2005;30:E17.Hagberg M, Harms-Ringdahl K, Nisell R, Hjelm EW.
Rehabilitation of neck-shoulder pain in women industrial workers:
a randomized trial comparing isometric shoulder endurance training
with isometric shoulder strength training.
Arch Phys Med Rehabil 2000;81: 10518.Ylinen J, Takala EP, Kautiainen H, et al.
Effect of long-term neck muscle training on pressure pain threshold:
a randomized controlled trial.
Eur J Pain 2005;9:67381.Ylinen J, Takala EP, Nykanen M, et al.
Active neck muscle training in the treatment of chronic neck pain in women:
a randomized controlled trial.
JAMA 2003;289:250916.Viljanen M, Malmivaara A, Uitti J, et al.
Effectiveness of dynamic muscle training, relaxation training, or
ordinary activity for chronic neck pain: randomised controlled trial.
BMJ 2003;327:475.Rosenfeld M, Seferiadis A, Carlsson J, Gunnarsson R.
Active intervention in patients with whiplash-associated disorders
improves long-term prognosis: a randomized controlled clinical trial.
Spine 2003;28:24918.Kay TM, Gross A, Goldsmith CH, et al.
Exercises for mechanical neck disorders.
Cochrane Database Syst Rev 2012;8:CD004250.Sihawong R, Janwantanakul P, Sitthipornvorakul E, Pensri P.
Exercise therapy for office workers with nonspecific neck pain: a systematic review.
J Manipulative Physiol Ther 2011;34:6271.Drescher K, Hardy S, Maclean J, et al.
Efficacy of postural and neck stabilization exercises for persons
with acute whiplash-associated disorders: a systematic review.
Physiother Can 2008;60:21523.Guzman J, Haldeman S, Carroll LJ, et al.
Clinical Practice Implications of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders:
From Concepts and Findings to Recommendations
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S199S212Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Abenhaim L, Rossignol M, Valat JP, et al.
The role of activity in the therapeutic management of back pain. Report
of the International Paris Task Force on Back Pain.
Spine 2000;25:1S33S.McGowan J, Sampson M, Lefebvre C, et al.
An evidence based checklist for the peer review of electronic search strategies (PRESS EBC).
Evidence Based Library Inform Pract 2010;5:14954.Sampson M, McGowan J, Cogo E, et al.
An evidence-based practice guideline for the peer review
of electronic search strategies.
J Clin Epidemiol 2009;62:94452.Harbour R, Miller J.
A new system for grading recommendations in evidence based guidelines.
MJ 2001;323:3346.van der Velde G, van Tulder M, Cote P, et al.
The sensitivity of review results to methods used to appraise
and incorporate trial quality into data synthesis.
Spine 2007;32:796806.Carroll LJ, Cassidy JD, Peloso PM, et al.
Systematic search and review procedures: results of the
WHO Collaborating Centre Tsk Force on Mild Traumatic Brain Injury.
J Rehabil Med 2004;(43 Suppl): 114.Carroll LJ, Cassidy JD, Peloso PM, et al.
Methods for the best evidence synthesis on neck pain and its associated disorders:
the Bone and Joint Decade 2000-2010 Task Force on Neck Pain
and Its Associated Disorders.
J Manipulative Physiol Ther 2009;32:S3945.Cote P, Cassidy JD, Carroll L, et al.
A systematic review of the prognosis of acute whiplash and a new
conceptual framework to synthesize the literature.
Spine 2001;26:E44558.Hayden JA, Cote P, Bombardier C.
Evaluation of the quality of prognosis studies in systematic reviews.
Ann Intern Med 2006;144: 42737.Hayden JA, van der Windt DA, Cartwright JL, et al.
Assessing bias in studies of prognostic factors.
Ann Intern Med 2013;158:2806.Slavin RE.
Best evidence synthesis: an intelligent alternative to meta-analysis
J Clin Epidemiol 1995;48:918.Cohen J.
A coefficient of agreement for nominal scales.
Educ Psychol Meas 1960;20:3746.Abrams KR, Gillies CL, Lambert PC.
Meta-analysis of heterogeneously reported trials assessing change from baseline.
Stat Med 2005;24:382344.Follmann D, Elliott P, Suh I, Cutler J.
Variance imputation for overviews of clinical trials with continuous response.
J Clin Epidemiol 1992;45:76973.Carroll LJ, Jones DC, Ozegovic D, Cassidy JD.
How well are you recovering? The association between a simple question
about recovery and patient reports of pain intensity and pain
disability in whiplash-associated disorders.
Disabil Rehabil 2012;34:4552.Lauche R, Langhorst J, Dobos GJ, Cramer H.
Clinically meaningful differences in pain, disability and quality of life
for chronic nonspecific neck paina reanalysis of 4 randomized controlled trials
of cupping therapy.
Complement Ther Med 2013;21:3427.Dunn AS, Passmore SR, Burke J, Chicoine D.
A Cross-sectional Analysis of Clinical Outcomes Following Chiropractic
Care in Veterans With and Without Post-traumatic Stress Disorder
Military Medicine 2009 (Jun); 174 (6): 578583McCarthy MJ, Grevitt MP, Silcocks P, Hobbs G.
The Reliability of the Vernon and Mior Neck Disability Index, and its
Validity Compared With the Short Form-36 Health Survey Questionnaire
European Spine Journal 2007 (Dec); 16 (12): 21112117Moher D, Liberati A, Tetzlaff J, Altman DG.
Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.
BMJ 2009;339:b2535.Salo P, Ylonen-Kayr N, Hakkinen A, et al.
Effects of long-term home-based exercise on health-related
quality of life in patients with chronic neck pain:
a randomized study with a 1-year follow-up.
Disabil Rehabil 2012;34:19717.Hakkinen A, Kautiainen H, Hannonen P, Ylinen J.
Strength training and stretching versus stretching only in the treatment
of patients with chronic neck pain: a randomized one-year follow-up study.
Clin Rehabil 2008;22:592600.von Trott P, Wiedemann AM, Ludtke R, et al.
Qigong and exercise therapy for elderly patients with chronic
neck pain (QIBANE): a randomized controlled study.
J Pain 2009;10:5018.Griffiths C, Dziedzic K, Waterfield J, Sim J.
Effectiveness of specific neck stabilization exercises or a general
neck exercise program for chronic neck disorders:
a randomized controlled trial.
J Rheumatol 2009;36:3907.Zebis MK, Andersen LL, Pedersen MT, et al.
Implementation of neck/shoulder exercises for pain relief
among industrial workers: a randomized controlled trial.
BMC Musculoskelet Disord 2011; 12:205.Rendant D, Pach D, Ludtke R, et al.
Qigong versus exercise versus no therapy for patients
with chronic neck pain: a randomized controlled trial.
Spine 2011;36:41927.Michalsen A, Traitteur H, Ludtke R, et al.
Yoga for chronic neck pain:
a pilot randomized controlled clinical trial.
J Pain 2012;13: 112230.Bronfort G, Evans R, Anderson AV, Svendsen KH, Bracha Y, Grimm RH.
Spinal Manipulation, Medication, or Home Exercise With Advice
for Acute and Subacute Neck Pain: A Randomized Trial
Annals of Internal Medicine 2012 (Jan 3); 156 (1 Pt 1): 110Evans R, Bronfort G, Schulz C, et al.
Supervised Exercise With And Without Spinal Manipulation Performs
Similarly And Better Than Home Exercise For Chronic Neck Pain:
A Randomized Controlled Trial
Spine (Phila Pa 1976). 2012 (May 15); 37 (11): 903914Kuijper B, Tans JT, Beelen A, et al.
Cervical collar or physiotherapy versus wait and see policy
for recent onset cervical radiculopathy: randomised trial.
BMJ 2009;339:b3883.Stewart MJ, Maher CG, Refshauge KM, et al.
Randomized controlled trial of exercise for chronic whiplash-associated disorders.
Pain 2007;128:5968.Andersen CH, Andersen LL, Gram B, et al.
Influence of frequency and duration of strength training for effective
management of neck and shoulder pain: a randomised controlled trial.
Br J Sports Med 2012;46:100410.Andersen LL, Christensen KB, Holtermann A, et al.
Effect of physical exercise interventions on musculoskeletal pain
in all body regions among office workers: a one-year randomized controlled trial.
Man Ther 2010;15:1004.Andersen LL, Jorgensen MB, Blangsted AK, et al.
A randomized controlled intervention trial to relieve and prevent neck/shoulder pain.
Med Sci Sports Exerc 2008;40:98390.Diab AA, Moustafa IM.
The Efficacy of Forward Head Correction on Nerve Root Function and
Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial
Clinical Rehabilitation 2012 (Apr); 26 (4): 351361Helewa A, Goldsmith CH, Smythe HA, et al.
Effect of therapeutic exercise and sleeping neck support on
patients with chronic neck pain: a randomized clinical trial.
J Rheumatol 2007;34:1518.Jull G, Falla D, Treleaven J, et al.
Retraining cervical joint position sense:
the effect of two exercise regimes.
J Orthop Res 2007;25: 40412.Lansinger B, Larsson E, Persson LC, Carlsson JY.
Qigong and exercise therapy in patients with long-term
neck pain: a prospective randomized trial.
Spine 2007;32:241522.Salo PK, Hakkinen AH, Kautiainen H, Ylinen JJ.
Effect of neck strength training on health-related quality of life in
females with chronic neck pain: a randomized controlled 1-year follow-up study.
Health Qual Life Outcomes 2010;8:48.Vikne J, Oedegaard A, Laerum E, et al.
A randomized study of new sling exercise treatment vs traditional
physiotherapy for patients with chronic whiplash-associated
disorders with unsettled compensation claims.
J Rehabil Med 2007;39:2529.Ylinen J, Kautiainen H, Wiren K, Hakkinen A.
Stretching exercises vs manual therapy in treatment of
chronic neck pain: a randomized, controlled cross-over trial.
J Rehabil Med 2007;39:12632.Ernst E, Pittler MH, Wider B, Boddy K.
Oxford Handbook of Complementary Medicine.
Oxford Medicine Online. Oxford University Press, Oxford, 2010. Available at:
http://oxfordmedicine.com/view/10.1093/med/9780199206773.001.0001/
med-9780199206773-chapter-3#med-9780199206773-div1-39
Accessed August 21, 2013.Johnson AP, Sikich NJ, Evans G, et al.
Health technology assessment: a comprehensive framework
for evidence-based recommendations in Ontario.
Int J Technol Assess Health Care 2009;25:14150.
Return to WHIPLASH
Return to EXERCISE AND CHIROPRACTIC
Since 10-14-2020


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |
