

The Course and Factors Associated with Recovery of
Whiplash-associated Disorders: An Updated Systematic
Review by the Ontario Protocol for Traffic
Injury Management (OPTIMa) CollaborationThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: European J Physiotherapy 2020 (Mar 25); 23 (5): 116 ~ FULL TEXT
OPEN ACCESS Heather M. Shearer Linda J. Carroll Pierre Cτtι Kristi Randhawa Danielle Southerst Sharanya Varatharajan Jessica J. Wong Hainan Yu Deborah Sutton Gabrielle van der Velde Margareta Nordin Douglas P. Gross Silvano Mior Maja Stupar Craig Jacobs Anne Taylor-Vaisey
UOIT-CMCC Centre for the Study of Disability Prevention and Rehabilitation,
Ontario Tech University and Canadian Memorial Chiropractic College (CMCC),
Oshawa, Canada
Purpose: To update the findings of the Bone and Joint Decade 20002010 Task Force on Neck Pain and Its Associated Disorders (Neck Pain Task Force) on prognostic factors for whiplash-associated disorder (WAD) outcomes.
Materials and methods: We conducted a systematic review and best-evidence synthesis. We systematically searched MEDLINE, EMBASE, CINAHL and PsycINFO from 20002017. Random pairs of reviewers critically appraised eligible studies using the Scottish Intercollegiate Guidelines Network criteria.
Results: We retrieved 10,081 articles. Of those, 100 met inclusion criteria. After critical appraisal, 74 were judged to have low risk of bias. This adds to the 47 admissible studies found by the Neck Pain Task Force. Twenty-two related to course of recovery; 59 to prognostic factors in recovery; and 16 reported other WADs outcomes. Some studies related to more than one category. Findings suggest that half of those with WADs will experience substantial improvement within three months and cessation of symptoms within six months. Among factors associated with recovery are post-crash psychological factors, including expectations for recovery and coping.
Conclusions: Our review adds to the Neck Pain Task Force by clarifying the role of prognostic factors. Evidence supports the important role of post-crash psychological factors in WADs recovery.
Keywords: Systematic review; whiplash; prognosis; recovery; neck pain
From the FULL TEXT Article:
Introduction
Whiplash injuries are common, with increasing frequency of visits to emergency rooms in the western world. [1] Recent estimates suggest that in North America and Western Europe, at least 300 per 100,000 inhabitants seek health care in emergency departments each year because of such injuries. [1] This figure does not capture those who do not attend emergency departments, and some estimates place the actual incidence at up to 600 per 100,000 inhabitants. [2]
Whiplash is an acceleration-deceleration mechanism of injury to the neck that results in whiplash-associated disorders (WADs). [3] In 1995, the Quebec Task Force on Whiplash-Associated Disorders proposed that WAD includes neck pain and other symptoms such as dizziness, headache, memory loss, and temporomandibular joint pain. [3] Subsequent studies have added other common symptoms such as low back pain, difficulty concentrating, depressive symptomatology and widespread pain to the list of WADrelated symptoms. [47] Because of limited evidence available at that time on prognostic factors for WAD recovery, the Quebec Task Force could only hypothesise that initial severity of injury predicted symptom persistence. [3]
Since the Quebec Task Force report, there have been several systematic reviews of WAD prognosis, including the 2008 best evidence synthesis from the Bone and Joint Decade 20002010 Task Force on Neck Pain and Its Associated Disorder (Neck Pain Task Force). [8] In that review, Carroll et al. provided an estimate that 50% of persons with WAD continue to experience symptoms one year postcollision, although fewer (approximately 10%) report daily neck pain or significant health impairment at that time. [8] In addition to the Neck Pain Task Force (NPTF) report, there have been several meta-analyses of risk factors for poor outcomes. [911] In the most recent updated meta-analysis, Walton et al. cited 12 significant factors, including prior pain, initial neck pain, catastrophizing and female sex, among other factors. [11] However, their inclusion/exclusion criteria were necessarily driven by the needs of the meta-analysis, and only nine studies representing four distinct cohorts were retained for their analysis. Thus, a systematic review (best evidence synthesis), designed to update the 2008 findings of the NPTF, was undertaken. In 2008, the current evidence suggested that initial symptom severity, psychological factors and type of compensation system/legal factors predicted poorer recovery. [8] However, even with the increased number of WAD studies available at the time of that review, the NPTF indicated that fundamental questions remained about prognostic factors for recovery. [8]
The aim of this systematic review was to update the findings of the NPTF on prognostic factors for WAD outcomes by identifying new evidence and integrating it with the evidence previously synthesised by the NPTF.
Materials and methods
Registration
The protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) on 17 May 2013 (CRD42013004610).

Eligibility criteria

Table 1 Study characteristics
Eligible studies met the following criteria during citation and full text screening:(1) English language;
(2) published between 1st January 2000 to 14th February 2017;
(3) longitudinal design; and
(4) 30 adults or children with WAD Grades IIII, using the Quebec Task Force classification (Table 1). [3]We excluded:
(1) letters, editorials, commentaries, unpublished manuscripts, dissertations, government reports, books and book chapters, conference proceedings, meeting abstracts, lectures and addresses, consensus development statements, or guideline statements;
(2) cross-sectional studies, case reports, qualitative studies, reviews, practice guidelines, biomechanical studies, or laboratory studies;
(3) studies primarily about intervention effectiveness; or
(4) cadaveric or animal studies.In addition, for course of recovery, we included those studies which tracked recovery with at least one follow-up point in the first six months post-injury, and which followed the participants at least until approximately half were recovered.
Information sources
We developed our search strategy with a health sciences librarian and a second librarian peer reviewed the strategy using the Peer Review of Electronic Search Strategies (PRESS) Checklist. [12, 13] We searched MEDLINE, EMBASE, CINAHL and PsycINFO. The search strategy was developed in MEDLINE (Supplementary Appendix 1) and adapted to the other bibliographic databases. Search terms included subject headings and free text words relevant to WAD prognosis or recovery. We downloaded the search results into reference managing software.
Study selection
We used a two-stage screening process (title/abstracts and full text) with randomly assigned pairs of independent reviewers. We stratified reviewers by level of experience with the systematic review/critical appraisal experience (senior vs. junior), and drew one name, blindly, from each group. The two individuals were paired for a set of reviews. We repeated this process to yield a different pairing for the next set of reviews. Disagreements were resolved by discussion. A third reviewer was used to resolve disagreements if consensus could not be reached.
Risk of bias assessment
Relevant studies were critically appraised by random pairs of trained, independent reviewers, using the Scottish Intercollegiate Guidelines Network criteria for cohort and case control studies. [14] Where consensus between reviewers could not be reached, a third reviewer was employed. Authors were contacted for further information when necessary. Those studies judged to have adequate internal validity (low-to-moderate risk of bias) were included in our synthesis. [15]
Data extraction and synthesis of results
The lead author extracted data from all scientifically admissible studies into evidence tables, which were independently checked by a second reviewer. Findings are reported in three main sections: course of recovery, factors associated with recovery, and other outcomes. For course of recovery, we combined those findings from studies reported by the NPTF and new studies that met our inclusion criteria. We classified the criteria used to define recovery as stringent, less stringent and other. We considered stringent criteria for recovery to include: no or almost no neck pain (self-report of no neck pain/symptoms or pain intensity of ≤1/10 on Numeric Rating Scale or ≤10/100 on Visual Analogue Scale); Neck Disability Index Score of ≤5/50 (classified as no disability) [16] and yes to have you recovered? We classified criteria as less stringent where cut-off scores were 3/10 on Numeric Rating Scale or 30/100 on Visual Analogue Scale (since scores up to 3/10 Numeric Rating Scale and 30/100 on Visual Analogue Scale have been shown to reflect mild pain) [17, 18]; 30% (15/50) on Neck Disability Index (which includes mild disability) [16], and self-report of all better or quite a bit improved (shown to reflect an average pain intensity score of 23/10 on Numeric Rating Scale). [19]

Table 2 In best evidence synthesis, more weight is given to studies whose designs make them least vulnerable to bias and confounding. Thus, for the synthesis of factors associated with recovery, we used a hierarchical classification system with three levels of evidence, Phases I, II or III (Table 2). [8, 2022]
Where the findings across studies were discordant, we used scientific judgment, based on methodological quality, to weigh the evidence, and gave the most weight to PhaseIII studies, followed by Phase-II studies and the least weight to Phase-I studies. This decision framework was adapted from work previously reported by the NPTF [8] and by Altman and Lyman. [23] Terminology used to report the summary of evidence is as follows:
- Evidence: at least one Phase-III study
- Preliminary evidence: Phase-I and Phase-II studies only
- Consistent: all studies agree on the association
- Preponderance: findings are variable, but there is agreement among the stronger studies or among the majority of studies of similar strength
- Varies: no agreement among studies of similar strength
- Limited: three or fewer studies on the topic are available
We present reviewer agreement for the screening of the titles/abstracts and for critical appraisals using kappa statistic (k) with 95% confidence interval (CI). [24]

Reporting
The systematic review was organised and reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. [25]
Results
Results of the search and screening
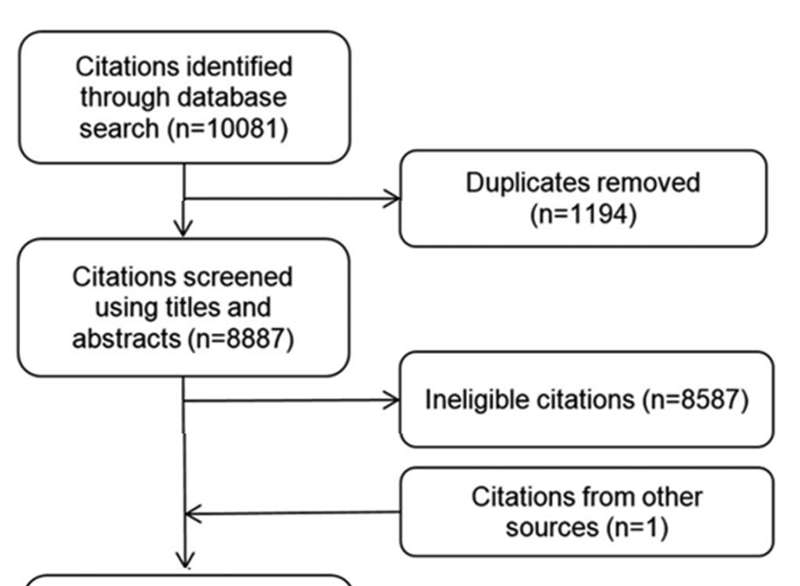
Figure 1
page 4

Table 3

Table 4+5
page 6+Our search yielded 10,081 articles. We removed 1,194 duplicates and screened 8,887 articles for eligibility (Figure 1). One hundred articles were relevant and had not been reviewed by the NPTF. After critical appraisal, 74 studies were judged to have low to moderate risk of bias and were included in our synthesis (Supplementary Appendix 2, Tables 1 and 2). Twenty-two studies related to course of recovery (Supplementary Appendix 3), 59 studies reported factors associated with WAD recovery (Supplementary Appendix 4) and 16 studies reported on WAD outcomes other than recovery (Supplementary Appendix 5). Some studies related to more than one topic and are therefore included in more than one evidence table. This adds to the eight studies on course of recovery reported by the NPTF and which meet the above criteria; to the 29 studies on factors associated with WAD recovery reported by the NPTF and to the nine studies of other outcomes reported by the NPTF. [8] All new studies were cohort studies and related to adults with WAD.
Inter-rater agreement for article screening was κ = 0.93 (95% CI 0.91, 0.96) and percentage agreement (prior to consensus discussions) for critical appraisals of articles was 81.6%. We did not perform a meta-analysis due to heterogeneity of studies with respect to patient populations, predictors and outcomes. A non-quantitative synthesis of findings from the studies with low to moderate risk of bias was performed according to principles of best evidence synthesis by combining evidence from the NPTF and our update. [8, 15] The findings were summarised and organised by type of criterion used to define recovery (course of recovery) and type of factor studied (factors predicting recovery). For detailed findings, see Supplementary Appendix 6. Tables 35 show the number of studies included from the NPTF and this update, as well as phase and type of factor studied.

Findings: course of WAD recovery
Please refer to Supplementary Appendix 3, Table 1 for additional detail.WAD recovery in children
Only one study from the NPTF reported on WAD recovery in children, and this study found rapid recovery, with a mean of 8.8 days to symptom cessation. [26] No study on WAD recovery in children was found in the update.
WAD recovery in adults
The NPTF concluded that one year after the injury event, 50% of adults have neck symptoms which they attribute to WAD. However, confidence in these findings was limited by a number of factors including: variability in definitions of recovery and a paucity of studies with sufficient and early enough follow-up points to accurately track recovery. Only eight of the 20 studies reported by the NPTF tracked recovery within the first six months and followed participants long enough for at least half to have recovered (our current inclusion criteria). [2, 2733] In addition, the NPTF pointed out that neck pain is endemic in the general population and therefore in some cases, neck symptoms attributed to WAD may in fact reflect the background prevalence of neck pain. [8]In addition to these eight studies found by the NPTF, the update found 22 studies consisting of 20 distinct cohorts. [3454] In combining findings from the NPTF and the update, recovery rate depended largely on the definition used for recovery. Fourteen studies (two from the NPTF and 12 studies of 11 distinct cohorts from the update) used a stringent criterion to define recovery. [30, 31, 3445] The preponderance of these studies found that approximately 50% of study participants reached that criterion at or about the six month mark. [3442] One of the preceding studies included two cohorts, one of which recovered more slowly [42], as did one other new study. [43] In contrast, four studies (two from the NPTF and two new studies, both from the same source population [44, 45]) found faster recovery. Source population did not seem to be related to discrepancies.
Three studies reported in the NPTF and eight studies of seven distinct cohorts from the update [27, 29, 32, 4653] used less stringent indices of recovery. The preponderance of these studies found that median time to recovery was less than six months. These studies included persons seeking health care, including those presenting to emergency departments, with and without insurance claims. In contrast, two new studies using less stringent indices of recovery, both studying insurance claimants, reported average recovery times of one year or longer. [52, 53]
Four studies (three from the NPTF and one new study) reported insurance injury claim closure as an index of recovery, with median time to claim closure varying from one month to more than two years. [2, 28, 33, 53] Whether there is a relationship between claim closure and other indices of recovery appears to vary by jurisdiction. Two of the studies reported by the NPTF found median time to claim closure varied from one month to one year; however, neither study related claim closure to other indices of recovery. [33, 54] A third study from the NPTF found that median time to claim closure varied from six months for no fault claims to one year for tort claims. [2] In that cohort, claim closure was associated with other indices of recovery. [2, 28] In contrast, the study found in the update that used claim closure as an outcome found little difference in pain intensity between those who did and did not settle their claims; however, only 30% had closed their claims at two years despite an average pain intensity of < 16/100 on Visual Analogue Scale. [53]
Finally, one new study reported that 36% of those with WAD reported neck pain at one year. However, the authors noted that not all individuals should be classified as having persistent pain since only 21% had reported symptoms at all three follow-ups (i.e. one-, three- and 12-month follow-up points). [55]

Findings: factors associated with WAD recovery

Table 6
page 8+Please refer to Supplementary Appendix 4, Table 1 for additional detail.
Detailed results of the factors associated with WAD recovery are provided in Supplementary Appendix 6 of the online supplemental material. We present a summary of these findings below and in Table 6.

Sociodemographic factorsSex
The combined preliminary evidence varies on the association between sex and pain recovery. [2, 26, 33, 41, 43, 44, 49, 52, 55, 5677]
There is consistent preliminary evidence of no association between sex and disability recovery, although there is limited preliminary evidence that women report poorer physical health-related quality of life at one year.
Age
The preponderance of combined preliminary evidence suggests that older age is not associated with pain recovery, but the preliminary evidence on the association between age and work capacity or self-perceived disability varies.
[2, 35, 41, 43, 44, 47, 49, 52, 55, 5767, 72, 74, 75, 7880]
Employment factors
The preponderance of preliminary evidence suggests that employment factors are not associated with WAD recovery.
[35, 41, 52, 55, 62, 63, 65, 67, 79]
Education
The preponderance of preliminary evidence now suggests that education is not associated with recovery.
[2, 35, 41, 52, 57, 58, 62, 63, 6567, 73, 79]
Pre-crash health factorsPrior pain
The preliminary evidence about the association of prior neck and other pain and WAD recovery now varies. [2, 34, 47, 55, 5659, 62, 63, 65, 72, 73, 81] However, most of the studies utilised post-injury self-reports of pre-injury pain, which has been shown to have limited validity. [82] However, one study assessing the role of documented pain-related work absence prior to the injury found it to be associated with poorer recovery. [56]
History of WAD
There is limited preliminary evidence that having a prior compensation claim (possibly a proxy for prior WAD) is associated with poorer disability recovery and longer time to claim closure. [52, 74] There is also limited evidence that a history of WAD increases the risk of future prevalent and incident episodes of neck pain. [26, 58, 83]
History of WAD
Body mass index, smoking There is limited evidence that body mass index (BMI) is not associated with recovery and consistent limited preliminary evidence that smoking is not associated with recovery. [52, 63, 64, 74, 84]
Body mass index, smoking
There is limited evidence that body mass index (BMI) is not associated with recovery and consistent limited preliminary evidence that smoking is not associated with recovery. [52, 63, 64, 74, 84]
Pre-injury health: physical and psychological
The preponderance of combined preliminary evidence indicates that pre-crash physical health is not associated with recovery for the longer term (i.e. three to 12 month followup). [2, 55, 62, 63, 65, 69, 73, 85] However, there is now also limited preliminary evidence that prior somatic symptoms may be associated with greater pain in the first six weeks after injury for those who are litigating (but not for non-litigants). [63] There is also limited preliminary evidence that being on extended sick benefits in the five years prior to the injury is associated with negative change in work/employment status one year post-injury. [73]
The preliminary evidence is consistent in suggesting that prior psychological health and personality are not associated with WAD recovery. [62, 65, 67, 69, 86] However, findings on the association between prior physical and psychological health should be interpreted cautiously because of difficulty in accurately ascertaining prior health.

Collision factors
Self-reported collision factors include type of road and reason for travel; front, rear or side collision; speed at the time of collision or speed of colliding vehicles (self-reported); perceived severity of the collision/damage to the vehicle; position in the vehicle; use of airbags, seatbelts and/or headrests; and awareness of impending collision. [2, 8, 26, 33, 55, 5763, 65, 67, 76, 87, 88] The preponderance of combined preliminary evidence related to self-reported collision factors indicates no association with WAD recovery. [2, 8, 26, 5763, 65, 67, 76]] However, there is limited preliminary evidence that: being injured in a car (as opposed to other types of vehicles) is associated with better recovery [33, 55]; while being injured in a vehicle with tow bars and being injured in a collision involving greater mean acceleration measured by a crash recorder are associated with poorer recovery. [87, 88]

Initial post-crash pain, disability, WAD grade and symptomsInitial neck pain intensity
The preponderance of preliminary evidence indicates that greater initial post-WAD neck pain intensity is associated with poorer recovery of pain, self-reported disability and work ability. [2, 43, 47, 49, 58, 6063, 66, 69, 70, 72, 73, 75, 77, 79, 81, 8993]
Initial self-perceived disability
The preponderance of preliminary evidence suggests that greater initial neck disability is associated with poorer disability recovery, but the limited preliminary evidence on the association between initial disability and pain recovery varies.
[52, 55, 64, 71, 72, 74, 75, 79, 80, 8991, 94]
WAD grade
In combining the evidence, the preponderance of preliminary evidence suggests that WAD Grade III was associated with poorer recovery but there is no clear evidence of a difference in recovery between Grades I and II.
[52, 55, 57, 58, 60, 62, 72, 9597]
Other post-crash symptoms and number of post-crash symptoms
The preponderance of limited and preliminary evidence suggests that initial poor concentration but not dizziness is associated with poorer WAD recovery; and there is limited preliminary evidence that greater numbers of symptoms predict poorer WAD recovery.
[34, 35, 43, 55, 62, 72, 98]
Radiographic imaging and physical findingsMagnetic resonance imaging findings
There is consistent preliminary evidence of no association between the following post-collision magnetic resonance imaging findings and WAD recovery: abnormal findings related to disc degeneration, protrusion, narrowing, foraminal stenosis; lordosis; kyphosis or straight cervical spine, alar and transverse ligament changes. [76, 77, 99102] There is limited, preliminary evidence that cervical fatty infiltration measured two weeks after a whiplash injury is associated with self-perceived disability. [64]
Neck range of motion
It should be noted that decreased range of motion is one of the key criteria in distinguishing between WAD Grade I and II. [3] The preliminary evidence varies on the association between initial range of motion and recovery. [61, 72, 76, 80, 81, 98, 103] However, the preponderance of preliminary evidence (reported above) suggests no significant difference in recovery between WAD I and WAD II.
Pain threshold, sympathetic vasoconstrictor response
The preponderance of limited preliminary evidence suggests that initial reduced time to peak pain threshold and postcrash cold pain threshold, but not pressure pain threshold or sympathetic vasoconstrictor response, are associated with poorer disability recovery. [71, 80, 104, 105]
Inflammatory biomarkers
There is limited, preliminary evidence that TNF-a (tumour necrosis factor-alpha) and CRP (C-reactive protein) are associated with disability recovery, while IL-1b (interleukin-1beta) is not. [106]
Eye movement
Limited, preliminary evidence indicates no association between smooth pursuit eye movement and recovery. [107]
Post-crash psychological factors and WAD recoveryAcute stress disorder/post-traumatic stress disorder
The preponderance of preliminary evidence suggests that early symptoms of acute stress disorder/post-traumatic stress disorder are associated with delayed recovery, and there is limited preliminary evidence that catastrophizing and fear avoidance may serve as mediators in this relationship. [34, 41, 64, 69, 71, 72, 77, 80, 89] All used self-report questionnaires rather than formal diagnoses of acute stress disorder or post-traumatic stress disorder.
Anxiety and fear
The preponderance of evidence indicates that post-crash anxiety and fear (pain-related fear/anxiety/worry/kinesiophobia) are associated with poorer recovery. [38, 41, 47, 62, 63, 68, 70, 72, 76, 79, 89, 91, 108]
General psychological health/distress, anger, frustration
The preliminary evidence on the role of post-crash general psychological health/general distress varies and there is limited evidence that pain-related anger and frustration are associated with poorer recovery. [52, 55, 61, 63, 72, 74, 75]
Pain-related beliefs, self-efficacy, perceived injustice
The studies provided limited evidence that certain pain beliefs (that pain can be medically cured and that pain is mysterious) are associated with poorer recovery, while the evidence on the role of perceived control over pain and selfefficacy varies. [45, 72, 89, 109, 110] Limited preliminary evidence suggests that perceived injustice does not predict delayed recovery, although delayed recovery appears to predict increases in perceptions of injustice. [45]
Depressive symptomatology
The preponderance of evidence indicates that early postcrash depressive symptoms are associated with poorer recovery.
[38, 41, 47, 63, 111]
Expectations for recovery
There is consistent evidence that poorer expectations for recovery are associated with poorer recovery.
[37, 44, 63, 66, 72, 77, 109, 112, 113]
Pain coping (excluding catastrophizing)
There is consistent evidence of an association between coping and WAD recovery, although studies were not uniform in what coping constructs they assessed. [67, 72, 78, 110, 111, 114, 115]
Catastrophizing
The preliminary evidence on the role of early post-injury catastrophizing on WAD recovery varies.
[52, 63, 72, 74, 75, 78, 79, 89, 109]
Compensation and legal factors
There was limited, preliminary evidence that claiming under a tort system was associated with slower recovery and that claim closure followed health recovery and limited, preliminary evidence that health recovery did not follow claim closure. [2, 48, 52, 53, 61, 63]
The preliminary evidence on the association between hiring a lawyer and poorer recovery varies. [2, 52, 63, 74, 75] Hiring a lawyer may be related to differing compensation systems and initial symptom severity. [2] Further, there is limited preliminary evidence that the impact of making a claim may be dependent on the severity of the injury. [48]
Post-collision health care factors
The preponderance of evidence indicates that high levels of initial health care utilisation are associated with poorer WAD recovery [47, 116118]; and there is also limited, preliminary evidence that seniority of first treating physician is not associated with recovery. [46]
Risk scores/prediction rules
Five risk scores or prediction rules were found. One Phase-II study reported a parsimonious group of factors associated with moderate-to-severe neck pain at 6 weeks post-injury using Lasso regression techniques, but without external validation. [63] For those not engaged in litigation, a combination of female sex, severe neck and overall pain predicted greater pain at six weeks; while for those litigating, a combination of female sex, having moderate or severe neck pain or severe overall pain, not being employed full time, having no health insurance, having had a rear-end collision, being a passenger rather than a driver, higher levels of peritraumatic distress, a predisposition to anger and higher age predicted greater pain. [63]
In two Phase I studies from the same cohort (and no external validation), a risk score was developed to predict WAD recovery; the risk score consisted of cervical range of motion, neck/head pain intensity, sex, number of non-pain symptoms and pain on palpation predicted WAD recovery outcomes. [98, 119]
In the update, one new Phase II study provided external validation that a set of factors (which had been identified in an earlier study [120]), consisting of high initial Neck Disability Index score, cold hyperalgesia, older age and symptoms of acute post-traumatic stress were associated with moderate/severe disability at 12 months. [80]
Ritchie et al. derived a clinical prediction rule in a Phase-II study [71] and conducted an external validation study on a different cohort. [94] A prediction rule of the combination of initial NDI score, older age and hyperarousal (on the PDS) had good specificity and positive predictive values, but only moderate sensitivity to predict recovery.
Finally, a prediction model was derived using a cohort of ER attendees, and subjected to external validation in a separate cohort of insurance claimants. The set of factors found to predict self-rated recovery in the model building study did not, as a set, adequately predict self-rated recovery in the validation study. [42]
Findings: WAD outcomes other than recoveryWAD and fibromyalgia
The limited and preliminary evidence varies on the association between WAD and onset of fibromyalgia [121123]
(Supplementary Appendix 5, Table 1).
WAD and widespread pain
There is limited preliminary evidence that the risk of widespread pain is similar after WAD and after non-WAD traffic injuries. [4, 63, 124] No factor predicting the onset of widespread pain after WAD was found to be common across these studies; factors included being female, having poorer health, greater pain, more symptoms, and more initial depressive symptoms.
WAD and jaw pain
There is limited preliminary evidence from three studies of two distinct cohorts that those with WAD are at greater risk of new onset of jaw pain than those with non-WAD injuries, either immediately after the injury or with onset during the year following the injury. [40, 125, 126]
WAD and psychological outcomes
There is limited preliminary evidence that WAD was associated with greater post-injury onset of depressive symptoms than non-WAD injuries. [76] There is now consistent but still limited preliminary evidence that poor prior mental health/depression is associated with greater post-collision depression. [7, 38]
There is limited preliminary evidence that initial dizziness is associated with persistent or recurrent post-collision depression [127]; and limited, preliminary evidence that prior anxiety, fear, anger and frustration are each associated with greater intensity of the corresponding pain-related anxiety, fear, anger and frustration at 6 weeks post-collision [38].
There is also limited, preliminary evidence that lower initial cold pain thresholds, greater initial pain intensity and older age are associated with greater severity of post-traumatic stress symptoms during the year following the crash. [49]
WAD and health care utilisation
There is limited preliminary evidence that those using passive pain coping strategies within 7 days of injury are more likely to use prescription pain medication at three weeks post-injury, and that those using few active and many passive pain coping strategies are less likely to comply with referral to an active rehabilitation programme. [128]
There is limited preliminary evidence that in comparison with an injured non-WAD group, those with WAD have greater health care utilisation both prior to and after the injury and are more likely to transition from low to high health care utilisation levels (primarily through visiting physical therapists). [129]
Factors associated with lawyer involvement and WAD
There is limited preliminary evidence that having greater initial self-perceived functional or work disability, speaking a language other than English at home and having poorer initial mental health, were associated with hiring a lawyer within 12 months of the injury. [52] In that study, age, sex, profession, admission to hospital after the collision, socioeconomic status, income, and catastrophization, were not associated with hiring a lawyer within 12 months of the injury.
WAD and muscle activation, spinal cord hyperexcitability, modic changes
There is limited preliminary evidence that those with WAD have no elevated muscle reactivity in the three months following the injury and that greater initial self-perceived disability is associated with reduction in recruitment of trapezius muscle during isometric exercise. [90] There is also limited preliminary evidence that throughout the first 24 weeks post-injury, greater pain and fear of movement are associated with reduction in trapezius muscle recruitment during exercise, and that higher levels of pain intensity strengthen the association between fear of movement and decreased muscle activity on electromyography. [39]
There is limited preliminary evidence that greater initial self-perceived neck disability is associated with spinal cord hyperexcitability at 3 months post-injury. [104]
Limited, preliminary evidence found no association between WAD and modic changes of the cervical spine (at C2-3 to C7-T1) in long term follow-up. [130]
WAD and headaches
There is limited preliminary evidence that headaches experienced after a collision are similar in those with and without WAD, and that the frequency of headaches in those with WAD is similar to individuals without WAD. [131]
Discussion
The current review adds 74 studies to the 47 WAD prognosis studies reported in the 2008 publication by the Bone and Joint Decade 20002010 Task Force on Neck Pain and Its Associated Disorders. The course of recovery has become clearer, and the evidence suggests that median time to recovery is three to six months, depending on the stringency of ones criteria for having recovered. Although our update identified more studies with follow-up points during the first six months post-crash, the synthesis of the data remains challenging for several reasons. First, there is much variability in the frequency and timing of follow-up and the study samples are heterogeneous (population-based WAD studies, compensation claim samples, emergency department sampling frames, hospital admissions or referrals to specialists, and those referred to research centres or RCTs). Therefore, it is difficult to identify clear and consistent patterns with time to recovery (e.g. recovery in six months or less, median time to claim closure, etc.) because of the heterogeneous nature of the studies.
Secondly, there is no predominant or standardised definition of recovery for this population. This has been discussed in previous work but little progress has been made in developing a standard list of outcomes. [11, 132] The current literature typically reports on neck pain and/or disability/functional outcomes as indices of recovery; however, there is variability in the criterion used to distinguish recovered from non-recovered. Additional definitions of recovery include self-ratings of global recovery, WAD symptoms other than neck pain (e.g. headache) and personal injury insurance claim closure. A qualitative study exploring what persons with recent musculoskeletal injuries (not limited to neck) considered recovered to mean found that there were two main definitions: either total pain/symptom cessation accompanied by pain-free function, or the ability to function despite some residual pain. [133] In contrast, another qualitative study examining how those with chronic trauma-related neck pain (including WAD) defined recovery found five main criteria: absent or manageable symptoms, ability to participate in life roles, having the physical capability one ought to have, feeling positive emotions, and feeling like oneself again. [134] It seems likely that for those with musculoskeletal conditions, their criteria for what constitutes recovery changes as pain problems fail to resolve.
Thirdly, a lack of WAD-grade stratified findings makes it difficult to determine usual course of recovery in those with WAD III. WAD III with confirmed radiculopathy is relatively uncommon, and although many studies in our update included WAD IIII in their inclusion criteria, they rarely reported the number of each grade in their studies.
With the increased body of literature, the prognostic role of many factors is clearer, although uncertainty remains for some, such as range of motion. In particular, new findings since the NPTF highlight the importance of post-collision psychological factors in WAD recovery. Pain coping and depression were identified as prognostic factors in the previous report. The update strengthens these conclusions and adds: poor expectations for recovery, symptoms of acute stress disorder or post-traumatic stress disorder, anxiety, fear and anger. Below, we report summary statements that integrate the main findings from the NPTF and the update, according to the strength of evidence for these findings.
Variables associated with poor recovery, based on strong evidence (from confirmatory studies) are: expecting a poor recovery; having pain-related depression, anxiety, fear, frustration or anger; poor coping; and high frequency of health care utilisation in the first weeks after an injury. In addition, prior WAD is a risk factor for future neck pain. Where these findings come from a single confirmatory study, we recommend replication in other samples.
Variables associated with poor recovery, based on preliminary evidence (from exploratory but not confirmatory studies) may include: greater initial pain intensity, greater initial self-reported disability, more symptoms or more severe symptoms, Grade III WAD, post-crash low cold pain threshold, symptoms of acute stress disorder/post-traumatic stress disorder, and kinesiophobia. However, confirmatory studies (Phase III) should be conducted to validate their prognostic value.
Variables not associated with pain recovery, based on preliminary evidence (from exploratory but not confirmatory studies) may include: older age (for pain recovery), sex (for disability recovery), education, employment factors, pre-collision physical and psychological health, self-reported collision characteristics, smoking, post-collision pressure pain threshold, sympathetic vasoconstrictor response, smooth pursuit eye movement, and several types of magnetic resonance imaging findings (degenerative spine changes, alar and transverse ligament changes, kyphosis, lordosis and straight cervical spine). These findings should also be confirmed in Phase III studies.
Finally, there is strong evidence that BMI is not associated with recovery. As above, this should be replicated in other samples.
Several findings in this review are similar to those by Walton et al. [11] These include the associations between initial post-WAD self-reported neck pain intensity and disability and WAD grade III injuries in poorer recovery and lack of association for certain collision factors. A recent meta-review qualitatively synthesised the results of 12 systematic reviews of prognostic factors for outcomes in acute WAD injury. [135] Again, there were consistent findings suggesting an association between initial post-injury pain and disability with ongoing pain and disability. Disparities in some results between reviews may be attributed to methodological differences between the reviews. Differences in eligibility criteria, indices of recovery, best-evidence synthesis using a hierarchical classification system with three levels of evidence, and no statistical pooling in our review (and thus the ability to include studies not reporting their findings in a way that meets the needs of a meta-analysis) may help explain the variances in reported prognostic factors of recovery.
The small number of studies of some prognostic factors means that uncertainty remains about their role in recovery. In addition, no new research study addressed prognostic factors for WAD recovery in children, and there was only one such study reported by the NPTF. It should also be noted that the role of prior physical and psychological health, and prior pain in recovery should still be considered uncertain because of the difficulty in accurately classifying prior health. These are generally assessed through self-report after the crash, and it has, for example, been shown that asking participants with WAD about prior neck pain results in systematic misclassification. [82] Thus, retrospective self-reports of prior health and prior pain should be viewed with caution.
Our review has several strengths. First, our literature search was comprehensive and methodologically rigorous. We broadened the scope of the NPTF search by using five electronic databases. A second, independent librarian reviewed the search strategy to minimise errors. We outlined detailed criteria to identify relevant citations from the searched literature. Second, we used pairs of independent reviewers to screen and critically appraise the literature. Third, we used the Scottish Intercollegiate Guidelines Network (SIGN) criteria to ensure standardisation of the critical appraisal process. Fourth, a standardised methodology was used and all reviewers were trained prior to initiation of this work. Finally, the risk of bias associated with using low quality studies was eliminated by using the best-evidence synthesis method to form our conclusions. [15]
Our review has limitations. First, potentially admissible studies may have been excluded because our literature search was restricted to the English language. However, previous systematic reviews have investigated the impact of language restriction and found that it does not lead to bias as the majority of studies and reviews are published in English. [136140] Second, it is possible that our search missed potentially relevant studies. Finally, the critical appraisal of articles may vary among reviewers. We minimised this potential bias by using standardised appraisal forms, conducting critical appraisal training sessions for reviewers, and using a consensus process to determine study admissibility.
Conclusion
The current best evidence synthesis updates findings published by the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders with respect to prognostic factors in WAD. This update provides a substantial body of evidence supporting the important prognostic role of post-collision psychological factors in WAD recovery.
Acknowledgements
The authors acknowledge and thank all of the individuals who have made important contributions to this review: Carlo Ammendolia, Richard Bohay, Robert Brison, J. David Cassidy, Michel Lacerte, Gail Lindsay, John Stapleton, Angela Verven, and Leslie Verville. The authors also thank Trish Johns-Wilson at the University of Ontario Institute of Technology for her review of the search strategy.
Disclosure statement
Dr Linda Carroll has received reimbursement for travel expenses to attend meetings for the study and grants from CIHR and Workers Compensation Boards in Manitoba and Alberta. Dr Pierre Cote has received a grant from the Ontario Government, Ministry of Finance, and a grant from Aviva Canada. The remaining authors report no declarations of interest.
Funding
This work was funded by the Ontario Ministry of Finance and the Financial Services Commission of Ontario (RFP No.: OSS_00267175). The funding agency was not involved in the collection of data, data analysis, interpretation of the data or drafting of the manuscript. This research was undertaken, in part, thanks to funding from the Canada Research Chairs program and from Alberta Innovates Health Solutions through a Health Senior Scholar Award.
References:
Holm, LW, Carroll, LJ, Cassidy, JD et al.
The Burden and Determinants of Neck Pain in Whiplash-associated Disorders
after Traffic Collisions: Results of the Bone and Joint Decade 20002010
Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S52-59Cassidy JD, Carroll LJ, Cote P, et al.
Effect of eliminating compensation for pain and suffering on
the outcome of insurance claims for whiplash injury.
N Engl J Med. 2000;342:11791186.Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Holm LW, Carroll LJ, Cassidy JD, et al.
Widespread pain following whiplash-associated disorders:
incidence, course, and risk factors.
J Rheumatol. 2007;34:193200.Hincapie CA, Cassidy JD, Cote P, et al.
Whiplash injury is more than neck pain: a population-based
study of pain localization after traffic injury.
J Occup Environ Med. 2010;52:434440.Ferrari R, Russell AS, Carroll LJ, et al.
A re-examination of the whiplash associated disorders (WAD) as a systemic illness.
Ann Rheum Dis. 2005;64:13371342.Carroll LJ, Cassidy JD, Cote P.
Frequency, timing, and course of depressive symptomatology after whiplash.
Spine. 2006;31: E5516.Carroll, LJ, Holm, LW, Hogg-Johnson, S et al.
Course and Prognostic Factors for Neck Pain in Whiplash-associated
Disorders (WAD): Results of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S8392Walton DM, Pretty J, MacDermid JC, et al.
Risk factors for persistent problems following whiplash injury:
results of a systematic review and meta-analysis.
J Orthop Sports Phys Ther. 2009; 39:334350.Kamper SJ, Rebbeck TJ, Maher CG, et al.
Course and prognostic factors of whiplash:
a systematic review and meta-analysis.
Pain. 2008;138:617629.Walton DM, MacDermid JC, Giorgianni AA, et al.
Risk factors for persistent problems following acute whiplash injury:
update of a systematic review and meta-analysis.
J Orthop Sports Phys Ther. 2013;43:3133.Sampson M, McGowan J, Cogo E, et al.
An evidence-based practice guideline for the peer review
of electronic search strategies.
J Clin Epidemiol. 2009;62:944952.McGowan J, Sampson M, Lefebvre C.
An evidence based checklist for the Peer Review of Electronic Search Strategies (PRESS EBC).
EBLIP. 2010;5:149154.Harbour R, Miller J.
A new system for grading recommendations in evidence based guidelines.
BMJ. 2001;323:334335.Slavin RE.
Best evidence synthesis: an intelligent alternative to meta-analysis.
J Clin Epidemiol. 1995;48:918.Vernon H, Mior S.
The Neck Disability Index: A Study of Reliability and Validity
J Manipulative Physiol Ther 1991 (Sep); 14 (7): 409415Gerbershagen HJ, Rothaug J, Kalkman CJ, et al.
Determination of moderate-to-severe postoperative pain on the numeric
rating scale: a cut-off point analysis applying four different methods.
Br J Anaesth. 2011;107:619626.Collins SL, Moore RA, McQuay HJ.
The visual analogue pain intensity scale: what is moderate pain in millimetres?
Pain. 1997; 72:9597.Carroll LJ, Jones D, Ozegovic D, et al.
How well are you recovering: the association between a simple question
about recovery and patient reports of pain intensity and
pain disability in whiplash-associated disorders.
Disabil Rehabil. 2012;34:4552.Cote P, Cassidy JD, Carroll LJ, et al.
A systematic review of the prognosis of acute whiplash and a
new conceptual framework to synthesize the literature.
Spine. 2001;26:E44558.Carroll LJ, Cassidy JD, Cote P.
Depression as a risk factor for onset of an episode
of troublesome neck and low back pain.
Pain. 2004;107:134139.Hogg-Johnson, S, van der Velde, G, Carroll, LJ et al.
The Burden and Determinants of Neck Pain in the General Population:
Results of the Bone and Joint Decade 20002010 Task Force on
Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S3951Altman DG, Lyman GH.
Methodological challenges in the evaluation of
prognostic factors in breast cancer.
Breast Cancer Res Treat. 1998;52:289303.Cohen J.
A coefficient of agreement for nominal scales.
Educ Psychol Meas. 1960;20:3746.Moher D, Liberati A, Tetzlaff J, et al.; The PRISMA Group.
Preferred reporting items for systematic reviews and meta-analyses:
the PRISMA Statement.
PLoS Med. 2009;6:e1000097.Bylund PO, Bjornstig U.
Sick leave and disability pension among passenger car occupants injured in urban traffic.
Spine (Phila Pa 1976.). 1998;23:10231028.Cassidy JD, Carroll LJ, Cote P, et al.
Does multidisciplinary rehabilitation benefit whiplash recovery?:
results of a population-based incidence cohort study.
Spine (Phila Pa 1976.). 2007; 32:126131.Cote P, Hogg-Johnson S, Cassidy JD, et al.
The association between neck pain intensity, physical functioning,
depressive symptomatology and time-to-claim-closure after whiplash.
J Clin Epidemiol. 2001;54:275286.Kasch H, Bach FW, Stengaard-Pedersen K, et al.
Development in pain and neurologic complaints after whiplash:
a 1-year prospective study.
Neurology. 2003;60:743749.Obelieniene D, Schrader H, Bovim G, et al.
Pain after whiplash: a prospective controlled inception cohort study.
J Neurol Neurosurg Psychiatry. 19 9;66:279283.Partheni M, Constantoyannis C, Ferrari R, et al.
A prospective cohort study of the outcome of acute whiplash injury in Greece.
Clin Exp Rheumatol. 2000;18:6770.Sterling M, Jull G, Vicenzino B, et al.
Development of motor system dysfunction following whiplash injury.
Pain. 2003;103:6573.Suissa S, Harder S, Veilleux M. Section 2.
The Quebec Whiplash-Associated Disorders Cohort Study.
Spine. 1995;20:12S20S.Buitenhuis J, de Jong PJ, Jaspers JP, et al.
Relationship between posttraumatic stress disorder symptoms
and the course of whiplash complaints.
J Psychosom Res. 2006;61:681689.Buitenhuis J, de Jong PJ, Jaspers JP, et al.
Work disability after whiplash: a prospective cohort study.
Spine. 2009;34:262267.Crutebo S, Nilsson C, Skillgate E, et al.
The course of symptoms for whiplash-associated disorders
in Sweden: 6-month followup study.
J Rheumatol. 2010;37:15271533.Carroll LJ, Holm LW, Ferrari R, et al.
Recovery in whiplash-associated disorders: do you get what you expect?
J Rheumatol. 2009; 36:10631070.Carroll LJ, Liu Y, Holm LW, et al.
Pain-related emotions in early stages of recovery in whiplash-associated disorders:
their presence, intensity, and association with pain recovery.
Psychosomatic Med. 2011;73:708715.Nederhand MJ, Hermens HJ, Ijzerman MJ, et al.
The effect of fear of movement on muscle activation
in posttraumatic neck pain disability.
Clin J Pain. 2006;22:519525.Carroll LJ, Ferrari R, Cassidy JD.
Reduced or painful jaw movement after collision-related injuries:
a population-based study.
J Am Dent Assoc. 2007;138:8693.Andersen TE, Karstoft KI, Brink O, et al.
Pain-catastrophizing and fear-avoidance beliefs as mediators between
post-traumatis stress symptoms and pain following whiplash injury -
a prospective cohort study.
Eur J Pain. 2016;20:12411252.Rydman E, Ponzer S, Ottosson C, et al.
Predicting non-recovery among whiplash patients in the
emergency room and in an insurance company setting.
Eur Spine J. 2017;26:12541261.Buitenhuis J, de Jong PJ, Jaspers JP, et al.
Catastrophizing and causal beliefs in whiplash.
Spine. 2008;33:24272433. Discussion 34.Ferrari A.
Predicting recovery from whiplash injury in the primary care setting.
Aust Fam Physician. 2014;43:559562.Ferrari R.
A prospective study of perceived injustice in whiplash
victims and its relationship to recovery.
Clin Rheumatol. 2015; 34:975979.Pieske O, Weinhold T, Buck J, et al.
Seniority of the first-treating doctor does not influence the
outcome of acute whiplash injury: a prospective cohort study.
Eur Spine J. 2010;19:16271634.Bohman T, Cote P, Boyle E, et al.
Prognosis of patients with whiplash-associated disorders consulting physiotherapy:
development of a predictive model for recovery.
BMC Musculoskelet Disord. 2012;13:264.Sterling M, Hendrikz J, Kenardy J.
Compensation claim lodgement and health outcome developmental trajectories
following whiplash injury: a prospective study.
Pain. 2010;150:2228.Sterling M, Hendrikz J, Kenardy J.
Similar factors predict disability and posttraumatic
stress disorder trajectories after whiplash injury.
Pain. 2011;152:12721278.Bostick GP, Brown CA, Carroll LJ, et al.
If they can put a man on the moon, they should be able to fix a neck injury:
a mixedmethod study characterizing and explaining pain beliefs about WAD.
Disabil Rehabil. 2012;34:16171632.Kamper SJ, Maher CG, Hush JM, et al.
Relationship between pressure pain thresholds and pain ratings
in patients with whiplash-associated disorders.
Clin J Pain. 2011;27:495501.Casey PP, Feyer AM, Cameron ID.
Associations with legal representation in a compensation setting 12 months after injury.
Injury. 2015;46:918925.Spearing NM, Gyrd-Hansen D, Pobereskin LH, et al.
Are people who claim compensation cured by a verdict?
A longitudinal study of health outcomes after whiplash?
J Law Med. 2012;20: 8292.Suissa S, Giroux M, Gervais M, et al.
Assessing a whiplash management model:
a population-based non-randomized intervention study.
J Rheumatol. 2006;33:581587.Atherton K, Wiles NJ, Lecky FE, et al.
Predictors of persistent neck pain after whiplash injury.
Emerg Med J. 2006;23:195201.Borchgrevink GE, Lereim I, Royneland L, et al.
National health insurance consumption and chronic symptoms
following mild neck sprain injuries in car collisions.
Scand J Soc Med. 1996;24: 264271.Miettinen T, Airaksinen O, Lindgren KA, et al.
Whiplash injuries in Finlandthe possibility of some sociodemographic
and psychosocial factors to predict the outcome after one year.
Disabil Rehabil. 2004;26:13671372.Berglund A, Bodin L, Jensen I, et al.
The influence of prognostic factors on neck pain intensity, disability,
anxiety and depression over a 2-year period in subjects
with acute whiplash injury.
Pain. 2006;125:244256.Sterner Y, Toolanen G, Gerdle B, et al.
The incidence of whiplash trauma and the effects of different factors on recovery.
J Spinal Disord Techniq. 2003;16:195199.Hartling L, Pickett W, Brison RJ.
Derivation of a clinical decision rule for whiplash associated disorders
among individuals involved in rear-end collisions.
Accid Anal Prev. 2002;34: 531539.Kasch H, Bach FW, Jensen TS.
Handicap after acute whiplash njury:
a 1-year prospective study of risk factors.
Neurology. 2001;56:16371643.Cobo EP, Mesquida ME, Fanegas EP, et al.
What factors have influence on persistence of neck pain after a whiplash?.
Spine. 2010;35:E338E343.McLean SA, Ulirsch JC, Slade GD, et al.
Incidence and predictors of neck and widespread pain after
motor vehicle collision among US litigants and non-litigants.
Pain. 2014;155:309321.Elliott JM, Courtney DM, Rademaker A, et al.
The rapid and progressive degeneration of the cervical multifidus
in whiplash: a MRI study of fatty infiltration.
Spine. 2015;40:E694E700.Carstensen TB, Frostholm L, Oernboel E, et al.
Post-trauma ratings of pre-collision pain and psychological distress
predict poor outcome following acute whiplash trauma: a 12-month followup study.
Pain. 2008;139:248259.Gehrt TB, Carstensen TBW, Ornbol E, et al.
The role of illness perceptions in predicting outcome after acute
whiplash trauma. A multicenter 12-month follow-up study.
Clin J Pain. 2015;31: 1420.Carstensen TB, Frostholm L, Oernboel E, et al.
Are there gender differences in coping with neck pain
following acute whiplash trauma? A 12-month follow-up study.
EJP. 2012;16:4960.Buitenhuis J, Jaspers JP, Fidler V.
Can kinesiophobia predict the duration of neck symptoms in acute whiplash?
Clin J Pain. 2006; 22:272277.Kongsted A, Bendix T, Qerama E, et al.
Acute stress response and recovery after whiplash injuries.
A one-year prospective study.
Eur J Pain. 2008;12:455463.Pedler A, Sterling M.
Assessing fear-avoidance beliefs in patients with whiplash-
associated disorders: a comparison of 2 measures.
Clin J Pain. 2011;27:502507.Ritchie C, Hendrikz J, Kenardy J, et al.
Derivation of a clinical prediction rule to identify both chronic
moderate/severe disability and full recovery following whiplash injury.
Pain. 2013;154: 21982206.Williamson E, Williams MS, Gates S, et al.
Risk factors for chronic disability in a cohort of patients with acute
whiplash associated disorders seeking physiotherapy
treatment for persisting symptoms.
Physiotherapy. 2015;101:3443.Carstensen TBW, Fink P, Oernboel E, et al.
Sick leave within 5 years of whiplash trauma predicts recovery:
a prospective cohort and register-based study.
PLoS One. 2015;10:e0130298.Casey PP, Feyer AM, Cameron ID.
Associations with duration of compensation following
whiplash sustained in a motor vehicle crash.
Injury. 2015;46:18481855.Casey PP, Feyer AM, Cameron ID.
Course of recovery for whiplash associated disorders in a compensation setting.
Injury. 2015;46:21182129.Richter M, Ferrari R, Otte D.
Correlation of clinical findings, collision parameters, and psychological
factors in the outcome of whiplash associated disorders.
J Neurol Neurosurg Psychiatry. 2004;75:758764.Vetti N, Krεkenes J, Eide GE, et al.
Are MRI high-signal changes of alar and transverse ligaments
in acute whiplash injury related to outcome?.
BMC Musculoskelet Disord. 2010;11:260.Kivioja J, Jensen I, Lindgren U.
Early coping strategies do not influence the prognosis after whiplash injuries.
Injury. 2005;36: 935940.Nieto R, Miro J, Huguet A.
Pain-related fear of movement and catastrophizing in whiplash-associated disorders.
Rehabil Psychol. 2013;58:361368.Sterling M, Hendrikz J, Kenardy J, et al.
Assessment and validation of prognostic models for poor functional recovery
12 months after whiplash injury: a multicentre inception cohort study.
Pain. 2012;153:17271734.Drottning M, Staff PH, Sjaastad O.
Cervicogenic headache (CEH) after whiplash injury.
Cephalalgia. 2002;22:165171.Don AS, Carragee EJ.
Is the self-reported history accurate in patients
with persistent axial pain after a motor vehicle accident?.
Spine J. 2009;9:412.Nolet PS, Cote P, Cassidy JD, et al.
The association between a lifetime history of a neck injury in a
motor vehicle collision and future neck pain:
a population-based cohort study.
Eur Spine J. 2010;19:972981.Yang X, Cote P, Cassidy JD, et al.
Association between body mass index and recovery from whiplash injuries:
a cohort study.
Am J Epidemiol. 2007;165:10631069.Palmof L, Cote P, Carroll LJ, et al.
Are prevalence self-reported cardiovascular disorders associated with
delayed recovery from whiplash-associated disorders:
a population-based cohort study.
Clin J Pain. 2015;31:247253.Pettersson K, BrNdstrM S, Toolanen GR, et al.
Temperament and character: prognostic factors in whiplash patients?.
Eur Spine J. 2004;13:408414.Krafft M, Kullgren A, Tingvall C, et al.
How crash severity in rear impacts influences short- and
long-term consequences to the neck.
Accident Anal Prev. 2000;32:187195.Krafft M, Kullgren A, Ydenius A, et al.
Influence of crash pulse characteristics on whiplash associated
disorders in rear impactscrash recording in real life crashes.
Traffic Inj Prev. 2002;3: 141149.Asenlof P, Bring A, Soderlund A.
The clinical course over the first year of whiplash associated disorders
(WAD): pain-related disability predicts outcome
in a mildly affected sample.
BMC Musculoskelet Disord. 2013;14:361.Nederhand MJ, Hermens HJ, IJzerman MJ, et al.
Chronic neck pain disability due to an acute whiplash injury.
Pain. 2003;102: 6371.Nederhand MJ, Ijzerman MJ, Hermens HJ, et al.
Predictive value of fear avoidance in developing chronic neck pain
disability: consequences for clinical decision making.
Arch Phys Med Rehabil. 2004;85:496501.Suissa S.
Risk factors of poor prognosis after whiplash injury.
Pain Res Manage. 2003;8:6975.Suissa S, Harder S, Veilleux M.
The relation between initial symptoms and signs
and the prognosis of whiplash.
Eur Spine J. 2001;10:4449.Ritchie C, Hendrikz J, Jull G, et al.
External validation of a clinical prediction rule to predict full
recovery and ongoing moderate/severe disability following acute whiplash injury.
J Orthop Sports Phys Ther. 2015;45:242250.Kivioja J, Jensen I, Lindgren U.
Neither the WAD-classification nor the Quebec Task Force follow-up regimen
seems to be important for the outcome after a whiplash injury.
A prospective study on 186 consecutive patients.
Eur Spine J. 2008;17: 930935.Hours M, Khati I, Charnay P, et al.
One year after mild injury: comparison of health status and quality
of life between patients with whiplash versus other injuries.
J Rheumatol. 2014;42: 528538.Boyd R, Massey R, Duane L, et al.
Whiplash associated disorder in children attending the emergency department.
Emerg Med J. 2002;19:311313.Kasch H, Qerama E, Kongsted A, et al.
Clinical assessment of prognostic factors for long-term pain and handicap
after whiplash injury: a 1-year prospective study.
Eur J Neurol. 2008;15: 12221230.Vetti N, Krakenes J, Ask T, et al.
Follow-up MR imaging of the alar and transverse ligaments
after whiplash injury: a prospective controlled study.
AJNR Am J Neuroradiol. 2011;32: 18361841.Kongsted A, Sorensen JS, Andersen H, et al.
Are early MRI findings correlated with long-lasting symptoms following
whiplash injury? A prospective trial with 1-year follow-up.
Eur Spine J. 2008;17:9961005.Matsumoto M, Okada E, Ichihara D, et al.
Prospective ten-year follow-up study comparing patients with whiplash-associated
disorders and asymptomatic subjects using magnetic resonance imaging.
Spine. 2010;35:16841690.Johansson MP, Baann Liane MS, Bendix T, et al.
Does cervical kyphosis relate to symptoms following whiplash injury?
Manual Ther. 2011;16:378383.Norris SH, Watt I.
The prognosis of neck injuries resulting from rear-end vehicle collisions.
J Bone Joint Surg Br. 1983;65: 608611.Sterling M.
Differential development of sensory hypersensitivity and a measure
of spinal cord hyperexcitability following whiplash injury.
Pain. 2010;150:501506.Kasch H, Stengaard-Pedersen K, Arendt-Nielsen L, et al.
Pain thresholds and tenderness in neck and head following
acute whiplash injury: a prospective study.
Cephalalgia. 2001;21: 189197.Sterling M, Elliott JM, Cabot PJ.
The course of serum inflammatory biomarkers following whiplash injury
and their relationship to sensory and muscle measures:
a longitudinal cohort study.
PLoS One. 2013;8:e77903.Kongsted A, Jorgensen LV, Leboeuf-Yde C, et al.
Are altered smooth pursuit eye movements related to chronic pain and disability
following whiplash injuries? A prospective trial with oneyear follow-up.
Clin Rehabil. 2008;22:469479.Kamper SJ, Maher CG, Menezes Costa Lda C, et al.
Does fear of movement mediate the relationship between pain intensity
and disability in patients following whiplash injury?
A prospective longitudinal study.
Pain. 2012;153:113119.Bostick GP, Carroll LJ, Brown CA, et al.
Predictive capacity of pain beliefs and catastrophizing
in whiplash associated disorder.
Injury. 2013;44:14651471.Soderlund A, Lindberg P.
Coping as a mediating factor between self-efficacy and
disability in whiplash associated disorders (WAD).
J Whiplash Related Disord. 2002;1:2537.Carroll LJ, Cassidy JD, Cote P.
The role of pain coping strategies in prognosis after whiplash injury:
passive coping predicts slowed recovery.
Pain. 2006;124:1826.Ozegovic D, Carroll LJ, Cassidy JD.
Does expecting mean achieving? The association between expecting to return
to work and recovery in whiplash associated disorders:
a population-based prospective cohort study.
Eur Spine J. 2009;18:893899.Holm LW, Carroll LJ, Cassidy JD, et al.
Expectations for recovery important in the prognosis of whiplash injuries.
PLoS Med. 2008;5:e105.Carroll LJ, Ferrari R, Cassidy JD, et al.
Coping and recovery in whiplash-associated disorders. Early use of passive
coping strategies is associated with slower recovery of
neck pain and painrelated disability.
Clin J Pain. 2014;30:18.Myrtveit SM, Carstensen T, Kasch H, et al.
Initial healthcare and coping preferences are associated with outcome
1 year after whiplash trauma: a multicentre 1-year follow-up study.
BMJ Open. 2015;5:e007239.Cote P, Hogg-Johnson S, Cassidy JD, et al.
Initial patterns of clinical care and recovery from
whiplash injuries: a population-based cohort study.
Arch Intern Med. 2005;165:22572263.Cote P, Hogg-Johnson S, Cassidy JD, et al.
Early aggressive care and delayed recovery from whiplash:
isolated finding or reproducible result?
Arthritis Rheum. 2007;57:861868.Skillgate E, Cote P, Cassidy JD, et al.
Effect of early intensive care on recovery from whiplash-associated disorders:
results of a population-based cohort study.
Arch Phys Med Rehabil. 2016;97: 739746.Kasch H, Kongsted A, Qerama E, et al.
A new stratified risk assessment tool for whiplash injuries
developed from a prospective observational study.
BMJ Open. 2013;3:e002050.Sterling M, Jull G, Vicenzino B, et al.
Physical and psychological factors predict outcome following whiplash injury.
Pain. 2005; 114:141148.Buskila D, Neumann L, Vaisberg G, et al.
Increased rates of fibromyalgia following cervical spine injury.
A controlled study of 161 cases of traumatic injury.
Arthr Rheumat. 1997;40:446452.Tishler M, Levy O, Amit-Vazina M.
Can fibromyalgia be associated with whiplash injury?
A 3-year follow-up study.
Rheumatol Int. 2011;31:12091213.Tishler M, Levy O, Maslakov I, et al.
Neck injury and fibromyalgia- are they really associated?
J Rheumatol. 2006;33:11831185.Wynne-Jones G, Jones GT, Wiles NJ, et al.
Predicting new onset of widespread pain following a motor vehicle collision.
J Rheumatol. 2006;33:968974.Sale H, Isberg A.
Delayed temporomandibular joint pain and dysfunction induced
by whiplash trauma: a controlled prospective study.
J Am Dent Assoc. 2007;138:10841091.Sale H, Bryndahl F, Isberg A.
A 15-year follow-up of temporomandibular joint symptoms and
magnetic resonance imaging findings in whiplash patients:
a prospective, controlled study.
Oral Surg Oral Med Oral Pathol Oral Radiol Endodont. 2014;117: 522532.Phillips LA, Carroll LJ, Cassidy JD, et al.
Whiplash-associated disorders: who gets depressed?
Who stays depressed?.
Eur Spine J. 2010;19:945956.Ferrari R, Louw D.
Coping style as a predictor of compliance with referral
to active rehabilitation in whiplash patients.
Clin Rheumatol. 2011;30:12211225.Joud A, Stjerna J, Malmstrom EM, et al.
Healthcare consultation and sick leave before and after neck injury:
a cohort study with matched population-based references.
BMJ Open. 2013;3: e003172.Matsumoto M, Ichihara D, Okada E, et al.
Modic changes of the cervical spine in patients with whiplash injury:
a prospective 11-year follow-up study.
Injury. 2013;44:819824.Stovner L, Obelieniene D.
Whiplash headache is transitory worsening of a pre-existing primary headache.
Cephalalgia. 2008;28: 2831.Walton D.
A review of the definitions of recovery used in prognostic
studies on whiplash using an ICF framework.
Disability & Rehabilitation. 2009;31:943957.Carroll LJ, Lis A, Weiser S, et al.
How well do you expect to recover, and what does recovery mean anyway?
Qualitative study of expectations after a musculoskeletal injury.
Physical Therapy. 2016;96:797807.Walton DM, Macdermid JC, Taylor T.
What does recovery mean to people with neck pain?
Results of a descriptive thematic analysis.
TOORTHJ. 2013;7:420427.Sarrami P, Armstrong E, Naylor JM, et al.
Factors predicting outcome in whiplash injury:
a systematic meta-review of prognostic factors.
J Orthopaed Traumatol. 2017;18:916.Juni PH, Sterne J, Bartlett C, et al.
Direction and impact of language bias in meta-analyses
of controlled trials: empirical study.
Int J Epidemiol. 2002;31:115123.Moher DF, Jadad A, Klassen T, et al.
Completeness of reporting of trials published in languages other than English:
implications for conduct and reporting of systematic reviews.
Lancet. 1996; 347:363366.Moher D, Pham B, Lawson M, et al.
The inclusion of reports of randomised trials published
in languages other than English in systematic reviews.
Health Technol Assess. 2003;7:190.Morrison AP, Husereau D, Moulton K, et al.
The effect of English-language restriction on systematic review-based
meta-analyses: a systematic review of empirical studies.
Int J Technol Assess Health Care. 2012;28:138144.Sutton AJ, Duval SJ, Tweedie RL, et al.
Empirical assessment of effect of publication bias on meta-analyses.
BMJ. 2000;320: 15741577.
Return to WHIPLASH
Return to CHRONIC NECK PAIN
Since 8-31-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |