

Do Chiropractors Identify with Complementary
and Alternative Medicine? Results of a SurveyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Altern Complement Med. 2008 (May); 14 (4): 361–368
Daniel Redwood, D.C., Cheryl Hawk, D.C., Ph.D., Jerrilyn Cambron, D.C., Ph.D., Sivarama Prasad Vinjamury, M.D. (Ayurveda), M.A.O.M., And Jennifer Bedard
Cleveland Chiropractic College-Kansas City,
Kansas City, MO 64131, USA.OBJECTIVE: To conduct a descriptive review of the scientific literature examining use rates of modalities and procedures used by CAM clinicians to manage chronic LBP and other conditions
DATA SOURCES: A literature of PubMed and MANTIS was performed using the key terms Chiropractic; Low Back Pain; Utilization Rate; Use Rate; Complementary and Alternative Medicine; and Health Services in various combinations.
DATA SELECTION: A total of 137 papers were selected, based upon including information about chiropractic utilization, CAM utilization and low back pain and other conditions.
DATA SYNTHESIS: Information was extracted from each paper addressing use of chiropractic and CAM, and is summarized in tabular form.
RESULTS: Thematic analysis of the paper topics indicated that there were 5 functional areas covered by the literature: back pain papers, general chiropractic papers, insurance-related papers, general CAM-related papers; and worker's compensation papers.
CONCLUSION: Studies looking at chiropractic utilization demonstrate that the rates vary, but generally fall into a range from around 6% to 12% of the population, most of whom seek chiropractic care for low back pain and not for organic disease or visceral dysfunction. CAM is itself used by people suffering from a variety of conditions, though it is often used not as a primary intervention, but rather as an additional form of care. CAM and chiropractic often offer lower costs for comparable results compared to conventional medicine.
From the Full-Text Article:
INTRODUCTION
Chiropractic in the United States exhibits characteristics of both mainstream health care and complementary and alternative medicine (CAM). Eisenberg et al.’s [1] classic 3-part definition states that CAM applies to health care methods that are not generally taught in medical schools, not generally available in hospitals, and not generally covered by health insurance. By this definition, chiropractic currently stands on the bridge between CAM and mainstream medicine (MM). [2] Chiropractic services are covered by most U.S. health insurance policies and are available in over 200 U.S. hospitals. [3] However, chiropractic procedures are not taught to medical students for use in their practices, although general presentations by chiropractors to medical students are common. [4]
Those outside the profession, including the National Center of Complementary and Alternative Medicine (NCCAM), tend to classify chiropractic as CAM. [5, 6] However, placement in this category is controversial among chiropractors. [5] A 1999 survey of a stratified random sample of U.S. chiropractors found that only 46% of respondents (confidence interval 0.42–0.50) felt that chiropractic should be termed “complementary.” [7] One chiropractor, in a strongly worded commentary in the Journal of the Canadian Chiropractic Association, even suggested a possible causal relationship between categorizing chiropractic within CAM and the decrease in chiropractic utilization rates noted in recent years. [5, 8]
Categorizing chiropractic as CAM or mainstream carries significant practical implications not only in terms of public perceptions of the profession but also with regard to the availability of specific revenue streams for chiropractic research. Because the NCCAM budget is now over $120 million, it has become a significant source of funds for chiropractic research projects. However, at least partly because NCCAM categorizes chiropractic under “manipulative and body-based therapies” rather than “whole medical systems,” chiropractic-related funding from this source tends to favor studies that focus on the effects of manual manipulation for relief of musculoskeletal pain.
Moreover, while in the past chiropractic researchers were able to compete (in some cases successfully) for grants from other instutes of the National Institutes of Health, such applications are now all referred to NCCAM, which thus has become the primary federal funding source for chiropractic research. A benign interpretation of these changes is that the process for securing funding for chiropractic research has been streamlined; another interpretation is that chiropractic research has been ghettoized.
A recent survey by Klimenko et al. [9] classified their practitioner samples as MM, integrative medicine (IM), and CAM. In that study, chiropractors were classified as CAM, along with acupuncturists, massage therapists, homeopaths, and hypnotherapists, and the responses of all these provider types were pooled. Topics addressed included practitioners’ definitions of health, disease, and healing, as well as factors that inhibit or enhance their ability to focus on the “whole person,” the preferred relationship between MM and CAM, ways to improve communication between MM and CAM providers, and concerns about integrating CAM and MM. The purpose of this project was to investigate the opinions of a sample of chiropractic faculty and practitioners on the appropriate classification of their profession, in terms of CAM versus mainstream, as well as on the definitions of health and healing described in the Klimenko et al. [9] survey
METHODS
Design
This was a descriptive study conducted by means of an electronically administered survey to a sample of chiropractic college faculty and field practitioners.
Sample population
The faculty sample consisted of all faculty members holding Doctor of Chiropractic (D.C.) degrees at 4 chiropractic colleges. Two (2) of the colleges are part of health science universities, both of which also have massage and acupuncture training programs. One of these institutions, National University of Health Sciences (NUHS), is in the Midwest (50 D.C. faculty) and the other, Southern California University of Health Sciences (SCUHS), in southern California (69 D.C. faculty). The other 2 are separate campuses of 1 chiropractic college system, Cleveland Chiropractic College (CCC), 1 in the Midwest with 42 D.C. faculty and 1 in southern California with 30 D.C. faculty. Thus there was fairly broad geographic representation in the sample. A total of 191 faculty members were sent invitations to participate in the survey.
The practitioner sample consisted of all 108 participants in a chiropractic practice-based research network (PBRN). These D.C.s, who had volunteered to participate in the PBRN, were located in 32 states in the United States, with the highest proportions in California (14%), Kansas (12%), Missouri (9%), and Pennsylvania (6%). They were recruited through letters sent to a random sample of CCC alumni as well as invitations sent to D.C.s who had participated in a large national chiropractic PBRN that had been shown to be representative of U.S. D.C.s. [10]
Survey instrument
We used the survey instrument with permission from its authors. [9] The survey had been developed to gather information about respondents’ concepts and definitions of health and disease, in order to compare the broad categories of practitioners — MM, IM, and CAM. The survey had been developed through an extensive qualitative process using interviews and focus groups of practitioners in New York City. [11] In this qualitative process, MM practitioners interviewed were physicians and nurses from a variety of specialties. IM practitioners interviewed were osteopaths and MM practitioners who also had CAM training. CAM practitioners in the following fields were interviewed: acupuncture, homeopathy, Ayurveda, Reiki, hypnotherapy, rolfing, shamanism, neurolinguistic programming, therapeutic touch, and massage therapy. Chiropractic was not mentioned as one of the fields included; however, chiropractic was specifically mentioned as being categorized as CAM/ [11]
We introduced the survey with a cover letter explaining the purpose and context of the survey, including this explanatory statement about the terms used in the survey:
Complementary and alternative medicine (CAM) has been defined in many ways, depending upon the context. In a recent survey of health care providers done in New York by Klimenko and colleagues, respondents were pre-classified by the authors as:
Complementary and alternative medicine (CAM),
main stream medicine (MM) or
integrated medicine (IM), as follows:MM: M.D.s, nurses, physician’s assistants, social workers, psychologists without CAM training
CAM: chiropractors, acupuncturists, massage therapists, homeopaths, naturopaths, hypnotherapists
IM: osteopaths and MM providers who also have CAM trainingIn order to know your opinion of how your profession should be classified, as well as your input on the models of health survey by Klimenko’s group, we would like to survey a sample of the providers termed “CAM” by the Klimenko group. We would also like to ask for your input on the most appropriate classification for your profession, given that the term is apparently in flux.
We added 3 additional questions to this survey in order to gather information about chiropractors’ opinions on the categories into which responses had been placed in the published results of the Klimenko survey.
These were:
Do you agree with the way these professions are categorized? (response categories: yes, no, or no opinion)
If “no,” please place any professions you feel are misplaced into the correct categories or describe other changes you think should be made (open-ended response, no limit)
Do you have any additional comments about these categories? (open-ended response, no limit)
Human subjects’ considerations
Before administering the survey, the project was approved by the Institutional Review Board of each of the participating institutions. All survey responses were completely anonymous; data were collected through an online survey system (Zoomerang) that protects users’ identities through confidential data collection. No names or e-mail addresses were collected by this system.
Survey administration
We obtained e-mail addresses for all D.C. faculty at the 4 targeted colleges. Each investigator e-mailed the cover letter (signed by all investigators) to his or her faculty members in order to personalize the communication. The PBRN office had the 108 practitioners’ e-mail addresses already on file, and the cover letter was e-mailed to them, signed by the investigators who were also the director and coordinator of the PBRN. The cover letter explained the survey process and provided the URL link to the survey. The survey was administered via the Zoomerang system. Reminders were sent out to the entire sample population twice, at 1-week intervals.
Data management and analysis
All data were downloaded from Zoomerang into Excel, and then exported to SPSS, version 14.0 (Chicago, IL) for computation of descriptive statistics. Chi-square analyses with significance testing (p 0.05) were used to assess differences between respondent groups (faculty and practitioners). Comparisons with the published results of the Klimenko study [*] were made graphically, with no significance testing.
RESULTS

Table 1

Table 2

Table 3

Table 4
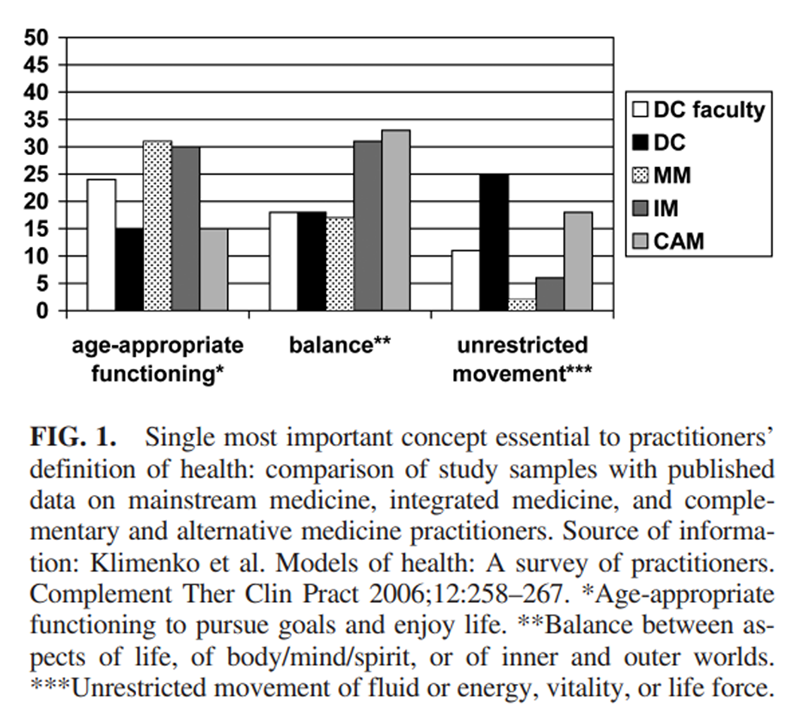
Figure 1
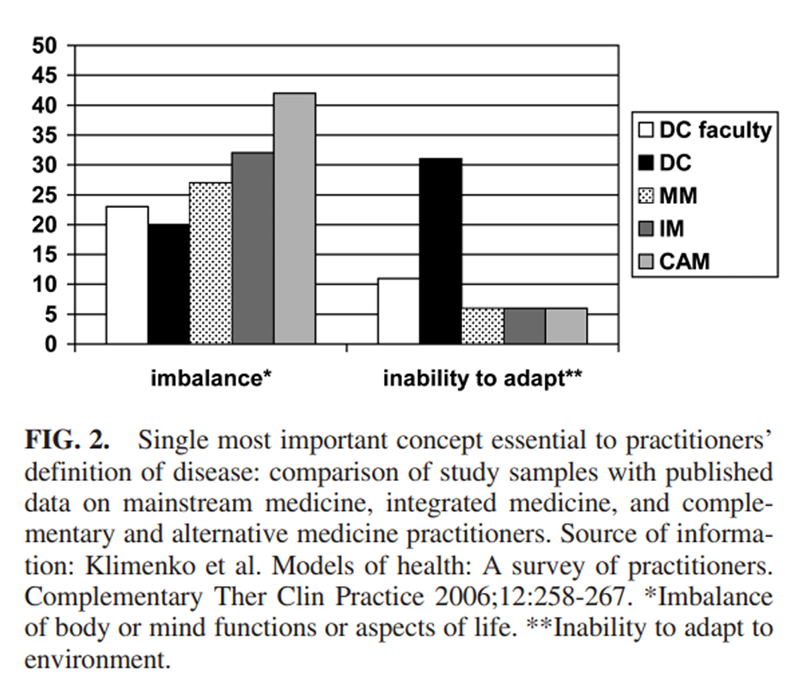
Figure 2

Figure 3

Figure 4

Figure 5 Sample population
Of 191 D.C. faculty invited to participate, 71 (37%) completed the survey. Of the 108 practicing D.C.s invited to participate, 61 (57%) completed the survey. Their characteristics are summarized in Table 1. Both samples were predominantly white, male, and had completed their professional training more than 20 years ago. A few (10% in each sample) had additional training in acupuncture or massage therapy.
Chiropractic and CAM
Of the total sample of 132, 31% agreed with the categorization of professions from the Klimenko study [9]; 3 respondents (all were in the practitioner sample) had no opinion. Although the difference between respondent groups was not statistically significant, 37% of faculty respondents and 25% of practitioner respondents agreed with categorizing chiropractic as CAM.
The 69% who did not consider chiropractic CAM expressed a variety of opinions on how the categories should be organized. As shown in Table 2, the largest group (27% of the total sample of 132) thought that chiropractors should be classified as IM rather than CAM. Twenty percent of practitioners and 6% of faculty felt that chiropractic should be categorized as MM. When the faculty were categorized by the institution where they were employed (SCUHS, CCC, or NUHS), there was a difference in the percent of responders who agreed with the proposed categorization of professions (47%, 39%, and 35% respectively), although it was not statistically significant.
Chiropractors’ opinions on health, disease, healing, and interprofessional relationships
Definition of health. As detailed in Table 3, faculty and practitioners in our sample differed in which concept they felt was most important to their definition of health. The concept the highest proportion of faculty (24%) felt was most important was age-appropriate functioning, which was also the most important concept to MM and IM practitioners in the Klimenko survey. [9] For D.C. practitioners, it was unrestricted movement of fluid or energy (25%), which was not selected by any group in the Klimenko survey as the most important concept. Overall, in our sample, 11% (14) indicated that none of the concepts was the most important, and 12 respondents wrote in additional concepts (see Table 3). The D.C. practitioners’ open-ended responses all focused on exclusively physiologic concepts.Definition of disease. For the most important concept in defining disease, the highest proportion of faculty in our sample (23%) and all 3 provider groups in the Klimenko survey [9] selected “imbalance of body or mind functions or aspects of life.” The highest proportion of our D.C. practitioner sample (32%) selected “inability to adapt to the environment,” although 20% selected the previous concept, imbalance of body or mind. In our sample, 9% (12) indicated that none of the concepts was most important; their responses are shown in Table 4. The D.C. practitioners’ open-ended responses, again, focused on physical or physiologic concepts.
Definition of healing. With respect to the most important concept in their definition of healing, “returning to normal activity/functioning” was selected by the highest proportion of respondents in both our samples and all the groups in the Klimenko survey. [9] Figures 1 through 5 compare the faculty and practitioner samples in this study with the MM, IM, and CAM samples in the Klimenko survey. [9]Each figure shows the single concept that was most commonly selected by each provider group. Overall, there was no clear pattern evident between our samples and MM, IM, or CAM or even between D.C. faculty and D.C. practitioners.
DISCUSSION
This was a small exploratory study designed to provide food for thought on assessing the validity of the assumption that chiropractors can accurately be aggregated into a general category of “CAM providers.” It has a number of limitations. First, the sample was small and the sampling method was non-random. However, these are somewhat offset by the facts that the sample included all D.C. faculty at 3 institutions and all the practitioners in a PBRN database, and the institutions were in 3 widely diverse geographic areas. In terms of the representativeness of the philosophical position of the respondents, NUHS and SCUHS are considered to be on the liberal end of the spectrum of chiropractic philosophy, and Cleveland is considered to be on the conservative side of the spectrum, although not at the extreme end. [12] Thus our sample may represent some bias toward a more liberal philosophy. Our response rate for faculty (37%) was similar to the average reported for electronically administered surveys (39.6%), [13] and that for practitioners was considerably higher (57%). The practitioners represented 32 states and a wide range of years in practice, although it is certainly possible that practitioners who volunteer to participate in research may differ from those who do not.
Another possible limitation is that the concepts represented in the survey instrument may not truly represent concepts held by different provider groups, especially because no formal testing of its content validity has been done. In fact, it appears, from our results, that in this time of constant change in the health care arena, concepts of health and disease may be in flux and may reflect more of an individual belief among providers rather than being held professionwide. This may be particularly true of chiropractors, whose profession is viewed by those both within it and outside it as being at a crossroads between mainstream and complementary health care.
When we seek to define the boundaries of MM, IM, and CAM, it is important to remember that over extended periods of time, individual healing arts arise, evolve, merge, and in some cases disappear down the corridors of history. Broader categories of healing arts also undergo such changes. The very nature of the health care mainstream, as well as its component parts, is constantly in flux. Historians are better at defining such trends in retrospect than are the participants in real time.
As an alternative healing art enters the mainstream, a kind of definitional vertigo may ensue, at least temporarily. Years ago, it was clear to both chiropractors and mainstream medical practitioners that the chiropractic profession was alternative, not mainstream. Over the past several decades, chiropractic has gradually acquired more mainstream characteristics, which is now causing the validity of this categorical identification to be called into question. Current mainstream characteristics of chiropractic include licensure throughout most of the Western world, an increasingly strong scientific research base, widespread insurance coverage, tens of millions of patients per year, a well-developed educational infrastructure, and inclusion in numerous multidisciplinary clinics and hospital staffs and on the health care teams serving the military, veterans, professional sports teams, and Olympic athletes. One can reasonably argue that at present chiropractic cannot be accurately characterized as either as CAM or mainstream, that it exhibits aspects of both, that it is a bridge between the two, and that its current transitional state constitutes our era’s first major test case of how a profession changes categories.
Although our sample was small and subject to the limitations described above, it is still worth noting that the majority (69%) of the chiropractors responding rejected being characterized as CAM practitioners. They differed on how they should be identified (27% see themselves as part of IM, 12% as MM, and perhaps most tellingly, 14% as “not CAM, but no alternative suggested”). The primary message of our study is that a substantial majority of at least this sampling of chiropractors is not comfortable with the CAM moniker.
Transition between categories is imbued with possibility and also with risk. Recognized membership in either the mainstream or the CAM categories carries measurable benefits. As noted earlier, if chiropractors were to lose access to NCCAM research funds as a result of opting out of CAM while not simultaneously gaining sufficient access to mainstream, non-0CAM funding sources, the consequences would be disastrous.
A personal experience of one of the authors (D.R.) is illustrative of the paradoxes that arise in mid-transition. He recalls that when he received an offer in the mid-1990s to write a chiropractic textbook as part of a CAM book series from a major health sciences publisher, the publisher overrode the series editor’s categorization scheme, forcefully asserting that chiropractic was part of mainstream health care, not CAM, and that the book should therefore be published as a stand-alone title rather than as part of the CAM series. To which the author responded, “I wish they would convince my local HMO [health maintenance organization; a common form of managed care insurance in the United States] that chiropractic is mainstream.” At the time, the major regional HMO in the author’s area denied chiropractic coverage because it was deemed not to be part of the health care mainstream. Being neither fish nor fowl can be costly.
Chiropractors are acutely aware of the perils of transition. When confronted with what is essentially a yes-or-no choice between being categorized as CAM or not, chiropractors in our sample tended to side against CAM affiliation. This may in fact be a trend that is on the rise, as a 1999 survey [7] of chiropractors found them divided approximately evenly on this issue. It appears that they may prefer to be part of categories labeled MM or IM, each of which implies a more mainstream status than does the CAM label. Summarizing our data on these somewhat confusing and overlapping categories, it seems fair to infer that chiropractors prefer to be defined as something more mainstream and less alternative.
Processes of self-definition are crucial exercises in any profession’s continuing evolution. The chiropractic profession exemplifies the difficulties of self-definition as evidenced by the various treatment approaches and philosophies within this profession. Even within this study, the percent of responders who agreed with the CAM label differed by as much as 20% based on the institution with which they were affiliated. But unless this self-definition is consistent within the chiropractic profession and is congruent with the way that other professions and the public define and categorize the group, an inherent contradiction or cognitive dissonance is created that must at some point be resolved, through either open conflict or more gentle methods of consensus and democratic process.
Perhaps the crucial question raised by our study is: Must chiropractors, or any group, make a “yes-or-no” choice? If so, why? No governmental body is demanding it. There is certainly no groundswell in the CAM community to eject chiropractors (who, after all, make up the largest cohort of CAM practitioners, as defined by NCCAM). Moreover, it would be a drastic over-statement to assert that MM is rolling out a rainbow-colored welcome mat for chiropractors. Certainly there are laudable signs of improvement in interprofessional relations and models of integration emerging, but in the grand scheme of things these still fall short of critical mass.
Comparing our data with that of the Klimenko survey, [9] we conclude that chiropractors reject being pigeonholed by those outside the profession, no matter how well meaning they may be. When asked to define the proper role for their discipline, chiropractors appear to endorse a trajectory of increasing inclusion in the health care mainstream and increasing distance from the outsider status implicit in CAM, while failing to achieve consensus as to which category or label accurately describes their current and future roles.
In times of great change, efforts to freeze-frame groups into descriptive categories are of limited value. Yet communication between and within groups often relies on such categories as an aid to understanding the health politics of a particular nation or time period. It is important to recognize the limits of language and sociologic analysis. We need to do the best we can within these limits and to make a sincere effort not to confuse the map with the territory.
References:
Eisenberg DM, Kessler RC, Foster C, Morlock FE, Calkins DR, Delbanco TL.
Unconventional Medicine in the United States:
Prevalence, Costs, and Patterns of Use
New England Journal of Medicine 1993 (Jan 28); 328 (4): 246–252Meeker W, Haldeman S.
Chiropractic: A Profession at the Crossroads
of Mainstream and Alternative Medicine
Annals of Internal Medicine 2002 (Feb 5); 136 (3): 216–227Haas M, Baird R, Colley F, Meeker W, Mootz R, Perillo M.
Proposal to establish an APHA section on chiropractic health care.
J Am Chiropractic Assoc 1996;33:41–47.Redwood D.
Presenting chiropractic to medical students.
J Manipulative Physiol Ther 2000;23:290–293.Morgan L.
Is chiropractic a CAM therapy or is it a separate profession?
J Can Chiropr Assoc 2005;49:133–136.Khalsa P, Pearson NJ.
Financial support for research training and career development in
complementary and alternative medicine from the
National Institutes of Health.
J Manipulative Physiol Ther 2007;30:483–490.Hawk C, Byrd L, Jansen R, Long C.
Use of complementary healthcare practices among chiropractors in the United States: A survey.
Altern Ther Health Med 1999;5:56–62.Tindle H, Davis RB, Phillips RS, Eisenberg DM.
Trends in use of complementary and alternative medicine by US adults: 1997–2002.
Altern Ther Health Med 2005;11:42–49.Klimenko E, Julliard K, Lu SH, Song H.
Models of health: A survey of practitioners.
Complement Ther Clin Pract 2006; 12:258–267.Hawk C, Long CR, Boulanger K, Morschhauser E, Fuhr A.
Chiropractic care for patients aged 55 years and older: Report from a practice-based research program.
J Am Geriatr Soc 2000;48:534–545.Julliard K, Klimenko E, Jacob MS.
Definitions of health among healthcare providers.
Nurs Sci Q 2006;19:265–271.Institute for Alternative Futures.
The Future of Chiropractic Revisited: 2005–2015
Alexandria, Virginia: The Institute for Alternative Futures; 2005.Cook C, Heath F, Thompson RL.
A meta-analysis of response rates in web- or internet-based surveys.
Educ Psychol Meas 2000;60:821–836.
Return to ALT-MED/CAM ABSTRACTS
Since 4-26-08


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |