Pancoast Tumor Presenting as Neck Pain
in the Chiropractic Office:
A Case Report and Literature ReviewThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: American J Case Reports 2022 (Jul 7); 23: e937052 ~ FULL TEXT
OPEN ACCESS Eric Chun-Pu Chu, Robert J Trager, John Sing Fai Shum, Colin Ritchie Lai
New Chiropractic and Physiotherapy Centre,
EC Healthcare,
Hong Kong, Hong Kong.
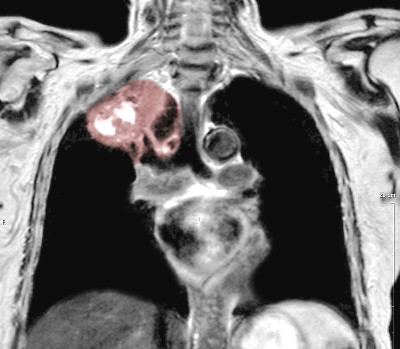
Pancoast Tumor Seen on MRIBACKGROUND Pancoast tumors, also called superior sulcus tumors, are a rare type of cancer affecting the lung apex. These tumors can spread to the brachial plexus and spine and present with symptoms that appear to be of musculoskeletal origin.
CASE REPORT A 59–year-old Asian man presented to a chiropractor in Hong Kong with a 1–month history of neck and shoulder pain and numbness that had been treated unsuccessfully with exercise, medications, and acupuncture. He had an active history of tuberculosis, which was currently treated with antibiotics, and a 50–pack-year history of smoking. Cervical magnetic resonance imaging (MRI) was performed urgently, revealing a small cervical disc herniation thought to correspond with radicular symptoms. However, as the patient did not respond to a brief trial of care, a thoracic MRI was urgently ordered, revealing a large superior sulcus tumor invading the upper to mid-thoracic spine. The patient was referred for medical care and received radiotherapy and chemotherapy with a positive outcome. A literature review identified 6 previously published cases in which a patient presented to a chiropractor with an undiagnosed Pancoast tumor. All patients had shoulder, spine, and/or upper extremity pain.
CONCLUSIONS Patients with a previously undiagnosed Pancoast tumor can present to chiropractors given that these tumors may invade the brachial plexus and spine, causing shoulder, spine, and/or upper extremity pain. Chiropractors should be aware of the clinical features and risk factors of Pancoast tumors to readily identify them and refer such patients for medical care.
Keywords: Chiropractic • Lung Neoplasms • Mycobacterium tuberculosis • Neck Pain • Pancoast Syndrome • Shoulder Pain
From the FULL TEXT Article:
Background
Pancoast tumors, also called superior sulcus tumors, are a rare type of lung cancer that invade the apical chest wall. [1] These tumors can be challenging to identify in practice and are often misdiagnosed, as their symptoms often resemble benign musculoskeletal conditions. [5] Pancoast tumors may invade the brachial plexus, sympathetic chain, and/or vertebral bodies, causing a constellation of symptoms termed Pancoast syndrome, which may include spinal, shoulder, and upper extremity pain and/or weakness, as well as Horner’s syndrome. [1, 3] The most common initial symptom of Pancoast tumors is shoulder pain. [1]
Chiropractors only rarely encounter patients with undiagnosed cancer, yet these patients are important to identify and refer for medical care. In a 2012 survey of chiropractors in the United States, respondents reported encountering a patient with undiagnosed cancer about once every 8 years on average. [4] In another United States survey from 2014, chiropractors reported seeing patients with a bone tumor or metastasis less than once per year. [5]
In the Hong Kong Special Administrative Region (HKSAR), the setting of the current case, it is unclear if chiropractors encounter a relatively higher or lower rate of cancer patients than in other countries. However, the incidence of tuberculosis in HKSAR is 10 times greater than that Western developed countries, with 0.6 of every 1000 persons developing tuberculosis per year. [6] Importantly, as illustrated in the current case, tuberculosis is a significant independent risk factor for lung cancer (hazard ratio of 1.6). [7]
Given the potential for chiropractors to rarely encounter patients with undiagnosed cancer, we present a case of Pancoast tumor invading the spine, which was first identified in a chiropractic office.
Case Report
Patient Information
A 59–year-old Asian man presented to a chiropractic clinic in HKSAR with a 1–month history of aching and numbness of his posterior neck and bilateral shoulders. He had an active 6–month history of tuberculosis, which caused an occasional productive cough, and was under medical treatment with a spectrum of antibiotics during this time (ie, isoniazid, rifampin, pyrazinamide, and ethambutol), as supervised by a specialty chest hospital with monthly follow-up visits and serial chest radiographs every 1–2 months.
The patient’s tuberculosis was first suspected 6 months prior after he developed a cough and underwent chest radiography. This was followed up by a Mantoux test, which was strongly positive. His previous providers also initially scheduled a flexible fiberoptic bronchoscopy, but later canceled it as his sputum culture was positive for Mycobacterium tuberculosis, and chest computed tomography (CT) findings were compatible with tuberculosis. At this point he began pharmacologic treatment for tuberculosis with directly observed therapy, which continued through presentation to the chiropractic office.
He described that the neck pain began secondary to episodes of coughing and had negatively impacted his sleep quality. The patient reported an 8 out of 10 pain severity on the numeric rating scale. He had a 50–pack-year history of smoking, was a social drinker, and worked as an interior decorator. The patient had a medical history of hereditary elliptocytosis, and at age 33 had a spontaneous pneumothorax. He denied having a history of cancer. His family history was significant for lung cancer (mother) and hereditary elliptocytosis (father). The patient endorsed occasional hoarseness but denied any bowel or bladder symptoms.

Figure 1 Previous treatment for his neck pain directed by his primary care provider included prescription pain medications (nonsteroidal anti-inflammatory drugs and acetaminophen) and rehabilitation exercises provided by a physical therapist. The patient also had received acupuncture for his neck pain. As no previous treatments provided the patient relief, he sought out chiropractic care (Figure 1).
The patient’s most recent chest radiograph report from 1 month prior reported patchy airspace opacities with a nodular appearance in the right upper lung zone, suggestive of pneumonia. Review of a report of his high-resolution computed tomography (CT) of the thorax from 6 months prior noted right apical fibrocalcific changes, mild bronchiectasis, tiny nodules up to 2 millimeters in both lungs, and shotty non-enlarged mediastinal and hilar lymph nodes. There was no mention of a suspicious lung mass or tumor in these reports.
Clinical Findings
On physical examination, the patient appeared physically fit. The chiropractor noted muscle hypertonicity of the paraspinal muscles from C5 to T2, rhomboids, and teres minors. Cervical range of motion was severely restricted in extension and right rotation and moderately restricted in all other planes. Maximal foraminal compression testing on each side exacerbated the patient’s shoulder pain and paresthesia. A motor examination revealed 4/5 strength (Medical Research Council Scale) of the right deltoid, with pain.
The chiropractor’s differential diagnosis chiefly included discogenic C6 radiculopathy given the patient’s neck and shoulder symptoms, deltoid weakness, and other examination findings. More serious pathology, including spinal tuberculosis, was also considered as a possibility. Considering the patient had severe pain, neurologic deficits, had failed previous conservative care, and had red flags including active tuberculosis, a family history of lung cancer, and history of smoking, the chiropractor ordered a cervical spine MRI on the day of the first visit, which was performed within the facilities’ imaging center on an urgent basis. A cervical spine MRI was ordered initially as the patient’s symptom distribution, sensory loss, and motor deficit suggested a mid- to lower cervical radiculopathy, involving the lateral regions of both shoulders and right deltoid weakness.

Figures
2–5The cervical spine MRI revealed no serious pathology but did identify a small cervical disc protrusion at C6–7, without corresponding central canal or neuroforaminal stenosis (Figure 2). This was considered to correlate with the patient’s suspected radicular symptoms. The patient consented to a trial of chiropractic care which began 2 days later, consisting of instrument assisted soft tissue manipulation, gentle spinal manipulative therapy via non-thrust joint mobilizations, and mechanical cervical flexion-distraction therapy. These therapies were applied daily for 4 consecutive days. Treatments were well-tolerated, and the patient reported that his pain severity initially reduced to a 4 out of 10 after treatments, but quickly returned to a severe level without lasting relief.
Given the patient’s lack of response to care as well as his other risk factors and red flags for serious pathology, the chiropractor conferred with the supervising chiropractic clinician and a decision was made to arrange for an urgent thoracic spine MRI. The thoracic spine MRI was completed 1 week after the patient’s initial presentation and revealed an abnormal mass in the medial right lung apex and superior mediastinum, which extended into the right paraspinal region and infiltrated the upper to mid-thoracic vertebrae (Figures 3–5). The radiologist noted the possibility of a Pancoast tumor and recommended further evaluation.
The chiropractor immediately referred the patient back to the chest hospital for further testing, which confirmed the diagnosis of a Pancoast tumor. The patient’s case was evaluated and managed by several specialists, including oncology and orthopedic spine surgery. CT-guided fine-needle aspiration was performed, revealing a histopathologic diagnosis of adenocarcinoma. The patient underwent follow-up CT of the thorax with contrast, which revealed areas of vertebral necrosis from T1 to T6. He also underwent full-spine MRI with gadolinium contrast, which additionally revealed an enhancing right epidural extension seen at the T2/3 to T5/6 disc levels causing cord compression and displacing the spinal cord to the left. Erosion and destruction of the corresponding head and contiguous part of right 3rd–5th ribs was also noted.
The spine surgery team deemed the patient to be ineligible for spine surgery due to the extent of the tumor invasion and necrotic involvement of multiple vertebral levels. The patient was initially treated with oral dexamethasone 4 mg qid and radiotherapy, then received ongoing chemotherapy under the care of an oncologist. After starting chemotherapy and radiotherapy, at 2 months’ follow-up the patient noted he currently felt lighter and had less severe neck and shoulder pain and numbness. He noted he could sleep longer but still had severe pain upon waking for 2–3 hours, which subsided through the day. Written informed consent was obtained from the patient to publish this case report and any accompanying images.
Discussion
In this case, the patient’s cervical disc herniation was likely not the cause of symptoms as it was small and not causing nerve compression. If the C6–7 disc had caused nerve compression, this would have more likely presented as a C7 radiculopathy with further distal symptoms. [8] While annular fissures can cause discogenic pain, these are frequently asymptomatic. [9] While neck pain was briefly reduced, it is possible this was due to a generalized hypoalgesic effect of spinal manipulation. [10] Conversely, the patient’s symptoms were improved with lasting effects via radiotherapy and chemotherapy, suggesting that the Pancoast tumor was responsible for his symptoms.
More specifically, the patient’s symptoms were likely caused by tumor invasion of the brachial plexus (ie, Pancoast syndrome). This is a common phenomenon in Pancoast tumors, which often involves the middle and inferior trunks of the brachial plexus. [11] In the current case, the middle trunk was potentially involved, as this gives rise to the axillary nerve and axillary superior lateral cutaneous nerve, and could account for both the patient’s deltoid weakness and shoulder numbness, respectively.
Pancoast tumors may be suspected via their risk factors, such as smoking, male sex, age in the 6th decade, clinical features of Pancoast syndrome, and imaging findings. [11] Radiographic series, in particular the anteroposterior lordotic view, may be a first step in evaluating for a Pancoast tumor. [11] However, these lesions can be missed by chest X-rays. [1] Chest CT can be used to confirm the presence of an apical mass, while MRI may be used to characterize any brachial plexus or spinal involvement. [1] As in the current case, when neck, shoulder, and/or upper extremity symptoms and examination findings are not explained by cervical spine MRI, thoracic and/or brachial plexus MRI could be considered as next steps.

Table 1 A literature search using the search terms “chiropractic,” “chiropractor,” “superior sulcus,” and “Pancoast” was conducted via PubMed, Google Scholar, and the Index to Chiropractic Literature on April 18, 2022, to identify other cases in which patients with an undiagnosed Pancoast tumor presented to a chiropractor. In addition, review articles on the topic of chiropractic case reports [12] and chiropractic care and cancer [13, 14] were hand-searched for relevant cases. This search identified 6 articles [15–20], each describing a single patient with an undiagnosed Pancoast tumor who presented to a chiropractor. The clinical features of each previous case, including the current case (in total 7), were summarized (Table 1).
Among the previously published cases and current case, patients were predominantly male (6 of 7 cases), with a mean age of 53 (SD)±8 years. This limited sample is concordant with the epidemiologic features of Pancoast tumors, which have a male predominance and most often present in the 6th decade of life. [11] Multiple patients had a risk factor or red flag for lung cancer, which was commonly smoking (5 of 7 cases), while in the current case both smoking and tuberculosis were risk factors. In 5 cases [15, 17, 19, 20], including the current case, the chiropractor identified the Pancoast tumor or referred the patient for medical evaluation, while in 2 cases the chiropractor did not identify or suspect the Pancoast tumor. [16, 18]
An important finding noted among these cases of Pancoast tumor presenting to chiropractors is that each patient presented with shoulder, spine, or upper extremity symptoms. While these are common symptoms of Pancoast tumors [1, 11], they are also frequent concerns that prompt patients to seek chiropractic care in general. [21] It is thus possible that patients seek chiropractic care because they believe the symptoms to be benign and of a musculoskeletal origin.
The role of chiropractors involves not only treatment but examination, diagnosis, and case management. Importantly, chiropractors must conduct a thorough history and examination to assess for serious pathology. This helps guide the treatment and determine whether to administer high-velocity, low-amplitude spinal manipulation, which is contraindicated in the case of spinal malignancy. [22] In the current case, gentle manual therapy techniques were used as a precaution until there was more diagnostic information given the patient’s extensive red flags.
Limitations
First, as a single case, the course of care may not be broadly generalizable, especially to countries with a low incidence of tuberculosis or different chiropractic practice characteristics. While chiropractors have the authority to order MRI in HKSAR and the United States [23, 24], they may not be able to in other countries, given the scope of practice. Diagnostic imaging may be more commonly used by HKSAR chiropractors, with 36% using MRI at least sometimes [24], compared to 1% of chiropractors in other countries [21], which could have affected the diagnostic pathway in the current case. Alternatively, chiropractors who do not have MRI readily available may refer patients suspected of having Pancoast tumor to other medical specialists for further evaluation.
Second, our conclusion that the patient’s brachial plexus was involved was based on the available clinical and radiologic evidence, whereas electrodiagnostic testing and brachial plexus MRI could have made the exact neuroanatomical site(s) of involvement of the tumor clearer.
Third, it is unclear if the patient’s Pancoast tumor was simply missed in his previous chest imaging or was not readily visible, as images were unavailable from his chest hospital upon request and only imaging reports could be obtained. Likewise, exact details regarding the patient’s chemotherapy, radiotherapy, and post-treatment imaging were unavailable.
Fourth, the chiropractic clinician may have accelerated the diagnosis of Pancoast tumor by ordering thoracic MRI in addition to cervical MRI on the initial day of consultation, but the patient’s clinical features guided the clinician’s working diagnosis toward a cervical radiculopathy. While cost and scanning time of MRI may be general factors to consider, a more comprehensive, multi-region imaging strategy could be useful in patients at risk for lung cancer. [25]
Conclusions
Chiropractors should be aware that patients may present to their office with shoulder, spine, or upper extremity pain caused by a previously undiagnosed Pancoast tumor, as its symptoms often resemble those of common musculoskeletal conditions. Typical risk factors for Pancoast tumor are illustrated in the current case, including male sex and smoking, while tuberculosis is another important risk factor in regions where it is endemic. Chiropractors should refer patients suspected of having Pancoast tumor in a timely manner for appropriate medical care.
Department and Institution Where Work Was Done
New Chiropractic and Physiotherapy Centre, EC Healthcare, Hong Kong.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
Marulli G, Battistella L, Mammana M, et al.
Superior sulcus tumors (Pancoast tumors).
Ann Transl Med. 2016;4:239Deng P, Luo Y, Hu C, Zhou L.
[Misdiagnosis of pancoast cancer: Analysis of 26 cases.]
Zhonghua Jie He He Hu Xi Za Zhi. 2011;34:663-65 [in Chinese]Arcasoy SM, Jett JR.
Superior pulmonary sulcus tumors and Pancoast’s syndrome.
N Engl J Med. 1997;337:1370-76Daniel DM, Ndetan H, Rupert RL, Martinez D.
Self-reported recognition of undiagnosed life threatening conditions in chiropractic practice: A random survey.
Chiropr Man Ther. Springer; 2012;20:1-6Himelfarb I, Hyland J, Ouzts N, et al.
National Board of Chiropractic Examiners:
Practice Analysis of Chiropractic 2020
Greeley, CO:Tuberculosis and Chest Service Department of Health –
Is TB a common disease? [Internet].
[cited 2022 Apr 19]. Available from:
https://www.info.gov.hk/tb_chest/en/contents/c122.htmWu C-Y, Hu H-Y, Pu C-Y, et al.
Pulmonary tuberculosis increases the risk of lung cancer: a population-based cohort study.
Cancer. 2011;117:618-24Iyer S, Kim HJ.
Cervical radiculopathy.
Curr Rev Musculoskelet Med. 2016;9:272-80Ernst CW, Stadnik TW, Peeters E, et al.
Prevalence of annular tears and disc herniations on MR images of the cervical spine in symptom free volunteers.
Eur J Radiol. 2005;55:409-14Gevers-Montoro C, Provencher B, Descarreaux M, et al.
Neurophysiological Mechanisms of Chiropractic
Spinal Manipulation for Spine Pain
European Journal of Pain 2021 (Aug); 25 (7): 1429–1448Panagopoulos N, Leivaditis V, Koletsis E, et al.
Pancoast tumors: Characteristics and preoperative assessment.
J Thorac Dis. 2014;6:S108Trager RJ, Dusek JA.
Chiropractic case reports: A review and bibliometric analysis.
Chiropr Man Ther. 2021;29:17Alcantara J, Alcantara JD, Alcantara J.
The Chiropractic Care of Patients with Cancer:
A Systematic Review of the Literature
Integrative Cancer Therapies 2012 (Dec); 11 (4): 304–312Laoudikou MT, McCarthy PW.
Patients with Cancer.
Is There a Role for Chiropractic?
J Can Chiropr Assoc. 2020 (Apr); 64 (1): 32-42Berntheizel E, Fischer C, Tollefson L, Stefanowicz E.
Pancoast tumor resulting in cervicobrachial neuralgia.
Association of Chiropractic Colleges Research Agenda Conference 2021
Abstracts of Proceedings. J Chiropr Educ. 2021;21:81Deltoff MN, Wyatt LH.
Superior pulmonary sulcus tumor.
J Can Chiropr Assoc. 1985;29:203-4Downs SE.
Bronchogenic carcinoma presenting as neuromusculoskeletal pain.
J Manipulative Physiol Ther. 1990;13:221-24Kim P, Hains F, Wallace MC, Mior SA.
Pancoast tumour: A case report.
J Can Chiropr Assoc. 1993;37:214-20Patel S, Ilsen PF.
Acquired Horner’s syndrome: Clinical review.
Optometry. 2003;74:245-56Weiner S, Gardiner L.
Pancoast tumor mimicking musculoskeletal pain: A case study.
J Neuromusculoskel Syst. 2001;9:16-20Beliveau PJH, Wong JJ, Sutton DA, Simon NB, Bussieres AE, Mior SA, et al.
The Chiropractic Profession: A Scoping Review of Utilization Rates,
Reasons for Seeking Care, Patient Profiles, and Care Provided
Chiropractic & Manual Therapies 2017 (Nov 22); 25: 35World Health Organization (WHO)
WHO Guidelines on Basic Training and Safety in Chiropractic
Geneva, Switzerland: (November 2005)Chang M.
The Chiropractic Scope of Practice in the United States:
A Cross-sectional Survey
J Manipulative Physiol Ther. 2014 (Jul); 37 (6): 363–376Leung KY, Chu E.
Hong Kong chiropractic survey: Analysis of data.
Asia-Pac Chiropr J. 2021;2:3Wang Y-XJ, Lo GG, Yuan J, et al.
Magnetic resonance imaging for lung cancer screen.
J Thorac Dis. 2014;6:1340-48
Return to CASE STUDIES
Since 12-11-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |