Adverse Events From Spinal Manipulations in
the Pregnant and Postpartum Periods:
A Systematic Review and UpdateThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Can Chiropr Assoc 2021 (Apr); 65 (1): 32–49 ~ FULL TEXT
OPEN ACCESS Carol Ann Weis • Kent Stuber • Kent Murnaghan • Shari Wynd
Canadian Memorial Chiropractic College.

Background: The purpose of this study is to update a previous critical review of adverse events in pregnant and postpartum populations.
Methods: The following databases were searched: PubMed, CINAHL, Index to Chiropractic Literature, Cochrane Database of Systematic Reviews/Cochrane Central Register of Controlled Trials and MEDLINE. We included all study design types as it was determined a priori that there would not be enough high-quality research on spinal manipulative therapy (SMT) in these populations to make any determinations. The Scottish Intercollegiate Guidelines Network (SIGN) and CARE (CAse REport) checklists were used for quality rating.
Results: This update found one case study that demonstrated a serious adverse event in the cervical spine following SMT and a handful of minor and transient adverse events in the low back following SMT.
Conclusions: There was limited evidence of adverse events following SMT in these populations. Although we are calling for improved reporting of such events in future studies, it may be that such injuries are rare.
Keywords: adverse events; chiropractic; manual therapy; postpartum; pregnancy; spinal manipulative therapy.
From the Full-Text Article:
Introduction
Musculoskeletal pain is a frequent complaint during pregnancy and the postpartum period. Low back pain (LBP), pelvic girdle pain (PGP), carpal tunnel syndrome, and mid-back pain are common complaints in these groups, with LBP being the most common complaint among pregnant women. The prevalence of low back pain during pregnancy has been reported as up to 90% of pregnant women [1-6] and may continue into the postpartum period with up to 75% of women reporting symptoms six months following birth [7-12] and approximately 8–20% still suffering from pregnancy-related pain two to three years after giving birth. [13] Both pregnant and postpartum women have described the back pain as moderate, severe or disabling [1, 7] and interfering with life in general; interrupting activities of daily living, sleep and child rearing. [1, 8, 13, 14]
Unfortunately, many primary health care providers consider pregnancy-related back pain to be a normal and unavoidable occurrence [15-17] and patients often receive little or no treatment suggestions to manage their condition. [18, 19] The etiology of pregnancy-related back pain is unknown. [17, 20] It has been suggested that causation is multifactorial and some of the proposed mechanisms include, but are not limited to, maternal weight gain, biomechanical changes due to pregnancy [17, 21], changes in abdominal musculature to accommodate the growing fetus [22-24] and/ or increased circulating relaxin [25] producing ligamentous laxity. [26]
In general, women are more susceptible to increases in joint laxity than men. [27, 28] It has been suggested that hormonal changes may be responsible for these differences. [29-31] By the twelfth week of pregnancy production of the hormone relaxin is increased and “relaxes” the joints and ligaments for labour and delivery of the baby through the vaginal canal. [32, 33] This change in hormonal milieu does not dissipate upon delivery and it is suggested that women immediately postpartum may continue to experience hormone-mediated ligament laxity. It is important to note that this increase in ligament laxity is not targeted just at the pelvis [34] thereby making these women more susceptible to various musculoskeletal injuries during this time.
Low back pain (LBP) [35], neck pain [36-38] and headaches [39] are significant causes of pain and disability in the non-pregnant population. Approximately 80% of the population experience at least one episode of LBP in their lifetime [35], 30–50% experience neck pain in a given year [40] and approximately 50% of people will experience a headache within the last year. [41]
One effective treatment option for patients experiencing any of these pains includes spinal manipulative therapy (SMT) [42-47]; whereby a localized force of high velocity and low amplitude (HVLA) is applied in the direction of the spinal segment. In the non-pregnant population, severe adverse events following SMT are rare [48-53] with most events being reported in lower level of evidence studies such as case reports or case series. [54, 55] It is noteworthy that there are published case reports describing vertebral artery dissection and stroke following manipulation in the non-pregnant population. [52]
However, most cases of extracranial vertebral artery dissections are thought to occur spontaneously in individuals with other risk factors such as connective tissue disorders, migraine, hypertension or vessel abnormalities. [52] At this time, the current evidence does not find excess risk for vertebral artery dissection from individuals seeking care from chiropractors compared to primary care. [52, 56]
Effective treatment options for pregnancy or postpartum related-back pain are not well known. [57-59] There are few well designed randomized controlled trials [60-62] (RCTs) investigating chiropractic care on pregnancy and postpartum-related spine pain, with most of the current evidence for this population being case studies. Although chiropractors report seeing pregnant and postpartum patients regularly [59, 63], the lack of evidence for these two populations is surprising given the impact pain can have on a woman’s life during these time periods. Similarly, there is little information regarding the safety of treatment options, such as SMT, in these populations. Given the coagulability status [64, 65] of these women and the plethora of hormonal and biomechanical changes that occur as a result of pregnancy and into the postpartum period, it is possible that some treatment options, such as SMT, may be contraindicated in these populations.
Our 2012 critical review of the literature identified four case reports [50, 51, 66, 67] and one prospective observational cohort study [68] reporting adverse events in seven individuals (five pregnant and two postpartum) following SMT. [69] Events ranged from minor pain following treatment, to fracture, stroke and epidural hematoma. This is an update of that previous paper and our aim is to systematically review the literature for any reported cases of iatrogenic injuries following SMT and other manual treatments.
Methods
Similar to our first review69, in this updated review we determined a priori that limiting our review to systematic reviews (SR) and RCTs would exclude valuable information regarding adverse events, so cohort and case reports were included. The review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews (PRISMA) and was registered with PROSPERO (no. CRD42019048918).
Literature search parameters
A literature search strategy (Appendix 1) was developed in collaboration with a health sciences librarian (KM). The following items were considered in developing the strategy:
Participants/Population
Women who were either pregnant or postpartum (up to 6 weeks after birth) with spine and/or pelvic girdle musculoskeletal complaints.
Intervention
The interventions examined included spinal SMT and any other manual therapies performed by chiropractors, osteopaths and physiotherapists; as the latter two can deliver similar treatment plans to pregnant women, these terms were also included. [57, 58, 70]
Comparators
There were no restrictions for the comparison group which may include: active treatments (such as exercise), placebos/shams, usual obstetric care (UOBC) or no treatments.
Outcomes
The presence of adverse events/iatrogenic injuries.
Search strategy
The following databases were used in the search strategy: PubMed, CINAHL, Index to Chiropractic Literature, Cochrane Database of Systematic Reviews/Cochrane Central Register of Controlled Trials and MEDLINE. Search terms consisted of subject headings specific to each database (i.e. MeSH in MEDLINE) and free text words relevant to pregnancy, postpartum, low back pain, pelvic girdle pain, chiropractic, etc. Publications in the search were restricted to the English language and from the date of our last review (October 2011) until November 2018. An additional search strategy was employed when reviewing systematic reviews (SR). Similar to Hawk et al. [71] and others [46], two investigators (CAW and SW) searched each included SR for eligible studies not identified through the formal search. Any that were deemed potentially acceptable were added to the list of studies to be analyzed.
Screening
Titles were screened independently by two reviewers (SW and CAW). Disagreements on eligibility were resolved by discussion. The same two investigators reviewed the abstracts and articles. If there was disagreement between the reviewers, a third investigator also reviewed (KS) either the abstract or full-text article and the majority rating was used following a group discussion. Studies of unacceptable quality were excluded from the evidence tables.
Eligibility criteria
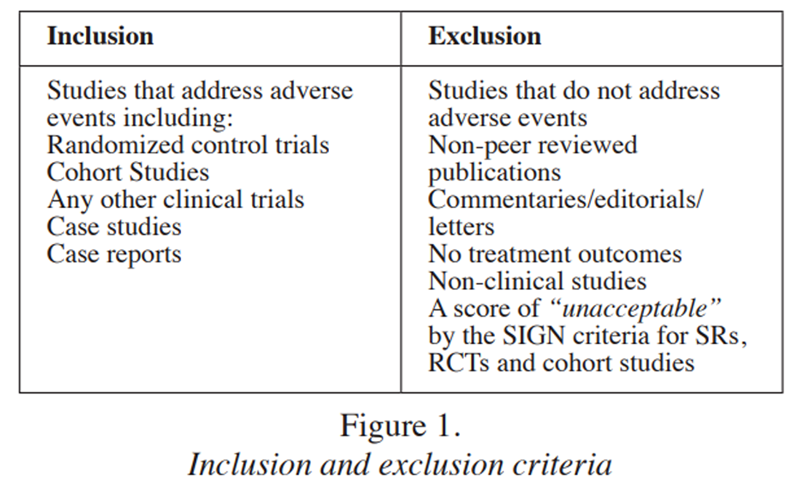
Figure 1
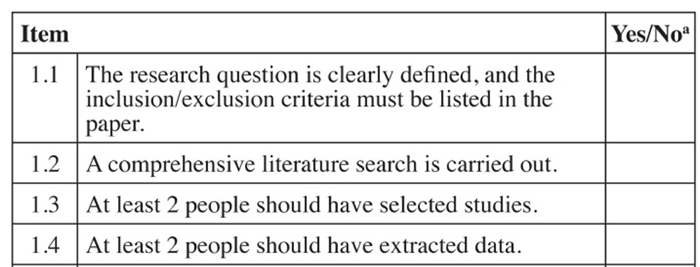
Figure 2
Figure 3
Figure 4
Figure 5 The eligibility criteria for articles in the search can be found in Figure 1.
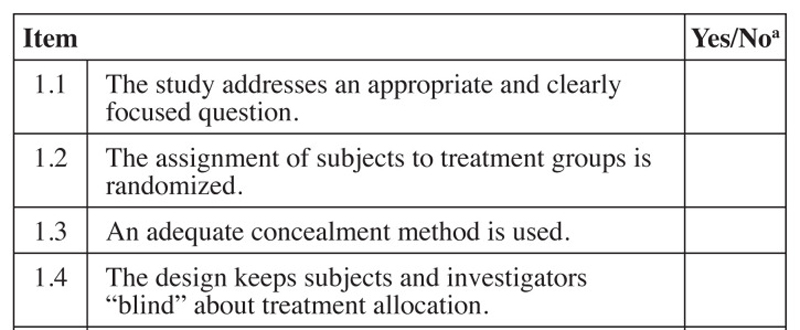
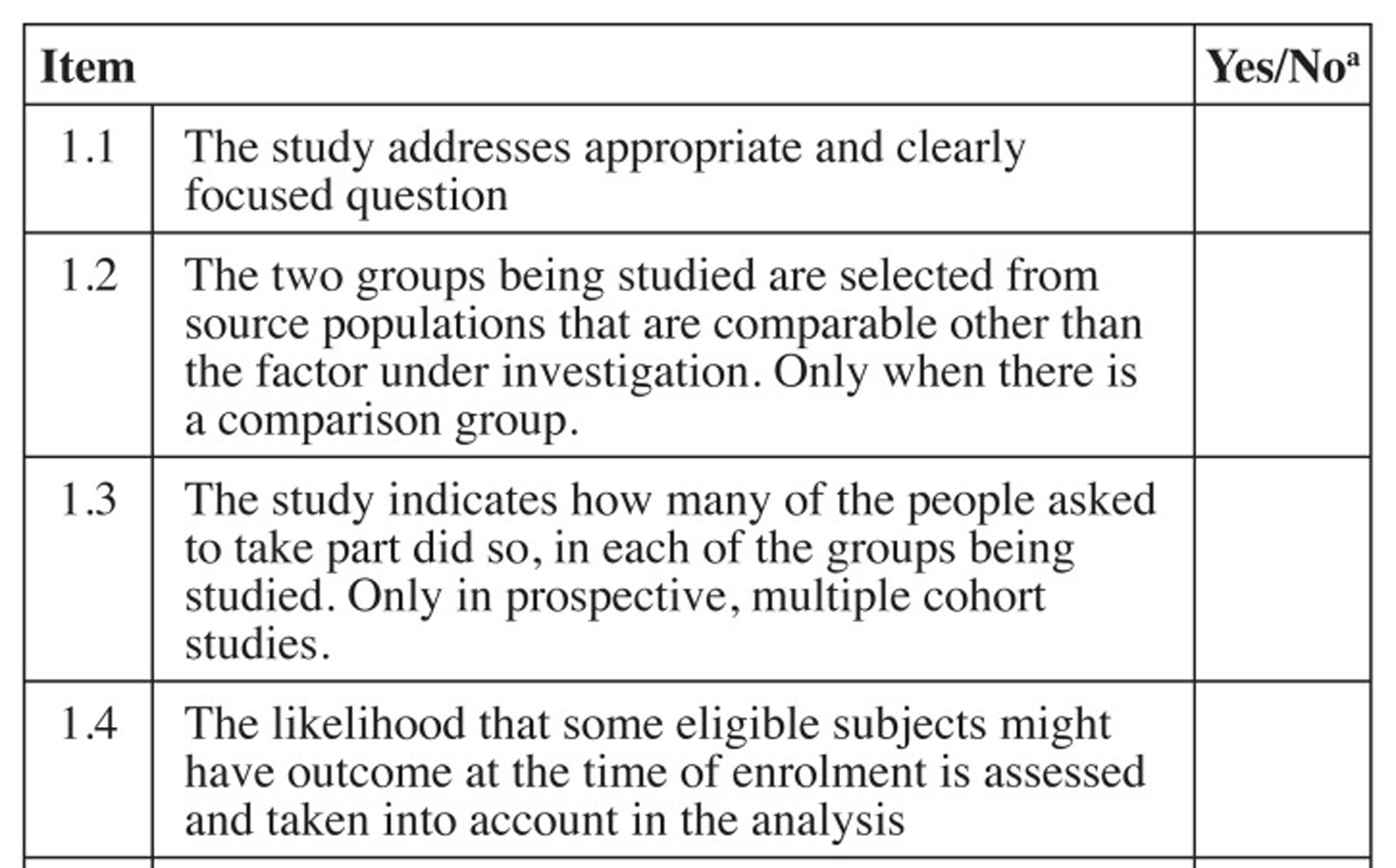
As previously performed by Hawk et al. [71] and others [57, 58] the Scottish Intercollegiate Guideline Network (SIGN) checklists were used to evaluate systematic reviews/meta-analyses [72] (both abbreviated as “SR”) and cohort studies [73] and a modified SIGN checklist was used to review RCTs. [71, 74] The modified SIGN RCT checklist combined information from the original checklist about concealment and blinding of the investigators, and it added three other items including patient blinding, sample size justification and if the required sample same size was reached (items 3, 4, 5 and 9). Unlike the original SIGN RCT checklist [74], the modified one did not take into consideration dropouts or compare results from different sites. [71] Two of the original The SIGN checklists score each article as “high quality, low risk of bias”, “acceptable quality, moderate risk of bias”, “low quality, high risk of bias” or “unacceptable” quality. Any studies that were scored as “unacceptable” quality were removed from further analysis. Each level was defined by scoring the checklists and assigning a value of “1” for each “yes” response. Figures 2, 3 and 4 list the items in each checklist and explain the scoring system used to determine quality rating.
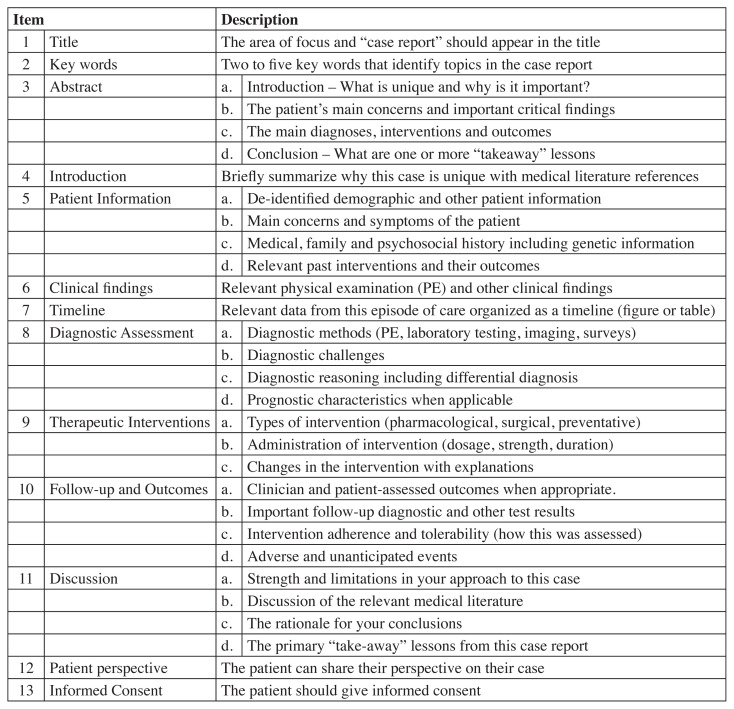
For case reports, the CARE (CAse REport) checklist for case reports was employed. [75] The CARE checklist evaluates 13 main areas over 30 specific items (Figure 5). Although there is no scoring system for this checklist, we decided a priori that each item would be worth “1” and a high score would indicate a more robust case report. A consensus-based decision between reviewers on whether the internal validity of the case reports was acceptable for inclusion in the current review.
Two investigators (CAW and SW) evaluated each article. If there was a disagreement between the two reviewers, a third investigator (KS) was asked to review. The majority rating was used after discussion among reviewers.
Data extraction
Variables for data extraction was determined a priori and completed by two investigators (CAW and SW) and the third author (KS) verified all of the data presented in the tables. All information extracted was entered into a Microsoft Word table.
Systematic Reviews (SRs)
Information extracted from SRs included: citation (first author and year of publication) and quality assessment, type of treatment/intervention, number of studies included, number of participants and type of studies included, results of that assessment and overall conclusions of the review.
Randomized Controlled Trials (RCTs)
Information extracted from RCTs included: study identification by citation (first author and year of publication) and quality assessment, patient population information, mean age and mean symptom duration, treatment/intervention, comparison group, dosage, adverse events reported and overall study conclusions.
Cohort studies
Information extracted from cohort studies included: study identification by citation (first author and year of publication) and quality assessment, patient population information, mean age and mean symptom duration, intervention, dosage, adverse events reported and overall study conclusions.
Case reports
Data extracted from the case reports included: study identification by citation (first author and year of publication), case presentation, treatment, and adverse events reported.
Results
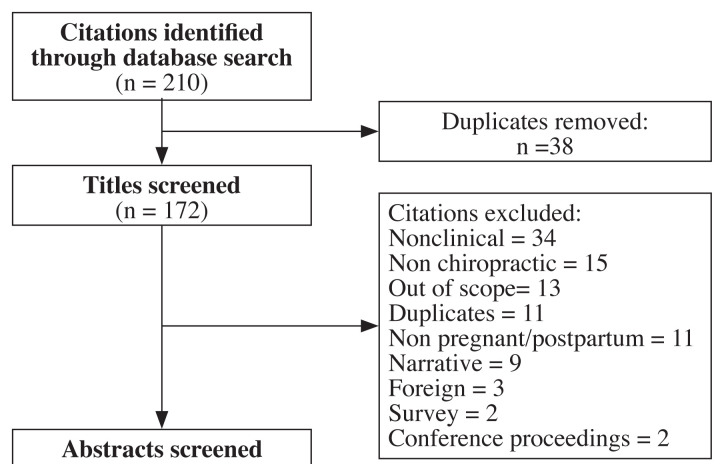
Figure 6 The initial database searches yielded 210 manuscripts (172 after duplicates removed). Of these, 21 were included in the review (8 SRs, 7 RCTs, 5 cohort, and 1 case study); see Figure 6 for the study flow diagram. Reasons for exclusion included: adverse events not reported, outside of the scope of the review, commentary/letter/ narrative review, no outcomes reported, not a clinical study, non-chiropractic, abstract/conference proceeding, non-English, and not reported in a peer-reviewed journal. Excluded studies are listed in Appendix 2.
Systematic reviews

Table 1 Table 1 lists each item on the Risk of Bias assessment instrument of included SRs. Of the eight SRs included, four were of “high quality” [18, 76–78], two were of “acceptable quality” [70, 79], and two were of “unacceptable quality” [80, 81] and removed from analysis. Overall, only a qualitative analysis could be completed because of the lack of homogeneity between the trials (specifically regarding SMT) and limited methodological quality, as well as variation between individual studies (i.e., gestational age, number of participants, types of intervention, duration and frequency of intervention, outcome measures, and condition diagnosis).

Table 2 Table 2 summarizes the included SRs. One of the SRs examined a variety of treatment options [75] for the pregnant patient experiencing back pain, two examined osteopathic manipulative therapy (OMT) [77, 78], one assessed complementary and alternative medicine (CAM) [18] as a treatment option, one examined modalities [70] and the final SR looked at physical therapy [79] in general. The four “high quality” SRs recorded adverse events of which almost all were considered transient and minor. [18, 76–78] In addition, one of the SRs stated that there were no issues related to any of the deliveries or neonates [76] and another suggested that CAM, such as chiropractic, was a safe option compared to no treatment at all for pregnancy-related back pain. [18] The two “acceptable quality” SRs [70, 79] did not record specific adverse events for any intervention they examined.
Randomized controlled trials

Table 3

Table 4 Table 3 lists each item on the Risk of Bias assessment instrument of included RCTs. Of the seven RCTs identified, six were of “acceptable quality” [60, 82–86] and one was of “low quality”. [87] Table 4 shows the data extraction of each RCT. There were five studies involving OMT [83–87] as the intervention, one study examining SMT [60], and one study which provided multimodal treatment. [82] Of the five studies that examined OMT, four were compared to sham or placebo ultrasound and/or usual obstetric care (UOBC) [83–85, 87] and one did not have a comparison group. [86] All of the studies that applied an OMT protocol to pregnant women in the third trimester did not report any specific adverse events with respect to worsening their back pain and/or an increase in poor labour and delivery outcomes. [83–85, 87] One study that examined the effects of OMT in women experiencing postpartum-related back pain did state that there were no serious adverse events reported, however occasionally participants did complain of being tired following the intervention. [83]
Two RCTs included SMT in their study design; one compared a multimodal approach including SMT to UOBC [82] and the other compared SMT and exercise to neuroemotional technique (NET) and a control group consisting of individual home exercises and information. Both of these studies asked patients to recall any negative reactions to treatment at the follow up visit. Both studies did not have any serious adverse or long-lasting events to report. However, the study involving SMT and exercise compared with NET did state that 6% and 18% of participants experienced soreness, respectively.
Cohort Studies

Table 5

Table 6 Table 5 lists each item on the Risk of Bias assessment instrument of included cohort studies. Of the cohort studies included two were of “acceptable quality” [88, 89], one was of “low quality” [90] and two were considered “unacceptable quality”. [91, 92] The two “unacceptable quality” studies were removed. Table 6 shows the data extraction of each cohort study. In the first “acceptable quality” cohort study, it was determined that following a high velocity thrust technique (HVTT) for a maximum of two attempts per symptomatic side, 80% of participants reported an improvement of 50% or more within the first 24 to 72 hours following the intervention. [88] In this cohort study, no subject was determined to have greater disability or pain after the intervention. [88] The second “acceptable quality” cohort study examined chiropractic treatment (unspecified method or frequency, left up to the treating clinician) on pregnant women with LBP and/or PGP at one, three, six and 12 months following the start of treatment. [89] A large proportion of women undergoing chiropractic treatment reported clinically relevant improvements in their symptoms at all time points. Eighty-five percent of the participants were “very happy” or “happy” with their treatment and the authors reported that no adverse events had occurred. [89]

Table 7

Table 8 The final cohort study of “low quality” determined the effects of a 20 to 30 minute OMT treatment on women who delivered within 48 hours. Although their preliminary results suggested that OMT is efficacious for postpartum pain management, 18.6% of participants experienced a slight increase in tenderness and sharpness immediately following their treatment. [90]
Case studies
Table 7 lists each item on the CARE checklist. [75] Only one case study [93] reported a serious adverse event following SMT on the cervical spine in a 16 week pregnant woman (Table 8). Immediately following a cervical SMT treatment the patient experienced right-sided anterior neck pain and developed ipsilateral Horner’s syndrome as a result of a dissection of the right internal carotid artery. Four days following the treatment, the patient miscarried. The patient was admitted to the ICU and treated accordingly. One year later, the Horner’s symptoms still persisted.
Discussion
This systematic review provides an update of the literature regarding SMT during pregnancy and the postpartum period, as well as a review of any adverse events associated with the reported studies. With the exception of one case study, all studies reported only minor and transient events. The case study demonstrated an adverse event following cervical spinal manipulation. When added to the results of our 2012 review (four events following cervical SMT and three events following lumbar SMT) adverse events following SMT in these populations still appear to be scarce.
One important revelation in this review is the lack of adverse events being reported, which was also highlighted in a few of the studies included in this review. [77, 82] Tracking of adverse events was not common practice in higher quality studies, such as RCTs, until the CONSORT guidelines [94, 95] were developed and changed over the years to encourage researchers to do so. Unfortunately, the reporting of adverse events is a missing component of research papers. In the current paper, the fact that very few adverse events were reported, does not mean that others did not happen. There has to be a greater effort made by researchers to report not only adverse events associated with studies but also to clearly state that no adverse events occurred when that is the case. Future research should not only focus on reporting the presence or absence of adverse events, [76] but also determining the adverse events that occur at each of the different pain locations experienced by pregnant and postpartum patients. Recently, there has been a greater emphasis on delineating the various pain locations (lumbar spine LBP versus PGP versus combined pain) experienced by pregnant and postpartum patients. [57, 58, 76, 96, 97] Robust trials on the effectiveness of SMT for cervical and thoracic spine in these populations are required to help inform decisions regarding care. By utilizing all of this information, future studies can be designed and ultimately determine possible prevention and effective management strategies for these populations.
Chiropractors are well versed in treating pregnant and postpartum patients. [59] However, the evidence with respect to safe and effective treatment options, including SMT, in these patients is limited. Two recent SRs regarding pregnancy [58] and postpartum-related back pain [57] have suggested that SMT should be considered as a possible modality to treat these two populations. Although the strength for SMT in these two SRs was inconclusive, it has been suggested that a trial of care may be warranted to see if it produces symptomatic relief for patients. [4, 57, 58] Determining conclusive evidence in these populations may be difficult simply because of the rarity of these events. [93] In one RCT examining the effects of a multimodal program including SMT on LBP the authors suggest that although adverse events during pregnancy are rare, treatments should not be performed unless there is a positive response within a trial of care period. [82] Unfortunately, there is even less evidence with respect to the safety and suggested treatment strategies for neck pain during the pregnant and postpartum period.
We continue to support the suggestions from our previous review: [69](1) that contraindications to SMT are evident during a careful history and physical exam;
(2) clinicians treating these two populations should consider prothrombotic and joint laxity risk factors when determining their treatment plan and attempt to minimize the risk of potentially dangerous and neurological complications; and
(3) pregnant and postpartum women at higher risk for complications, such as those in a post-thrombotic state or possible joint laxity, should be treated with additional caution.
These patients should be counselled with respect to the risks of SMT and educated as to the signs and symptoms of possible neurovascular complications. [69] In addition, we believe that future studies should include the presence or absence adverse events. Reporting this information will help to inform stakeholders of the actual possible adverse events that may occur in these populations.
Strengths and limitations
A key strength of this review is that a thorough search of the literature was conducted by a health science librarian, multiple electronic databases were searched, and we employed a number of broad search terms. Another strength for this review is that we expanded our search to include all forms of literature including SRs and meta-analyses, RCTs, cohort and case studies. In general, the information garnered in this paper should provide practicing chiropractors, chiropractic educators, chiropractic patients and other allied health professionals a reasonable and evidence-based rationale to the safety of SMT in these two populations.
There are a few limitations associated with this review. The first is the number of studies available and the hierarchy of available evidence. Similar to our 2012 review, the majority of the papers identifying serious adverse events were case studies, and they are considered lower levels of evidence because of their high risk of bias. The second limitation is the reporting of adverse events, or lack thereof in clinical trials. In most of the papers included in this review there was no mention of whether or not an adverse event occurred following treatment. Similar to the limitations of our previous review, we suggest that given the lower levels of evidence and the lack of reporting of adverse events, the possibility of risk to pregnant and postpartum undergoing SMT cannot be measure or stated definitively. In addition, it cannot be determined if any such risk level is higher or lower than in non-pregnant or postpartum populations. There is a need to execute more robust high-quality studies, such as the SafetyNET active surveillance reporting system, [98, 99] to rigorously track adverse events and potentially develop mitigation strategies in these populations. The third limitation is the time frame since the current search was completed. Although it has been two years since the last search, similar to what we found between the original study and the current one, we do not anticipate any major changes with respect to the reporting of adverse events. However, a future update will be completed in a more expedient manner. The final limitation is the restriction of our postpartum timeline of six weeks. The hormonal changes that occur with pregnancy do not automatically revert back to a pre-pregnancy state with birth of a child. Therefore, we maybe limiting the number of studies that could have been retrieved and the adverse events associated with them. Extending the postpartum timeline should be considered for a future update.
Conclusions
High quality studies, such as RCTs, regarding SMT for pregnancy- and postpartum-related spinal pain are lacking. This update of our previous review found one case study [93] that demonstrated a serious adverse event following SMT in the cervical spine and a handful of minor and transient adverse events in the low back. [18, 60, 76, 77, 86] Although we are calling for improved reporting of such events in all papers going forward, it appears these events are rare. Future research should focus on the proper reporting of all adverse events while assessing efficacy of appropriate treatment options for these populations.
Supplementary MaterialAppendix 1. Search strategy terms (141.4KB, pdf)
Appendix 2. Excluded articles (141.4KB, pdf)
Footnotes
The authors have no disclaimers, competing interests, or sources of support or funding to report in the preparation of this manuscript.
References:
Malmqvist S, Kjaermann I, Andersen K, Økland I, Brønnick K, Larsen JP.
Prevalence of low back and pelvic pain during pregnancy
in a Norwegian population.
J Manipulative Physiol Ther. 2012;35(4):272-278.Kovacs FM, Garcia E, Royuela A, González L, Abraira V.
Prevalence and factors associated with low back pain and
pelvic girdle pain during pregnancy: a multicenter study
conducted in the Spanish National Health Service.
Spine. 2012;37(17):1516-1533.Vermani E, Mittal R, Weeks A.
Pelvic girdle pain and low back pain in pregnancy: a review.
Pain Pract. 2010;10(1):60-71.Vleeming A, Albert H, Ostgaard H, Sturesson B, Stuge B.
European Guidelines for the Diagnosis and Treatment
of Pelvic Girdle Pain
Eur Spine J. 2008;17(6):794-819.
European Commission, Research Directorate-General,
Department of Policy, Coordination and StrategyBrowning M.
Low Back and Pelvic Girdle Pain of Pregnancy:
Recommendations for Diagnosis
and Clinical Management
J Clinical Chiropractic Pediatrics 2010 (Dec); 11 (2): 775—779Mogren I, Pohjanen A.
Low back pain and pelvic pain during pregnancy.
Spine. 2005;30(8):983-991.Stapleton DB, MacLennan AH, Kristiansson P.
The prevalence of recalled low back pain during and
after pregnancy: a South Australian population survey.
Aust N Z J Obstetr Gyn. 2002;42(5):482-485.Schytt A, Lindmark G, Waldenstrom U.
Physical symptoms after childbirth: prevalence and
associations with self-rated health.
BJOG. 2005;112(2):210-217.Bastiaenen C, Bie R, Vlaeyen J, Goossens M, Leffers P, Wolters P, et al.
Long-term effectiveness and costs of a brief self-management
intervention in women with pregnancy-related
low back pain after delivery.
BMC Pregnancy Childbirth. 2008; 8(19).Mogren IM.
Physical activity and persistent low back pain
and pelvic pain post partum.
BMC Public Health. 2008;8:417.Lindal E, Hauksson A, Arnardottir S, Hallgrimsson J.
Low back pain, smoking and employment during pregnancy
and after delivery - a 3-month follow-up study.
J Obstet Gynaecol. 2000;20(3):263-266.Turgut F, Turgut M, Cetinsahin M.
A prospective study of persistent back pain after pregnancy.
Eur J Obstetr Gynec Reprod Biol. 1998;80:45-48.Gutke A, Lundberg M, Ostgaard H, Oberg B.
Impact of postpartum lumbopelvic pain on disability, pain intensity,
health-related quality of life, activity level,
kinesiophobia, and depressive symptoms.
Eur Spine J. 2011;20(3):440-448.Stuge B, Laerum E, Kirkesola G, Vøllestad N.
The efficacy of a treatment program focusing on specific
stabilizing exercises for pelvic girdle pain after
pregnancy: a randomized controlled trial.
Spine. 2004;29(4):351-359.Pierce H, Homer CS, Dahlen HG, King J.
Pregnancyrelated lumbopelvic pain:
listening to Australian women.
Nurs Res Pract. 2012;2012:387428.Ansari N, Hasson S, Naghdi S, Keyhani S, Jalaie S.
Low back pain duirng pregnancy in Iranian women.
Physiother Theory Pract. 2010;26:40-48.Sipko T, Grygier D, Barczyk K, Eliasz G.
The occurrence of strain symptoms in the lumbosacral region
and pelvis during pregnancy and after childbirth.
J Manip Physiol Ther. 2010;33(5):370-377.Hall H, Cramer H, Sundberg T, Ward L, Adams J, Moore C, et al.
The effectiveness of complementary manual therapies for
pregnancy-related back and pelvic pain:
a systematic review with meta-analysis.
Medicine. 2016;95(38).Skaggs C, George J, Nelson D, Gross G, Prather H, Thompson P.
Back and Pelvic Pain in an Underserved United States
Pregnant Population: A Preliminary Descriptive Survey
J Manipulative Physiol Ther. 2007 (Feb); 30 (2): 130–134Lisi AJ.
Chiropractic spinal manipulation for low back pain
of pregnancy: a retrospective case series.
J Midwif Women Health. 2006;51(1):e7-e10.Pennick VE, Young G.
Interventions for preventing and treating
pelvic and back pain in pregnancy.
Cochrane Database Syst Rev. 2007(2):CD001139.Fast A, Weiss L, Ducommun EJ, Medina E, Butler JG.
Low-back pain in pregnancy. Abdominal muscles,
sit-up performance, and back pain.
Spine. 1990;15(1):28-30.Gilleard W, Brown J.
Structure and function of the abdominal muscles in primgravid
subjects during pregnancy and the immediate postbirth period.
Phys Ther. 1996;76(7):750-762.Weis CA, Triano JJ, Barrett J, Campbell MD, Croy M, Roeder J.
Ultrasound assessment of abdominal muscle thickness
in postpartum vs nulliparous women.
J Manip Physiol Ther. 2015;38(5):352-357.Kristiansson P, Savardsudd K, von Schoultz B.
Back pain during pregnancy. A prospective study.
Spine. 1996;21(6):702-709.Mens J, Vleeming A, Stoeckart R, Stam H, Snijders C.
Understanding peripartum pelvic pain.
Implications of a patient survey.
Spine. 1996;21:1363-1370.Beighton P, Solomon L, Soskolne C.
Articular mobility in an African population.
Ann Rheumatol Dis. 1973;32:413-418.Carter C, Wilkinson J.
Persistent joint laxity and congenital dislocation.
J Bone Joint Surg (Br). 1964(46B):40-25.Bjorklund K, Bergstrom S, Nordström M, Ulmsten U.
Symphyseal distention in relation to serum relaxin levels
and pelvic pain in pregnancy.
Acta Obstet Gynecol Scand. 2000;70:269-275.Marnach M, Ramin K, Ramsey P, Song S, Stensland J, An K.
Characterization of the relationship between joing laxity
and maternal hormones in pregnancy.
Obstet Gynecol. 2003;101:331-335.Calguneri M, Bird H, Wright A.
Changes in joint laxity occurring during pregnancy.
Ann Rheumatol Dis. 1982;41: 126-128.Harvey M, Johnston S, Davies G.
Mid-trimester serum relaxin concentrations and
post-partum pelic floor dysfunction.
Acta Obstet Gynecol Scand. 2008;87(12):1315-1321.Hansen A, Jensen D, Larsen E, Wilken-Jensen C, Petersen K.
Relaxin is not realted to symptom-giving pelvic
relaxation in pregnant women.
Acta Obstet Gynecol Scand. 1996;75: 245-249.Mens J, Pool-Goudzwaard A, Stam H.
Mobility of the pelvic joints in pregnancy-related
lumbopelvic pian: a systematic review.
Obstet Gynecol Surv. 2009;64:200208.
doi: 10.1097/OGX.0b013e3181950f1b.Stuber KJ, Smith DL.
Chiropractic treatment of pregnancy-related low back pain:
a systematic review of the evidence.
J Manipulative Physiol Ther. 2008;31(6):447–454.
doi: 10.1016/j.jmpt.2008.06.009.Haldeman S, Carroll L, Cassidy J.
Findings from the Bone and Joint Decade 2000 to 2010
Task Force on Neck Pain and its Associated Disorders.
J Occupational Environ Med. 2010;52:424–427.
doi: 10.1097/JOM.0b013e3181d44f3b.Natvig B, Ihlebaek C, Grotle M, Brage S, Bruugsgaard D.
Neck pain is often a part of widespread pain and
is associated with reduced functioning.
Spine. 2010;35:E1285–E1289.
doi: 10.1097/BRS.0b013e3181e38e73.Bussieres AE, Stewart G, Al Zoubi F, Decina P, Descarreaux M, Hayden J.
The treatment of whiplash and neck pain associated disorders:
Canadian Chiropractic Guideline Initiative
clinical practice guideline.
J Manip Physiol Ther. 2016;39:523–604.
doi: 10.1016/j.jmpt.2016.08.007.Coulter I, Hurwitz E, Adams A.
Patients Using Chiropractors in North America:
Who Are They, and Why Are They in Chiropractic Care?
Spine (Phila Pa 1976) 2002 (Feb 1); 27 (3): 291–298Carbonell JL, Varela L, Velazco A, Cabezas E, Fernández C, Sánchez C.
Oral methotrexate and vaginal misoprostol for early abortion.
Contraception. 1998;57(2):83–88.
doi: 10.1016/s0010-7824(98)00004-3.World Health Organization.
Headache disorders.
Geneva, Switzerland: World Health Organization; 2016.
[Available from:
http://www.who.int/news-room/fact-sheets/detail/headache-disorders.Bishop P, Quon J, Fisher C, Dvorak M.
The Chiropractic Hospital-based Interventions Research
Outcomes (CHIRO) study: A Randomized Controlled Trial
on the Effectiveness of Clinical Practice Guidelines
in the Medical and Chiropractic Management of Patients
with Acute Mechanical Low Back Pain
Spine J. 2010 (Dec); 10 (12): 1055?1064McMorland G, Suter E.
Chiropractic managment of mechanical neck and low back pain:
a retrospective, outcome-based analysis.
J Manip Physiol Ther. 2000;23:307–311.Shekelle P, Coulter I.
Cervical spine manipulation: summary report of a systematic
review of the literature and multidisciplinary expert panel.
J Spinal Dis. 1997;10:223226.Nelson C.
Principles of effective headache management.
Topics Clin Chiropr. 1998;5:55–61.Bryans R, Descarreaux M, Duranleau M, Marcoux M, Potter B, Ruegg R, et al.
Evidence-Based Guidelines for the Chiropractic Treatment
of Adults With Headache
J Manipulative Physiol Ther. 2011 (Jun); 34 (5): 274–289Khorsan R, Hawk C, Lisi AJ, Kizhakkeveettil A.
Manipulative Therapy for Pregnancy and Related Conditions:
A Systematic Review
Obstet Gynecol Surv 2009 (Jun); 64 (6): 416–427Chung CLR, Cote P, Stern PJ, L’Esperance G.
The association between cervical spine manipulation and
carotid dissection: a systematic reivew of the literature.
J Manip Physiol Ther. 2015;38(9):672–676.
doi: 10.1016/j.jmpt.2013.09.005.Hurwitz E, Carragee E, van der Velde G, Carroll L, Nordin M, Guzman J, et al.
Treatment of Neck Pain: Noninvasive Interventions:
Results of the Bone and Joint Decade 2000–2010
Task Force on Neck Pain and Its Associated Disorders
J Manipulative Physiol Ther 2009 (Feb); 32 (2): S141–S175Heiner J.
Cervical epidural hematoma after chiropractic spinal manipulation.
The Am J Emerg Med. 2009;27(8):1023.e1–2.
doi: 10.1016/j.ajem.2008.12.031.Schmitz A, Lutterbey G, von Engelhardt L, von Falkenhausen M, Stoffel M.
Pathological cervical fracture after spinal manipulation
in a pregnant patient.
J Manip Physiol Ther. 2005;28(8):633–636.
doi: 10.1016/j.jmpt.2005.08.017.Cassidy J, Boyle E, Cote P, Hogg-Johnson S, Silver F, Bondy S.
Risk of Vertebrobasilar Stroke and Chiropractic Care:
Results of a Population-based Case-control
and Case-crossover Study
Spine (Phila Pa 1976) 2008 (Feb 15); 33 (4 Suppl): S176–183Oliphant D.
Safety of Spinal Manipulation in the Treatment
of Lumbar Disk Herniations: A Systematic
Review and Risk Assessment
J Manipulative Physiol Ther 2004 (Mar); 27 (3): 197–210Hurwitz E, Randhawa K, Torres P, Yu H, Verville L, Hartvigsen J, et al.
The global spine care initiative: a systematic review of individual
and communitybased burden of spinal disorders in rural populations
in low- and middle-income communities.
Eur Spine J. 2017;27(Supplement 6):802–815.
doi: 10.1007/s00586-017-5393-z.Carroll LJ, Hurwitz EL, Cote P, Hogg-Johnson S, Carragee E, Nordin M, et al.
Research Priorities and Methodological Implications:
The Bone and Joint Decade 2000-2010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S214–S220Boyle E, Cote P, Grier AR, Cassidy JD.
Examining Vertebrobasilar Artery Stroke
in Two Canadian Provinces
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S170–175 .Weis CA, Pohlman KA, Draper C, da Silva-Oolup S, Stuber K, Hawk C.
Chiropactic care of adults with postpartum-related low back,
pelvic girdle and combination pain: a systematic review.
J Manip Physiol Ther. 2020;43(7):732–743.
doi: 10.1016/j.jmpt.2020.05.006.Weis CA, Pohlman KA, Draper C, da Silva-Oolup S, Stuber K, Hawk C.
Chiropractic care for adults with pregnancy-related low back,
pelvic girdle or combination pain: a systematic review.
J Manip Physiol Ther. 2020;43(7):714–731.
doi: 10.1016/j.jmpt.2020.05.005.Yuen T, Wells K, Benoit S, Yohanathan S, Capelletti L, Stuber K.
Therapeutic interventions employed by Greater Toronto Area chiropractors
on pregnant patients: results of a cross-sectional online survey.
J Can Chiropr Assoc. 2013;57(2):132–142.Peterson C, Haas M, Gregory W.
A pilot randomized controlled trial comparing the efficacy of exercise,
spinal manipulation, and neuro emotional technique for the
treatment of pregnancy-related low back pain.
Chiropr Man Therap. 2012;20(1):18.
doi: 10.1186/2045-709X-20-18.George J, Skaggs C, Thompson P, Nelson D, JAG, Gross G.
A Randomized Controlled Trial Comparing a Multimodal
Intervention and Standard Obstetrics Care for
Low Back and Pelvic Pain in Pregnancy
Am J Obstet Gynecol. 2013 (Apr); 208 (4): 295.e1-7Kamel DM, Raoof NAA, Tantawy SA.
Efficacy of lumbar mobilization on postpartum low back pain
in Egyptian females: a randomized control trial.
J Back Musculoskelet Rehabil. 2016;29(1):55–63.
doi: 10.3233/BMR-150598.Sadr S, Pourkiani-Allah-Abad N, Stuber K.
The Treatment Experience of Patients with
Low Back Pain During Pregnancy and Their
Chiropractors: A Qualitative Study
Chiropractic & Manual Therapies 2012 (Oct 9); 20 (1): 32Drife J.
Thromboembolism: reducing maternal death and disability during pregnancy.
Br Med J. 2003;67(1):177–190.Stella C, Sibai B.
Thrombophilia and adverse maternalperinatal outcome.
Clin Obstet Gynecol. 2006;49:850–860.
doi: 10.1097/01.grf.0000211954.66959.e1.Ng KP, Doube A.
Stroke after neck manipulation in the post partum period.
N Z Med J. 114(1143):498.Parkin PJ, Wallis WE, Wilson JL.
Vertebral artery occlusion following manipulation of the neck.
N Z Med J. 1978;88:441–443.Murphy DR, Hurwitz EL, McGovern EE.
Outcome of Pregnancy-Related Lumbopelvic Pain
Treated According to a Diagnosis-Based
Decision Rule: A Prospective
Observational Cohort Study
J Manipulative Physiol Ther 2009 (Oct); 32 (8): 616–624Stuber KJ, Wynd S, Weis CA.
Adverse Events From Spinal Manipulation
in the Pregnant and Postpartum Periods:
A Critical Review of the Literature
Chiropractic & Manual Therapies 2012 (Mar 28); 20: 8Gutke A, Betten C, Degerskar K, Pousette S, Olsen MF.
Treatments for pregnancy-related lumbopelvic pain: a
systematic review of physiotherapy modalities.
Acta Obstet Gynecol Scand. 2015;94(11):1156–1167.
doi: 10.1111/aogs.12681.Hawk C, Minkalis A, Khorsan R, Daniels C, Homack D, Gliedt J, et al.
Systematic Review of Nondrug, Nonsurgical
Treatment of Shoulder Conditions
J Manipulative Physiol Ther 2017 (Jun); 40 (5): 293–319Scottish Intercollegiate Guideline Network (SIGN)
Methodology checklist 1: systematic reviews and metaanalyses
[Internet] Edinburgh: SIGN; 2015. [cited 2018 Sep 17].
Available from:
https://www.sign.ac.uk/what-we-do/methodology/checklists/Scottish Intercollegiate Guideline (SIGN)
Methodology checklist 3: cohort studies
[Internet] Edinburgh: SIGN; 2015. [cited 2018 Sep 17].
Available from:
https://www.sign.ac.uk/what-we-do/methodology/checklists/Scottish Intercollegiate Guideline (SIGN)
Methodology checklist 2: controlled trials
[Internet] Edinburgh: SIGN; 2015. [cited 2018 Sep 17].
Available from:
https://www.sign.ac.uk/what-we-do/methodology/checklists/Gagnier J, Kienle G, Altman D, Moher D, Sox H, Riley D.
The CARE guidelines: Consensus-based clinical
case reporting guideline development.
Glob Adv Health Med. 2013;2(5):38–43.
doi: 10.7453/gahmj.2013.008.Liddle Sarah D, Pennick V.
Interventions for preventing and treating
low-back and pelvic pain during pregnancy.
Cochrane Database Syst Rev. 2015;(9)
doi: 10.1002/14651858.CD001139.pub4.Ruffini N, D’Alessandro G, Cardinali L, Frondaroli F, Cerritelli F.
Osteopathic manipulative treatment in gynecology
and obstetrics: a systematic review.
Compl Ther Med. 2016;26:72–78.
doi: 10.1016/j.ctim.2016.03.005.Franke H, Franke J-D, Belz S, Fryer G.
Osteopathic manipulative treatment for low back and pelvic girdle pain
during and after pregnancy: a systematic review and metaanalysis.
J Bodywork Mov Ther. 2017;21(4):752–762.
doi: 10.1016/j.jbmt.2017.05.014.Sharma A, Sharma S, Steiner LA, Brudvig TJ.
Identification and effectiveness of physical therapy interventions
for sacroiliac joint dysfunction in pregnant and
nonpregnant adults: a systematic review.
J Women Health Phys Ther. 2014;38(3):110–117.Majchrzycki M, Wolski H, Seremak-Mrozikiewicz A, Lipiec J, et al.
Application of osteopathic manipulative technique in
the treatment of back pain during pregnancy.
Ginekologia Polska. 2015;86(3):224–228.
doi: 10.17772/gp/2066.Posadzki P, Ernst E.
Spinal manipulation: an update of a systematic review
of systematic reviews.
N Z Med J. 2011;124(1340):55–71.Gausel A, Kjaermann I, Malmqvist S, Andersen K, Dalen I, Larsen J, et al.
Chiropractic management of dominating one-sided pelvic
girdle pain in pregnant women; a randomized controlled trial.
BMC Pregnancy Childbirth. 2017;17(1):331.
doi: 10.1186/s12884-017-1528-9.Licciardone J, Buchanan S, Hensel K, King H, Fulda K, Stoll S.
Osteopathic manipulative treatment of back pain and related
symptoms during pregnancy: a randomized controlled trial.
Am J Obstet Gynecol. 2010;202(1):43:e1e8.
doi: 10.1016/j.ajog.2009.07.057.Licciardone J, Aryal S.
Prevention of progressive backspecific dysfunction during pregnancy:
an assessment of osteopathic manual treatment based on
Cochrane Back Review Group criteria.
J Am Osteopath Assoc. 2013;113(10):728–736.
doi: 10.7556/jaoa.2013.043.Hensel KL, Roane BM, Chaphekar AV, Smith-Barbaro P.
PROMOTE Study: safety of osteopathic manipulative treatment during
the third trimester by labor and delivery outcomes.
J Am Osteopath Assoc. 2016;116(11):698–703.
doi: 10.7556/jaoa.2016.140.Schwerla F, Rother K, Rother D, Ruetz M, Resch K-L.
Osteopathic manipulative therapy in women with postpartum low back
pain and disability: a pragmatic randomized controlled trial.
J Am Osteopath Assoc. 2015;115(7):416–425.
doi: 10.7556/jaoa.2015.087.Hensel K, Carnes M, Stoll S.
Pregnancy research on osteopathic manipulation optimizing
treatment effects: the PROMOTE study protocol.
J Am Osteopath Assoc. 2016;116(11):716–724.
doi: 10.7556/jaoa.2016.142.Al-Sayegh N, George S, Boninger M, Rogers J, Whitney S, Delitto A.
Spinal mobilization of postpartum low back and pelvic girdle pain:
an evidence-based clinical rule for predicting responders and nonresponders.
PM R. 2010;2(11):995–1005.
doi: 10.1016/j.pmrj.2010.07.481.Peterson C, Muhlemann D, Humphreys B.
Outcomes Of Pregnant Patients With Low Back Pain Undergoing
Chiropractic Treatment: A Prospective Cohort Study With
Short Term, Medium Term and 1 Year Follow-up
Chiropractic & Manual Therapies 2014 (Apr 1); 22 (1): 15Hastings V, McCallister AM, Curtis S, Valant R, Yao S.
Efficacy of osteopathic manipulative treatment for
management of postpartum pain.
J Am Osteopath Assoc. 2016;116(8):502–509.
doi: 10.7556/jaoa.2016.103.Haavik H, Murphy B, Kruger J.
Effect of Spinal Manipulation on Pelvic Floor Functional
Changes in Pregnant and Nonpregnant Women:
A Preliminary Study
J Manipulative Physiol Ther. 2016 (Jun); 39 (5): 339–347Skarica B.
Effectiveness of manual treatment on pregnancy symptoms:
sefulness of manual treatment in treating pregnancy symptoms.
Med Arch. 2018;72(2):131135.
doi: 10.5455/medarh.2018.72.131-135.Morton A.
Internal carotid artery dissection following chiropractic treatment
in a pregnant woman with Systemic Lupus Erythematosus.
Chiropr Man Ther. 2012;20(38)
doi: 10.1186/2045-709X-20-38.Ioannidis JPA, Evans SJW, Gotzsche PC, O’Neill RT, Altman DG, Schulz K, et al.
Better reporting of harms in randomized trials:
an extension of the CONSORT Statement.
Ann Intern Med. 2004;141:781–788.
doi: 10.7326/0003-4819-141-10-200411160-00009.Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, et al.
CONSORT 2010 explanation and elaboration: updated guidelines
for reporting parallel group randomised trials.
Intl J Surg. 2010;10(1):28–55.
doi: 10.1016/j.ijsu.2011.10.001.Tavares P, Barrett J, Hogg-Johnson S, Ho S, Corso M, Batley S, et al.
Prevalence of low back pain, pelvic girdle pain, and
combination pain in a postpartum Ontario population.
J Obstet Gynaecol Canada. 2020;42(4):473480.
doi: 10.1016/j.jogc.2019.08.030.Weis C, Barrett J, Tavares P, Draper C, Ngo K, Leung J, et al.
Prevalence of low back pain, pelvic girdle pain, and
combination pain in a pregnant Ontario population.
J Obstet Gynaecol Canada. 2018;40(8):1038–1043.
doi: 10.1016/j.jogc.2017.10.032.Vohra S, Kawchuk G, Boon H, Caulfield T, Pohlman KA.
SafetyNET: An interdisciplinary team supporting a safety
culture for a spinal manipulation therapy.
Eur J Integrat Med. 2014;6(4):473–477.Pohlman KA, Funabashi M, Ndetan H, Hogg-Johnson S, Bodnar P, Kawchuk G.
Assessing adverse events after chiropractic care at a
chiropractic teaching clinic: an active surveillance pilot study.
J Manip Physiol Ther. 2020;43(9):845–854.
doi: 10.1016/j.jmpt.2020.05.007.
Return to ADVERSE EVENTS
Since 10-27-2024


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |