

Reliability and Validity of Self-reported Questionnaires
to Measure Pain and Disability in Adults with Neck Pain
and its Associated Disorders: Part 3 - A Systematic
Review From the CADRE CollaborationThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: European Spine Journal 2019 (May); 28 (5): 1156–1179 ~ FULL TEXT
Lemeunier N, da Silva-Oolup S, Olesen K, Shearer H, Carroll LJ, Brady O, Côté E, Stern P, et al,
Institut Franco-Européen de Chiropraxie,
72 chemin de la Flambère,
31300, Toulouse, France.
nlemeunier@ifec.net
PURPOSE: To determine the reliability and validity of self-reported questionnaires to measure pain and disability in adults with grades I-IV neck pain and its associated disorders (NAD).
METHODS: We updated the systematic review of the 2000-2010 Bone and Joint Decade Task Force on Neck Pain and its Associated Disorders and systematically searched databases from 2005 to 2017. Independent reviewers screened and critically appraised studies using standardized tools. Evidence from low-risk-of-bias studies was synthesized according to best evidence synthesis principles. Validity studies were ranked according to the Sackett and Haynes classification.
RESULTS: We screened 2,823 articles, and 26 were eligible for critical appraisal; 18 were low risk of bias. Preliminary evidence suggests that the Neck Disability Index (original and short versions), Whiplash Disability Questionnaire, Neck Pain Driving Index, and ProFitMap-Neck may be valid and reliable to measure disability in patients with NAD. We found preliminary evidence for the validity and reliability of pain measurements including the Body Pain Diagram, Visual Analogue Scale, the Numeric Rating Scale and the Pain-DETECT Questionnaire.
CONCLUSION: The evidence supporting the validity and reliability of instruments used to measure pain and disability is preliminary. Further validity studies are needed to confirm the clinical utility of self-reported questionnaires to assess pain and disability in patients with NAD. These slides can be retrieved under Electronic Supplementary Material.
KEYWORDS: Neck pain · Disability · Self-reported questionnaire · Reliability/validity · Systematic review
From the FULL TEXT Article:
Introduction
Clinicians use self-reported questionnaires to measure pain and disability in individuals with neck pain and its associated disorders (NAD). In 2008, the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders (NPTF) reviewed the literature to determine the psychometric properties of self-reported questionnaires used to measure neck pain and its related disability. [1] The NPTF found preliminary evidence supporting the validity or reliability of the Cervical Spine Outcomes Questionnaire, Whiplash Disability Questionnaire, Copenhagen Neck Functional Disability Scale, Neck Pain and Disability Scale, and Neck Disability Index. However, little evidence was found to support the clinical utility of these instruments.
A more recent systematic review by Schellingerhout et al. [2] evaluated the psychometric properties of eight questionnaires used to assess disability in patients with NAD. The authors found evidence to support the use of the Neck Disability Index. Limited evidence was available to support the use of the seven other questionnaires. [2]
Our systematic review updates the NPTF findings on the reliability and validity of self-reported questionnaires assessing pain and disability in adults with NAD. This review is the third in a series of five systematic reviews updating the NPTF on assessment of patients with NAD. [3-7] These reviews will inform the development of a clinical practice guideline for the clinical assessment of NAD.
Methods
Registration
We registered this protocol with the International Prospective Register of Systematic Reviews (PROSPERO) on February 4, 2016 (registration number: CRDXXXXXXXXXXX).
Eligibility criteriaPopulation Our review targeted studies of adults with NAD [8] and whiplash-associated disorder (WAD) grades I–IV [9] (Appendix 1).
Definitions Self-reported questionnaires measure subjective health constructs such as pain or disability. [10-12] Questionnaires can be completed electronically, on paper, or in interview. Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage. [13] Disability is an umbrella term, covering impairments in body function, activity/functional limitations, and participation restrictions. [14] Reliability describes the consistency of measurements across people or instruments. [15] Validity is the degree to which a test measures what it is intended to measure. [15]
Study characteristics Eligible studies included:(1) English or French peerreviewed publication;
(2) reliability and/or validity study of self-reported questionnaires for pain and/or disability;
(3) adults (≥ 18 years) with NAD or WAD I–IV grades.We excluded:
(1) guidelines, letters, editorials, commentaries, unpublished manuscripts, dissertations, government reports, books and book chapters, conference proceedings, meeting abstracts, lectures and addresses, consensus development statements, guideline statements;
(2) literature reviews, and case studies;
(3) cadaveric or animal studies;
(4) studies solely targeting individuals with grade IV NAD or WAD; or
(5) studies with a sample size < 20 per group.
Data sources and searches
With the assistance of a health science librarian, we developed a search strategy which was reviewed by a second librarian. We searched MEDLINE, CINAHL, PubMed, PsycInfo and the Cochrane Central Register of Controlled Trials from January 1, 2005, to November 7, 2017. Our search overlapped the NPTF search by 1 year to ensure studies were not missed during this period. We used a broad search strategy with terms related to subject headings specific to each database (i.e. MeSH in MEDLINE) and free text words (Appendix 2). We developed the search in MEDLINE through clinical EBSCOhost Online and adapted it to the other databases. Finally, we hand-searched the reference lists of a recent systematic review. [2]
Study selection
We used a two-stage screening process to identify eligible studies. In stage one, three paired reviewers independently screened citation titles and abstracts. Studies were classified as relevant, possibly relevant, or irrelevant. In stage two, four pairs of reviewers independently screened possibly relevant studies to determine eligibility. Reviewers met to resolve disagreements on studies’ eligibility in both stages. We involved a third independent reviewer if consensus could not be reached.
Assessment of risk of bias
Pairs of independent reviewers critically appraised relevant studies. To evaluate the internal validity of eligible studies, we used the modified Quality Appraisal Tool for Studies of Diagnostic Reliability (QAREL) [16] criteria for diagnostic reliability studies and the modified Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) [17] criteria for diagnostic accuracy studies. We modified the original QAREL and QUADAS-2 instruments to include: (1) a question on whether the study objective was clear; (2) “not applicable options” to some items (QAREL item # 3, 4, 5, 6, 8, QUADAS item # 3.1, 3.2, 3.3 and 3.B and (3) the Sackett and Haynes classification (in the QUADAS-2 instrument) to determine the level of scrutiny to which a test has been subjected and determine its clinical utility (described in Appendix 3). [18]
Reviewers met to reach consensus on the internal validity of studies. We contacted authors if we needed additional information to complete the critical appraisal. We included low-risk-of-bias studies in our best evidence synthesis. [19] We classified each low-risk-of-bias validity study according to the classification system by Sackett and Haynes. [18] Phase I or II studies of diagnostic tests provide preliminary evidence of clinical utility, whereas phase III or IV studies are needed to inform the validity and utility of a test in clinical practice (Appendix 3). [18]
Data extraction and synthesis of results
Two reviewers extracted data from studies with low risk of bias and built evidence tables. A third reviewer independently verified the extracted data. Disagreements were resolved through discussion. In addition, a senior epidemiologist reviewed the accuracy of the extracted data by cross-checking it with the original studies. As meta-analysis was not possible due to heterogeneity of studies regarding patient population, clinical setting, and questionnaires evaluated, we performed a qualitative synthesis of findings from low-risk-of-bias studies and developed evidence statements according to principles of best evidence synthesis. [19] We used evidence tables to outline the best evidence on each topic, identify consistencies and inconsistencies in the evidence, and formulate summary statements to describe the body of evidence. We stratified our synthesis by neck-specific questionnaire (assessing pain and/or disability) and type of evidence (reliability and/or validity).
Statistical analyses
We computed the inter-rater agreement using the Kappa coefficient with 95% confidence interval (CI) for each stage of screening. [20] We calculated the percentage agreement for critical appraisal of articles.
Reporting We organized and reported the systematic review based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [21] and Statement for Reporting Studies of Diagnostic Accuracy (STARD). [22]
Results
Study selection
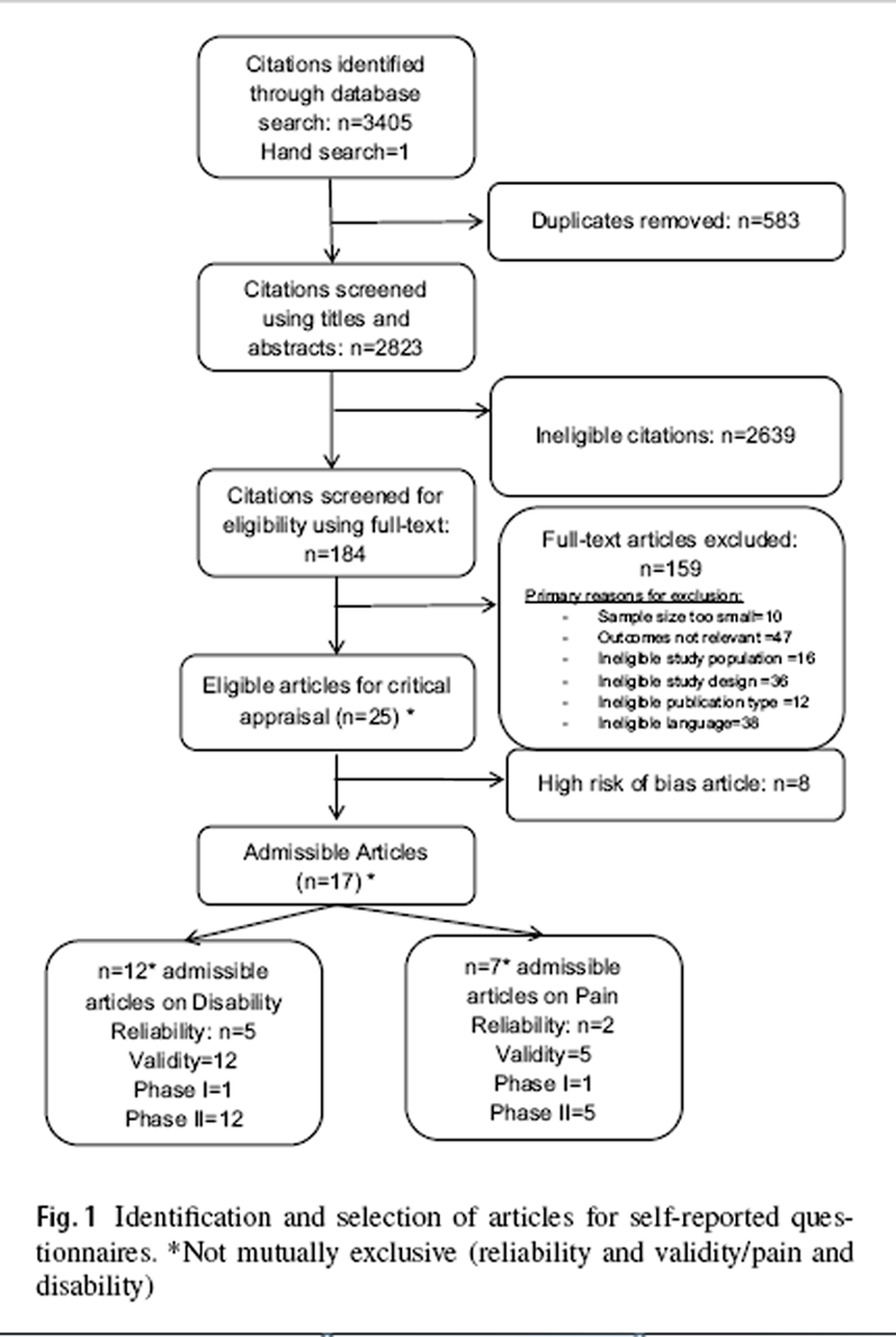
Figure 1 We screened 2,823 citations. Of those, 2,638 were deemed irrelevant in stage one screening and 159 studies were deemed irrelevant in stage-two screening (Figure 1). The inter-rater agreement was: (1) k = 0.44 (95% CI 0.37, 0.50) for title and abstracts; (2) k = 0.19 (95% CI 0.01, 0.38) for full text articles.
The percentage agreement for critical appraisal of the studies was 78% (25/32 studies). Two authors provided clarification on outcome definition and study methodology when contacted. [31, 37]
Study characteristics
Eighteen articles had low risk of bias (seven reliability and 15 validity studies) and were included in our best evidence synthesis. [23–40] One validity study included both phase I and II analyses [66]; one article was a phase I [38] and the other 13 were phase II studies [23, 25–27, 30–32, 34–37, 39, 40].
Articles assessed:(1) pain questionnaires (n = 5) [28, 29, 37, 38, 40],
(2) disability questionnaires (n = 11) [23–27, 31–35, 39], and
(3) both pain and disability questionnaires (n = 2). [30, 36]
Risk of bias
All low-risk-of-bias reliability articles had clear research questions, representative samples of subjects and raters, appropriate blinding of outcome measurements, administration of tests, time intervals and statistical measures (Table 1). Moreover, in 5/7 studies the order of examination did not vary. [23–26, 28] All low-risk-of-bias validity articles had appropriate research questions and used appropriate index tests and reference standards (Table 2). However, these studies had limitations regarding:(1) patient selection (not randomized or consecutive) (9/15) [23, 25, 26, 30, 31, 33, 37, 38, 40] and
(2) unclear time interval between the index test and the reference standard (3/15). [26, 31, 38]Eight articles were deemed high risk of bias due to: inadequate or undisclosed blinding (5/8) [41, 42, 44–46], selection bias (7/8) [41–44, 46–48], and unclear methodology for questionnaire administration (2/8). [42, 45] Furthermore, one reliability study of one low-risk-of-bias article had inappropriate time interval, so reliability findings were not included in our synthesis. [40]
Summary of evidence (questionnaires described in Appendix 4)
For each questionnaire, we provide a summary of the NPTF findings when there are. [1]
Pain questionnaires
ReliabilityVisual Analogue Scale Our review adds evidence for the reliability of the Visual Analogue Scale. [28] One study reported that the Visual Analogue Scale may be reliable to assess pain intensity in NAD patients. The test–retest reliability of the Visual Analogue Scale for pain intensity (retest period = 5–11 days) was ICC = 0.67 (p < 0.008, 95% CI not reported) in adults with persistent NAD II (Table 3). [28]
Body Pain Diagram The inter-method reliability between paper and electronic versions for the measurement of pain location and distribution suggested that neck pain distribution may be reliably scored by either method. [29] The inter-examiner reliability of the Body Pain Diagram was ICC = 0.925 (95% CI 0.901–0.946) for the paper version and 0.997 (95% CI 0.995–0.998) for the electronic version in adults with recent-onset NAD I–II (Table 3). [29]
ValidityPain-DETECT Questionnaire Preliminary evidence from one phase I study suggests that the Pain-DETECT Questionnaire may differentiate the character of the pain in NAD III patients compared to healthy people. The Pain-DETECT Questionnaire scores were found lower for cold/heat pain thresholds and dynamic mechanical allodynia in adults with persistent NAD III than healthy controls [38] (Table 4).
Body Pain Diagram Preliminary evidence suggested that the Body Pain Diagram may be valid to measure pain in NAD patients. One phase II validity study reported a correlation between pain location, pain overlap and pain frequency from the Body Pain Diagram and pain intensity (Visual Analogue Scale; Spearman’s r = 0.28; p = 0.03) and disability (Neck Disability Index; Spearman’s r = 0.40; p = 0.002) in NAD I–III adults [40] (Table 4). However, pain location from the Body Pain Diagram was not correlated with psychological distress (K-10 scale; Spearman’s r = – 0.04, p > 0.05) and cognitive function (Montreal Cognitive Assessment; Spearman’s r = – 0.08, p > 0.05)
Numerical (Pain) Rating Scale Evidence from three phase II studies suggests that the Numerical (Pain) Rating Scale may be valid to measure pain intensity in individuals with persistent and variable duration neck pain [30, 36, 37] (Table 4). In NAD I–II adults, one study reported that pain intensity in the past week was correlated with recorded pain intensity ratings during the prior week (four pain measurements per day for the previous week) (0.79 < Pearson’s r < 0.95). [37] Moreover, two phase II studies assessing the Numerical Rating Scale in NAD I–III adults found a mean difference in pain intensity between individuals reporting improvement versus no improvement on the Global Rating of Change Scale. [30, 36] Specifically, Cleland et al. [30] reported a correlation (Pearson’s r = 0.57; p = 0.01) between change in pain intensity on Numerical Rating Scale and self-reported improvement on Global Rating of Change Scale.
Disability questionnaires
ReliabilityNeck Disability Index Two studies suggest that the Neck Disability Index and its short version are reliable to measure disability in NAD patients. The intra-rater reliability of the Neck Disability Index was ICC = 0.64 (95% CI 0.19–0.84) with a 3-week testing interval [27], and ICC = 0.92 (95% CI 0.85–0.96) with a 1-week interval [26] in adults with chronic NAD I–III. The 1-week test–retest reliability of the short-form Neck Disability Index (5 items) was ICC = 0.91 (95% CI 0.83–0.96) in adults with NAD I–III of unspecified duration [26] (Table 3).
Profile Fitness Mapping Neck Questionnaire (ProfitMap-Neck) The ProFitMap-Neck questionnaire is reliable to assess disability in NAD patients. The 1-week test–retest reliability of the ProFitMap-Neck questionnaire was ICC = 0.90 (95% CI 0.82–0.95) in adults with NAD I–III [23] (Table 3).
Whiplash Disability Questionnaire One study suggests that the Whiplash Disability Questionnaire is reliable to assess disability in patients with WAD. In adults with recent-onset WAD I–III, the intra-rater reliability (3–5 days) was included between 0.82 (95% CI 0.70–0.91) < ICC (95% CI) < 0.89 (95% CI 0.83–0.92) according to WAD grades (Table 3). [24]
Neck Pain Driving Index One study reported that the reliability of the Neck Pain Driving Index is ICC = 0.73 (p < 0.01) in adults with persistent WAD I–III (Table 3). [25]
ValidityDisability of Arm, Shoulder and Hand Questionnaire (DASH) and Quick DASH Two studies (phases I and II) provide preliminary evidence for the validity of the DASH and Quick DASH questionnaires to measure disability in individuals with NAD I–III [31, 33] (Table 4). In a phase I study, a difference of 30.03/100 (95% CI 21.77–38.29) in the mean DASH score was found between individuals with WAD and healthy aged-matched asymptomatic controls. [33] A phase II study reported that the DASH questionnaire scores correlated with the Neck Disability Index [Spearman’s r = 0.77; p < 0.01)]; Visual Analogue Scale—pain intensity (Spearman’s r = 0.53; p < 0.05) and Patient-Specific Functional Scale— stiffness (Spearman’s r = – 0.56; p < 0.01). [33] A second phase II study reported that the DASH and Quick DASH questionnaires are correlated with disability (Neck Disability Index) (0.82 < Pearson’s r < 0.83, p < 0.01), pain severity (Cervical Spine Outcome Questionnaire) (0.55 < Pearson’s r < 0.68, p < 0.01), and pain intensity (Visual Analogue Scale) (0.64 < Pearson’s r < 0.66, p < 0.01) in adults with NAD I–III of variable duration. [31]
Patient-Specific Functional Scale In adults with persistent NAD III, one phase II study provides preliminary evidence of the validity of the Patient- Specific Functional Scale. [36] Individuals with NAD III who reported improvement have a mean difference of 1.6/10 (95% CI 0.9–2.3) compared to those who reported no change on the Global Rating of Change scale [36] (Table 4).
Neck Disability Index New evidence identified in our review combined with the results of the NPTF support the validity of the Neck Disability Index (5, 8, and 10 items) questionnaire to assess disability in individuals with neck pain. Four phase II validity studies suggest that the Neck Disability Index is valid to measure neck disability in individuals with NAD I–III [27, 30, 32, 36] (Table 4).
Three studies found a change in the Neck Disability Index between participants reporting improvement [mean difference from 6.1 (95% CI 3.4–9.5) to 12.9 (95% CI 9.3–16.5)] compared to those who remained stable on the Global Rating of Change Scale [27, 30, 36]. In addition, two articles reported that the Neck Disability Index scores were significantly correlated with self-reported improvement on the Global Rating of Change scale (Pearson’s r = 0.52; p < 0.000 [30]; Pearson’s r = 0.58, p = 0.01 [27]). Finally, one study found that the Neck Disability Index was correlated with VAS—pain intensity (Pearson’s r = – 0.63, p < 0.001), health-related quality of life (SF-12 and the SF-6D) (– 0.50 < Pearson’s r < – 0.77, p < 0.001), and health-related quality of status (EuroQol-5D, EQ-5D) (Pearson’s r = – 0.76, p < 0.001) in adults with WAD I–III. [32]
Two articles reported preliminary evidence supporting the validity of the short versions of the Neck Disability Index to assess disability in NAD patients. [26, 35] One phase II validity study reported significant correlations between the Neck Disability Index-5 (5 items) and pain intensity (Numeric Pain Rating Scale) (Pearson’s r = 0.71, 95% CI 0.49–0.85), kinesiophobia (Tampa Scale for Kinesiophobia) (Pearson’s r = 0.53, 95% CI 0.23–0.74), and pain catastrophizing (Pain Catastrophizing Scale) (Pearson’s r = 0.64, 95% CI 0.38–0.81) in NAD I–III adults of unknown duration [26] (Table 4).
van der Velde et al. performed a Rasch analysis assessing the unidimensionality of the Neck Disability Index in NAD I–III adults (Table 4). The analysis identified that the original 10-item Neck Disability Index was not unidimensional due to 2 items (regarding headache and lifting items); when removed, the 8-item Neck Disability Index was shown to be unidimensional. The construct validity of the 8-item and 10-item Neck Disability Index questionnaires was similar when compared to neck pain intensity. [35]
Profile Fitness Mapping Neck Questionnaire (ProfitMap-Neck) One article provides preliminary evidence (phase II) for the validity of the ProfitMap-Neck assessing functionality of the cervical spine in NAD patients. This study found positive correlations between the ProFitMap-Neck and disability (Neck Disability Index) (Spearman’s r = 0.78) and health-related quality of life (Functional Self-Efficacy Scale: r = 0.58) (p values not reported) in NAD I–III adults [23] (Table 4).
Whiplash Disability Questionnaire Evidence from two phase II validity studies suggests that the Whiplash Disability Questionnaire is valid to measure disability in adults with recent-onset neck pain [34, 39] (Table 4). A phase II study reported that the Whiplash Disability Questionnaire is correlated with pain intensity (Numerical Rating Scale: Pearson’s r = 0.64, p < 0.05), disability (Neck Disability Index: Pearson’s r = 0.80; p < 0.05; and Neck Bournemouth Questionnaire: Pearson’s r = 0.89; p < 0.05), depression (Center for Epidemiologic Studies Depression Scale: Pearson’s r = 0.67; p < 0.05), and healthrelated quality of life (SF-36v2: Pearson’s r = 0.72; p < 0.05) in adults with recent-onset WAD I–III. [34] A phase II validity study found that individuals who recovered from WAD had a mean difference in Whiplash Disability Questionnaire scores of 27.4/130 (95% CI 23.5, 31.3) compared to those who did not report recovery. [39]
Neck Pain Driving Index One phase II study provides preliminary evidence of the Neck Pain Driving Index validity. There are correlations between the Neck Pain Driving Index and pain intensity (Numeric Rating Scale; Spearman’s r = 0.51, p < 0.01) and disability (Neck Disability Index; Spearman’s r = 0.80, p < 0.01) in adults with persistent WAD I–III (Table 4). [25]
Discussion
Our systematic review updated the NPTF findings regarding the reliability and validity of self-reported questionnaires measuring pain and disability in adults aged 18 years or older with NAD I–IV. We identified 18 low-risk-of-bias studies; these studies were included in our best evidence synthesis. Our findings combined with those of the NPTF provide evidence for the measurements of pain location, pain intensity and disability in patients with NAD and WAD.
Update of the NPTF
The Neck Pain Task Force previously identified 19 different low-risk-of-bias studies evaluating 13 self-administered instruments for the evaluation of pain or disability in patients with NAD. [1] The NPTF found evidence to support the: (1) reliability and validity of the Aberdeen Spine Pain Scale, Cervical Spine Outcomes Questionnaire, and Copenhagen Neck Functional Disability Scale; and (2) validity of the Bournemouth Questionnaire, Neck Pain and Disability Scale, and Neck Disability Index. The NPTF did not find low-risk-of-bias studies assessing the Visual Analogue Scale in patients with neck pain. Nevertheless, the NPTF concluded that the Visual Analogue Scale is the most cited pain measure and considered it the gold standard to measure pain intensity. Our review adds evidence for the reliability of the Visual Analogue Scale. [28]
New evidence identified in our review combined with the results of the NPTF support the validity of the Neck Disability Index (5, 8, and 10 items) questionnaire to assess disability in individuals with neck pain. Strengths and limitations Our review has several strengths. First, the search strategy was developed with a health sciences librarian and reviewed by a second librarian for accuracy and completeness.
Second, the inclusion and exclusion criteria were detailed, and independent pairs of reviewers screened and critically appraised the literature. We also contacted authors to obtain further information and clarification when necessary. Finally, our conclusions are based on the QAREL and QUADAS- 2 criteria for qualitative evaluation of study quality rather than applying an arbitrary cut-off score. This helps to minimize the risk of bias associated with using low-quality studies in our best-evidence synthesis.
Our review has limitations. First, studies may have been excluded as our literature search was restricted to the English and French languages. However, previous systematic reviews of clinical trials investigating the impact of language restriction reported that this does not lead to bias as most reviews are published in English. [49-54] Second, it is possible that our search may have missed potentially relevant studies despite our broad definition of self-reported questionnaires for activity limitations and disability.
Third, the critical appraisal of articles may vary between reviewers. This potential bias was minimized by using standardized appraisal forms, conducting critical appraisal training sessions for reviewers, and using a consensus process to determine study admissibility. The inter-rater agreement for the screening of titles and abstracts was low in our review. Possible explanations for disagreements include difficulties in identifying questionnaire language, as our criteria were only English or French questionnaires, and identifying specific psychometric properties of disability questionnaires being measured in studies (i.e. physical ability or psychological aspect).
Clinical implications and future research directions
Self-reported questionnaires evaluating pain and disability are important tools for the management of NAD. By using these in conjunction with other objective findings, clinicians may gain a more representative view of the injury and how it is truly impacting an individual. Most clinical diagnostic tests are used by clinicians to determine or rule out a cause of injury, pathology or to reproduce pain. While many clinicians may focus on the pain aspect of a disease, patient disability is a major contributing factor to the disease state. Disability is an umbrella term, encompassing impairments in body function, activity/functional limitations, and participation restrictions.
Most physical examination tests aim to understand the “body structure and function” related to disability. However, valid and reliable questionnaires must be used to measure “activity limitations” and “participation restrictions” in patients with NAD. For example, the NDI has different sections that can represent these categories. For instance, the sections pain intensity and headaches could be indicators of body function or alterations in body structure; lifting, work, and driving could represent activity; and recreation may be indicator of participation.
Further research is needed to confirm the validity and clinical utility of pain and disability self-assessment questionnaires in the assessment of NAD. Specifically, future studies should focus on phase III and IV validity studies to appropriately assess the validity in specific clinical populations (suspected to have the disease).
Conclusion
We found preliminary evidence (phase I and II validity studies) combined with the results of the NPTF to support the use of self-reported questionnaires on pain and disability to assess NAD patients. Clinicians may consider these questionnaires to complete their evaluation regarding all aspect of the symptoms (pain and disability) in NAD and WAD patients.
Appendix 1: Definition of neck pain and associated disorders
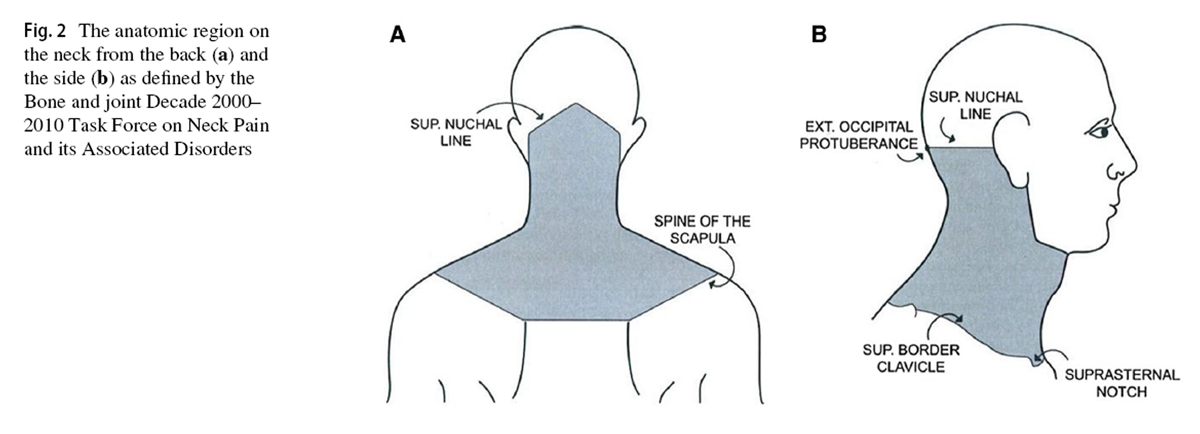
Figure 2 Neck pain is pain located in the anatomic region of the neck outlined in Figure 2 [8]
NAD includes non-traumatic neck pain and neck pain subsequent to a traffic collision (whiplash), with or without its associated disorders, which include arm pain radiating from the neck and upper thoracic pain, and/or headache, and/ or temporomandibular joint pain where they are associated with neck pain.
According to the Neck Pain Task Force [8], NAD is classified into four grades:
Grade I Pain related to low levels of disability and no or minor interference with activities of daily living. No signs or symptoms suggestive of major structural.
Grade II Pain associated with high level of disability and major interference with activities of daily living. No signs or symptoms of major structural pathology.
Grade III No signs or symptoms of major structural pathology, but presence of neurologic signs such as decreased deep tendon reflexes, weakness, and/or sensory deficits.
Grade IV Pain associated with signs or symptoms of major structural pathology, such as fracture, myelopathy, neoplasm, or systemic disease; requires prompt investigation and treatment.
The Québec Task Force Classification of Grades of Whiplash-associated Disorders. [9]
Grade I WAD Neck pain and associated symptoms in the absence of objective physical signs.
Grade II WAD Neck pain and associated symptoms in the presence of objective physical signs and without evidence of neurological involvement.
Grade III WAD Neck pain and associated symptoms with evidence of neurological involvement including decreased or absent reflexes, decreased or limited sensation, or muscular weakness.
Grade IV WAD Neck pain and associated symptoms accompanied by fracture and dislocation.
Appendix 2: Medline search strategy
1. MH “Reproducibility of Results+”
2. MH “Sensitivity and Specificity”
3. MH “Predictive Value of Tests”
4. reproducibility
5. sensitiv*
6. specificity
7. predict* n2 value*
8. reliab*
9. valid*
10. false positiv*
11. false negativ*
12. accura*
13. roc curve* or received operating characteristic*
14. kappa coefficient* or kappa co-efficient*
15. MH “Observer Variation”
16. intra-rater* or inter-rater* or interrrater* or intrarater* or rater* or intra-examiner* or inter-examiner* or intraexaminer* or interexaminer* or inter-observ* or intra-observ* or interobserv* or intraobserv*
17. utility n2 test*
18. likelihood ratio*
19. likelihood function*
20. MH “Odds Ratio”
21. odds ratio*
22. MH “Likelihood Functions”
23. MH “ROC Curve”
24. test–retest* or test* n2 re-test*
25. responsive*
26. MH “Diagnosis”
27. MH “Diagnostic Techniques and Procedures”
28. MH “Diagnostic Self Evaluation”
29. diagnos* n2 (neck* or cervical* or technique* or procedur* or evaluat*)
30. assess* n2 (neck* or cervical*)
31. evaluat* n2 (neck* or cervical*)
32. exam* n2 (neck* or cervical*)
33. procedure* n2 (neck* or cervical*)
34. screen* n2 (neck* or cervical*)
35. or/1-34
36. MH “Neck Pain”
37. MH “Neck Injuries+”
38. MH “Whiplash Injuries”
39. MH “Radiculopathy”
40. MH “Brachial Plexus Neuropathies”
41. MH “Torticollis”
42. MH “Neck Muscles”
43. MH “Cervical Vertebrae + ”
44. MH “Cervical Cord”
45. neck-pain* or “neck pain” or neck pain* or pain* n2 neck*
46. neck/shoulder pain*
47. neck* n2 injur*
48. whiplash*
49. (radiculopath* or radiating or radicular*) n2 cervical*
50. (radiculopath* or radiating or radicular*) n2 neck*
51. brachial plexus n2 neuropath*
52. torticollis*
53. cervical* n2 headache*
54. cervical* n2 pain*
55. neck* n2 ache* or neckache*
56. cervicalg*
57. cervicodyn*
58. neck* n2 (sprain* or strain*)
59. neck* n2 muscle*
60. (neck or cervical) n2 vertebr*
61. cervical axis
62. cervical cord
63. cervical disc n2 herniat* or cervical disk* n2 herniat*or (herniated dis* n2 neck*) or (herniated dis* n2 cervical*) 64. cervical* n2 stenos*
or (disk herniat* n2 neck*) or (disc herniat*
n2 cervical*) cervical disc herniation or cervical disk herniation
65. cervical* n2 spine*
66. cervical* n2 muscle*
67. cervical plexus*
68. cervical* n2 (sprain* or strain*)
69. cervical* n2 (sore* or discomfort* or dysfunction*) or neck* n2 (sore* or discomfort* or dysfunction*)
70. or/36–69
71. MH Self-report
72. MH Surveys and Questionnaires
73. MH Pain Measurement
74. MH Outcome Assessment (Health Care)
75. MH Patient Outcome Assessment
76. MH Symptom Assessment
77. Questionnaire*
78. Pain measurement*
79. Symptom assessment*
80. Outcome assessment*
81. Outcome measure*
82. Self-report*
83. Patient-report*
84. PROM
85. Self-administer*v 86. Self-assess*
87. Self-complete*
88. Self-evaluat*
89. Instrument* n2 rating
90. pain n2 (diagram* or drawing*)
91. body n2 (diagram* or drawing*)
92. Score* n2 (pain* or outcome* or NDI or SF-12 or SF-36)
93. Scale*
94. Survey*
95. Aberdeen /Spine Pain Scale*
96. Total Disability Index*
97. Bournemouth Questionnaire*
98. Cervical Spine Outcome Questionnaire*
99. Short Form-36 or Short Form-12 or sf-36 or sf-12
100. Core Outcome Measures Index*
101. Current Perceived Health-42
102. Neck Disability Index*
103. Problem Elicitation Technique*
104. Sickness Impact Profile*
105. Visual Analog Scale* or Visual Analogue Scale*
106. Whiplash Disability Questionnaire*
107. Quality-of-Life
108. Copenhagen Neck*
109. Global Assessment of Neck Pain
110. (Neck Pain*) n2 “Disability Scale”
111. Northwick Park Neck*
112. Numeric Rating Scale*
113. Patient-Specific Functional Scale*
114. Neck Functional Status Questionnaire
115. (Global Rating*) n2 “Change Scale”
116. Tampa Scale n2 Kinesiophobia
117. Functional Rating Index*
118. Health Assessment Questionnaire*
119. Wong-Baker FACES*
120. Or/71-120
121. 35 AND 70 AND 120
122. Limits ENGLISH, FRENCH
123. Limits Jan 2000-current dateAppendix 3: Validity studies classification [18]
This classification system is useful to determine the level of scrutiny to which a test has been subjected and determine its clinical utility. Diagnostic studies are classified into four phases based on the type of research question:(1) Phase I:
Do test results in patients with the target disorder differ from those in normal people?;
(2) Phase II:
Are patients with certain test results more likely to have the target disorder than patients with other test results?;
(3) Phase III:
Does the test result distinguish patients with and without the target disorder among patients in whom it is clinically reasonable to suspect that the disease is present?;
(4) Phase IV:
Do patients who undergo this diagnostic test fare better (in their health outcomes) than similar patients who are not tested? Phase I or II studies of novel tests provide preliminary evidence of clinical utility, whereas phase III or IV studies are needed to inform the validity and utility of a test in clinical practice. [18]
Appendix 4: Glossary for all the questionnaires included in our low-risk-of-bias articles
Body Pain Diagram
The Body Pain Diagram consists of an outline of the entire body from anterior and posterior views. As recommended by Margolis et al. [55], an overlay was created dividing the Body Pain Diagram into 45 anatomical regions. An electronic overlay was used to score the electronic diagrams on a desktop computer. An identical overlay (converted to a transparency) was used to score the paper diagrams. The overlay was placed over the Body Pain Diagram, and the examiner recorded a score of 1 if pain was indicated and 0 if no pain was indicated in each of the 45 regions. Pain was considered present if any portion of the region was shaded, no matter how small. Marks outside the body and marks directing the examiners’ attention to severity of the pain rather than intensity were not counted. Circled areas were treated as though the entire circle was shaded. [29]
Disabilities of Arm, Shoulder and Hand (DASH) or simplified version Quick DASH
Self-reported questionnaire conceptualizes the upper limb as a single functional unit. The DASH consists of one 30-item module assessing upper limb function and symptoms and two optional 4-item modules evaluating symptoms and function related to work and recreational activities. A 5-point Likert scale is used to score each item, which is totalled, divided by the number of responses, subtracted by one and multiplied by 25 to provide a score out of 100 (most severe disability). [56] The Quick DASH consists of 11 items derived from the DASH. [31]
Neck Disability Index (NDI)
Self-reported questionnaire assesses symptom severity and disability due to neck pain. It includes 10 items individually quoted from 0 (no disability) to 5 (maximal disability) for a total score of 50. Patients with higher scores have higher disability. [57]
Neck Pain Driving Index (NPDI)
Self-reported questionnaire includes 12 driving tasks to assess the degree of perceived driving difficulty in the chronic whiplash population. Questions could have the following answers: no difficulty (score = 0), slight difficulty (score = 1), moderate difficulty (score = 2) and great difficulty (score = 4). The total score is then translated in percentages. Higher percentages represent a higher limitation to drive. [25]
Numerical Pain Rating Scale (NPRS)
Verbal scale from 0 (no pain) to 10 (maximal pain) assesses pain intensity. [58]
Pain-DETECT Questionnaire (PD-Q)
Self-report tool consists of seven weighted sensory descriptor items, plus one item related to temporal pain characteristics and one item related to spatial pain characteristics. [59]
Profile fitness mapping neck pain
The symptom scale consists of two indices of separate aspects of symptomatology, the intensity and the frequency of the symptoms, and the functional limitation scale yields one function index. Each scale had 6 levels: (1) from 1 (never or rarely) to 6 (very often, always) for pain frequency; (2) from 7 (no pain) to 12 (maximal pain) for pain intensity; (3) from 13 (no limitation) to 18 (very difficult, impossible) for activity limitations. [23]
Patient-Specific Functional Scale (PSFS)
A functional outcome scale requires patients to list three activities that are difficult to perform as a result of their symptoms, injury, or disorder. The patient rates each activity on a 0–10 scale, with 0 representing the inability to perform the activity and 10 representing the ability to perform the activity, and they could before the onset of symptoms. The final score is determined by averaging the three activity scores. Higher scores represent a greater level of function. [36]
Visual Analogue Scale (VAS)
It measures pain intensity with a visual scale from 0 (no pain) to 10 (maximal pain). [60]
Whiplash Disability Questionnaire (WDQ)
Thirteen items measure the effect of whiplash. Each item is scored on a numerical scale from 0 (no impact) to 10 (greatest impact). The responses are summed from 0 (no disability) to 130 (complete disability). [34] As recommended by developers, missing item values were considered zeros
Acknowledgements
The authors acknowledge and thank Mrs. Sophie Despeyroux, librarian at the Haute Autorité de Santé, for her suggestions and review of the search strategy. This research was undertaken, in part, thanks to funding from the Canada Research Chairs program to Dr. Pierre Côté, Canada Research Chair in Disability Prevention and Rehabilitation at the University of Ontario Institute of Technology.
Funding
This study was funded by the Institut Franco-Européen de Chiropraxie, the Association Française de Chiropraxie and the Fondation de Recherche en Chiropraxie in France. None of these associations were involved in the collection of data, data analysis, interpretation of data, or drafting of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest
References:
Nordin M, Carragee EJ, Hogg-Johnson S, Weiner SS, Hurwitz EL, Peloso PM, et al.
Assessment of Neck Pain and Its Associated Disorders:
Results of the Bone and Joint Decade 2000–2010 Task Force on
Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S101–S122Schellingerhout JM, Verhagen AP, Heymans MW, Koes BW, de Vet HC, Terwee CB (2012)
Measurement properties of diseasespecific questionnaires in patients with neck pain: a systematic review.
Qual Life Res 21(4):659–670Lemeunier N; da Silva-Oolup S; Chow N; Southerst D; Carroll L; Wong JJ; et al..
Reliability and Validity of Clinical Tests to Assess the Anatomical Integrity of the Cervical Spine
in Adults with Neck Pain and its Associated Disorders: Part 1- A Systematic Review from the
Cervical Assessment and Diagnosis Research Evaluation (CADRE) Collaboration
European Spine Journal 2017 (Sep); 26 (9): 2225–2241Moser N, Lemeunier N, Southerst D, Shearer H, Murnaghan K, Sutton D, Cote P (2017)
Validity and Reliability of Clinical Prediction Rules used to Screen for Cervical Spine Injury
in Alert Low-risk Patients with Blunt Trauma to the Neck: Part 2. A Systematic Review
from the Cervical Assessment and Diagnosis Research Evaluation
(CADRE) Collaboration
European Spine Journal 2018 (Jun); 27 (6): 1219–1233Lemeunier N, da Silva-Oolup S, Olesen K, Carroll LJ, Shearer H, Wong JJ, et al. (2019)
Reliability and Validity of Self-reported Questionnaires to Measure Pain and Disability in Adults
with Neck Pain and its Associated Disorders: Part 3 - A Systematic Review From the CADRE Collaboration
European Spine Journal 2019 (May); 28 (5): 1156–1179Lemeunier N, Jeoun EB, Suri M, Tuff T, Shearer H, Mior S, Wong JJ, da Silva-Oolup S, et al, (2018)
Reliability and Validity of Clinical Tests to Assess Posture, Pain Location, and Cervical Spine
Mobility in Adults with Neck Pain and its Associated Disorders: Part 4. A Systematic Review
from the Cervical Assessment and Diagnosis Research Evaluation (CADRE) Collaboration
Musculoskeletal Science & Practice 2018 (Dec); 38: 128–147Lemeunier N, Suri M, Welsh P, Shearer H, Nordin M, Wong, JJ, Torres, da Silva-Oolup S (2017)
Reliability and Validity of Clinical Tests to Assess the Function of the Cervical Spine in Adults with
Neck Pain and its Associated Disorders: Part 5. A Systematic Review from the Cervical Assessment
and Diagnosis Research Evaluation (CADRE) Collaboration
European Journal of Physiotherapy 2019 (Jul 8); 1–32Guzman J, Hurwitz EL, Carroll LJ et al (2010)
A New Conceptual Model Of Neck Pain: Linking Onset, Course, And Care
lts of the Bone and Joint Decade 2000–2010 Task Force on
Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S14–23Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Holbrook A.
Self-reported measure. Encyclopedia of survey research methods.
http://srmo.sagep ub.com/view/encyc loped iaof-surve y-resea rch-metho ds/n523.xmlJarvis M, Russel J.
Chapter 4—Research methods.
In: Broché (ed) Exploring psychology: AS student book for AQA A,
Broché Editions, p 91Haywood KL (2006)
Patient-reported outcome I: measuring what matters in musculoskeletal care.
Musculoskelet Care 4(4):187–203Bonica J (1979)
The need of a taxonomy.
Pain 6(3):247–248World Health Organization (2016)
World Health Organization [internet].
World Health Organization, Geneva, Switzerland.
Disabilities; 2016 [cited 4 Oct 2016].
http://www.who.int/topic s/disabilities/en/Fletcher RH, Fletcher SW, Fletcher GS (2012)
Clinical epidemiology: the essentials, 5th edn.
Lippincott Williams & Wilkins, PhiladelphiaLucas N, Macaskill P, Irwig L, Moran R, Rickards L, Turner R, Bogduk N (2013)
The reliability of a quality appraisal tool for studies of diagnostic reliability (QAREL).
BMC Med Res Methodol 13:111Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. (2011)
QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies.
Ann Intern Med 155(8):529–536Sackett DL, Haynes RB (2002)
The architecture of diagnostic research.
BMJ 324(7336):539–541Slavin RE (1995)
Best evidence synthesis: an intelligent alternative to meta-analysis.
J Clin Epidemiol 48(1):9–18Viera AJ, Garrett JM (2005)
Understanding interobserver agreement: the kappa statistic.
Fam Med 37(5):360–363Moher D, Liberati A, Tetzlaff J, Altman DG, Grp P (2009)
Preferred Reporting Items for Systematic Reviews
and Meta-Analyses: The PRISMA Statement
PLoS Medicine 2009 (Jul 21); 6 (7): e1000100Bossuyt PM, Reitsma JB, Bruns DE et al (2003)
Toward complete and accurate reporting of studies diagnostic accuracy: the STARD initiative.
Am J Clin Pathol 119:18–22Björklund M, Hamberg J, Heiden M, Barnekow-Bergkvist M (2012)
The ProFitMap-neck—reliability and validity of a questionnaire for measuring symptoms and
functional limitations in neck pain.
Disabil Rehabil 34(13):1096–1107Stupar M, Côté P, Beaton DE, Boyle E, Cassidy JD (2015)
A test–retest reliability study of the whiplash disability questionnaire in patients with acute
whiplash-associated disorders.
J Manip Physiol Ther 38:629–636Takasaki H, Johnston V, Treleaven JM, Jull GA (2012)
The Neck Pain Driving Index (NPDI) for chronic whiplash-associated disorders:
development, reliability, and validity assessment.
Spine J 12:912–920Walton DM, MacDermid JC (2013)
A brief 5-item version of the Neck Disability Index shows good psychometric properties.
Health Qual Life Outcomes 11:108Young BA, Walker MJ, Strunce JB, Boyles RE, Whitman JM, Childs JD (2009)
Responsiveness of the Neck Disability Index in patients with mechanical neck disorders.
Spine J 9:802–808Prushansky T, Handelzalts S, Pevzner E (2007)
Reproducibility of pressure pain threshold and visual analog scale findings in chronic whiplash patients.
Clin J Pain 23(4):339–345Southerst D, Stupar M, Côté P, Mior S, Stern P (2013)
The reliability of measuring pain distribution and location using body pain diagrams in patients with acute
whiplash-associated disorders.
National University of Health Sciences, Lombard, pp 395–402Cleland JA, Childs JD, Whitman JM (2008)
Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients
with mechanical neck pain.
Arch Phys Med Rehabil 89(1):69–74Mehta SH, Macdermid JC, Carlesso LC, McPhee C (2010)
Concurrent validation of the DASH and the QuickDASH in comparison to neck-specific scales
in patients with neck pain.
Spine 35(24):2150–2156Pink J, Petrou S, Williamson E, Williams M, Lamb SE (2014)
Properties of patient-reported outcome measures in individuals following acute whiplash injury.
Health Qual Life Outcomes 12(1):1See KS, Treleaven J (2015)
Identifying upper limb disability in patients with persistent whiplash.
Man Ther 20(3):487–493Stupar M, Côté P, Beaton DE, Boyle E, Cassidy JD (2015)
Structural and construct validity of the Whiplash Disability Questionnaire in adults
with acute whiplash-associated disorders.
Spine J 15(11):2369–2377van der Velde G, Beaton D, Hogg-Johnston S, Hurwitz E, Tennant A (2009)
Rasch analysis provides new insights into the measurement properties of the neck disability index.
Arthritis Care Res 61(4):544–551Young IA, Cleland JA, Michener LA, Brown C (2010)
Reliability, construct validity, and responsiveness of the neck disability index, patient-specific
functional scale, and numeric pain rating scale in patients with cervical radiculopathy.
Am J Phys Med Rehabil 89(10):831–839Bolton JE, Humphreys BK, Van Hedel HJA (2010)
Validity of weekly recall ratings of average pain intensity in neck pain patients.
J Manip Physiol Ther 33(8):612–617Tampin B, Briffa NK, Slater H (2013)
Self-reported sensory descriptors are associated with quantitative sensory testing parameters in patients
with cervical radiculopathy, but not in patients with fibromyalgia.
Eur J Pain (UK) 17(4):621–633Ferrari R, Russell A, Kelly AJ (2006)
Assessing whiplash recovery— the Whiplash Disability Questionnaire.
Aust Fam Physician 35(8):653–654Barbero M, Moresi F, Leoni D, Gatti R, Egloff M, Falla G (2015)
Test–retest reliability of pain extent and pain location using a novel method for pain drawing analysis.
Eur J Pain 19:1129–1138Hayashi K, Arai YC, Morimoto A, Aono S, Yoshimoto T, Nishihara M, et al. (2015)
Associations between pain drawing and psychological characteristics of different body region pains.
Pain Pract 15(4):300–307Odole AC, Adegoke BO, Akomas NC (2011)
Validity and test retest reliability of the neck disability index in the Nigerian clinical setting.
Afr J Med Med Sci 40(2):135–138Provenzano DA, Fanciullo GJ, Jamison RN, McHugo GJ, Baird JC (2007)
Computer assessment and diagnostic classification of chronic pain patients.
Pain Med 8(suppl 3):S167–S175Çakit BD, Genç H, Altuntas V, Erdem HR (2009)
Disability and related factors in patients with chronic cervical myofascial pain.
Clin Rheumatol 28(6):647–654En MC, Clair DA, Edmondston SJ (2009)
Validity of the Neck Disability Index and Neck Pain and Disability Scale for measuring disability
associated with chronic, non-traumatic neck pain.
Man Ther 14(4):433–438Forestier R, Françon A, Saint Arroman F, Bertolino C (2007)
French version of the Copenhagen neck functional disability scale.
Jt Bone Spine 74(2):155–159Malik AA, Robinson S, Khan WS, Dillon B, Lovell ME (2017)
Assessment of range of movement, pain and disability following a whiplash injury.
Open Orthop J 11:541–545Gabel A, Cuesta-Vargas Barr S, Winkeljohn Black S, Osborne JW, et al. (2016)
Confirmatory factor analysis of the neckdisability index, comparing patients with whiplash
associated disorders to a control group with non-specific neck pain.
Eur Spine J 8:2078–2086Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL et al (2010)
The COSMIN checklist for assessing the methodological quality of studies on measurement properties
of health status measurement instruments: An international Delphi study.
Qual Life Res 19(4):539–549Juni P, Holenstein F, Sterne J et al (2002)
Direction and impact of language bias in meta-analyses of controlled trials: empirical study.
Int J Epidemiol 31:115–123Moher D, Fortin P, Jadad AR et al (1996)
Completeness of reporting of trials published in languages other than English:
implications for conduct and reporting of systematic reviews.
Lancet 347:363–366Moher D, Pham B, Lawson ML et al (2003)
The inclusion of reports of randomised trials published in languages other than English
in systematic reviews.
Health Technol Assess 7:1–90Morrison A, Polisena J, Husereau D et al (2012)
The effect of English- language restriction on systematic review-based metaanalyses:
a systematic review of empirical studies.
Int J Technol Assess Health Care 28:138–144Sutton AJ, Duval SJ, Tweedie RL et al (2000)
Empirical assessment of effect of publication bias on meta-analyses.
BMJ 320:1574–1577Margolis RB, Chibnall JT, Tait RC (1998)
Test–retest reliability of the pain drawing instrument.
Pain 33:49–51Hudak PL, Amadio PC, Bombardier C, Beaton D, Cole D, Davis A et al (1996)
Development of an upper extremity outcome measure: the DASH.
Am J Ind Med 30:372Vernon H, Mior S.
The Neck Disability Index: A Study of Reliability and Validity
J Manipulative Physiol Ther 1991 (Sep); 14 (7): 409–415Bijur PE, Latimer CT, Gallagher EJ (2003)
Validation of a verbally administered numerical rating scale of acute pain for use
in the emergency department.
Acad Emerg Med 10:390–392Freynhagen R, Baron R, Gockel U, Tölle TR (2006)
Pain-DETECT: a new screening questionnaire to identify neuropathic components in patients with back pain.
Curr Med Res Opin 22:1911–1920Carlsson AM (1983)
Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogic scale.
Pain 16:87–101Pinfold M, Niere KR, O’Leary EF, Hoving JL, Green S, Buchbinder R (2004)
Validity and internal consistency of a chiplashspecific disability measure.
Spine 29:263–268
Return to SPINAL PALPATION
Since 3-16-2020


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |