Spinal Manipulation Therapy: Is It All About the Brain?
A Current Review of the Neurophysiological Effects of ManipulationThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Integrative Medicine 2019 (Sep); 17 (5): 328–337 ~ FULL TEXT
OPEN ACCESS Giles Gyer, Jimmy Michael, James Inklebarger, Jaya Shanker Tedla
The London College of Osteopathic Medicine,
London NW1 6QH, United Kingdom.
info@osteon.co.ukSpinal manipulation has been an effective intervention for the management of various musculoskeletal disorders. However, the mechanisms underlying the pain modulatory effects of spinal manipulation remain elusive. Although both biomechanical and neurophysiological phenomena have been thought to play a role in the observed clinical effects of spinal manipulation, a growing number of recent studies have indicated peripheral, spinal and supraspinal mechanisms of manipulation and suggested that the improved clinical outcomes are largely of neurophysiological origin.
In this article, we reviewed the relevance of various neurophysiological theories with respect to the findings of mechanistic studies that demonstrated neural responses following spinal manipulation. This article also discussed whether these neural responses are associated with the possible neurophysiological mechanisms of spinal manipulation. The body of literature reviewed herein suggested some clear neurophysiological changes following spinal manipulation, which include neural plastic changes, alteration in motor neuron excitability, increase in cortical drive and many more. However, the clinical relevance of these changes in relation to the mechanisms that underlie the effectiveness of spinal manipulation is still unclear. In addition, there were some major methodological flaws in many of the reviewed studies. Future mechanistic studies should have an appropriate study design and methodology and should plan for a long-term follow-up in order to determine the clinical significance of the neural responses evoked following spinal manipulation.
KEYWORDS: Complementary therapies; Occupational injuries; Occupational therapists; Physical therapists; Public health
From the FULL TEXT Article:
Introduction
Spinal manipulation is a specialized form of manual therapy that uses non-invasive, “handson” treatment techniques to treat musculoskeletal pain and disability. The therapy has proven to be an effective treatment option for the management of various musculoskeletal disorders and is practiced worldwide by health-care practitioners from various specialities, including osteopaths, chiropractors, naturopathic physicians and physiotherapists. However, little is yet understood about the physiological mechanisms of this therapy, especially how it exerts its pain modulatory effects. Over the past decade, many theories have been proposed to explain the mechanisms of spinal manipulation [1–4], but the available data from mechanistic studies are insufficient to clarify the short- or long-term clinical outcomes of manipulation.
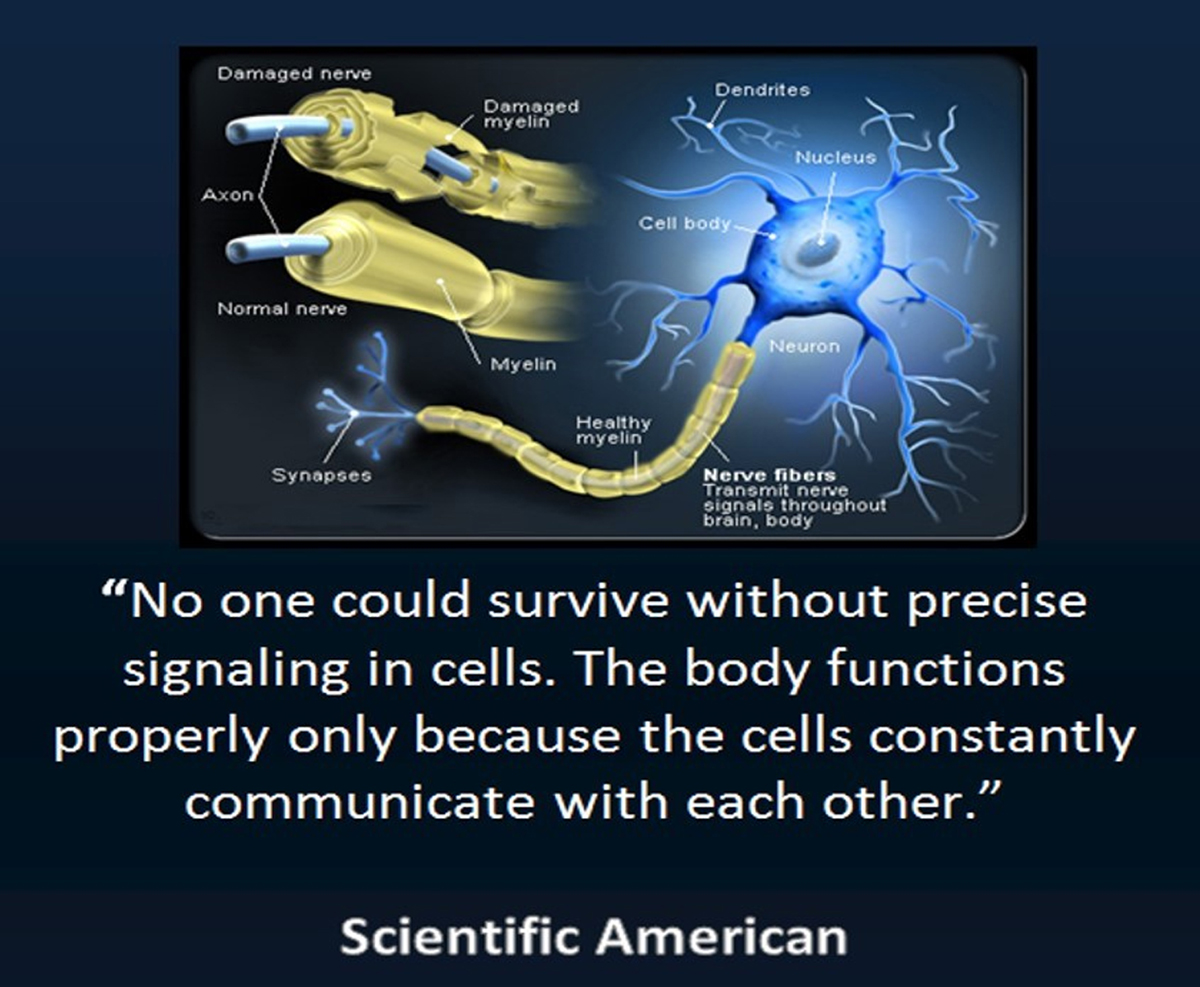
Most of the early theories proposed to explain the analgesic and hypoalgesic effects of spinal manipulation were heavily focused on the biomechanical changes following the intervention [1–3]. In recent years, however, there has been a paradigm shift towards a neurophysiological mechanism of spinal manipulation, as an increasing number of recent studies have reported various neural effects of spinal manipulation such as changes in somatosensory processing, muscle-reflexogenic responses, central motor excitability, motor neurone activity, neuroplastic brain changes, Hoffmann reflex (H-reflex) responses, sympathetic activity and central sensitisation [5–11]. These studies have suggested a cascade of neurochemical responses in the central and peripheral nervous system following spinal manipulation. Hence, it has been hypothesised that the observed pain modulatory effects of spinal manipulation are largely due to neurophysiological mechanisms mediated by peripheral, spinal and supraspinal structures. These mechanisms have been thought to be triggered by mechanical stimulus or biomechanical forces applied during the manipulative act.
To date, Pickar [5] is the only one that provided a theoretical framework for the neurophysiological effects of spinal manipulation. Although Bialosky et al. [12] later proposed a comprehensive model and a new framework to visualise potential individual mechanisms associated with pain reduction, their work was based on different forms of manual therapy and not exclusive to spinal manipulation alone. Hence, there has been a need for a comprehensive review that presents an updated framework based on the current knowledge and understanding of the neurophysiological effects of spinal manipulation. On the other hand, over the last decade, a growing number of mechanistic studies have been conducted to understand the neurophysiological mechanisms of spinal manipulation. These studies have demonstrated various neural responses following manipulation. However, no review has been written to evaluate the relevance of these findings regarding the proposed theories as well as the observed clinical effects. Therefore, the purpose of this article is to examine all the recent findings on the neurophysiological effects of spinal manipulation and review their relevance with respect to the improved clinical outcomes of spinal manipulation.
Relationship between biomechanical changes and
neurophysiological responses to spinal manipulation
The clinical effects of spinal manipulation are thought to be mediated by biomechanical and/or neurophysiological mechanisms. However, the exact mechanism through which spinal manipulation exerts pain modulatory effects, influences tissue repair and healing, and restores functional ability has remained a mystery. Over the past decades, numerous hypotheses have been offered to explain these mechanisms, but evidence to support these theories is still limited. The evidence to date suggests that the effects of spinal manipulation are beyond biomechanical changes; in fact, a cascade of neurophysiological mechanisms may be initiated [13]. Biomechanical changes that occur due to spinal manipulation are thought to be produced by vertebral movement. The high-velocity thrust introduced at the vertebral level during spinal manipulation mobilizes the vertebrae on one another and is presumed to alter segmental biomechanics. In addition, the produced vertebral movement is known to be complex, as several adjacent vertebral levels are mobilized simultaneously [3, 4].
There are four main theories of biomechanical changes elicited by spinal manipulation. These include(1) release of entrapped synovial folds or meniscoids;
(2) restoration of buckled motion segments;
(3) reduction of articular or periarticular adhesions; and
(4) normalisation of “hypertonic” muscle by reflexogenic effect [2].However, the relevance of these theories to clinical outcomes remains uncertain. Although several studies have quantified motion with spinal manipulation, biomechanical effects were found to be transient in nature [14–17] and no credible evidence has yet been found in support of a lasting positional change [18]. So far, only the muscular reflexogenic theory has some plausible evidence in support of its mechanical explanation [8, 19, 20]; nevertheless, the clinical assertion that hypertonic muscles are influenced by an increased stretch reflex gain is not proven yet [21].
Furthermore, successful outcomes of spinal manipulation are commonly attributed to biomechanical dynamic changes, specifically corrections to position and movement faults that can be detected in palpatory examination. However, acceptance of this explanation has been controversial. This is because palpation has not been established as a reliable indicator of spinal abnormalities, due to poor inter-rater agreement. Some studies even suggested it as an unreliable procedure to identify areas requiring spinal manipulation [22, 23]. In addition, the thrust applied during a therapeutic manipulation may not be specific to an intended location [24] and can vary among practitioners [25]. However, systematic reviews done to assess the quality of literature have found significant statistical and methodological shortcomings in most studies [26, 27]. In fact, some later studies have shown comparatively higher inter-rater reliability than previous literature [28–31].
Cooperstein and Young [32] noted that in most of the earlier studies, the confidence level of examiners and degrees of spinal stiffness were not taken into consideration, which resulted in lower reliability scores. The success of spinal manipulation in treating musculoskeletal disorders, despite theoretical inconsistencies in its supposed biomechanical mechanisms, indicates the possibility of concurrent additional mechanisms. Biomechanical changes evoked as a result of spinal manipulation may induce neurophysiological responses by influencing the inflow of sensory input to the central nervous system (CNS) [5]. Moreover, the mechanical force applied during spinal manipulation could either stimulate or silence mechanosensitive and nociceptive afferent fibers in paraspinal tissues, including skin, muscles, disk, facet joints, tendons and ligaments [8, 10]. These inputs are thought to stimulate pain-processing mechanisms and other physiological systems connected to the nervous system [4, 5, 11, 12, 18, 20]. In support of this hypothesis, Pickar and Bolton [33] developed the notion that neural responses arising from the nervous system due to mechanical stimuli might be due to alterations in peripheral sensory input from paraspinal tissues.
Taken together, it can be said that changes in spinal biomechanics trigger the chain of neurophysiological responses that effects the therapeutic outcomes associated with spinal manipulation, and there is a potential for combined biomechanical and neurophysiological effects following spinal manipulation. However, the possible interaction of these effects has frequently been overlooked in the current literature. The possibility of a combined effect is important to consider, as biomechanical characteristics of spinal manipulations are shown to have a unique dose-response relationship with biomechanical, neuromuscular and neurophysiological responses [25, 34, 35].
For example, paraspinal electromyographic (EMG) responses have an apparent dependence on the force-time characteristics of the mechanical thrust applied during spinal manipulation [14]. Therefore, future clinical studies should investigate the relationship between variations in mechanical parameters (e.g., preload, peak force and thrust) and physiological responses and the correlations among various parameters and biological and therapeutic outcomes.
Neurophysiological effects of spinal manipulation
Many authors have long postulated that spinal manipulation exerts its therapeutic effects through several neurophysiological mechanisms working on their own or in combination [5, 12, 18]. These mechanisms involve complex interactions between the peripheral nervous system and the CNS and are thought to be activated when spinal manipulation stimulates paraspinal sensory afferents [33]. The activation of sensory neurons is presumed to occur either during the maneuver itself and/or because of changes in spinal biomechanics. These paraspinal sensory inputs are assumed to alter neural integration either by directly influencing reflex activity or by affecting central neural integration within motor, nociceptive and possibly autonomic neuronal pools [5]. However, current biomechanical studies of spinal manipulation are unable to observe the changes occurring in the brain following the therapy. Thus, the validity and relevance of theorised neurophysiological mechanisms in relation to therapeutic outcomes remain unclear. Implications for specific neural mechanisms of manipulation are suggested from associated neurophysiological responses, which have been observed in mechanistic studies.
Over the past decades, a number of specific and nonspecific neural effects of spinal manipulation have been reported, including increased afferent discharge [33], central motor excitability [5], alterations in pain processing [7], reduction of temporal summation [10], stimulation of autonomic nervous system (ANS) [6], lessening of pain perception [36] and many more. These neural responses collectively implicate mechanisms mediated by the nervous system. Fig. 1 presents a new theoretical model that illustrates proposed neurophysiological effects of spinal manipulation based on the findings of current mechanistic literature. This model is heavily inspired from the comprehensive model.
Neuromuscular effects
Muscle activation
The muscular reflexogenic response is an important theory that is frequently used to explain the mechanism of spinal manipulation. The muscles of the human body have some reflex responses, by means of their reflex arcs, to protect themselves from potentially harmful force [1]. In manual therapy literature, the reflexogenic effect is often explained using one of the prominent theories of pain, the pain-spasm-pain cycle [37], which suggests that pain causes muscular hyperactivity (spasm) and muscle spasm reflexively produces pain, establishing a self-perpetuating cycle. Although this pain model lacks unequivocal support from the literature [38], it is known that low back pain (LBP) patients experience significantly higher levels of paraspinal muscle activity than normal healthy individuals during static postures [39–41]. Spinal manipulation is thought to disrupt the pain-spasm-pain cycle by reducing muscle activity through reflex pathways. Pickar [5] postulated that the mechanical stimulation of paraspinal tissues from manipulation might cause the sensory receptors to inhibit muscle activity and suggested that afferent stimuli would target this inhibition as a reflex response. Herzog [42] proposed that the neuromuscular response to spinal manipulation could involve two reflex pathways, the capsule mechanoreceptor pathway and the muscle spindle pathway, and that these pathways might differentiate by muscle activity onset delay.
EMG signals are commonly used to quantify changes in muscle activation following spinal manipulation. Amplitude and timing of EMG signals are the two aspects that quantify muscle activity changes [8]. Experimental studies assessing neuromuscular responses to spinal manipulation found both increases and decreases in EMG amplitude following manipulation [43–46]. Note that most authors, including Lehman and McGill [45] reported a reduction of paraspinal muscle activity in the resting phase following manipulation. The conflicting results, however, appeared when EMG amplitudes were analysed during dynamic activity (flexion or extension). Nevertheless, most of the high-quality experiments published to date reported reduced paraspinal voluntary EMG amplitude during extension and relaxation phases [44]. The changes in EMG amplitude in response to manipulation indicate that the underlying mechanism of spinal manipulation may involve the disruption of pain-spasm-pain model.
The timing of the EMG signal is another measure of the muscle activity changes. Muscle activity onset delay quantifies the reflex response of a given spinal manipulation. Onset delay of a muscle following manipulation varies widely, from 1 to 400 ms, but is still relatively short [8, 47, 48]; thus, it is unlikely to be activated voluntarily [42]. On the other hand, because a spinal reflex is assumed to take place within 120 ms [49], there is a high likelihood that a spinal reflex response may be involved with the muscle activity onset delay. Furthermore, in a recent study, Currie et al. [8] quantified differences in muscle activity onset delay between symptomatic and asymptomatic participants, following lumbar manipulation, and found that those with LBP (symptomatic) had longer onset delays than their healthy (asymptomatic) counterparts, although the difference in timing was only 5 ms. The authors suggested that the delayed neuromuscular response after spinal manipulation, in the symptomatic group, might be due to the involvement of capsule mechanoreceptor pathways. In support of this claim, they cited Herzog’s [42] work, where the author anticipated faster activation of muscle spindle pathways than capsular reflex pathways because of their reliance on large-diameter Ia afferents.
More recently, after investigating the soleus-evoked V-wave, H-reflex and maximum voluntary contraction (MVC) signals of the plantar flexors, some recent studies performed on different patient populations have provided further evidence in support of the above assumption. A randomized controlled crossover trial conducted to evaluate the effect of a single-session spinal manipulation on 11 elite Taekwondo athletes has reported an increase in muscle strength and cortical drive [50]. Niazi et al. [51] also reported similar findings, but on a symptomatic population, 10 patients with spinal dysfunction. The authors suggested that spinal manipulation leads to neural plastic changes, altering the net excitability of the lowthreshold motor units, changing the synaptic efficacy of the Ia synapse and increasing corticospinal excitability. The modulation of neural plasticity by spinal manipulation is also supported in the work of Holt et al. [52]. After performing a randomised trial on 12 chronic stroke patients, they concluded that the increase in muscle strength might be modulated from a supraspinal level.
From the above discussion, it is evident that spinal manipulation results in neuromuscular responses, involves spinal reflex pathways and may reduce muscle hyperactivity. However, it is not yet clear whether the evoked short-latency changes in EMG, V-wave, H-reflex and MVC signals following manipulation indicate a clinically significant outcome or merely a short-term effect.
Modulation of γ motor neuron activity
Korr’s theory of the facilitated segment [53] is a decades-old theory that has been used to interpret the mechanism of manipulation. From the early evidential basis, Korr [53] hypothesised that a painful segment has a facilitatory response and proposed that an increase in γ motor neuron activity could lead to muscle hypertonicity by reflexively facilitating the α motor neuronal hyperexcitability. The author suggested that spinal manipulation could calm the excited γ motor neurons by increasing joint mobility and producing a barrage of proprioceptive afferent impulses. However, one major limitation of Korr’s theory is that it lacks the neural pathways (i.e., afferent input likely to arise and reflex pathways that may be activated due to spinal manipulation) for its proposed mechanism of action. Interestingly, the pain-spasm-pain cycle [37] sheds some light on the neural pathway that may be involved in the γ motor neuron excitability. Johansson and Sojka [54] proposed that this neural pathway would involve a hyperactive spinal stretch reflex, which is a process that involves skeletal muscle contraction and is thought to occur when the muscle spindles and Ia afferents are activated due to stretching of the muscle [55]. Johansson and Sojka [54] postulated that nociceptive afferents directly project on the γ motor neurons, which react by increasing the output of muscle spindles and allowing the associated afferent nerves to signal changes in muscle length. This in turn results in hyperexcitability of α motor neurons and subsequently leads to increased muscle activation.
As stated before, the pain-spasm-pain model is not unequivocally supported in the literature. Several authors have suggested that the sensitivity of muscle spindles is not affected by LBP or paraspinal tissues do not undergo noxious stimulation [56, 57]. However, some authors supported the concept that spinal manipulation disrupts the pain-spasm-pain cycle and works by decreasing the hyperactivity of underlying nociceptors and consequently, leads to stretch reflex attenuation and subsequent reduction in muscle activation [3, 33, 42]. Recently, two novel studies have established that with spinal manipulation, corticospinal or stretch reflex excitability can be attenuated. In the first study done to quantify the effects of spinal manipulation on stretch reflex excitability, Clark et al. [20] observed an attenuation of stretch reflex of the erector spinae muscles when spinal manipulation produced an audible cracking sound. The authors suggested that manipulation might mechanistically act to reduce the output of muscle spindles and other segmental sites in the Ia reflex pathway. The second study was conducted by Fryer and Pearce [58] on asymptomatic participants. The authors demonstrated a significant reduction in corticospinal and spinal reflex excitability following HVLAT manipulation that produced an audible cavitation. They also suggested that considerable alterations in corticospinal excitability could lead to changes in motor recruitment strategies.
These findings provide more insight into the possible segmental mechanisms of spinal manipulation. In addition, because an increased stretch reflex gain forms the basis of one of the neural pathways of the pain-spasm-pain cycle, it can be said that spinal manipulation may function via the pain model by attenuating stretch reflex hyperactivity and consequently reducing the hyperexcitability of γ motor neurons.
Modulation of α motor neuron activity
The involvement of α motor neurons in the modulation of musculoskeletal pain has been proposed by two of the prominent theories of pain: (1) the pain-spasm-pain cycle [37] and (2) the pain-adaptation model [59]. The pain-spasm-pain model proposes two distinct neural pathways that contribute to pain. However, both theories have one common basis that hyperexcitability of the α motor neuron pool leads to increased muscle activity. One neural pathway is described above (see 4.2. Modulation of γ motor neuron activity). Another pathway involves the projections of nociceptors onto α motor neurons via excitatory interneurons. On the other hand, the pain-adaptation model postulates that pain increases muscle activity when the muscle acts as antagonist but decreases it when acting as an agonist. The neural pathway proposed for this model involves feedback of nociceptive afferents projecting onto α motor neurons via both excitatory and inhibitory interneurons. The CNS is thought to control the function of these interneurons and provide motor command of whether to excite or inhibit the α-motoneuronal pool [38]. In short, regardless of the exact neural pathways, it may be said that the α motor neuron excitability forms the basis in the mechanism of musculoskeletal pain, as the modulation of α motor neurons correlates with changes in muscle activation.
Spinal manipulation has been thought to relax or normalise hypertonic muscle through modulating α motor neuron activity. However, the exact effect of manipulation on motor neurons is still unknown. As described above (see 4.1. Muscle activation), most of the higherquality EMG studies have demonstrated a significant attenuation of muscle activity, following manipulation, during forward bend or lying prone position [44]. In a recent study on LBP patients, after observing reductions in EMG muscle activity during the flexionrelaxation phase, Bicalho et al. [43] suggested that such decreases in EMG amplitude might be due to two different scenarios: (1) the hyperexcitability of α-motoneuronal pool was decreased following spinal manipulation or (2) manipulation increased the inhibition of the α motor unit. More recently, using surface and intramuscular fine wire electrodes, Haavik et al. [60] recorded EMG of the tibialis anterior muscle to analyse cortical silent periods. The authors reported an increase in low-threshold motor neuron excitability in the lower-limb muscle with spinal manipulation, compared to control. Nevertheless, the clinical relevance of EMG amplitude changes to the motor neuron pool is unclear, as EMG muscle activity changes were found to be transient in nature and several studies have reported conflicting results.
Two experimental techniques that have been used to effectively measure the motor neuron activity after mechanical stimulation include the H-reflex and the transcranial magnetic stimulation (TMS). The H-reflex technique assesses the spinal reflex pathways that project onto the target muscle, bypassing the muscle spindle. It reveals an estimate of changes to α motor neuron excitability following spinal manipulation [61]. In contrast, the TMS technique uses changing magnetic fields to measure the corticospinal tract excitability between the motor cortex and targeted muscle. It reveals the alterations in the motor cortex excitability after manipulation. When the motor cortex is stimulated utilising TMS, motor-evoked potentials (MEPs) are elicited. MEPs are used to measure the excitability of involved corticospinal motor pathways. Changes in MEPs could be an indication of alterations in preupper motor neuron excitability, lower motor neuron excitability, the neuromuscular junction or anywhere in between [62].
The study of Murphy et al. [63] is probably the first study that reported a significant decrease in H-reflex amplitude following spinal manipulation. A series of later studies conducted by Dishman et al. [64–68] have consistently reported a significant but temporary attenuation of α-motoneuronal excitability after spinal manipulation using H-reflexes. These studies, however, could be subjected to several methodological shortcomings including a lack of intervention control group, single H-reflex-based analysis, and no methodological relevance with relevant neurophysiology literature. Moreover, the findings of Dishman et al. were contrasted by Suter et al. [69], who, after observing no alteration in H-reflexes in a subgroup, argued that the decreases in the H-reflex could be due to movement artifact during manipulation. In contrast, Fryer and Pearce [58] supported the findings of Dishman et al. but opposed the Suter et al.’s conclusion. They reported that inhibition of H-reflexes was not associated with a movement artifact, as the control group showed no significant changes when undergoing the same repositioning of the intervention group. In a recent cross-sectional study that included both asymptomatic healthy volunteers and subacute LBP patients, Dishman et al. [70] again reported suppression of the Ia afferent α-motoneuronal pathway and a valid and reliable attenuation of the Hmax/Mmax ratio following spinal manipulation, which was beyond movement or position artifacts. More recently, while Niazi et al. [51] reported a significantly reduced H-reflex threshold with spinal manipulation, two studies with randomised controlled crossover designs have reported no significant changes in H-reflex threshold between the control and manipulation groups [50, 52]. Taken together, it can be said that the findings of manipulation studies published to date on H-reflex changes are largely inconsistent.
Over the past decades, changes in MEPs following spinal manipulation have been examined by only a few researchers and they reported conflicting results. While Dishman et al. [71, 72] reported a transient but significant increase in MEPs after manipulation, Clark et al. [20] found a slight decrease, but no significant decrease in the amplitude of erector spinae MEP. In contrast, Fryer and Pearce [58] observed a significant reduction in MEP amplitudes following manipulation. Note that Fryer and Pearce followed an established protocol to measure MEPs and recorded amplitudes roughly 10 min after the intervention, and thus the authors speculated that a transient facilitation of MEPs might have occurred at the beginning. However, although Dishman et al. [71, 72] observed changes in MEPs returned to baseline 30–60 s following manipulation, their work had several methodological flaws. More recently, Haavik et al. [73], with a methodologically sound study design, reported an increase in maximum motor evoked potential for both upper and lower limb muscle following spinal manipulation. Nevertheless, such conflicting data do not establish the clinical relevance of spinal manipulation-induced changes in corticospinal tract excitability.
Thus, although spinal manipulation has been reported to result in significant changes in Hreflexes and EMG amplitudes, yet, the clinical relevance of such short-lived changes to the motor neuron pool is unknown, and there is no consensus on the mechanisms that underlie the effectiveness of spinal manipulation.
Autonomic responses
The ANS acts largely unconsciously and controls involuntary responses that maintain the body’s internal environment. It regulates several body processes (e.g., heart rate, respiratory rate, sweat and salivary secretion, blood pressure and pupillary response) and innervates various internal organs that have smooth muscle (e.g., heart, lungs, pupils, salivary, liver, kidneys, bladder and digestive glands). The system is regulated from the hypothalamus portion of the brain and is also in control of the underlying mechanisms during a fight-orflight response [74]. The ANS also has potential interactions with the nociceptive (pain) system on multiple levels, which include the brain stem, fore brain, periphery and dorsal horn [75]. Hence, any intervention that influences the functions of the ANS may have significant implications, as this may provide important mechanistic information and even shed some light on the possible neurophysiological mechanisms of that intervention.
In the manual therapy literature, autonomically mediated responses following spinal manipulation have been well established. A variety of outcome measures have been used to determine ANS activity after manipulation, including skin blood flow (SBF) indexes, blood pressure changes, pupillary reflex and heart rate variability (HRV). Studies performed to assess short-term changes in SBF following manipulation suggested a sympatho-excitatory effect, though this effect might be challenged because of overlooked local endothelial mechanisms regulating SBF [76]. Comparison of blood pressure changes pre- and postmanipulation has demonstrated ANS involvement [77, 78]. Pupillary reflex is also reported as an indicator of ANS activity [79]. HRV is another well-established marker of cardiac autonomic neural activity and reflects whether the sympathetic or parasympathetic branch of the ANS is influenced [77]. Therefore, it has been presumed that the effects of spinal manipulation on the ANS might lead to opioid independent analgesia, influencing the reflex neural outputs on the segmental and extra-segmental levels [6].
Significance of ANS changes following manipulation
Anatomically, the two complementary parts of the ANS include the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The interaction between these systems is known to influence the stress response of tissues [80]. The SNS plays an active role in mediating the fight-or-flight response and serves as a medium for the efferent communication between the immune system and the CNS. It releases catecholamine as an end product, which modulates several immune parameters during acute and chronic inflammation [81, 82]. The mediating role of SNS between somatic and supportive processes has been demonstrated in Korr’s pioneering work [83]. In addition, it has also been found that musculoskeletal abnormalities are associated with alterations in cutaneous patterns of sympathetic activity [84]. In the manual therapy literature, this modulatory effect of the SNS on inflammation has been of special interest, as it may explain some of the neurophysiological effects observed after spinal manipulation. Hence, in the proposed physiological mechanisms of spinal manipulation, a prominent role of the peripheral SNS (PSNS) in the modulation of pain and inflammation has been theorised by both Pickar [5] and Bialosky et al. [12].
Over the past decades, a number of studies have investigated the effects of spinal manipulation on SNS. While some studies have reported immediate activation of the SNS following spinal manipulation [76–78, 85], others reported no change in sympathetic activity [73–76, 79]. Welch and Boone [78] suggested that the autonomic responses observed after manipulation might vary based upon the specific segment(s) of the spine manipulated. The authors concluded that sympathetic responses are likely to be elicited from thoracic/lumbar manipulation, while parasympathetic responses might result from cervical spine manipulation. Several studies have supported this hypothesis to some extent [77, 85, 86]. However, contrary findings have also been reported. After measuring the HRV in healthy asymptomatic subjects at two separate time points, Zhang et al. [87] reported a dominance of the PNS following thoracic manipulation. Recently, using both HRV and baroreflex sensitivity, another study [88] conducted on acute back pain patients has also demonstrated an increased parasympathetic autonomic control after lumbar manipulation.
However, there were methodological differences between these studies and no gold standard technique was used to measure the SNS changes. In addition, the differences in findings were somewhat dependant on the type of outcome measure used. It appears that the conflicting results mostly came from studies [77, 78, 85–89] that used HRV analysis to determine the nature of autonomic responses after manipulation. The findings of these studies were in favour of either the SNS or the PNS. On the other hand, a recent systematic review on postmanipulation SBF changes has reported the presence of a short-term sympatheto-excitatory response [76].
One possible reason for such differences might be the use of low frequency (LF)/high frequency (HF) ratio as an indicator of ANS activity, where HF represents PNS efferent activity and LF corresponds to both PNS and SNS efferent activity. This method of assessing HRV has been criticised due to oversimplification of the complex non-linear interactions between the SNS and the PNS [90]. More recently, Sampath et al. [91], using a reliable measure (near infrared spectroscopy) to assess SNS activity, reported an immediate sympathetic excitation following thoracic manipulation. Interestingly, this study also investigated pre- and post-manipulation HRV data but found no statistically significant difference between the groups. Nevertheless, the findings of this study need to be interpreted cautiously, as it was based on asymptomatic male subjects, and there has been a report of the ANS dysregulation in chronic pain patients. Hence, more research on symptomatic population is warranted.
Effects of manipulation-induced autonomic changes on supraspinal mechanisms
As discussed above, there is a complex interaction between the ANS and the pain system, and the PSNS plays a significant role in modulating pain and inflammation. Hence, considering the evidence of immediate sympatheto-excitatory responses following manipulation, Kovanur Sampath et al. [6] suggested that these SNS changes might be linked to changes in painmodulating supraspinal mechanisms. In support of this hypothesis, the authors cited two imaging studies [92, 93]. The first study conducted on neck pain patients demonstrated effects of manipulation on several supraspinal structures including the cerebellar vermis, middle temporal gyrus, visual association cortex, inferior prefrontal cortex and anterior cingulate cortex. The second study on healthy asymptomatic patients reported a significant association between insular cortex activation and subjective pain ratings.
Interestingly, all these structures have been reported to be involved in the regulation of autonomic function [94]. On the other hand, there has been a growing body of evidence in support of the manipulationinduced neural plastic changes, occurring in various brain structures such as the cerebellum, basal ganglia, prefrontal cortex, primary sensory cortex and primary motor cortex [95, 96]. A recent randomized study on subclinical pain populations, however, reported that the alteration in somatosensory processing occurs particularly within the prefrontal cortex [7]. Taken together, although there is no direct evidence in support of the Kovanur Sampath et al.’s hypothesis [6], this might be a fruitful area of research for future studies.
Co-activation of the neuroendocrine system
The hypothalamus region is known for coordinating stress responses by activating the hypothalamic-pituitary axis and a neural pathway involving the PSNS. The hypothalamicpituitary- adrenal (HPA) axis is considered to be the central stress response system and is known to release adrenal glucocorticoid (cortisol), which is a class of corticosteroids that are well recognized in the literature for their anti-inflammatory and immunosuppressive actions [97]. On the other hand, as discussed above, the SNS has been reported to serve as a mediator between the somatic and supportive processes. Hence, it has been well established that both the SNS and the HPA axis could play a significant role in the modulation of acute and chronic inflammation, and the neuroendocrine (SNS-HPA axis) mechanisms are involved in the pain relief and tissue-healing processes [97, 98]. These two systems have also been reported to work together, overlapping the underlying neural circuitry [98]. In addition, the evidence suggests that spinal manipulation could influence the activity of both the SNS and the HPA axis. Several studies have assessed the effect of spinal manipulation on the HPA axis, and an immediate increase in serum cortisol levels following manipulation has been observed in both symptomatic and asymptomatic patients [99, 100].
Considering the above facts, Kovanur Sampath et al. [6] hypothesized that there could be an association between SNS changes and HPA axis responses, and post-manipulation changes in the SNS might be accompanied by HPA axis changes. The authors proposed possible neural reflex pathways in support of this hypothesis. They suggested that HVLAT at the thoracolumbar segment of the spine would result in excitation of the preganglionic sympathetic cells and subsequent stimulation of mechanoreceptors. These inputs would then travel to several regions of the brain stem and lead to opioid-independent analgesia by influencing the hypothalamus and periaqueductal gray (PAG) in the midbrain. The hypothalamic release of corticotropin-releasing factor would then occur to modulate the SNS and HPA axis response. The neuroendocrine (SNS-HPA axis) system would then release its end products (catecholamines and glucocorticoids) to initiate anti-inflammatory and tissuehealing actions. However, to date only one study [91] has been conducted to investigate the SNS-HPA axis response to manipulation in the same trial. Although this study reported a reduction in salivary cortisol level immediately after thoracic manipulation and observed an immediate effect of manipulation on the SNS, the clinical relevance of such changes is so far unknown. Therefore, more research is needed to determine the true clinical significance of neuroendocrine response following manipulation.
Hypoalgesic effects
Hypoalgesic effects of spinal manipulation are thought to be caused by three types of mechanisms.
Segmental inhibition
The concept of this mechanism is based on the Melzack and Wall’s [101] gate control theory of pain. This theory proposes that nociceptive (small-diameter) A-δ and C sensory fibers carry the pain stimuli to the dorsal horn and “open” the substantia gelatinosa layer, whereas non-nociceptive (large-diameter) A-β fibers inhibit the transmission of pain signals by blocking the entry of A-δ and C fibers. Because mechanical stimulus applied during spinal manipulation may alter peripheral sensory input from paraspinal tissues, it has been presumed that manipulation may influence the gate closing mechanism by stimulating the A-β fibers from muscle spindles and facet joint mechanoreceptors [3]. Systematic reviews by Millan et al. [102] and Coronado et al. [103] have critically reviewed studies that examined hypoalgesic effects of spinal manipulation on experimentally induced pain. Most of the studies included in these two reviews observed a segmental hypoalgesic effect of manipulation and suggested that supraspinal pathways might be involved in the segmental mechanism. In addition, the involvement of a segmental mechanism in the modulation of pain perception has been proposed by numerous studies that investigated neuromuscular effects of spinal manipulation (see 4. Neuromuscular effects). However, it needs to be determined whether the observed local hypoalgesic effect following manipulation is merely a reflex effect on the pre-existing painful condition itself or due to activation of the endogenous pain inhibitory system.
Activation of descending pain inhibitory pathways
This mechanism is based on the effects of spinal manipulation on pain modulatory neural circuitry. Manipulation has long been thought to modulate the nonopioid hypoalgesic system by activating the descending pain modulation circuit, especially serotonin and noradrenaline pathways, from the PAG and rostral ventromedial medulla of the brain stem [5, 104, 105]. This hypothesis has been supported by both animal model and human studies. In laboratory animal models [106–108], objective evidence supports a central antinociceptive effect that appeared to be mediated by serotoninergic and noradrenergic inhibitory pathways. The findings of human studies [109–111] conducted on both symptomatic and asymptomatic subjects are also consistent with the findings of animal models.
However, although human research supports a nonopioid form of manipulation-induced hypoalgesic effect through activation of some type of descending inhibitory mechanism, the exact circuit is yet not agreed upon. Because neural responses following spinal manipulation may vary depending on the rate of force application and the location at which the thrust is applied [25, 34, 35], it has been assumed that variations in mechanical parameters of manipulation may activate different descending inhibitory pathways [112]. Therefore, future research should investigate the exact descending pain modulatory circuit involved after spinal manipulation, and these studies should also carefully consider the force/time and contact site characteristics of the intervention. Non-specific cerebral responses
The relevance of non-specific variables, such as expectation and psychosocial factors, in the mechanisms of spinal manipulation cannot be totally dismissed [12]. Expectation of good functional outcomes may decrease pain perception without spinal involvement. In addition, a systematic review indicated that spinal manipulation is associated with better psychological outcomes than verbal interventions [113]. Investigations of the influence of non-specific cerebral processes in manipulation-induced hypoalgesia have found that manipulation has greater and specific effects on pain sensitivity than expectations of receiving the intervention [36, 114]. Nevertheless, additional work is needed to determine whether spinal manipulation with increased positive expectations could provide an additive effect on pain perception.
Temporal summation
Effects of spinal manipulation on temporal summation of pain constitute another experimental model that can be used to explain the mechanisms of manipulation-induced hypoalgesia. Temporal summation refers to an increased perception of pain evoked by repetitive painful (noxious) stimuli of same amplitude and frequency. It represents a psychophysical correlate of a frequency-dependent, progressively increasing excitability of dorsal horn neurones (i.e., wind-up) [115]. Wind-up is an interesting model to study for manual therapy researchers, as it is a central phenomenon and not mediated by peripheral mechanisms [116]. The constant nociceptive input into dorsal horn neurons through temporal summation can trigger transcriptional and translational changes that are related to short-lived aspects of central sensitization [115, 117]. Thus, temporal summation can be used to characterize mechanisms of central processing in chronic pain conditions.
Early experimental studies [36, 118] done with cutaneous heat application to examine effects of lumbar spinal manipulation have reported immediate reduction of temporal summation in the lower extremity regions but not in upper limb dermatomes. This finding suggested that the hypoalgesic effects observed following manipulation might be regionally specific or segmental in nature. To confirm this hypothesis, Bishop et al. [119] conducted a study to test whether thoracic spinal manipulation reduces temporal summation of pain. In contrast to earlier findings, they reported that temporal summation was reduced in both upper and lower extremities, which suggested an involvement of both segmental and descending inhibitory mechanisms in manipulation-induced hypoalgesia. Recently, Randoll et al. [10], using repeated electrical stimulus, also found that temporal summation of pain was reduced by thoracic spinal manipulation. The authors supported an involvement of segmental mechanism and suggested that deep high-threshold mechanoreceptors might be responsible for HVLAinduced hypoalgesia. However, further research is needed to establish the clinical relevance of these findings.
Conclusion
In this review, we discussed various theories that have been proposed to explain the neurophysiological effects of spinal manipulation and reviewed mechanistic studies that have been conducted to validate the relevance of these theories. So far, the exact mechanism through which spinal manipulation works has not been established. Experimental studies conducted on both animal and human subjects have indicated that the mechanical stimulation of manipulation produces a barrage of input into the dorsal horn of the spinal cord, which initiates a cascade of neural responses involving complex interactions between the peripheral nervous system and CNS. By observing neurophysiological responses following spinal manipulation, these studies have suggested possible mechanisms underlying the neuromuscular, autonomic, neuroendocrine and hypoalgesic effects of manipulation. Some clear neurophysiological effects of spinal manipulation have been demonstrated, including central neuroplastic changes, alterations in motor neuron excitability, improved muscle strength, increase in cortical drive, activation of the descending pain modulation circuit and central sensitisation.
The relevance of these findings in relation to the observed clinical effects remains unclear. This is because most of the mechanistic studies published to date mainly investigated short latency changes or immediate effects of spinal manipulation using their experimental models. These studies, however, had many methodological shortcomings, such as poor study design, no-intervention control group, lack of a standardised protocol, selective reporting of results and no follow-up of patients. Although a number of randomised controlled trials have been published recently, the number is still too limited. Long-term double-blind randomised trials with sham interventions and/or placebo as control are required to determine the true clinical significance of spinal manipulation. Furthermore, there is also a need for meticulous investigation of the dose-response relationship associated with specific neural effects of manipulation. Therefore, future work should explore possible neural mechanisms of spinal manipulation with careful attention to study design, and should carefully consider the implications of their findings.
Competing interests
The authors declare that they have no competing interests.
References:
Evans DW.
Mechanisms and Effects of Spinal High-velocity, Low-amplitude Thrust Manipulation:
Previous Theories
J Manipulative Physiol Ther 2002 (May); 25 (4): 251–262Evans DW, Breen AC.
A biomechanical model for mechanically efficient cavitation production during spinal manipulation:
prethrust position and the neutral zone.
J Manipulative Physiol Ther 2006;29(1):72–82.Potter L, McCarthy CJ, Oldham JA.
Physiological effects of spinal manipulation: a review of proposed theories.
Phys Ther Rev 2005;10(3):163–70.Maigne JY, Vautravers P.
Mechanism of action of spinal manipulative therapy.
Joint Bone Spine 2003;70(5):336–41.Pickar JG.
Neurophysiological Effects of Spinal Manipulation
Spine J (N American Spine Society) 2002 (Sep); 2 (5): 357–371Kovanur Sampath K, Mani R, Cotter JD, Tumilty S.
Measureable changes in the neuro-endocrinal mechanism following spinal manipulation.
Med Hypotheses 2015;85(6):819–24.Lelic, D.; Niazi, I.K.; Holt, K.; Jochumsen, M.; Dremstrup, K.; Yielder, P.; Murphy, B.
Manipulation of Dysfunctional Spinal Joints Affects Sensorimotor Integration in the Prefrontal Cortex:
A Brain Source Localization Study
Neural Plast. 2016 (Mar 7); 2016: 3704964Currie SJ, Myers CA, Durso C, Enebo BA, Davidson BS.
The neuromuscular response to spinal manipulation in the presence of pain.
J Manipulative Physiol Ther 2016;39(4):288–93.Zafereo J, Deschenes BK.
The role of spinal manipulation in modifying central sensitization.
J Appl Biobehav Res 2015;20(2):84–99.Randoll C, Gagnon-Normandin V, Tessier J, Bois S, Rustamov N, et al.
The mechanism of back pain relief by spinal manipulation relies on decreased temporal summation of pain.
Neuroscience 2017;349:220–8.Haavik, H and Murphy, B.
The Role of Spinal Manipulation in Addressing Disordered Sensorimotor Integration and
Altered Motor Control
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 768–776Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ.
The Mechanisms of Manual Therapy in the Treatment of Musculoskeletal Pain:
A Comprehensive Model
Man Ther. 2009 (Oct); 14 (5): 531–538Schmid A, Brunner F, Wright A, Bachmann LM.
Paradigm shift in manual therapy? Evidence for a central nervous system component in the response
to passive cervical joint mobilisation.
Man Ther 2008;13(5):387–96.Colloca CJ, Keller TS, Harrison DE, Moore RJ, Gunzburg R, Harrison DD.
Spinal manipulation force and duration affect vertebral movement and neuromuscular responses.
Clin Biomech (Bristol, Avon) 2006;21(3):254–62.Colloca CJ, Keller TS, Gunzburg R:
Biomechanical and Neurophysiological Responses to Spinal Manipulation in Patients With
Lumbar Radiculopathy
J Manipulative Physiol Ther. 2004 (Jan); 27 (1): 1–15Coppieters MW, Butler DS.
Do ‘sliders’ slide and ‘tensioners’ tension? An analysis of neurodynamic techniques and
considerations regarding their application.
Man Ther 2008;13(3):213–21.Funabashi M, Kawchuk GN, Vette AH, Goldsmith P, Prasad N.
Tissue Loading Created During Spinal Manipulation in Comparison to Loading Created by
Passive Spinal Movements
Sci Rep. 2016 (Dec 1); 6: 38107Bialosky JE, George SZ, Bishop MD.
How spinal manipulative therapy works: why ask why?
J Orthop Sports Phys Ther 2008;38(6):293–5.Colloca CJ, Keller TS.
Stiffness and neuromuscular reflex response of the human spine to posteroanterior manipulative thrusts
in patients with low back pain.
J Manipulative Physiol Ther 2001;24(8):489–500.Clark B, Goss D, Walkowski S, Hoffman R, Ross A, Thomas J.
Neurophysiologic Effects of Spinal Manipulation in Patients With Chronic Low Back Pain
BMC Musculoskelet Disord. 2011 (Jul 22); 12: 170Zedka M, Prochazka A, Knight B, Gillard D, Gauthier M.
Voluntary and reflex control of human back muscles during induced pain.
J Physiol 1999;520(2):591–604.Walker BF, Koppenhaver SL, Stomski NJ, Hebert JJ.
Interrater reliability of motion palpation in the thoracic spine.
Evid Based Complement Alternat Med 2015;2015:815407.Seffinger MA, Najm WI, Mishra SI, Adams A, Dickerson VM, Murphy LS, et al.
Reliability of spinal palpation for diagnosis of back and neck pain: a systematic review of the literature.
Spine (Phila Pa 1976) 2004;29(19):E413–25.Frantzis E, Druelle P, Ross K, McGill S.
The accuracy of osteopathic manipulations of the lumbar spine: a pilot study.
Int J Osteopath Med 2015;18(1):33–9.Cambridge ED, Triano JJ, Ross JK, Abbott MS.
Comparison of force development strategies of spinal manipulation used for thoracic pain.
Man Ther 2012;17(3): 241–5.Haneline MT, Cooperstein R, Young M, Birkeland K.
Spinal Motion Palpation: A Comparison of Studies That Assessed
Intersegmental End Feel vs Excursion
J Manipulative Physiol Ther. 2008 (Oct); 31 (8): 616–626van Trijffel E, Anderegg Q, Bossuyt PM, Lucas C.
Inter-examiner reliability of passive assessment of intervertebral motion in the cervical and
lumbar spine: a systematic review.
Man Ther 2005;10(4):256–69.Holt, K., Russell, D., Young, M., Sherson, M., Haavik, H.
Interexaminer Reliability of Seated Motion Palpation for the Stiffest Spinal Site
J Manipulative Physiol Ther. 2018 (Sep); 41 (7): 571–579Holt, K., Russell, D., Cooperstein, R., Young, M., Sherson, M., Haavik, H.
Interexaminer Reliability of a Multidimensional Battery of Tests
Used to Assess for Vertebral Subluxations
Chiropractic Journal of Australia 2016; 46 (1): 100–117Cooperstein R, Young M, Haneline M (2013)
Interexaminer Reliability of Cervical Motion Palpation Using Continuous Measures
and Rater Confidence Levels
J Can Chiropr Assoc. 2013 (Jun); 57 (2): 156–164Cooperstein R, Haneline M, Young M (2010)
Interexaminer Reliability of Thoracic Motion Palpation Using
Confidence Ratings and Continuous Analysis
J Chiropractic Medicine 2010 (Sep); 9 (3): 99–106Cooperstein R, Young M.
The Reliability of Spinal Motion Palpation Determination of
the Location of the Stiffest Spinal Site is Influenced by
Confidence Eatings: A Secondary Snalysis of Three Studies
Chiropractic & Manual Therapies 2016 (Dec 20); 24: 50Pickar JG, Bolton PS.
Spinal Manipulative Therapy and Somatosensory Activation
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 785–794Nougarou F, Pagé I, Loranger M, Dugas C, Descarreaux M.
Neuromechanical response to spinal manipulation therapy: effects of a constant rate of force application.
BMC Complement Altern Med 2016;16:161.Downie AS, Vemulpad S, Bull PW:
Quantifying the High-velocity, Low-amplitude Spinal Manipulative Thrust: A Systematic Review
J Manipulative Physiol Ther. 2010 (Sep); 33 (7): 542-53Bialosky JE, Bishop MD, Robinson ME, Barabas JA, George SZ.
The Influence of Expectation on Spinal Manipulation Induced Hypoalgesia:
An Experimental Study in Normal Subjects
BMC Musculoskelet Disord. 2008 (Feb 11); 9: 19Travell J, Rinzler S, Herman M.
Pain and disability of the shoulder and arm: treatment by intramuscular infiltration with procaine hydrochloride.
J Am Med Assoc 1942;120(6):417–22.van Dieën JH, Selen LP, Cholewicki J.
Trunk muscle activation in low-back pain patients, an analysis of the literature.
J Electromyogr Kinesiol 2003;13(4):333–51.Hodges PW, Moseley GL.
Pain and motor control of the lumbopelvic region: effect and possible mechanisms.
J Electromyogr Kinesiol 2003;13(4):361–70.Geisser ME, Haig AJ, Wallbom AS, Wiggert EA.
Pain-related fear, lumbar flexion, and dynamic EMG among persons with chronic musculoskeletal low back pain.
Clin J Pain 2004;20(2):61–9.Lewis S, Holmes P, Woby S, Hindle J, Fowler N.
The Relationships Between Measures of Stature Recovery, Muscle Activity and Psychological Factors
in Patients with Chronic Low Back Pain
Manual Therapy 2012 (Feb); 17 (1): 27-33Herzog W.
Clinical biomechanics of spinal manipulation.
London: Churchill Livingstone; 2000.Bicalho E, Setti JA, Macagnan J, Cano JL, Manffra EF.
Immediate effects of a highvelocity spine manipulation in paraspinal muscles activity of nonspecific
chronic low-back pain subjects.
Man Ther 2010;15(5):469–75.Lehman G.
Kinesiological research: the use of surface electromyography for assessing the effects of spinal manipulation.
J Electromyogr Kinesiol 2012;22(5):692–6.Lehman GJ, McGill SM.
Spinal manipulation causes variable spine kinematic and trunk muscle electromyographic responses.
Clin Biomech (Bristol, Avon) 2001;16(4):293–9.Ferreira ML, Ferreira PH, Hodges PW.
Changes in postural activity of the trunk muscles following spinal manipulative therapy.
Man Ther 2007;12(3):240–8.Colloca CJ, Keller TS, Gunzburg R.
Neuromechanical Characterization Of In Vivo Lumbar Spinal Manipulation.
Part II. Neurophysiological Response
J Manipulative Physiol Ther. 2003 (Nov); 26 (9): 579–591Keller TS, Colloca CJ, Gunzburg R.
Neuromechanical Characterization of in vivo Lumbar Spinal Manipulation.
Part I. Vertebral Motion
J Manipulative Physiol Ther. 2003 (Nov); 26 (9): 567–578Wilder DG, Aleksiev AR, Magnusson ML, Pope MH, Spratt KF, Goel VK.
Muscular response to sudden load. A tool to evaluate fatigue and rehabilitation.
Spine (Phila Pa 1976) 1996;21(22):2628–39.Christiansen TL, Niazi IK, Holt K, Nedergaard RW, Duehr J, Allen K, et al.
The effects of a single session of spinal manipulation on strength and cortical drive in athletes.
Eur J Appl Physiol 2018;118(4):737–49.Niazi IK, Turker KS, Flavel S, Kinget M, Duehr J, Haavik H.
Changes in H-reflex and V-waves Following Spinal Manipulation
Experimental Brain Research 2015 (Apr); 233 (4): 1165–1173Holt K, Niazi IK, Nedergaard RW, Duehr J, Amjad I, Shafique M, et al.
The effects of a single session of chiropractic care on strength, cortical drive, and
spinal excitability in stroke patients.
Sci Rep 2019;9:2673.Korr IM.
Proprioceptors and somatic dysfunction.
J Am Osteopath Assoc 1975;74(7):638–50.Johansson H, Sojka P.
Pathophysiological mechanisms involved in genesis and spread of muscular tension in occupational
muscle pain and in chronic musculoskeletal pain syndromes: a hypothesis.
Med Hypotheses 1991;35(3):196–203.Trompetto C, Marinelli L, Mori L, Pelosin E, Currà A, Molfetta L, et al.
Pathophysiology of spasticity: implications for neurorehabilitation.
Bio Med Res Int 2014;2014:354906.Birznieks I, Burton AR, Macefield VG.
The effects of experimental muscle and skin pain on the static stretch sensitivity of human muscle spindles
in relaxed leg muscles.
J Physiol 2008;586(11):2713–23.Zedka M, Prochazka A, Knight B, Gillard D, Gauthier M.
Voluntary and reflex control of human back muscles during induced pain.
J Physiol 1999;520(Pt 2):591–604.Fryer G, Pearce AJ.
The effect of lumbosacral manipulation on corticospinal and spinal reflex excitability on asymptomatic participants.
J Manipulative Physiol Ther 2012;35(2):86–93.Lund JP, Donga R, Widmer CG, Stohler CS.
The pain-adaptation model: a discussion of the relationship between chronic
musculoskeletal pain and motor activity.
Can J Physiol Pharmacol 1991;69(5):683–94.Haavik H, Niazi IK, Jochumsen M, Ugin?ius P, Sebik O, Y?lmaz G, et al.
Chiropractic spinal manipulation alters TMS induced I-wave excitability and shortens the cortical silent period.
J Electromyogr Kinesiol 2018;42:24–35.Burke D.
Clinical uses of H reflexes of upper and lower limb muscles.
Clin Neurophysiol Pract 2016;1:9–17.Klomjai W, Katz R, Lackmy-Vallée A.
Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS).
Ann Phys Rehabil Med 2015;58(4):208–13.Murphy BA, Dawson NJ, Slack JR.
Sacroiliac joint manipulation decreases the Hreflex.
Electromyogr Clin Neurophysiol 1995;35(2):87–94.Dishman JD, Bulbulian R.
Spinal reflex attenuation associated with spinal manipulation.
Spine (Phila Pa 1976) 2000;25(19):2519–24.Dishman JD, Bulbulian R.
Comparison of effects of spinal manipulation and massage on motoneuron excitability.
Electromyogr Clin Neurophysiol 2001;41(2):97–106.Dishman JD, Cunningham BM, Burke J.
Comparison of tibial nerve H-reflex excitability after cervical and lumbar spine manipulation.
J Manipulative Physiol Ther 2002;25(5):318–25.Dishman JD, Burke J.
Spinal reflex excitability changes after cervical and lumbar spinal manipulation: a comparative study.
Spine J 2003;3(3):204–12.Dishman JD, Dougherty PE, Burke JR.
Evaluation of the effect of postural perturbation on motoneuronal activity following various
methods of lumbar spinal manipulation.
Spine J 2005;5(6):650–9.Suter E, McMorland G, Herzog W.
Short-term effects of spinal manipulation on Hreflex amplitude in healthy and symptomatic subjects.
J Manipulative Physiol Ther 2005;28(9):667–72.Dishman JD, Burke JR, Dougherty P.
Motor neuron excitability attenuation as a sequel to lumbosacral manipulation in subacute low back pain
patients and asymptomatic adults: a cross-sectional H-reflex study.
J Manipulative Physiol Ther 2018;41(5):363–71.Dishman JD, Ball KA, Burke J.
First Prize: Central motor excitability changes after spinal manipulation:
a transcranial magnetic stimulation study.
J Manipulative Physiol Ther 2002;25(1):1–9.Dishman JD, Greco DS, Burke JR.
Motor-evoked potentials recorded from lumbar erector spinae muscles: a study of corticospinal
excitability changes associated with spinal manipulation.
J Manipulative Physiol Ther 2008;31(4):258–70.Haavik H, Niazi IK, Jochumsen M, Sherwin D, Flavel S, Turker KS.
Impact of Spinal Manipulation on Cortical Drive to Upper and Lower Limb Muscles
Brain Sci. 2017 (Jan); 7 (1): 2Cannon WB.
Bodily changes in pain, hunger, fear, and rage: an account of recent researches into the
function of emotional excitement.
New York: Cornell University Library; 1915.Benarroch EE.
Pain-autonomic interactions.
Neurol Sci 2006;27(Suppl 2):S130–3.Zegarra-Parodi R, Park PY, Heath DM, Makin IR, Degenhardt BF, Roustit M.
Assessment of skin blood flow following spinal manual therapy: a systematic review.
Man Ther 2015;20(2):228–49.Win NN, Jorgensen AMS, Chen YS, Haneline MT.
Effects of Upper and Lower Cervical Spinal Manipulative Therapy on Blood Pressure and Heart Rate Variability
in Volunteers and Patients With Neck Pain: A Randomized Controlled, Cross-Over, Preliminary Study
Journal of Chiropractic Medicine 2015 (Mar); 14 (1): 1–9Welch A., Boone R.
Sympathetic and Parasympathetic Responses to Specific Diversified Adjustments to Chiropractic
Vertebral Subluxations of the Cervical and Thoracic Spine
Journal of Chiropractic Medicine 2008 (Sep); 7 (3): 86–93Sillevis R, Cleland J, Hellman M, Beekhuizen K.
Immediate effects of a thoracic spine thrust manipulation on the autonomic nervous system:
a randomized clinical trial.
J Man Manip Ther 2010;18(4):181–90.Cramer G, Darby S.
Clinical anatomy of the spine, spinal cord, and ANS. 3rd ed.
Missouri: Mosby; 2013.Elenkov IJ, Wilder RL, Chrousos GP, Vizi ES.
The sympathetic nerve—an integrative interface between two supersystems: the brain and the immune system.
Pharmacol Rev 2000;52(4):595–638.Pongratz G, Straub RH.
The sympathetic nervous response in inflammation.
Arthritis Res Ther 2014;16(6):504.Korr IM.
The neurobiologic mechanisms in manipulative therapy.
Boston: Springer US; 2012.Korr IM, Wright HM, Thomas PE.
Effects of experimental myofascial insults on cutaneous patterns of sympathetic activity in man.
Acta Neuroveg (Wien). 1962;23:329–55.Budgell B, Polus B.
The effects of thoracic manipulation on heart rate variability: a controlled crossover trial.
J Manipulative Physiol Ther 2006;29(8):603–10.Giles PD, Hensel KL, Pacchia CF, Smith ML.
Suboccipital decompression enhances heart rate variability indices of cardiac control in healthy subjects.
J Altern Complement Med 2013;19(2):92–6.Zhang J, Dean D, Nosco D, Strathopulos D, Floros M.
Effect of chiropractic care on heart rate variability and pain in a multisite clinical study.
J Manipulative Physiol Ther 2006;29(4):267–74.Ward J, Coats J, Tyer K, Weigand S, Williams G.
Immediate effects of anterior upper thoracic spine manipulation on cardiovascular response.
J Manipulative Physiol Ther 2013;36(2):101–10.Younes M, Nowakowski K, Didier-Laurent B, Gombert M, Cottin F.
Effect of spinal manipulative treatment on cardiovascular autonomic control in patients with acute low back pain.
Chiropr Man Therap 2017;25:33.Billman GE.
The effect of heart rate on the heart rate variability response to autonomic interventions.
Front Physiol 2013;4:222.Sampath KK, Botnmark E, Mani R, Cotter JD, Katare R, Munasinghe PE, et al.
Neuroendocrine response following a thoracic spinal manipulation in healthy men.
J Orthop Sports Phys Ther 2017;47(9):617–27.Ogura, T, Tashiro, M, Masud, M et al.
Cerebral Metabolic Changes in Men After Chiropractic Spinal Manipulation for Neck Pain
Altern Ther Health Med. 2011 (Nov); 17 (6): 12–17Sparks C, Cleland JA, Elliott JM, Zagardo M, Liu WC.
Using functional magnetic resonance imaging to determine if cerebral hemodynamic responses to pain change
following thoracic spine thrust manipulation in healthy individuals.
J Orthop Sports Phys Ther 2013;43(5):340–8.Kenney MJ, Ganta CK.
Autonomic nervous system and immune system interactions.
Compr Physiol 2011;4(3):1177–200.Daligadu J, Haavik H, Yielder PC, Baarbe J, Murphy B.
Alterations in Cortical and Cerebellar Motor Processing in Subclinical Neck Pain Patients
Following Spinal Manipulation
J Manipulative Physiol Ther. 2013 (Oct); 36 (8): 527–537Haavik-Taylor H, Murphy B.
Altered Central Integration of Dual Somatosensory Input After Cervical Spine Manipulation
J Manipulative Physiol Ther. 2010 (Mar); 33 (3): 178–188Ulrich-Lai YM, Herman JP.
Neural regulation of endocrine and autonomic stress responses.
Nat Rev Neurosci 2009;10(6):397–409.Chrousos GP.
Stress and disorders of the stress system.
Nat Rev Endocrinol 2009;5(7):374–81.Padayachy K, Vawda GH, Shaik J, McCarthy PW.
The immediate effect of low back manipulation on serum cortisol levels in adult males with mechanical low back pain.
Clin Chiropr 2010;13(4):246–52.Plaza-Manzano G, Molina F, Lomas-Vega R, Martínez-Amat A, Achalandabaso A
Changes in Biochemical Markers of Pain Perception and Stress Response After Spinal Manipulation
J Orthop Sports Phys Ther. 2014 (Apr); 44 (4): 231–239Melzack R, Wall PD.
Pain mechanisms: a new theory.
Science 1965;150(3699):971–9.Millan M, Leboeuf-Yde C, Budgell B, Amorim MA.
The Effect of Spinal Manipulative Therapy on Experimentally Induced Pain:
A Systematic Literature Review
Chiropractic & Manual Therapies 2012 (Aug 10); 20 (1): 26Coronado RA, Gay CW, Bialosky JE, Carnaby GD, Bishop MD, George SZ.
Changes in Pain Sensitivity Following Spinal Manipulation: A Systematic Review
and Meta-analysis
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 752–767Vernon, H.
Qualitative Review of Studies of Manipulation-induced Hypoalgesia
J Manipulative Physiol Ther 2000 (Feb); 23 (2): 134–138Wright A.
Hypoalgesia post-manipulative therapy: a review of a potential neurophysiological mechanism.
Man Ther 1995;1(1):11–6.Skyba DA, Radhakrishnan R, Rohlwing JJ, Wright A, Sluka KA.
Joint Manipulation Reduces Hyperalgesia By Activation of Monoamine Receptors
But Not Opioid or GABA Receptors in the Spinal Cord
Pain. 2003 (Nov); 106 (1-2): 159–168Reed WR, Pickar JG, Sozio RS, Long CR.
Effect of spinal manipulation thrust magnitude on trunk mechanical activation thresholds of lateral thalamic neurons.
J Manipulative Physiol Ther 2014;37(5):277–86.Song, XJ, Gan, Q, Cao, J-L, Wang, Z-B, and Rupert, RL.
Spinal Manipulation Reduces Pain and Hyperalgesia After
Lumbar Intervertebral Foramen Inflammation in the Rat
J Manipulative Physiol Ther. 2006 (Jan); 29 (1): 5–13Alonso-Perez JL, Lopez-Lopez A, La Touche R, Lerma-Lara S, Suarez E et al.
Hypoalgesic effects of three different manual therapy techniques on cervical spine and psychological interaction:
a randomized clinical trial.
J Bodyw Mov Ther 2017;21(4):798–803.O’Neill S, Ødegaard-Olsen Ø, Søvde B.
The Effect of Spinal Manipulation on Deep Experimental Muscle Pain in Healthy Volunteers
Chiropractic & Manual Therapies 2015 (Sep 7); 23: 25Sterling M, Jull G, Wright A.
Cervical mobilisation: concurrent effects on pain, sympathetic nervous system activity and motor activity.
Man Ther 2001;6(2):72–81.Savva C, Giakas G, Efstathiou M.
The role of the descending inhibitory pain mechanism in musculoskeletal pain following high-velocity,
low amplitude thrust manipulation: a review of the literature.
J Back Musculoskelet Rehabil 2014;27(4):377–82.Williams NH, Hendry M, Lewis R, Russell I, Westmoreland A, Wilkinson C.
Psychological Response in Spinal Manipulation (PRISM): A Systematic Review of Psychological Outcomes
in Randomised Controlled Trials
Complementary Therapies in Medicine 2007 (Dec); 15 (4): 271–283Bialosky JE, George SZ, Horn ME, Price DD, Staud R, Robinson ME.
Spinal manipulative therapy—specific changes in pain sensitivity in individuals with low back pain (NCT01168999).
J Pain 2014;15(2):136–48.Anderson RJ, Craggs JG, Bialosky JE, Bishop MD, George SZ, Staud R, et al.
Temporal summation of second pain: variability in responses to a fixed protocol.
Eur J Pain 2013;17(1):67–74.Herrero JF, Laird JM, Lopez-Garcia JA.
Wind-up of spinal cord neurones and pain sensation: much ado about something?
Prog Neurobiol 2000;61(2):169–203.Staud R, Craggs JG, Robinson ME, Perlstein WM, Price DD.
Brain activity related to temporal summation of C-fiber evoked pain.
Pain 2007;129(1–2):130–42.George SZ, Bishop MD, Bialosky JE, Zeppieri G, Robinson ME.
Immediate effects of spinal manipulation on thermal pain sensitivity: an experimental study.
BMC Musculoskelet Disord 2006;7:68.Bishop MD, Beneciuk JM, George SZ.
Immediate reduction in temporal sensory summation after thoracic spinal manipulation.
Spine J 2011;11(5):440–6.
Return to ABOUT SPINAL ADJUSTING
Since 5-27-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |