

The Bárány Society Position
on ‘Cervical Dizziness’This section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Journal of Vestibular Research 2022 (Nov 15): 1–13 ~ FULL TEXT
OPEN ACCESS Seemungal, Barry M. | Agrawal, Yuri | Bisdorff, Alexander | Bronstein, Adolfo | Cullen, Kathleen E. | Goadsby, Peter J. | et al.
Centre for Vestibular Neurology,
Department of Brain Sciences,
Imperial College London, UK
This paper describes the Bárány Society Classification OverSight Committee (COSC) position on Cervical Dizziness sometimes referred to as Cervical Vertigo. This involved an initial review by a group of experts across a broad range of fields, and then subsequent review by the Bárány Society COSC. Based upon the so far published literature, the Bárány Society COSC takes the view that the evidence supporting a mechanistic link between an illusory sensation of self-motion (spinning or otherwise) and neck pathology and/or symptoms of neck pain - either by affecting the cervical vertebra, soft tissue structures or cervical nerve roots - is lacking. When a combined head and neck movement triggers an illusory sensation of spinning, there is either an underlying common vestibular condition such as migraine or BPPV or less commonly a central vestibular condition including, when acute in onset, dangerous conditions such as a dissection of the vertebral artery with posterior circulation stroke and, exceedingly rarely, a vertebral artery compression syndrome.
The Committee notes however, that migraine, including vestibular migraine, is by far, the commonest cause for the combination of neck pain and vestibular symptoms. The committee notes that since head movement aggravates symptoms in almost any vestibular condition, the common finding of increased neck muscle tension in vestibular patients, may be linked as both cause and effect, to reduced head movements. Additionally, there are theoretical mechanisms, which have never been explored, whereby cervical pain may promote vaso-vagal, cardio-inhibitory reflexes and hence by presyncopal mechanisms, elicit transient disorientation and/or imbalance. The committee accepts that further research is required to answer the question as to whether those rare cases in which neck muscle spasm is associated with a vague sense of spatial disorientation and/or imbalance, is indeed linked to impaired neck proprioception.
Future studies should ideally be placebo controlled and double-blinded where possible, with strict inclusion and exclusion criteria that aim for high specificity at the cost of sensitivity. To facilitate further studies in “cervical dizziness/vertigo”, we provide a narrative view of the important confounds investigators should consider when designing controlled mechanistic and therapeutic studies. Hence, currently, the Bárány COSC, refrains from proposing any preliminary diagnostic criteria for clinical use outside a research study. This position may change as new research evidence is provided.
From the FULL TEXT Article:
Introduction
The relationship between imbalance and dizziness (or overt vertigo - see 3rd paragraph below) with neck problems has long been debated, but the first modern hypothesis was elaborated by Barré and Lieou of a cervical spondylotic irritation of the sympathetic plexus affecting blood flow in the brainstem [1] and then by Ryan and Cope [2] of a spondylosis-related modulation of cervical afferent signals synapsing in the vestibular nuclear complex. A key concept common to these explanations was that of a neck problem causing dizziness and imbalance.
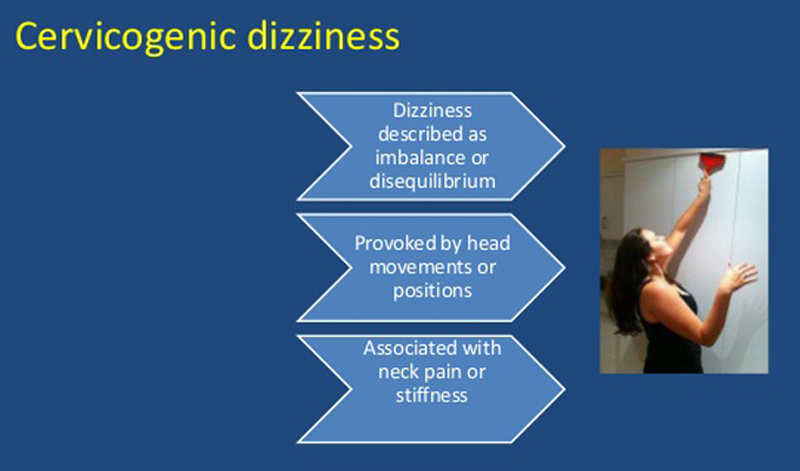
Note that this paper considers vascular vertigo — i.e., the exceedingly rare syndrome of spondylotic occlusion of the vertebral arteries during head turns [3] — a separate entity and this is not considered here. Whiplash is also beyond the scope of this document primarily because acceleration of the neck is always accompanied by acceleration to the head (and brain) thus definitive statements on the neck contribution to symptoms and signs are difficult, particularly since emerging data show that vestibular system dysfunction (from the labyrinth to the cerebral cortex) is extremely common in traumatic brain injury (TBI) [4], but also that at least acutely, traumatic brain injury disrupts patient’s perception of vertigo [5] explaining the poor correspondence between symptoms and signs in acute TBI. [6] Hence studies that included patients with whiplash,ziness including associative terms, e.g., cervical dizziness or cervical vertigo; or terms with aetiological implications, e.g., cervicogenic dizziness or cervicogenic vertigo. Regarding neck-related dizziness, the following are consistent features described in the literature [7-11]:
Neck stiffness and pain are aggravated during neck movements.
Neck movements* trigger transient imbalance and/or light-headedness and/or illusory self-motion (* studies do not distinguish combined head-neck movement from isolated neck movement).
Neck-directed therapy improves neck pain, neck stiffness and dizziness.
This means that the cervical dizziness (see paragraph below on the use of the terms of dizziness and vertigo) can be excluded if:
There is no neck pain or discomfort.
The dizziness ever occurs spontaneously (i.e., can occur without head or neck movement), or if the dizziness is exclusively positional (i.e., when the head orientation with respect to gravity changes).
Regarding terminology, we propose to use the term Cervical Dizziness for several reasons. First, the Bárány Society uses the term ‘vertigo’ [12] to indicate illusory self-motion of any cause. Illusory self-motion (i.e., ‘vertigo’) is however not ubiquitous (nor common) in this syndrome as described in the literature. Patients instead always complain of at least one (or more) of imbalance, light-headedness, and disorientation [13] or presyncope [7], i.e., ‘dizziness’. While we do include reports of illusory self-motion (‘vertigo’) in this position paper, their relative frequency compared to the more common reports of dizziness means that it is more appropriate to use the word Dizziness.
Put another way, there is always ‘dizziness’, and in some cases, there is in addition ‘vertigo’, hence using the term ‘Cervical Vertigo’ only satisfies a minority of the literature and using the cumbersome term ‘Cervical Dizziness/Vertigo’, although descriptively correct for some cases, manifests redundancy in terms of identifying the patients.
Thus, it should be understood that the specific term ‘Cervical Dizziness’ will include the minority of cases with vertigo, even if not indicated in the name, for the reasons above (note that this use still satisfies the Bárány Society distinction between vertigo and dizziness as we have defined our use of the terms as above). Secondly, as the aetiology is unclear, or at least the data to support underlying mechanisms in humans are inconclusive, and there is no diagnostic test, the term Cervicogenic implies a mechanistic knowledge that is currently lacking. Hence, we propose to use the term Cervical.
Methods
The work presented here is part of an ongoing project to develop an International Classification of Vestibular Disorders (ICVD). The ICVD uses a structured process to develop consensus diagnostic criteria for vestibular symptoms and disorders. The process of establishing criteria is overseen by the Classification Committee of the Bárány Society. For each diagnostic category, an international team of content experts from multiple disciplines is established to propose initial criteria based on the best available scientific evidence. For cervical dizziness, a literature review was performed, and an initial document produced that was commented upon by the subcommittee members in March 2017. Comments were gathered and combined into and an initial position paper which was presented in Berlin to the Classification Committee in November 2019. The position presented here is supported by a process of discussion and refinement as established by the classification committee for the ICVD. The sections presented below have been carefully considered to account for broad applicability to the international community of otolaryngologists, physical therapists, neurophysiologists, audiologists, neurologists, neurosurgeons, cardiologists, and general physicians, who may be seeing patients with this syndrome.
Epidemiology
There are no high-quality epidemiological data for cervical dizziness for the simple reason that (a) there is no accepted consensus diagnosis; (b) there is no agreed diagnostic test; (c) and patients present in different ways to different specialists. The Global Burden of Disease study [14] showed that neck pain was the fourth commonest condition worldwide (with a global point prevalence of 5%). One study assessing a population sample of 797 people found a one-year prevalence of neck pain of 68.4%. [15] Conversely, dizziness (including disequilibrium) and vertigo, affects 11–20% of the population every year. [16, 17] It follows that a significant proportion of the population will have dizziness and neck pain purely coincidentally.
Proponents of cervical dizziness will point to time-locked triggering of neck pain and dizziness on head movements, however, head movement aggravates almost all vestibular conditions, providing a means by which vestibular patients with co-existent neck pain may appear to have a cervical-mediated dizziness –especially if there is not an exhaustive attempt to exclude concurrent vestibular disorders. Indeed, Ryan and Cope [2] who first proposed the somatosensory hypothesis of cervical vertigo in 1955, are likely to have based their observations primarily upon cases with benign paroxysmal positional vertigo (BPPV) who had coincident neck pain (although BPPV was previously described by Robert Bárány in 1908, it had only come to the fore in 1952 following Dix and Hallpike’s publication [18]). Furthermore, neck pain is a recognised feature of vestibular disturbances of almost any cause, as patients’ avoidance of natural head movements (that worsen their vertigo) can lead to neck stiffness and pain. [19] Migraine requires a special mention, being a common cause of dizziness (particularly imbalance [20]) and vertigo, it is also independently associated with neck pain with a 76% one-year prevalence of neck pain in migraineurs. [15] It follows that there are several reasons why dizziness and neck pain can be linked even if there is not a cervical genesis to the problem.
Pathophysiology
Here, we review the proposed pathophysiology of cervical dizziness to provide a rational approach to the investigation and management of this syndrome.
The Somatosensory input hypothesis
It is generally accepted that the vestibular system is part of a multimodal sensorimotor system in which signals generated by the labyrinth interact with other sensory inputs, implying that vestibular inputs and hence symptoms may also originate from a variety of non-labyrinthine end-organs or systems (e.g., limb and proprioception – discussed below). Despite this, that a structure is shown to be intimately bound to vestibular signaling, does not automatically predict what kind of symptoms may originate from disturbance to this structure. For example, extraocular eye muscles are densely innervated by muscle spindles with projections to the vestibular nuclei [21], yet vestibular syndromes do not generally occur with eye muscle disease nor with interventions such as strabismus surgery or Botox injections.
Neck proprioceptive signals are an integral component of the vestibular system, with animal data showing that cervical afferents provide input to secondary vestibular neurones in the vestibular nuclear complex. [22-27] Ryan and Cope [2] proposed that this physiological link could manifest as dizziness such that abnormal neck joint proprioception could modulate vestibular neuronal activity and hence lead to dizziness and imbalance. Brown [28] considered that abnormal neck muscle proprioception, including from muscle disease or reduced movement relating to pain [10], could contribute to cervical dizziness, including via a mismatch between signals of expected (efference copy) and actual (including vestibular and proprioceptive inputs) head movements. Indeed, during active head movements in primates, suppression of vestibular afferent input is found in vestibular nuclei neurones that generate vestibulo-spinal reflexes [29, 30], as well as in the ascending posterior thalamocortical vestibular pathway. [31] Notably, this suppression of vestibular afferent input only occurs when there is congruence between expected and real neck proprioceptive feedback and is mediated by cerebellum-dependent mechanisms. [32]
In conditions where vestibular afferent input becomes less reliable in primates (e.g., with peripheral vestibular lesioning), neck inputs including neck proprioceptive and neck motor efference copy signals, partially substitute for the labyrinthine-derived signals at the level of single neurones in both reflex and ascending vestibular pathways. [31, 33–36] Thus overall, the substitution by neck proprioceptive and motor efference signals inputs in vestibular pathways, and/or a mismatch between intended and real head-on-neck movements, may provide the basis by which distorted brainstem vestibular signaling could be transmitted via vestibular thalamic relay pathways to cortical regions. It should be noted that vestibular cortical processing — shown to be anatomically diffuse across the cerebral cortex in animals [37] and humans [38, 39] — is employed for both perceptual and non-perceptual mechanisms, such as postural control. [5] Thus, locating a vestibular signal at cortical level does not automatically indicate its relevance for perception and hence symptom generation. Although abnormal brainstem plasticity may contribute to chronic vestibular symptoms, in humans, higher order processes — including perceptual and non-perceptual mechanisms — likely dominate bottom-up processes [38, 40, 41] in the success or failure of symptomatic recovery from peripheral vestibular dysfunction. [42, 43]
One cross-species study involved the injection of local anaesthetic in or around the upper cervical muscles which led to a gait ataxia in lower mammals, primates and one healthy human subject. [44] Nystagmus was evoked in animals but not in the healthy human who did, however, report a sensation of tilting, disequilibrium and disorientation, and position-induced tilting sensation (over several hours), but there was no frank illusory sensation of spinning. Importantly, there was no report of pain by the human subject. Indeed, the use of local anaesthesia in this study undermines its suitability as a model for cervical dizziness. Importantly, the more modern approach using Botox (Botulinum Toxin A) to neck muscles for dystonia, affecting muscle spindles via gamma motor neurones, does not induce vertigo. [45]
Cervical inputs can generate a weak cervico-ocular reflex (COR) nystagmus in humans during trunk rotations in the dark, with the head fixed in space. One study noted equivalent COR responses in 40 healthy subjects versus 30 patients with problems of the upper cervical spine. [46] The COR, which is more prominent in patients with peripheral vestibular dysfunction [47], can be enhanced in such patients with neck muscle vibration [48] or following vestibular rehabilitation exercises [49], indicating the COR’s plasticity. An enhanced COR in patients with preserved vestibular function is also found in cerebellar disorders — however, trunk-on-head or head-on-trunk rotation failed to induce dizziness or vertigo [50], indicating that a prominent COR may not be accompanied by symptomatic complaint.
One study [51] investigating a cervical proprioceptive hypothesis for cervical dizziness found that following an uncomfortable EMG-guided saline injection into paraspinal muscles at C2/3 in healthy subjects, there was a degraded accuracy (compared to baseline) in subjects’ positioning their head at 30° eccentrically. The subjects’ accuracy in head positioning in the neutral position was however unaffected post-injection. Although the finding of impaired positioning in the head-eccentric condition is supportive of a proprioceptive model for cervical dizziness, there were several limitations of this study [51] including:(a) a baseline asymmetry in head-in-space positioning;
(b) the lack of report upon whether the degree of head-positioning accuracy correlated with extent of pain;
(c) the persistence of the performance deficit even after the pain had subsided (weakening the link between pain and impaired head-on-neck positioning performance);
(d) only 4 of 11 subjects reported dizziness and imbalance, indicating that head-on-neck positioning impairment was not consistently linked to symptoms (pain) and signs (imbalance), features that are typically associated with putative cervical dizziness.Despite supportive animal physiology discussed above and experimental human data [44, 51], there are also important confounds that need to be controlled when experimentally assessing the Somatosensory Hypothesis in humans. For example, laboratory experiments have demonstrated arthrokinetic nystagmus accompanied by vertigo [52], yet there is no indication that patients with chronic upper limb pain may complain of dizziness (just as there are many patients with severe neck pain without dizziness). Indeed, the “Somatosensory Hypothesis” should predict that most patients with severe cervical radiculopathy should have dizziness and the degree of dizziness should correlate with the extent of the measured neck proprioceptive deficit. On the other hand, as most cervical radicular disease is chronic in nature, related proprioceptive deficits might not cause dizziness due the adaptive plasticity of vestibular circuits. These questions remain unanswered however, as there are no prospective, blinded, and controlled studies that have assessed the mechanisms and incidence of dizziness in patients with severe cervical radiculopathy and their progress, following surgical intervention.
An additional complication in humans is the powerful influence of top-down effects that can induce not only illusory sensations of vertigo but also induce a nystagmus in the absence of any peripheral vestibular activation or any actual movement of the head or body by mere ‘suggestion’. [41] Indeed, the coupling between vestibular sensation and vestibular reflex responses in humans is not straightforward and maybe affected by central adaptive processes in healthy subjects [38] or by brain disease. [5] For example, in healthy subjects, although measures of vestibular-perceptual and VOR thresholds to self-motion overlap in magnitude [53], perceptual thresholds are generally greater than VOR thresholds, but this perceptuo-reflex disparity is hugely amplified in patients with a brain dysfunction who manifest ‘vestibular agnosia’ [5, 54] (in vestibular agnosia, significant peripheral vestibular activation may not be accompanied by a vertigo sensation).
Some healthy subjects who are adapted to vestibular stimulation from training (e.g., pilots and ballet dancers [38, 55]) may also show a reduced perceptual sensitivity to vestibular activation. Conversely, patients with functional dizziness (‘PPPD’ - persistent postural-perceptual dizziness [56]) may have a heightened sensitivity to vestibular sensations including that emanating from expectation. [57, 58] The powerful influence of cognition on outcome measures may explain the equivalent impact upon neck position proprioceptive performance (obtained by a blinded assessor) in 45 patients with neck pain [59], following one of three different interventions, comprising two different mental training interventions or neck vibration. All three interventions improved neck position proprioceptive performance, although only vibration reduced neck pain. [59]
It follows that in humans, sensations of illusory self-motion, imbalance, spatial disorientation and even neck proprioception, are influenced by powerful top-down cognitive mechanisms. This thus mandates that all interventional studies in cervical dizziness, must be double-blinded and for treatment studies, controlled with placebo or some other intervention. Furthermore, the confounds of the effects of central adaptation in healthy subjects [38, 55] and the impact of brain disease in patients [4–6, 60] (e.g., TBI) on perceptuo-reflex uncoupling underline the importance of patient selection in studies of cervical dizziness.
Triggered migraine hypothesis
The consensus definition of vestibular migraine [61] includes a ‘head motion-induced vertigo, occurring during head motion’, which if combined with neck pain and stiffness would produce a clinical picture of cervical dizziness. Since neck pain is a core feature of cervical dizziness then pain inputs to trigeminal circuits will be ubiquitous in these patients and trigeminal nociceptive activation is implicated in migraine mechanisms. This could provide an indirect means for neck-pain mediated dizziness via a triggered vestibular migraine. Conversely, migraine can cause a secondary neck stiffness [15] again producing a clinical picture of cervical dizziness. Additionally, during acute vestibular migraine, 95% of patients display a gait ataxia, in addition to dizziness. [62] Thus, migraine is an important confound for the diagnosis of cervical dizziness. Indeed, as Goadsby argued [63], neck pain may trigger migraine and hence provide a mechanism by which migraine symptoms can result from a neck problem. Moreover, the presence of neck discomfort in the premonitory phase of migraine, where the headache has not yet started [64, 65], complicates the interpretation of vertigo in that setting. Additionally, it is not sufficient to exclude patients with only vestibular migraine but since it is likely that “ . . . migraine subtypes represent a spectrum . . . ” [66], it would be prudent to exclude all migraineurs from studies of cervical dizziness. Although a minority of interventional trials of cervical dizziness have migraine in their exclusion criteria [8], it is not clear whether in these studies, a thorough neurological history was obtained to exclude less severe migraine phenotypes.
It follows that any pain input mediated by trigeminal circuits could potentially provoke dizziness via a triggered migraine. Consistent with this, supra-orbital pain (i.e., non-neck pain) induced experimentally by cutaneous electrical stimulation, triggered a vestibular nystagmus in 8 out of 10 migraineurs but not in any non-migraineur controls. [67] Importantly, median nerve origin pain did not trigger nystagmus in any of the subjects (symptoms of dizziness and disequilibrium were however not recorded). Proponents of a neck mediated cervical dizziness may point to the lack of patients with e.g., supraorbital pain complaining of dizziness. However, it is relatively easy to avoid touching a painful point on the scalp whereas it is difficult to completely suppress the habit of making a head turn that may trigger neck pain (and dizziness). That such a scenario (e.g., supra-orbital tenderness-related-dizziness) could evade empirical observation is not so difficult to imagine given the effect of cognitive biases in patients and clinicians in supressing the recognition of diagnoses not previously entertained.
Trigeminal Hypothesis not invoking migraine
Since neck pain is a ubiquitous feature in cervical dizziness then trigeminal involvement must be obligatory. Although trigeminal stimulation is intimately involved in migraine mechanisms, theoretically, trigeminal mechanisms may independently of migraine –at least in non-migraineurs –be involved in cervical dizziness. It is instructive to note that the neurophysiological rationale used for explaining the origin of cervical headache has significant overlap with that used in explaining the origin of cervical dizziness, particularly that concerning the somatosensory hypothesis. [63, 68] Cervicogenic headache is considered to be referred pain (localised to the cranium) emanating from the cervical spine. Nociceptive afferents from the ophthalmic trigeminal division and from spinal nerves C1, C2 and C3, converge onto second-order neurones in the trigeminocervical nucleus. [69-71] This convergence enables C1-3 origin pain to be referred over much of the cranium.
There are no prospective controlled studies assessing the incidence of dizziness in patients with high cervical lesions (nerve root or otherwise) presenting primarily with pain, and whether treatment (surgical or medical) for their cervical-related pain alleviated their dizziness. In one small study of 17 patients assessed for vertigo post-surgery for cervical discectomy or spondylosis, there were no reported vestibular symptoms. [72] Baron [73] performed a retrospective case note review of 147 patients attending a tertiary “otoneurology/headache clinic” undergoing greater-occipital nerve injection and/or nearby trigger-point injection, based upon palpation-induced symptoms. The authors’ premise was that greater-occipital nerve injection-related improvements were primarily treating cervicogenic symptoms.
The patients’ chief complaint was dizziness in 93% with headache being the chief complaint in 3%. Dizziness of any severity affected 97% and headache of any severity affected 88% of patients. The authors reported that half of the patients reported improved dizziness with greater-occipital nerve injection, an improvement that was a little less marked than that for improved range of neck movement (70%) and headache (60%). Major limitations of this study include the lack of a control or placebo comparison, the unblinded nature of assessments and the non-standardised approach to injection points. Perhaps the most important limitation, as the authors admit, is that the retrospective nature of the study meant they were unable to rigorously classify headaches into strict criteria, including that for migraine. Given the range of headache disorders for which greater occipital nerve injection has been reported to be useful [74-76], this is a considerable limitation.
If we consider a trigeminal involvement in dizziness, then there are two possible mechanisms by which Trigeminal reflexes can produce dizziness with neck movement.
Trigemino-Vestibular reflexes: There are extensive inputs (and reciprocal outputs) to the vestibular nuclei from trigeminal afferents. [22, 77] The data supporting prominent trigemino-vestibular reflexes in humans is however limited. The Marano study [67] showing that supra-orbital (i.e., trigeminal) pain triggered vestibular mechanisms could support such mechanisms in humans however the effect was seen only in migraineurs (in whom mechanisms other than direct trigemino-vestibular reflexes could be implicated).
Trigemino-Cardiac reflexes: There is an extensive literature of the influence of trigeminal activation elicited by cranial stimulation as a potent drive to increasing vagal tone, including triggering asystole. [78, 79] Whether neck pain, aggravated by a rapid head turn could similarly affect cardiac output transiently in cases of cervical dizziness is not known since this would require continuous cardiac monitoring during head movement related neck pain and dizziness episodes, and such experiments have, to our knowledge, never been conducted. One study, however, did find that patients with neck pain and dizziness were significantly more likely to have postural hypotension compared to a control group of patients. [80] Importantly, drugs that potentiate the trigemino-cardiac reflex include opiates which are commonly prescribed in patients with chronic neck pain (other potentiators include beta-blockers and calcium channel antagonists which are also used in migraine). Compounding their potential to potentiate trigemino-cardiac responses, opiates may also compromise vestibulo-cerebellar functioning, adding to the sensed and/or real imbalance. [81] It follows that trigemino-cardiac reflexes are an important potential confound that should be considered when investigating cervical dizziness in future definitive studies.
Neurovascular hypotheses of Barré and Lieou
In 1926, Barré and Lieou hypothesised that mechanical compression by cervical spine spondylosis of the sympathetic plexus that surrounds the vertebral arteries could trigger vertigo via vertebrobasilar constriction. [1] Subsequent laboratory experiments in animals could not find evidence for this hypothesis [82, 83] and is generally considered a discredited hypothesis. [84]
Carotid sinus syndrome and associated syncope-mediated hypotheses
Another hypothesis that has been mentioned but not consistently assessed is that of the carotid sinus syndrome. The carotid sinus, found in the internal carotid artery and just superior to the bifurcation of the common carotid artery, is the main baroceptor in the cardiovascular system. Carotid sinus syndrome is due to excessive sensitivity of the carotid sinus body whose palpation (or massage) leads to a vagally-mediated cardio-inhibitory response leading to a bradycardia and hypotension. As specialists tend to be less well acquainted with areas of medicine that they do not work within, it is possible that some of the cases diagnosed as having cervical dizziness have in fact a carotid sinus syndrome with coincident neck pain. Certainly, in such a patient, a rapid head turn could trigger both neck pain and transient bradycardia and hypotension that could cause light headedness and presyncopal symptoms.
Anecdotally, cardiologists expert in syncope do not recognise seeing patients with carotid sinus syndrome with neck pain, although this could arise from referral bias or because cardiologists do not ask, or ponder, about neck pain. As previously mentioned, Morinaka [80] found (in a retrospective study of 176 patients) that patients with musculoskeletal neck pain were more likely to have orthostatic hypotension than those without neck pain, although age was a potential confound as patients with neck pain were older than those without neck pain. Physiological studies in healthy humans [85] have not shown significant modulation of cardiovascular reflexes by neck afferents, although there is evidence in animals that neck afferents modulate cardiovascular reflexes to a modest extent, hence it is theoretically possible that such modulation could exist in some rare cases. In summary, although theoretically possible, the notion that neck pain can induce cardio-inhibitory responses requires controlled studies.
Clinical interventional studies
There have been many interventional series involving neck surgery [72, 86, 87] neck manipulation [88], assessing the impact upon dizziness and imbalance but almost all were of poor quality from a trials’ criteria. A systematic review of therapeutic interventions for cervical dizziness [88] found only four studies of sufficient quality to be included. [8, 89–91] None of the studies mentioned blinding of the clinicians providing the intervention. Indeed, other studies are generally poorly controlled often without blinding, placebo intervention or randomisation. Many studies do not overtly exclude migraineurs or explicitly state their omission including the four studies that were identified by systematic review [92]. Excluding (or controlling for) migraine as a confound in future interventional studies is important for reasons discussed previously. For example, headache rates of over 70% were reported in two interventional studies [7, 91], and the provoking factors worsening both headache/neckache and dizziness were typical migraine triggers such as stress and hormonal flux. Finally, no study [7–9, 72, 87, 89, 91, 93–101] considered cardiac and/or vaso-vagal mediated mechanisms although Malmström [91] reported presyncope in one of their healthy subjects during an experimental model of cervical dizziness.
The two randomised, blinded and controlled interventional studies in cervical dizziness were published by the same group [8, 9, 89, 98], which is problematic from a replication standpoint. In an initial small study [89], 34 patients were randomised to either a neck manipulation intervention or placebo (neck laser). Although ‘migraine associated vertigo’ was excluded, patients with headache — of whom there is no detail — were included in the study and therapists were not blinded to the intervention. This study [89] found reduced dizziness and pain measured by a 10-point visual analogue scale at 6 and 12 weeks but using the Dizziness Handicap Inventory (DHI), intervention and placebo differed only at 6 weeks. Notably however, there was no concomitant improvement in balance performance at any time compared to the placebo group.
In a larger treatment study of 86 patients, dizziness and pain were reported at 6 weeks [8] and at one year [98] following active treatment and placebo. The interventions used were (i) Mulligan’s sustained natural apophyseal glides [102] (‘SNAG’, 29 patients); and (ii) Maitland’s passive joint mobilisations [103] (29 patients). In the placebo group (28 patients), a deactivated laser was applied to the neck. In this study, the groups’ baseline characteristics were well matched except the placebo group had greater baseline neck pain (P = 0.06) and relatively fewer women (placebo: 36% vs. intervention groups: 52% and 62%). In the report of early outcomes [8], the intervention groups showed improvements in the primary outcome of dizziness intensity both immediately and at 12 weeks whereas no effect on dizziness intensity was noted in the placebo group. In contrast, at 12 months [98], all groups showed a significant improvement in dizziness intensity and critically, there was no difference between any of the groups’ dizziness intensity at 12 months, indicating that the active interventions were no better than the deactivated laser (placebo) for the primary outcome of dizziness intensity at one year. The secondary outcome of pain was noted to be reduced across all groups immediately and at 12 weeks. As for the primary outcome of dizziness, there was no difference between groups in pain intensity at 12 months. Finally, the immediate benefit of the intervention on dizziness was not associated with head repositioning accuracy or improved balance performance [9], weakening the “Somatosensory Hypothesis”, i.e., that cervical dizziness is related to a mismatch between impaired proprioceptive and vestibular input during head upon neck movement.
In summary, the only well powered, blinded, and controlled study [8, 98], showed early symptomatic benefit but failed to find any effect in the primary outcome of dizziness intensity at 12 months. Additionally, the secondary outcomes of early benefit of pain and dizziness was not associated with improved head repositioning or balance performance [9], weakening support for the “Somatosensory Hypothesis” of cervical dizziness. All future interventional studies, to be considered as evidence, must be double blinded and placebo controlled since, as described previously, top-down effects in humans (including expectation) can provoke dizziness and nystagmus in human subjects even in the absence of any peripheral vestibular activation. [41] It follows that simply showing an effect on subjective features of dizziness by an intervention, on its own, cannot provide evidence for the existence of Cervical Dizziness and hence, using a therapeutic response cannot be part of any proposed definition to be used for research.
Considerations for future clinical research in Cervical dizziness
High quality data supporting the existence of cervical dizziness as a distinct entity, and the effect of intervention, are relatively few. Investigators planning clinical therapeutic and mechanistic studies should combine optimal clinical trial methodology (double-blinded, placebo-controlled therapeutic or sham-active controlled mechanistic studies) linked to specific a priori hypotheses. The hypothesised pathophysiological mechanism should therefore provide testable predictions measurable as primary outcomes (e.g., some clinical measure) and secondary outcomes (e.g., laboratory or mechanistically based outcome). We provide a narrative view of the many confounds and their potential amelioration, that researchers should consider when designing studies in cervical dizziness.
Firstly, since cervical dizziness is a cross-cutting complaint that presents to different specialities in different guises, it can be viewed through different speciality-specific lenses. Thus, we recommend the research team be multi-disciplinary, with representatives from (but not limited to) cardiology, neurology, neurosurgery, otolaryngology, and physiotherapy.
Controlled studies (placebo- or sham-controlled) are especially important in cervical dizziness research because, as described previously, top-down effects in humans can provoke dizziness and nystagmus in human subjects even in the absence of any peripheral vestibular activation. [41] Relevant reporting guidelines such as CONSORT should be used to ensure academic rigour when carrying out such studies [http://www.consort-statement.org]. Investigators should involve statisticians when designing studies to ensure the study is sufficiently powered to convincingly demonstrate positive results, and to reduce the risk of false-negative findings.
Given the scepticism about the existence of cervical dizziness, it is important for trialists to focus upon designing studies with high specificity even at the cost of low sensitivity, which means not only well-defined inclusion criteria, but particular attention should be paid to the exclusion criteria. Thus, initial studies should strive to recruit a cohort of ‘pure’ cervical dizziness patients. Thus, critical to this is the demonstration that investigators have made an exhaustive effort looking for common vestibular diagnoses whose manifestations may overlap with cervical dizziness. Thus, the investigators will enhance credibility by looking for and excluding, patients with BPPV, any form of migraine and via systematic assessment, any patients with laboratory measured evidence of peripheral or central vestibular dysfunction (e.g., looking for reduced VOR gain or cerebellar signs). The investigators, as experienced vestibular clinicians, can easily list some absolute exclusion criteria, e.g., the presence of spontaneous vestibular symptoms, since dizziness occurring without any head or neck movement, would seem an obvious first-pass exclusion.
Cardiogenic diagnoses should be considered and cardiac measures of pulse, blood pressure and ECG (ideally all by continuous monitoring) could be measured. We would strongly advise that any patient with significant postural hypotension (i.e., a systolic blood pressure fall of >20 mmHg on standing from lying [104]), be excluded. As noted, triggered cardiac conduction disturbances, e.g., via the trigemino-cardiac reflex, or the sick sinus syndrome, could be screened and excluded in robustly designed studies.
Patients’ medication should be carefully documented in all study participants and patients on drugs that may confound the results, be excluded. For example, opiates, beta-blockers, and calcium channel antagonists, all potentiate the trigemino-cardiac reflex, a potential confound as described above.
We would advise that patients with head and neck trauma be excluded given the scope for multiple vestibular diagnoses in TBI in whom there is a poor correlation between objective and subjective features. [4-6] In patients without a history of trauma and no evidence of deficit on neurological examination, the role for neck imaging in the inclusion or exclusion criteria seems limited, particularly since systematic reviews have found no consistent relationship between MR imaging of the cervical spine and neck pain. [105]
Once the exclusion criteria have been considered, the investigators should then consider the inclusion criteria. Neck pain and dizziness, both consistently and simultaneously aggravated by neck movements, seem a prerequisite. Investigators may then want to confirm if these symptoms are also triggered when the head is kept earth-fixed and the body rotated beneath the stationary head, since it is in this dynamic configuration that there is true neck movement without any head motion. Depending upon investigators’ a priori hypothesis of the mechanism mediating cervical dizziness, they may want to measure objective markers of vestibular activation (e.g., nystagmus or increased postural sway) during a provocatory manoeuvre. In this case, investigators may consider defining a priori, what is to be considered a positive result, e.g., a triggered nystagmus that is visible in at least 3 out of 5 trials (with clear definition for a triggered nystagmus). Some researchers may consider abnormal neck proprioception an inclusion-criteria, and depending upon their desired measure of neck proprioception, may require the development and validation of appropriate tests. Of course, whether researchers attempt some measure of neck proprioception may depend upon their a priori hypothesis mediating cervical dizziness but for investigators invoking a neck proprioception deficit, some measure of neck proprioception would seem essential. For some researchers, continuous cardiac monitoring during a provocatory manoeuvre (to exclude cardiogenic mechanisms for dizziness) may also be considered an important consideration.
The final consideration for researchers is the duration of follow-up in prospective interventional studies. A follow-up period of at least one year would seem sensible since at least one positive interventional study showing an early benefit of intervention over placebo, found that this benefit above placebo was not sustained at one year. [8, 98]
In summary, there are several confounds that make research into cervical dizziness challenging. Given the current data, we cannot at present, recommend any specific diagnostic criteria for cervical dizziness, nor can we presently recommend any specific therapy. We hope that investigators with a research interest in cervical dizziness can decrease the uncertainty over this putative clinical entity, by designing rigorous clinical trials via multi-centre, randomised, blinded, controlled studies.
References:
Barré J.A.
Sur un syndrome sympathique cervical postérieuret sa cause frequente, làrthrite cervicale
Revue Neurologique 1 (1926), 1246–1248.Ryan G. and Cope S.
Cervical vertigo
Lancet 269 (1955), 1355–1358.Sorensen B.F.
Bow hunter’s stroke
Neurosurgery 2(3) (1978).
doi: 10.1227/00006123-197805000-00013.Marcus H.J. , et al.
Vestibular Dysfunction in Acute Traumatic Brain Injury
J Neurol 2019 (Oct); 266 (10): 2430–2433Calzolari E. , et al.
Vestibular agnosia in traumatic brain injury and its link to imbalance
Brain 144(1) (2021), 128–143.
doi: 10.1093/brain/awaa386.Sargeant M. , et al.
The utility of the sports concussion assessment tool
in hospitalized traumatic brain injury patients
Journal of Concussion 2 (2018).
doi: 10.1177/2059700218808121.Karlberg M. , Magnusson M. , Malmstrfim E.-M. , Melander A. and Moritz U.
Postural and symptomatic improvement after physiotherapy in
patients with dizziness of suspected cervical origin, 1996.Reid S.A. , Rivett D.A. , Katekar M.G. and Callister R.
Comparison of mulligan sustained natural apophyseal glides and
maitland mobilizations for treatment of cervicogenic dizziness:
A randomized controlled trial
Physical Therapy 94(4) (2014), 466–476.
doi: 10.2522/ptj.20120483.Reid S.A. , Callister R. , Katekar M.G. and Rivett D.A.
Effects of cervical spine manual therapy on range of motion, head repositioning,
and balance in participants with cervicogenic dizziness: A randomized controlled trial
Archives of Physical Medicine and Rehabilitation 95(9) (2014), 1603–1612.
doi: 10.1016/j.apmr.2014.04.009.Brandt T. and Huppert D.
A new type of cervical vertigo: Head motion-induced spells in acute neck pain
Neurology 86(10) (2016), 974–975.
Lippincott Williams and Wilkins.
doi: 10.1212/WNL.0000000000002451.Thompson-Harvey A. and Hain T.C.
Symptoms in cervical vertigo
Laryngoscope Investigative Otolaryngology 4(1) (2019), 109–115.
doi: 10.1002/lio2.227.Bisdorff A. , von Brevern M. , Lempert T. and Newman-Toker D.E.
Classification of vestibular symptoms:
Towards an international classification of vestibular disorders
J Vestibular Research 19(1,2) (2009).
doi: 10.3233/VES-2009-0343.Furman J. , Cass S. and Whitney S. , Eds.
Balance Disorders: A Case-Study Approach.
Philadelphia, 1996.Hoy D, March L, Brooks P, et al.
The Global Burden of Low Back Pain:
Estimates from the Global Burden of Disease 2010 study
Ann Rheum Dis. 2014 (Jun); 73 (6): 968–974Ashina S, Bendtsen L, Lyngberg AC, Lipton RB, Hajiyeva N, Jensen R.
Prevalence of Neck Pain in Migraine and Tension-type Headache:
A Population Study
Cephalalgia. 2015 (Mar); 35 (3): 211–219Neuhauser H.K.
The epidemiology of dizziness and vertigo, (2016).
doi: 10.1016/B978-0-444-63437-5.00005-4.Corrales C.E. and Bhattacharyya N.
Dizziness and death: An imbalance in mortality
The Laryngoscope 126(9) (2016).
doi: 10.1002/lary.25902.Dix M.R. and Hallpike C.S.
LXXVIII the pathology, symptomatology and diagnosis of
certain common disorders of the vestibular system
Annals of Otology, Rhinology & Laryngology 61(4) (1952).
doi: 10.1177/000348945206100403.Shumway-Cook A. , Horak F. and Yardley L.
Rehabilitation of balance disorders in patients with vestibular pathology.
In: Balance posture and gait., 1st ed.
London, 1996.von Brevern M. , Zeise D. , Neuhauser H. , Clarke A.H. and Lempert T.
Acute migrainous vertigo: Clinical and oculographic findings
Brain 128(2) (2005), 365–374.
doi: 10.1093/brain/awh351.Ashton J.A. , Boddy A. , Dean S.R. , Milleret C. and Donaldson I.M.L.
Afferent signals from cat extraocular muscles in the medial vestibular nucleus,
the Nucleus praepositus hypoglossi and adjacent brainstem structures
Neuroscience 26(1) (1988).
doi: 10.1016/0306-4522(88)90132-7.Matesz C.
Termination areas of primary afferent fibers of the trigeminal nerve in the rat
Acta Bioloigica Hungarica 1 (1983), 31–44.McKelvey-Briggs D.K. , Saint-Cyr J.A. , Spence S.J. and Partlow G.D.
A reinvestigation of the spinovestibular projection in
the cat using axonal transport techniques
Anatomy and Embryology 180(3) (1989).
doi: 10.1007/BF00315886.Neuhuber W.L. and Zenker W.
Central distribution of cervical primary afferents in the rat,
with emphasis on proprioceptive projections to vestibular,
perihypoglossal, and upper thoracic spinal nuclei
The Journal of Comparative Neurology 280(2) (1989).
doi: 10.1002/cne.902800206.Bankoul S. and Neuhuber W.L.
A cervical primary afferent input to vestibular nuclei as demonstrated
by retrograde transport of wheat germ agglutinin-horseradish peroxidase in the rat
Experimental Brain Research 79(2) (1990).
doi: 10.1007/BF00608252.Buisseret-Delmas C. , Compoint C. , Delfini C. and Buisseret P.
Organisation of reciprocal connections between trigeminal
and vestibular nuclei in the rat
J Comp Neurol 409 (1999), 153–168.Barmack N.H.
Central vestibular system: Vestibular nuclei and posterior cerebellum
Brain Research Bulletin 60(5–6) (2003), 511–541.
Elsevier Inc. doi: 10.1016/S0361-9230(03)00055-8.Brown J.
Cervical contributions to balance: Cervical vertigo.
In: The Head Neck Sensory Motor System.
New York: Oxford University Press, 1992.Roy J.E. and Cullen K.E.
Dissociating self-generated from passively applied head motion:
Neural mechanisms in the vestibular nuclei
Journal of Neuroscience 24(9) (2004), 2102–2111.
doi: 10.1523/JNEUROSCI.3988-03.2004.Roy J.E. and Cullen K.E.
Selective processing of vestibular reafference during self-generated head motion
The Journal of Neuroscience 21(6) (2001).
doi: 10.1523/JNEUROSCI.21-06-02131.2001.Dale A. and Cullen K.E.
The ventral posterior lateral thalamus preferentially encodes externally
applied versus active movement: Implications for self-motion perception
Cerebral Cortex 29(1) (2019).
doi: 10.1093/cercor/bhx325.Brooks J.X. and Cullen K.E.
Early vestibular processing does not discriminate active from passive
self-motion if there is a discrepancy between predicted and actual proprioceptive feedback
Journal of Neurophysiology 111(12) (2014).
doi: 10.1152/jn.00600.2013.Jamali M. , Mitchell D.E. , Dale A. , Carriot J. , Sadeghi S.G. and Cullen K.E.
Neuronal detection thresholds during vestibular compensation:
Contributions of response variability and sensorysubstitution
The Journal of Physiology 592(7) (2014).
doi: 10.1113/jphysiol.2013.267534.Sadeghi S.G. , Minor L.B. and Cullen K.E.
Neural correlates of motor learning in the vestibulo-ocular reflex:
Dynamic regulation of multimodal integration in the macaque vestibular system
Journal of Neuroscience 30(30) (2010).
doi: 10.1523/JNEUROSCI.1368-10.2010.Sadeghi S.G. , Minor L.B. and Cullen K.E.
Multimodal integration after unilateral labyrinthine lesion:
Single vestibular nuclei neuron responses and implications for postural compensation
Journal of Neurophysiology 105(2) (2011).
doi: 10.1152/jn.00788.2010.Sadeghi S.G. , Minor L.B. and Cullen K.E.
Neural correlates of sensory substitution in vestibular pathways
following complete vestibular loss
Journal of Neuroscience 32(42) (2012).
doi: 10.1523/JNEUROSCI.2493-12.2012.Rancz E.A. , Moya J. , Drawitsch F. , Brichta A.M. , Canals S. and Margrie T.W.
Widespread vestibular activation of the rodent cortex
The Journal of Neuroscience 35(15) (2015).
doi: 10.1523/JNEUROSCI.1869-14.2015.Nigmatullina Y. , Hellyer P.J. , Nachev P. , Sharp D.J. and Seemungal B.M.
The neuroanatomical correlates of training-related
perceptuo-reflex uncoupling in dancers
Cerebral Cortex 25(2) (2015), 554–562.
doi: 10.1093/cercor/bht266.Zaeem H. , et al.
Vestibular Agnosia is linked to abnormal functional brain networks
bioRxiv (2021).
doi: 10.1101/2021.12.03.471139.Seemungal B.M. , Masaoutis P. , Green D.A. , Plant G.T. and Bronstein A.M.
Symptomatic recovery in miller fisher syndrome parallels
vestibular–perceptual and not vestibular–ocular reflex function
Frontiers in Neurology 2 (2011).
doi: 10.3389/fneur.2011.00002.Nigmatullina Y. , Arshad Q. , Wu K. , Seemungal B. , Bronstein A. and Soto D.
How imagery changes self-motion perception
Neuroscience 291 (2015), 46–52.
doi: 10.1016/j.neuroscience.2015.01.021.zu Eulenburg P. , Stoeter P. and Dieterich M.
Voxel-based morphometry depicts central compensation after vestibular neuritis
Annals of Neurology 68(2) (2010).
doi: 10.1002/ana.22063.Cousins S. , et al.
Visual dependency and dizziness after vestibular neuritis
PLoS ONE 9(9) (2014).
doi: 10.1371/journal.pone.0105426.Jong P.T.V.M. , Vianney de Jong J.M.B. , Cohen B. and Jongkees L.B.W.
Ataxia and Nystagmus Induced by Injection of Local Anesthetics in the Neck.Castelão M. , et al.
Botulinum toxin type A therapy for cervical dystonia
Cochrane Database of Systematic Reviews (2017).
doi: 10.1002/14651858.CD003633.pub3.Holtmann S. , Reiman V. and Schöps P.
Zur klinischen bedeutung zerviko-okulärer reaktionen
Laryngo-Rhino-Otologie 72(06) (1993).
doi: 10.1055/s-2007-997906.Bronstein A.M. and Derrick Hood J.
The cervico-ocular reflex in normal subjects and patients
with absent vestibular function
Brain Research 373(1–2) (1986).
doi: 10.1016/0006-8993(86)90355-0.Popov K.E. , Lekhel H. , Faldon M. , Bronstein A.M. and Gresty M.A.
Visual and oculomotor responses induced by neck vibration
in normal subjects and labyrinthine-defective patients
Experimental Brain Research 128(3) (1999).
doi: 10.1007/s002210050854.Schubert M.C. , Das V. , Tusa R.J. and Herdman S.J.
Cervico-ocular reflex in normal subjects and patients with
unilateral vestibular hypofunction
Otology & Neurotology 25(1) (2004).
doi: 10.1097/00129492-200401000-00013.Bronstein A.M.
Plastic changes in the human cervicoocular reflex, Sensing and C
Annals of the New York Academy of Sciences 656(1) (1992).
doi: 10.1111/j.1749-6632.1992.tb25248.x.Eva-Maj M. , Hans W. , Per-Anders F. , Mikael K. and Måns M.
Experimentally induced deep cervical muscle pain distorts
head on trunk orientation
European Journal of Applied Physiology 113(10) (2013), 2487–2499.
doi: 10.1007/s00421-013-2683-y.Brandt Th. , Büchele W. and Arnold F.
Arthrokinetic nystagmus and ego-motion sensation
Experimental Brain Research 30–30(2–3) (1977).
doi: 10.1007/BF00237260.Seemungal B.M. , Gunaratne I.A. , Fleming I.O. , Gresty M.A. and Bronstein A.M.
Perceptual and nystagmic thresholds of vestibular function in yaw
Journal of Vestibular Research 14 (2004), 461–466.Hadi Z. , elena Calzolari , Pondeca Y. , Sharp D. , Mahmud M. and Seemungal B.
The brain networks mediating vestibular self-motion perception
Journal of Neurological Sciences,
In Press. doi: 10.1016/j.jns.2022.120458.Guedry F.E.
Psychophysics of Vestibular Sensation, 1974.
doi: 10.1007/978-3-642-65920-1_1.Staab J.P. , et al.
Diagnostic criteria for persistentpostural-perceptual dizziness (PPPD):
Consensus document of thecommittee for the Classification
of Vestibular Disorders of the Bárány Society
Journal of Vestibular Research 27(4) (2017).
doi: 10.3233/VES-170622.Seemungal B.M. and Passamonti L.
Persistent postural-perceptual dizziness: A useful new syndrome
Practical Neurology 18(1) (2018).
doi: 10.1136/practneurol-2017-001817.Espay A.J. , et al.
Current concepts in diagnosis and treatment
of functional neurological disorders
JAMA Neurology 75(9) (2018).
doi: 10.1001/jamaneurol.2018.1264.Beinert K. , Preiss K. , Huber M. and Taube W.
Cervical joint position sense in neck pain. Immediate effects
of muscle vibration versus mental training interventions:
An RCT
Eur J Phys Rehab Med 52 (2015), 825–832.Seemungal B.M.
The cognitive neurology of the vestibular system
Current Opinion in Neurology 27(1) (2014).
doi: 10.1097/WCO.0000000000000060.+Lempert T. , et al.
Vestibular migraine: Diagnostic criteria
J Vestibular Research: Equilibrium and Orientation 22(4) (2012), 167–172.
doi: 10.3233/VES-2012-0453.von Brevern M. , Zeise D. , Neuhauser H. , Clarke A.H. and Lempert T.
Acute migrainous vertigo: Clinical and oculographic findings
Brain 128(2) (2005), 365–374.
doi: 10.1093/brain/awh351.Goadsby P.J.
Cervicogenic headache:
A pain in the neck for some neurologists?
The Lancet Neurology 8(10) (2009).
doi: 10.1016/S1474-4422(09)70243-1.Karsan N. and Goadsby P.J.
Biological insights from the premonitory symptoms of migraine
Nature Reviews Neurology 14(12) (2018).
doi: 10.1038/s41582-018-0098-4.Schoonman G. , Evers D. , Terwindt G. , van Dijk J. and Ferrari M.
The prevalence of premonitory symptoms in migraine:
A questionnaire study in 461 patients
Cephalalgia 26(10) (2006).
doi: 10.1111/j.1468-2982.2006.01195.x.Lempert T. and Seemungal B.M.
How to define migraine with brainstem aura?
Brain 143(5) (2020).
doi: 10.1093/brain/awaa077.Marano E. , et al
Trigeminal stimulation elicits a peripheral vestibular
imbalance in migraine patients
Headache: The Journal of Head and Face Pain 45(4) (2005).
doi: 10.1111/j.1526-4610.2005.05069.x.Bogduk N. and Govind J.
Cervicogenic headache: An assessment of the evidence on
clinical diagnosis, invasive tests, and treatment
The Lancet Neurology 8(10) (2009), 959–968.
doi: 10.1016/S1474-4422(09)70209-1.Piovesan E.J. , Kowacs P.A. and Oshinsky M.L.
Convergence of cervical and trigeminal sensory afferents
Current Pain and Headache Reports 7(5) (2003).
doi: 10.1007/s11916-003-0037-x.Bartsch T. and Goadsby P.J.
Increased responses in trigeminocervical nociceptive neurons
to cervical input after stimulation of the dura mater
Brain 126(8) (2003).
doi: 10.1093/brain/awg190.Bartsch T. and Goadsby P.
Stimulation of the greater occipital nerve induces
increased central excitability of dural afferent input
Brain 125(7) (2002).
doi: 10.1093/brain/awf166.Freppel S. , et al.
Visuo-proprioceptive interactions in degenerative cervical
spine diseases requiring surgery
Neuroscience 255 (2013).
doi: 10.1016/j.neuroscience.2013.09.060.Baron E.P. , Cherian N. and Tepper S.J.
Role of greater occipital nerve blocks and trigger point injections
for patients with dizziness and headache
Neurologist 17(6) (2011), 312–317.
doi: 10.1097/NRL.0b013e318234e966.Inan L.E. , et al.
Greater occipital nerve blockade for the treatment of chronic migraine:
A randomized, multicenter, double-blind, and placebo-controlled study
Acta Neurologica Scandinavica 132(4) (2015), 270–277.
doi: 10.1111/ane.12393.Ambrosini A. , et al.
Suboccipital injection with a mixture of rapid- and long-acting
steroids in cluster headache: A double-blind placebo-controlled study
Pain 118(1) (2005), 92–96.
doi: 10.1016/j.pain.2005.07.015.Afridi S.K. , Shields K.G. , Bhola R. and Goadsby P.J.
Greater occipital nerve injection in primary headache syndromes –
prolonged effects from a single injection
Pain 122(1) (2006), 126–129.
doi: 10.1016/j.pain.2006.01.016.Buisseret-Delmas C. , Compoint C. , Delfini C. and Buisseret A.P.
Organisation of Reciprocal Connections Between Trigeminal and
Vestibular Nuclei in the Rat Indexing terms: Sensory
trigeminal system; anterograde/retrograde tracing;
morphometry, (1999).
doi: 10.1002/(SICI)1096-9861(19990621)409:1<153:
:AID-CNE11>3.0.CO;2.Schaller B. , Chowdhury T. and Rosemann T.
Editorial: The trigeminocardiac reflex: Beyond the diving reflex
Frontiers in Neuroscience 11(DEC) (2017).
Frontiers Media S.A.,
doi: 10.3389/fnins.2017.00673.Lapi D. , Scuri R. and Colantuoni A.
Trigeminal cardiac reflex and cerebral blood flow regulation
Frontiers in Neuroscience 10(OCT) (2016).
Frontiers Media S.A.,
doi: 10.3389/fnins.2016.00470.Morinaka S.
Musculoskeletal diseases as a causal factor of cervical vertigo
Auris Nasus Larynx 36(6) (2009), 649–654.
doi: 10.1016/j.anl.2009.04.009.Rottach K.G. , Wohlgemuth W.A. , Dzaja A.E. , Eggert T. and Straube A.
Effects of intravenous opioids on eye movements in humans: Possible mechanisms
Journal of Neurology 249(9) (2002).
doi: 10.1007/s00415-002-0806-1.Sadoshima S. and Heistad D.D.
Regional cerebral blood flow during hypotension in normotensive
and stroke-prone spontaneously hypertensive rats:
Effect of sympathetic denervation
Stroke 14(4) (1983).
doi: 10.1161/01.STR.14.4.575.Mueller S.M. , Heistad D.D. and Marcus M.L.
Total and regional cerebral blood flow during hypotension, hypertension,
and hypocapnia. Effect of sympathetic denervation in dogs
Circulation Research 41(3) (1977).
doi: 10.1161/01.RES.41.3.350.Foster C.A. and Jabbour P.
Barré–Lieou syndrome and the problem of the obsolete eponym
The Journal of Laryngology & Otology 121(7) (2007).
doi: 10.1017/S002221510600346X.Bolton P.S. and Ray C.A. , PII S0361-9230(00)00307-5
Neck afferent involvement in cardiovascular control during movement, 2000.Peng B. and Li Y.
Pathogenesis, diagnosis, and treatment of cervical vertigo,
2015. [Online]. Available:
www.painphysicianjournal.comwww.painphysicianjournal.comRen L. , et al.
Mid-term efficacy of percutaneous laser disc
decompression for treatment of cervical vertigo
European Journal of Orthopaedic Surgery & Traumatology 24(S1) (2014).
doi: 10.1007/s00590-013-1264-4.Yaseen K, Hendrick P, Ismail A, Felemban M, Alshehri MA (2018)
The Effectiveness of Manual Therapy in Treating
Cervicogenic Dizziness: A Systematic Review
J Phys Ther Sci 2018 (Jan); 30 (1): 96-102Reid S.A. , Rivett D.A. , Katekar M.G. and Callister R.
Sustained natural apophyseal glides (SNAGs) are an
effective treatment forcervicogenic dizziness
Manual Therapy 13(4) (2008), 357–366.
doi: 10.1016/j.math.2007.03.006.Reid S, Rivett D.
Manual Therapy Treatment of Cervicogenic Dizziness: A Systematic Review
Manual Therapy 2005 (Feb); 10 (1): 4–13Malmström E.M. , Karlberg M. , Melander A. , Magnusson M. and Moritz U.
Cervicogenic dizziness - Musculoskeletal findings
before and after treatment and long-term outcome
Disability and Rehabilitation 29(15) (2007), 1193–1205.
doi: 10.1080/09638280600948383.Yaseen K. , HendricK P. , Ismail A. , Felemban M. and Abdullah Alshehri M.
The effectiveness of manual therapy in treating
cervicogenic dizziness: A systematic review, (2018), 96–102.
doi: 10.1589/jpts.30.96.Peng B. , Yang L. , Yang C. , Pang X. , Chen X. and Wu Y.
The effectiveness of anterior cervical decompression and fusion
for the relief of dizziness in patients with cervical spondylosis
The Bone & Joint Journal 100-B(1) (2018).
doi: 10.1302/0301-620X.100B1.BJJ-2017-0650.R2.Wetzler G. , Roland M. , Fryer-Dietz S. and Dettmann-Ahern D.
Cranio Sacral therapy and visceral manipulation:
A new treatment intervention for concussion recovery
Medical Acupuncture 29(4) (2017), 239–248.
doi: 10.1089/acu.2017.1222.Moustafa
The effect of normalizing the sagittal cervical configuration on dizziness
Europ J Physical and Rehab Med 2017.Bittar R. , Alves N.G.P. , Bertoldo C. , Brugnera C. and Oiticica J.
Efficacy of carbon microcoils in relieving cervicogenic dizziness
International Archives of Otorhinolaryngology 21(1) (2017), 4–7.
doi: 10.1055/s-0036-1592418.Minguez-Zuazo A. , Grande-Alonso M. , Saiz B.M. , la Touche R. and Lara S.L.
Therapeutic patient education and exercise therapy in patients
with cervicogenic dizziness: A prospective case series clinical study
Journal of Exercise Rehabilitation 12(3) (2016), 216–225.
doi: 10.12965/jer.1632564.282.Reid S.A. , Callister R. , Snodgrass S.J. , Katekar M.G. and Rivett D.A.
Manual therapy for cervicogenic dizziness:
Long-term outcomes of a randomised trial
Manual Therapy 20(1) (2015), 148–156.
doi: 10.1016/j.math.2014.08.003.Humphries K.M. , Ward J. , Coats J. , Nobert J. , Amonette W. and Dyess S.
Immediate effects of lower cervical spine manipulation on
handgrip strength and free-throw accuracy of asymptomatic
basketball players: A pilot study
Journal of Chiropractic Medicine 12(3) (2013), 153–159.
doi: 10.1016/j.jcm.2013.10.008.Strunk R, Hawk C.
Effects of Chiropractic Care on Dizziness, Neck Pain, and Balance:
A Single-group, Preexperimental, Feasibility Study
J Chiropractic Medicine 2009 (Dec); 8 (4): 156–164Heikkilä H. , Johansson M. and Wenngren B.I.
Effects of Acupuncture, Cervical Manipulation and NSAID Therapy on
Dizziness and Impaired Head Repositioning of Suspected Cervical Origin:
A Pilot Study
Manual Therapy 2000 (Aug); 5 (3): 151–157Mulligan B.
Vertigo...manual therapy may be needed,
+In: Manipulative Physiotherapists Association of Australia 7th Biennial Conference,
1991, pp. 46e7-undefined.Hengeveld E. and Banks K. , Maitland’s Vertebral Manipulation, 2001.
Consensus statement on the definition of orthostatic hypotension,
pure autonomic failure, and multiple system atrophy
Neurology 46(5) (1996).
doi: 10.1212/WNL.46.5.1470.Hill L. , et al.
Do findings identified on magnetic resonance imaging predict future neck pain? A systematic review
Spine Journal 18(5) (2018).
Elsevier Inc., 880–891.
doi: 10.1016/j.spinee.2018.01.025.
Return to VERTIGO and/or BALANCE
Since 11-23-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |