

A Retrospective Analysis of Pain Changes
and Opioid Use Patterns Temporally Associated
with a Course of Chiropractic Care at a
Publicly Funded Inner-city FacilityThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Can Chiropr Assoc 2022 (Aug); 66 (2): 107–117 ~ FULL TEXT
OPEN ACCESS Steven Passmore, Hons BKin, MS, DC, PhD, Quinn Malone, BSc, MSc1, Christian Manansala, BSc, DC, MSc, Spencer Ferbers, BSc, E. Audrey Toth, DC, Gerald M. Olin, BSc, DC, CDir
Faculty of Kinesiology and Recreation Management,
University of Manitoba,
102- Frank Kennedy Centre,
420 University Crescent,
Winnipeg, MB, R3T 2N2 Canada
FROM: Kazis et. al, BMJ Open 2019Background: Non-pharmacologic treatment, including chiropractic care, is now recommended instead of opioid prescriptions as the initial management of chronic spine pain by clinical practice guidelines. Chiropractic care, commonly including spinal manipulation, has been temporally associated with reduced opioid prescription in veterans with spine pain.
Purpose: To determine if chiropractic management including spinal manipulation was associated with decreased pain or opioid usage in financially disadvantaged individuals utilizing opioid medications and diagnosed with musculoskeletal conditions.
Methods: A retrospective analysis of quality assurance data from a publicly funded healthcare facility was conducted. Measures included numeric pain scores of spine and extremity regions across three time points, opioid utilization, demographics, and care modalities.
Results: Pain and opioid use significantly decreased concomitant with a course of chiropractic care.
Conclusions: A publicly funded course of chiropractic care temporally coincided with statistically and clinically significant decreases in pain and opioid usage in a financially disadvantaged inner-city population.
Keywords: analgesics, back pain, chiropractic, chronic pain, low-income population, musculoskeletal manipulations, musculoskeletal pain, opioid, single-payer system, spine
] and is a viable first line treatment option prior to the use of opioid prescription medication. Additionally, many individuals with chronic non-cancer pain (46%) seek chiropractic as a treatment option. [32] Chiropractic care is congruent with recommendations from both the American College of Physicians11 and Canadian Chiropractic Guideline Initiative [13] because it has demonstrated positive outcomes for spinal pain and has been associated with safety, cost effectiveness, and reductions in opioid use. [12–14, 33–35]
From the FULL TEXT Article:
Introduction
Since 1994, there has been a 4–fold increase in opioid prescription in the United States and long-term opioid use has become a major public health concern. [1, 2] In recent years there has been a decrease in opioid prescription for chronic pain; [3] however, opioid prescription for back pain remains high [4–6], and prescription rates in the US and Canada are two or three times higher than in most European countries. [4] This is problematic because of the high incidence of addiction and overdose related deaths associated with opioid use and the paucity of evidence that opioids actually aid those suffering from chronic musculoskeletal conditions, such as back pain. [7–9 ] Opioid medications impair the ability to engage in activities of daily living [5] and are no more effective than alternative treatments for pain-related dysfunction [10], creating financial and quality of life challenges. While there may be situations where opioid medication prescription is clinically necessary; for those patients with chronic, non-cancer conditions such as those suffering from musculoskeletal conditions including back and neck pain; there are other options that are recommended by clinical practice guidelines (CPGs). [11–14]
Back pain has been cited as the leading cause of activity limitation and work disability worldwide and has become one of the most common reasons for seeking care. [6, 15–17] Most adults will experience back pain at some point in their life18 and total costs associated with back pain are estimated as high as $100 billion per year in the United States [11, 19] and $6–$12 billion per year in Canada. [13] People afflicted with back pain tend to have significantly higher health care utilization and costs. [6, 20] Additionally, studies have provided evidence that more expensive therapies and diagnosis techniques do not result in better patient outcomes. [20–22] Given the ballooning costs of healthcare systems around the world, health policy stakeholders, such as governmental policy makers, clinicians, governing bodies of healthcare professions, insurance companies, workers’ compensation groups, and the general public, should consider more affordable, cost-efficient, and effective approaches for the management back pain that are congruent with CPGs.
According to recent CPGs, a trial of non-pharmacologic care should be considered as a first line treatment for those suffering back pain. Spinal manipulative therapy (SMT) is one such recommended treatment option. [11–14, 23, 24] Spinal manipulative therapy has been demonstrated to be a cost-effective treatment option for the management of back pain [25–28] and results in high reported levels of patient satisfaction. [29–31] Chiropractic care, which involves spinal manipulation and adjunctive therapies, is consistent with recent CPGs [11–14]
Unfortunately, low-income individuals may not have equitable access to chiropractic care as a treatment option. In the Canadian healthcare system, individuals with incomes below a certain point are compensated for any prescription drugs they purchase by provincial pharmaceutical programs, while full reimbursement for chiropractic care is not currently covered. While more affluent individuals may access chiropractic care through third party insurance or out-of-pocket payments, low-income individuals may be unable to access such CPG recommended treatment options. Low-income individuals are therefore unable to access chiropractic care due to financial barriers even though it is a less expensive and less harmful form of treatment than prescription opioids. An investigation of whether a low-income demographic benefits from a course of chiropractic care would help to demonstrate if extending equitable access to this form of therapy is warranted. With the present opioid crisis, SMT should be considered as a possible treatment option for patients to transition from opioid prescriptions or illicit use towards more effective and less harmful pain management options such as chiropractic.
The purpose of this study was to investigate opioid utilization and musculoskeletal pain rating among low-income patients receiving chiropractic care in a publicly funded healthcare system. It was our hypothesis that such individuals would decrease their opioid use concomitant with decreased pain intensity ratings associated with a course of chiropractic care.
Methods
Ethics approval for this study was granted by the University of Manitoba Health Research Ethics Board.
Study design
The study was a retrospective review of prospectively collected quality assurance data obtained from the chiropractic program database of a publicly funded clinic.
Setting
All information collected for this study was obtained from a publicly funded clinic in Winnipeg, Manitoba with integrated on-site chiropractic services. The data used for this study is securely maintained at the publicly funded clinic by the treating clinicians on site. Patient data was completely de-identified upon entry to an anonymized database prior to analysis and interpretation.
Patients and variables

Table 1

Table 4
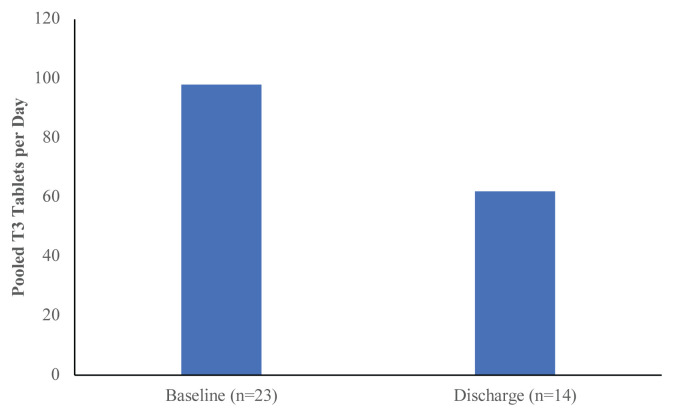
Figure 2 The data was collected between January 2011 to December 2017. Inclusion criteria for database review included patients identified/indicated as having: (a) experienced pain >3 months duration, (b) a history of opioid utilization at admission or during their care, and (c) received a course of chiropractic care. Eligibility for chiropractic treatment included: (a) residence in a pre-identified low-income neighbourhood, and (b) lack healthcare insurance coverage for chiropractic care. Immigrants and refugees to Canada living in pre-determined geographic locales for less than three years and individuals who did not have a standing claim involving an automobile injury claim or Workers Compensation Board funding who were referred by partner programs/organizations also received care and were included in this analysis. The eligibility for chiropractic treatment, and therefore the focus on low-income individuals, was determined by the treatment and data collection site, which is dedicated to providing healthcare services to economically disadvantaged individuals in Winnipeg, Manitoba. Sociodemographic information derived from the eligible patient database entries is provided in Table 1.
Independent variables included the pain site and time point. Pain sites were indicated according to their anatomical site as follows: cervical spine (CS), thoracic spine (TS), lumbar spine (LS), sacroiliac region (SI), and extremity (EXT). Time points included: baseline (BL) which was the time of first treatment, visit 5 (V5), and discharge (DIS). Dependent variables included pain level, opioid use at baseline/discharge, and the number of Tylenol 3 (T3) pills used per day. Pain level experienced at each symptomatic site was assessed by a numeric rating scale (NRS), an 11–point Likert scale with 0 representing “no pain” and 10 representing “worst pain imaginable.” [36] The minimally clinically important difference (MCID) was determined to be 2–points on the pain rating Likert scale. [11] The number of patients using opioids at BL, DIS, or neither was reported (Table 4). If the opioid being used at BL or DIS was T3, the number of T3 tablets utilized per day was reported (Figure 2).
Bias
This study was funded by the Canadian Chiropractic Association (CCA). However, the CCA had no influence over the reported results, data reduction, analysis, or statistical modelling. Statistical tests were performed by an individual who had no contact with the granting organization directly or indirectly throughout the process. Another source of bias may have occurred from patients refusing to disclose or misreporting their own opioid use.
Chiropractic treatment methods and frequency
Patients receiving chiropractic treatment underwent a history and physical examination followed by a course of pragmatic care as determined by the attending chiropractors. Follow up visits during a course of care consisted of; diversified spinal or extremity joint manipulation and/or mobilization, soft tissue therapy, acupuncture, and/or other modalities, including but not limited to ultrasound, electrical stimulation, thermal treatment`, exercise, home advice, and Kinesiotaping, when clinically indicated. All aforementioned treatments were delivered by a licensed chiropractor. Re-evaluation visits were scheduled after every four to six treatment visits to assess response to care. New patient assessments were scheduled for 30 to 60 minutes, while treatment visits and re-evaluation visits were 15 to 30 minutes in duration.
Statistical analyses
Descriptive analyses included demographic and treatment modality means and standard deviations, as well as the number of patients and their percentage change in T3 tablets taken per day for the subset of patients with T3 prescriptions over the course of chiropractic care. Analyses were conducted using jamovi (The jamovi project, v. 0.9). All analyzed outcomes were calculated as p-values and the level of significance was set to α=0.05. One-way repeated measures analysis of variance (ANOVA) models (3 timepoints – baseline, visit 5, discharge) were used to establish main effects for time under care at each pain site, after which Tukey’s honestly significant differences was used to determine the location of main effects. McNemar’s test was used to analyze the difference in opioid utilization rates at baseline and discharge.
Results
Patients
Out of the 482 patients treated by the chiropractic program in the analyzed timeframe (January 2011 to December 2017) at the publicly funded clinic, 62 individuals met the inclusion criteria. Out of the eligible patients, 67.7% were referred by their Primary Care Provider (PCP) to the onsite chiropractic program. The majority of study participants were woman (61.3%), who self-identified as Caucasian (48.4%), with a mean age of 48.6, SD=13.6 years old, and a BMI of 31.6, SD=8.5 kg/m2 (obese). The most commonly reported painful spinal complaints were in the lumbar (80.6%), sacral (66.1%) and thoracic (64.5%) regions. The overwhelming majority of patients had pain in multiple regions, specifically: 14 out of 62 patients had pain in two regions, 17 had pain in three regions, 14 had pain in four regions and 16 had pain in five regions. At the end of their course of chiropractic care, 8.1% of patients were referred back to their PCP for alternate treatment consideration. As a result, 91.9% of chiropractic patients using opioids were able to be discharged without further referral for their musculoskeletal spine pain following a course of chiropractic care (Table 1).

Table 2 Thirty-three of the opioid using patients utilized a singled course of chiropractic care, which allowed us to confirm specific start and end dates of the course of care. The average duration of that course of care was M=15.77 weeks, SD=17.40 weeks; with M =16.38 treatment visits, SD=16.70 treatment visits over that period of time. A limitation of the dataset is that the number of weeks in a course of care is not possible to determine when multiple courses of care are engaged in by a single patient. For all patients with opioid medication prescriptions, dosage, onset, and offset of medication was guided by the prescribing physician. A breakdown of care modalities employed is shown in Table 2.
Pain by region and time point

Figure 1

Table 3

Table 4 We observed a statistically and clinically significant decrease in pain level over a course of care from baseline compared to visit 5 and baseline compared to time of discharge for patients using opioid medications. Pain was reduced by amounts exceeding minimally clinically important differences (MCID) in all anatomical regions. The MCID was determined to be 2–points on the pain rating Likert scale.11 Mean reported pain between BL and V5 pain changed by –2.50 (CS), –3.15 (TS), –2.72 (LS), –2.97 (SI), and –3.48 (EXT); between BL and DIS, pain changed by –2.63 (CS), –3.11 (TS), –3.56 (LS), –3.72 (SI), and –3.78 (EXT). Between V5 and DIS, further pain changes were no longer statistically significant, though trends toward further reductions were seen, with the exception of the thoracic region: –0.125 (CS), 0.037 (TS), –0.844 (LS), –0.750 (SI), and –0.304 (EXT), respectively (Figure 1; Table 2). Main effects for time were found in the ANOVA for each anatomical region. Post-hoc analysis revealed that the BL timepoint was different from V5 and DIS, while there were no significant differences between V5 and DIS in any comparison (Table 3).
Opioid usage by time point
A significant number of people who utilized opioids at BL no longer did at DIS (n=15). Although some people who did not use opioids at BL did at DIS (n=4), McNemar’s test revealed that the number of people who stopped using opioids during the study period was significantly greater than those who began (p=0.012) (Table 4). Therefore, there was a significant decrease in the number of people who used opioids at DIS compared to BL. This translated into a 59.0% reduction in the number of patients using opioids after progressing through a course of chiropractic care (Table 4).
Tylenol 3 tablet usage per 24–hour period
Tylenol 3 tablets (T3 – 30mg of codeine phosphate) were the most commonly prescribed opioid for the chiropractic clinic patients between BL and DIS. At BL the pooled daily usage of T3 tablets was 98 tablets per day based on a sample size of 23 patients. At DIS the pooled daily usage of T3 tablets reduced to 62 tablets per day. There was a 36.7% reduction in usage (number of tablets per 24–hour period, excluding PRN [pro re nata, or “at will”] prescriptions) following a course of chiropractic care. Upon closer examination, the relationship is linked to the number of patients continuing to be on a T3 prescription. Individuals taking T3 were consuming about the same amount on average per person at the start and the end of care (98 tablets/23 people=4.26 tablets per person, 62 tablets/14 people=4.43 tablets per person), but overall fewer people 14/23 =60.9% (a 39.1% reduction) remained on T3 by the end of a course of care.
Discussion
The hypothesis of this study; that low-income individuals would experience decreased pain and a reduced rate of opioid utilization after a course of chiropractic care; is supported by the present results. Pain decreased over a course of care, with statistically and clinically significant differences being observed after five visits for every anatomical pain region examined and treated. The sample considered in this study was more likely to have ceased their opioid usage at discharge than to have commenced opioid utilization over that course of care. Nearly 40% fewer individuals used Tylenol 3 at the end of their course of care compared to their baseline.
A population frequently exposed to opioid medications are those with spinal pain, specifically low back pain. Usual medical care for low back pain patients is not consistent with CPG recommendations. Studies report up to 30% of patients who see their family physician with low back pain receive opioid prescriptions and 60% of patients reporting to the Emergency Department with low back pain do as well. [37] This indicates the overuse of opioid prescription in these settings. The low-income population is a group that is inordinately at risk of opioid addiction and mortality following exposure through prescription. [38] A potential solution to consider for patients with chronic spinal pain is a course of chiropractic care, a non-pharmacological healthcare intervention. A recent review by Corcoran suggested that those utilizing chiropractic services had 64% lower odds of being prescribed opioid medications compared to people not utilizing chiropractic services. [35] The results of the present study and those referenced above suggest that enabling economically disenfranchised people to have access to chiropractic services may reduce pain and may reduce opioid use.
The present study was conducted in an environment that alleviated the financial barrier for access to chiropractic care through public funding from a provincial government in Canada. The results observed were that a course of chiropractic treatment for those who utilized opioids occurred concomitantly with a statistically and clinically significant decrease in patient reported chronic pain. Most cases (91.9%) did not require further referral to another healthcare provider upon discharge from chiropractic care, providing evidence that most musculoskeletal pain issues were resolved to a point where the patients no longer sought additional healthcare services for their musculoskeletal pain at the end of the course of care. A low rate of further referral to other healthcare disciplines following a course of chiropractic care is in agreement with previously published studies. [39] Chiropractic management has been shown to be a relatively cost-effective non-pharmacological treatment for back pain. [26, 28] Not requiring further referral in most cases and a decrease in chronic pain intensity after a brief course of care provide evidence that chiropractic management is potentially a cost-efficient and effective treatment option to consider for integration into publicly funded health systems. [39]
There are limitations to the current study. As this is a retrospective analysis and patients were not randomized to a chiropractic care or control group, causation is not possible to determine using this design. The lack of control over additional comorbidity and life circumstances of the sample population mean that unpredicted factors may have impacted patient outcomes. The population is somewhat heterogenous, in that while all patients utilized opioid medications, some patients were prescribed opioid medications, while others admitted self-medicating with opioids that were not attained through prescription or legal sources. A limitation of the dataset is that the number of weeks in a course of care is not possible to determine when multiple courses of care are engaged in by a single patient. Additionally, the use of a design that does not require a control group means that the effects of time or other interventions were not controlled for.
This also includes not being able to control for the updated opioid prescribing guidelines for chronic pain in Canada that were introduced in 2011, and were updated in 2017. [40, 41] Given that chronic pain may fluctuate over time, but is not likely to spontaneously resolve, and the treatments offered were congruent with CPG recommendations, [11] the improvements observed are promising and should not be discounted; they can be a catalyst for further prospective study.
Conclusions
The results of the present study found a statistically and clinically significant pain reduction concomitant with publicly funded chiropractic management in a low-income population who utilized opioids. Additionally, a reduction in opioid use, compared to baseline, was found following a course chiropractic management at a multidisciplinary healthcare facility where the majority of patient referrals came from primary care physicians, and resulted in an endpoint of musculoskeletal care for the majority of individuals treated by the onsite chiropractors.
Acknowledgements
The authors would like to acknowledge the support of the Mount Carmel Clinic for providing the database records used to perform this study and the Canadian Chiropractic Association for providing grant support for the project. The granting agency had no impact or input on the design, analysis methods selected, results, or interpretation.
Availability of data and materials
The data underlying this article were provided by the Mount Carmel Clinic with permission. Data will be shared on request by the corresponding author with the permission of the Mount Carmel Clinic.
References:
Henk HJ, et al.
Opioid prescribing for opioid-naive patients in emergency departments
and other settings: characteristics of prescriptions and association with longterm use.
Ann Emerg Med. 2018;71(3): 326-336.e19.Paulozzi LJ, Mack KA, Hockenberry JM.
Vital signs: variation among states in prescribing of opioid
pain relievers and benzodiazepines -- United States, 2012.
Morbid Mortal Weekly Rep. 2014;63(26): 563–568.Salvatore PP, Guy GP, Mikosz CA.
Changes in opioid dispensing by medical specialties after release
of the 2016 CDC guideline for prescribing opioids for chronic pain.
Pain Med. 2022: pnac068. doi: 10.1093/pm/pnac068. Epub ahead of print.Deyo RA, Von Korff M, Duhrkoop D.
Opioids for low back pain.
BMJ (Online). 2015;350.Hudson TJ, Edlund MJ, Steffick DE, Tripathi SP, Sullivan MD.
Epidemiology of regular prescribed opioid use:
results from a national, population-based survey.
J Pain Symptom Management. 2008;36(3): 280–288.Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al.
Expenditures and Health Status Among Adults With Back and Neck Problems
JAMA 2008 (Feb 13); 299 (6): 656–664Gwira Baumblatt JA, Wiedeman C, Dunn JR, Schaffner W, Paulozzi LJ, Jones TF.
High-risk use by patients prescribed opioids for pain
and its role in overdose deaths.
JAMA Int Med. 2014;174(5): 796–801.Gomes T, Mamdani MM, Dhalla IA, Michael Paterson J, Juurlink DN.
Opioid dose and drug-related mortality in patients with nonmalignant pain.
Arch Int Med. 2011;171(7):686–691.Ross M.
Opioids for chronic pain.
Can Med Assoc J. 2018;190(9): E269.Krebs EE, Gravely A, Nugent S, Jensen AC, DeRonne B, Goldsmith ES, et al.
Effect of opioid vs nonopioid medications on pain-related function
in patients with chronic back pain or hip or knee osteoarthritis pain the SPACE randomized clinical trial.
J Am Med Assoc. 2018;319(9): 872–882.Qaseem, A, Wilt, TJ, McLean, RM, and Forciea, MA.
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Bussières, AE, Stewart, G, Al Zoubi, F et al.
The Treatment of Neck Pain-Associated Disorders and
Whiplash-Associated Disorders: Clinical Practice Guideline
J Manipulative Physiol Ther. 2016 (Oct); 39 (8): 523–564Bussieres AE, Stewart G, Al-Zoubi F, Decina P, Descarreaux M, Haskett D, Hincapie C, et al.
Spinal Manipulative Therapy and Other Conservative Treatments for Low Back Pain:
A Guideline From the Canadian Chiropractic Guideline Initiative
J Manipulative Physiol Ther. 2018 (May); 41 (4): 265–293Andronis L, Kinghorn P, Qiao S, Whitehurst DG, Durrell S, McLeod H.
Cost-Effectiveness of Non-Invasive and Non-Pharmacological Interventions
for Low Back Pain: A Systematic Literature Review
Applied Health Econ and Health Policy 2017 (Apr); 15 (2): 173–201Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J et al.
What Low Back Pain Is and Why We Need to Pay Attention
Lancet. 2018 (Jun 9); 391 (10137): 2356–2367
This is the second of 4 articles in the remarkable Lancet Series on Low Back PainHoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al.
The Global Burden of Low Back Pain:
Estimates from the Global Burden of Disease 2010 study
Annals of Rheumatic Diseases 2014 (Jun); 73 (6): 968–974Andersson GBJ.
Epidemiological features of chronic lowback pain.
Lancet. 1999;354: 581–585.Cassidy JD, Co P, Carroll LJ, Kristman V.
Incidence and course of lower back pain in the general population.
Spine. 2005;30(24): 1–7.Katz JN.
Lumbar disc disorders and low-back pain:
Socioeconomic factors and consequences.
J Bone Joint Surg – Series A. 2006;88 (Suppl 2): 21–24.Ivanova JI, Birnbaum HG, Schiller M, Kantor E, Johnstone BM, Swindle RW.
Real-world practice patterns, health-care utilization, and costs in patients
with low back pain: the long road to guideline-concordant care.
Spine J. 2011;11(7): 622–632.Deyo RA, Mirza SK, Turner JA, Martin BI.
Overtreating Chronic Back Pain: Time to Back Off?
J Am Board Fam Med. 2009 (Jan); 22 (1): 62–68Bishop PB, Wing PC.
Compliance with Clinical Practice Guidelines in Family Physicians
Managing Worker's Compensation Board Patients with Acute Lower Back Pain
Spine J 2003 (Nov); 3 (6): 442–450Globe G, Farabaugh RJ, Hawk C, Morris CE, Baker G, Whalen WM, et al.
Clinical Practice Guideline:
Chiropractic Care for Low Back Pain
J Manipulative Physiol Ther 2016 (Jan); 39 (1): 1–22Wong JJ, Cote P, Sutton DA, et al.
Clinical Practice Guidelines for the Noninvasive Management of Low Back Pain:
A Systematic Review by the Ontario Protocol for Traffic Injury
Management (OPTIMa) Collaboration
European J Pain 2017 (Feb); 21 (2): 201–216Passmore SR, Toth A, Kanavosky J, Olin G.
Initial Integration of Chiropractic Services into a Provincially Funded
Inner City Community Health Centre: A Program Description
J Can Chiropr Assoc 2015 (Dec); 59 (4): 363–372Dagenais, S, Brady, O, Haldeman, S, and Manga, P.
A Systematic Review Comparing the Costs of Chiropractic Care to other
Interventions for Spine Pain in the United States
BMC Health Serv Res. 2015 (Oct 19); 15: 474Michaleff ZA, Lin CW, Maher CG, van Tulder MW.
Spinal Manipulation Epidemiology:
Systematic Review of Cost Effectiveness Studies
J Electromyogr Kinesiol. 2012 (Oct); 22 (5): 655–662Smith M, Stano M.
Costs and Recurrences of Chiropractic and Medical Episodes of Low-back Care
J Manipulative and Physiological Therapeutics 1997 (Jan); 20 (1): 5–12Goertz CM, Long CR, Vining RD, Pohlman KA, Walter J, Coulter I.
Effect of Usual Medical Care Plus Chiropractic Care vs Usual Medical Care
Alone on Pain and Disability Among US Service Members With
Low Back Pain. A Comparative Effectiveness Clinical Trial
JAMA Network Open. 2018 (May 18); 1 (1): e180105 NCT01692275Goertz CM, Long CR, Hondras MA, Petri R, Delgado R, Lawrence DJ, et al.
Adding Chiropractic Manipulative Therapy to Standard Medical Care
for Patients with Acute Low Back Pain: Results of a Pragmatic
Randomized Comparative Effectiveness Study
Spine (Phila Pa 1976). 2013 (Apr 15); 38 (8): 627–634Cherkin, D.C. and MacCornack, F.A.
Patient Evaluations of Low Back Pain Care From
Family Physicians and Chiropractors
Western Journal of Medicine 1989 (Mar); 150 (3): 351–355Kawai K, Kawai AT, Wollan P, Yawn BP.
Adverse Impacts of Chronic Pain on Health-related Quality of Life,
Work Productivity, Depression and Anxiety in a Community-based Study
Family Practice 2017 (Nov 16); 34 (6): 656–661Dagenais S, Haldeman S.
Chiropractic.
Prim Care. 2002;29: 419–437.Lisi AJ, Corcoran KL, Derycke EC, Bastian LA, Becker WC, Edmond SN, et al.
Opioid Use Among Veterans of Recent Wars
Receiving Veterans Affairs Chiropractic Care
Pain Medicine 2018 (Sep 1); 19 (suppl_1): S54–S60Corcoran KL, Bastian LA, Gunderson CG, Steffens C, Brackett A, Lisi AJ.
Association Between Chiropractic Use and Opioid Receipt Among
Patients with Spinal Pain: A Systematic Review and Meta-analysis
Pain Medicine 2020 (Feb 1); 21 (2): e139–e145Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA.
Studies with pain rating scales.
Ann Rheumat Dis. 1978;37(4): 378–381.Kamper SJ, Logan G, Copsey B, Thompson J, Machado GC, Abdel-Shaheed C, et al.
What is Usual Care for Low Back Pain? A Systematic Review
of Health Care Provided to Patients with Low Back Pain
in Family Practice and Emergency Departments
Pain. 2020 (Apr); 161 (4): 694–702Grigoras CA, Karanika S, Velmahos E, Alevizakos M, Flokas ME, Kaspiris-Rousellis C, et al.
Correlation of opioid mortality with prescriptions and social determinants:
a cross-sectional study of medicare enrollees.
Drugs. 2018;78(1): 111–121.Scherrer JF, Schneider FD, Lustman PJ.
Opioid analgesics and chronic non-cancer pain:
A prescription for research in primary care.
Fam Pract. 2016;33(6): 569–571.Kahan M, Mailis-Gagnon A, Wilson L, Srivastava A;
National Opioid Use Guideline Group. Canadian guideline for safe and effective
use of opioids for chronic noncancer pain: clinical summary for family physicians.
Part 1: general population.
Can Fam Physician. 2011;57(11): 1257-1266, e407-418.Busse JW, Craigie S, Juurlink DN, Buckley DN, Wang L, Couban RJ, Agoritsas T, et al.
Guideline for Opioid Therapy and Chronic Noncancer Pain
CMAJ. 2017 (May 8); 189 (18): E659–E666
Return to OPIOID EPIDEMIC
Return to INITIAL PROVIDER/FIRST CONTACT
Since 9-19-2021


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |
