

First-Contact Care With a Medical vs Chiropractic
Provider After Consultation With a Swiss Telemedicine
Provider: Comparison of Outcomes, Patient Satisfaction,
and Health Care Costs in Spinal, Hip,
and Shoulder Pain PatientsThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther. 2015 (Sep); 38 (7): 477–483 ~ FULL TEXT
OPEN ACCESS Taco A.W. Houweling, DC, MRes, PhD, Andrea V. Braga, MD, MBA, Thomas Hausheer, DC,
arco Vogelsang, DC, Cynthia Peterson, RN, DC, MMedEd, B. Kim Humphreys, DC, PhD
Postdoctoral Research Fellow,
Department of Chiropractic Medicine,
University Hospital Balgrist, Forchstrasse 340, 8008
Zürich, Switzerland.
taco.houweling@balgrist.ch

Houweling, JMPT 2015 Liliedahl, JMPT 2010
JMPT's Editor-in-Chief Claire Johnson, DC, MEd,
emphasized the importance of the latest findings:“Comparative studies – in other words, research that compares the outcomes between two different providers or modalities – are rare for chiropractic care,” she said.
“Thus, this study by Houweling, et al., is especially important if payers and policy-makers are to better understand the 'triple aim' as it relates to chiropractic. Specifically, this study helps us better understand what type of care provides better patient satisfaction, is more cost effective, and improves population health.”
“The findings of this study support first-contact care provided by DCs as an alternative to first-contact care provided by MDs for a select number of musculoskeletal conditions. Restrictive models of care in which patients are required to contact a medical provider before consulting a chiropractic provider may be counterproductive for patients experiencing the musculoskeletal conditions investigated and possibly others.”OBJECTIVE: The purpose of this study was to identify differences in outcomes, patient satisfaction, and related health care costs in spinal, hip, and shoulder pain patients who initiated care with medical doctors (MDs) vs those who initiated care with doctors of chiropractic (DCs) in Switzerland.
METHODS: A retrospective double cohort design was used. A self-administered questionnaire was completed by first-contact care spinal, hip, and shoulder pain patients who, 4 months previously, contacted a Swiss telemedicine provider regarding advice about their complaint. Related health care costs were determined in a subsample of patients by reviewing the claims database of a Swiss insurance provider.
RESULTS: The study sample included 403 patients who had seen MDs and 316 patients who had seen DCs as initial health care providers for their complaint. Differences in patient sociodemographic characteristics were found in terms of age, pain location, and mode of onset. Patients initially consulting MDs had significantly less reduction in their numerical pain rating score (difference of 0.32) and were significantly less likely to be satisfied with the care received (odds ratio = 1.79) and the outcome of care (odds ratio = 1.52). No significant differences were found for Patient's Global Impression of Change ratings. Mean costs per patient over 4 months were significantly lower in patients initially consulting DCs (difference of CHF 368; US $368).
CONCLUSION: Spinal, hip, and shoulder pain patients had clinically similar pain relief, greater satisfaction levels, and lower overall cost if they initiated care with DCs, when compared with those who initiated care with MDs.
From the FULL TEXT Article:
Introduction
Pain of musculoskeletal origin represents a major health problem worldwide. In a Swiss survey conducted in 2007, back pain was a commonly reported health problem, with 43% of the population experiencing this complaint over the course of a year. [1] Of these, 33% reported that their symptoms led to reduced productivity at work. The burden of musculoskeletal conditions on the Swiss health care system is equally staggering, with health care expenditure resulting from this condition being estimated at 14 billion Swiss Francs (CHF) per year (US $14 billion) or 3.2% of the gross domestic product. [2]
First-contact care (ie, care provided at the entry point into the health care system including assessing and making appropriate referrals) for musculoskeletal conditions as covered by the compulsory Swiss health insurance (obligatorische Krankenpflegeversicherung) is provided by 2 medical professionals, that is, medical doctors (MDs) and doctors of chiropractic (DCs). [3] Although patients may be co-managed with other medical colleagues or paramedical providers (eg, physiotherapists), treatment for the same complaint may vary according to the type of first-contact provider. For instance, MDs tend to use medication, including analgesics, muscle relaxants, and anti-inflammatory agents, for the treatment of acute nonspecific spinal pain, whereas DCs favor spinal manipulative therapy as the primary treatment for this condition. [4]
Despite the importance of the role of MDs and DCs as first-contact care providers in the Swiss health care system, comparative research on outcomes and health care costs in patients initiating care with either of these 2 medical providers for musculoskeletal and other conditions has yet to be undertaken. Therefore, the purpose of this study was to compare differences in outcomes, including pain levels and perceived change in overall health, and patient satisfaction as well as related health care costs in spinal, hip, and shoulder pain patients who initiated care with MDs vs those who initiated care with DCs in Switzerland.
Methods
Design
The study was designed as a retrospective double cohort study of first-contact care patients with spinal, hip, and shoulder pain who, 4 months previously, contacted the Swiss telemedicine provider Medi24 regarding treatment advice about their complaint. Medi24 provides telemedicine consultation services to a number or Swiss health insurers. Such services can be used by insured patients to assist with specific complaints or general health queries and may enable the caller to access the appropriate medical service.
Study Sample
Consecutive spinal, hip, and shoulder pain patients contacting Medi24 between February 2011 and February 2013 were included in the study if they were advised to see a medical or chiropractic provider for further management of their complaint. Although patients were recommended to consult these providers, they were not obliged to follow the advice given by the telemedicine provider. Patients were excluded if they had symptoms or conditions warranting immediate referral to the emergency department (eg, heart attack and cauda equina syndrome), or if their musculoskeletal problem was a secondary complaint (ie, not the main reason for contacting Medi24). Patients were also excluded if they were covered by an insurance product requiring them to contact their general practitioner before consulting any other health care provider (Hausartzmodell), and if they were not literate in French or German. The Ethics Committee of the Canton Zürich raised no objection to the study (KEK-StV-Nr. 42/13).
Data
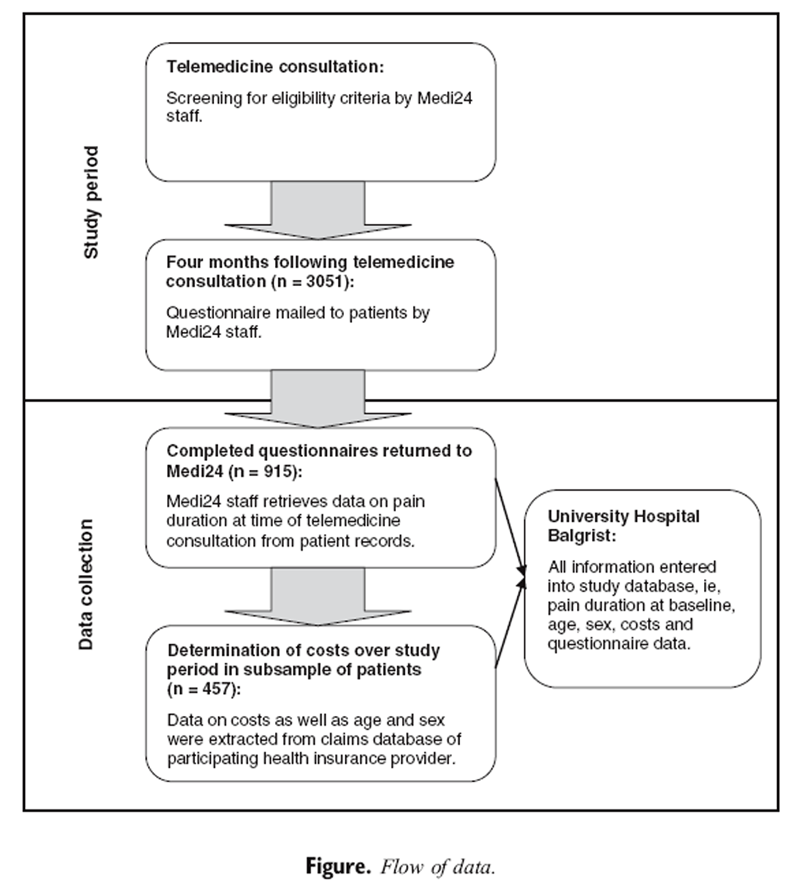
Figure A diagram of the flow of data throughout the study is shown in the Figure. Information on clinical characteristics, pain levels, Patient's Global Impression of Change (PGIC), patient satisfaction and use of health care services was collected using a self-administered questionnaire mailed to patients 4 months after the telemedicine consultation with Medi24. Patients were asked to report their pain levels at the time of completion of the questionnaire (today) and recall their pain 4 months previously (at the time of the telemedicine consultation), with these data being recorded on an 11–point numeric rating scale where 0, no pain and 10, the worst pain imaginable. The PGIC was assessed using a 7–point scale showing the categories “much better” and “much worse” at the extremes on which patients rated any change in their overall health that they had experienced since the beginning of the study. [5] Work loss (absenteeism) was determined by asking patients to report on the number of days off work over the study period due to their complaint. Satisfaction with the care received and the result of care were measured using a 5–point Likert scale ranging from “very satisfied” to “very unsatisfied.” [6] Variables referring to the use of health care services included providers consulted, treatments undergone, and diagnostic procedures received over the study period. A list of these variables is shown in Table 1.

Table 1 Information on related health care costs over the study period was available in a subsample of patients covered by an insurance product from a large Swiss insurance provider. Cost data were extracted from the health care claims database of this insurance provider, which is a record of all health care bills paid by the insurer including type and date of service. Data on the use of health care services as reported in questionnaires were linked up with the same data as seen in the claims database; hence, cost data could be attributed to each resource used by patients for the complaint investigated. Only claims made during the 4–month period starting from the time of the call to Medi24 were used for costs calculations. Providers were collapsed into 4 categories including MDs, DCs, physiotherapists, and complementary therapists, with emergency department visits being assigned to the MDs category.
Statistical Analysis
Descriptive results are given as means with SDs and as percentages. Baseline characteristics were compared using the χ2
Results

Table 2

Table 3

Table 4

Table 5

Table 6 Three thousand fifty-one patients were eligible to participate in the study, and of these, 915 (30%) responded to the questionnaire. Seven hundred nineteen patients met the inclusion criteria of the study, with the main reasons for excluding responders being
(i) seeing a provider other than MDs or DCs for first-contact care,
(ii) not consulting any health care professional, and
(iii) experiencing an unclear complaint.Four hundred fifty-seven patients were insured with the participating health insurance provider, and of these, a minority (131, 29%) did not claim for the costs of their care.
Baseline characteristics of patients who sought first-contact care with MDs and DCs can be seen in Table 2. Significant differences were found for age, pain location, and mode of onset. Patients who initially consulted MDs (mean, 45.7; SD, 13.87) were older than those who initially consulted DCs (mean, 41.3 years; SD, 12.93 years). Patients with neck pain were less likely to initiate care with MDs (68, 17%) compared with DCs (84, 27%), and patients with shoulder or hip pain were more likely to initiate care with MDs (126, 31%) compared with DCs (53, 17%). Patients with complaints of insidious onset were more likely to seek first-contact care with MDs (309, 77%) vs DCs (207, 66%).
Outcomes and satisfaction in patients seeking first-contact care with MDs and DCs are shown in Tables 3 and 4, respectively. Adjusted mean pain change scores were significantly lower (0.32) in patients who initially consulted MDs vs those who initially consulted DCs. No significant differences were found for PGIC ratings and the number of days off work due to the complaints investigated. Patients who initially consulted with MDs were significantly less likely to be satisfied with the care received and the results of care compared with those who initially consulted DCs (OR of 1.79 and 1.52, respectively).
Claims-based spinal, hip, and shoulder pain-related health care resource usage by patients seeking first-contact care with MDs and DCs is reported in Table 5, with total spinal, hip, and shoulder pain-related health care costs per patient shown in Table 6. Adjusted mean costs per patient were significantly lower in patients initiating care with DCs compared with those initiating care with MDs (CHF 368; US $368), with similar results observed for a complete-case analysis (CHF 415; US $415). The number of patients using health care resources other than visits to the first-contact care provider ranged from 7 to 115 (4%–61%) if MDs were initially consulted, compared with 1 to 18 (1%–13%) if MDs were initially consulted.
Discussion
The present study was the first at comparing data on health outcomes, patient satisfaction, and related health care costs in patients consulting differing first-contact care providers for musculoskeletal pain in Switzerland. This study showed that spinal, hip, and shoulder pain patients had modestly higher pain relief and satisfaction with care at lower overall cost if they initiated care with DCs, when compared with those who initiated care with MDs.
Although the differences in pain relief scores between groups were statistically significant, they were likely not of clinical significance. The minimal clinically important difference is a threshold beyond which the change in the score of an instrument used to measure a symptom is considered meaningful to the patient. Kovacs et al [7] suggested a minimal clinical important difference for the numerical pain rating scale of 1.5, which is 5 times higher than the differences observed in this study. Hence, the extent of the differences in pain relief observed might be too small for patients to notice a clinically meaningful difference. This assumption is supported in the present study, as it was found that the data on perceived change in overall health over the study period were similar in patients who initially consulted MDs compared with those who initially consulted DCs. The fact that nearly 3 quarters of patients in both groups had acute symptoms (no longer than 30 days) likely explains this lack of a difference. Indeed, a recent systematic review of spinal manipulative therapy for patients with acute low back found that the benefit of manipulation-based therapy compared with other available treatments is typically small and likely not clinically relevant. [8]
The findings of this study pertaining to patient satisfaction were in line with previous research comparing chiropractic care to medical care for back pain, which found that chiropractic patients are typically more satisfied with the services received than medical patients. [9–12] The reasons for the differences in satisfaction ratings observed in this study are unknown. One possible reason for these discrepancies may be the longer consultation time typically available for appointments with DCs compared with MDs. [13] A further explanation for these controversial findings is that patients consulting DCs might have appreciated not having to see multiple providers for treatment. In contrary, MDs commonly refer patients to a physiotherapist for further treatment of acute spinal pain. [14]
Mean total spinal, hip, and shoulder pain-related health care costs per patient during the 4–month study period were approximately 40% lower in patients initially consulting DCs compared with those initially consulting MDs. The reason for this difference was a lower use of health care services other than first-contact care in patients initially consulting DCs compared with those initially consulting MDs. Previous observational studies comparing medical and chiropractic care in terms of health care costs per patient have shown opposing results. Two studies conducted in the United States found that patients with low back pain treated in chiropractic clinics incurred higher costs than patients treated in medical clinics. [15, 16] One possible reason for these opposing findings is that differences were brought about by the methods of determining costs. In the studies conducted in the United States, costs were determined by chart audit, whereas in the present study, cost determinations were based on an insurance database review of all health care services used for the conditions investigated including the cost of visits to other health care providers. A further explanation for the discrepancy with previous research may be the different health care settings with different cost structures in which the studies were conducted.
The findings of this study support first-contact care provided by DCs as an alternative to first-contact care provided by MDs for a select number of musculoskeletal conditions. Restrictive models of care in which patients are required to contact a medical provider before consulting a chiropractic provider may be counterproductive for patients experiencing the musculoskeletal conditions investigated and possibly others. In addition to potentially reducing health care costs, direct access to chiropractic care may ease the workload on MDs, particularly in areas with poor medical coverage and hence enabling them to focus on complex cases. The minority of patients with complex health problems initially consulting a chiropractic provider would be referred to, or comanaged with, a medical provider to provide optimal care.
Limitations
This study had several limitations, with the principal limitations being the low response rate, the lack of standardized validated outcome measures, and the limited information on clinical characteristics. Although the use of reminders mailed to patients and additional questioning during the telemedicine consultation might have had a positive impact on these factors, the implementation of such procedures was not possible due to resource constraints. This might also have resulted in longer telephone consultation times, potentially adversely affecting the quality of services provided. Despite this, the response rate of this study was in line with that obtained in previously conducted retrospective research on primary care patients (ranging from 33% to 41%). [17]
Despite adjusting outcome, patient experience, and cost data for differences in patient characteristics, the impact of other unmeasured confounding factors on these data is unknown. Because of the large amount of missing data on age, sex, mode of onset, and working status, these data could not be taken into account in all regression models used. The limited data available showed that there were differences in these factors, supporting that the results of this study may have been subject to residual confounding. The fact that patients initiating care with MDs were more likely to be hospitalized than to those initiating care with DCs provides further evidence to support this hypothesis. Indeed, it is plausible that patients selecting a chiropractic provider for first-contact care are generally healthier than those choosing a medical provider for this purpose. This could have resulted in higher satisfaction ratings and lower costs for patients initially consulting DCs compared with MDs. Nevertheless, the use of an observational design with its potential limitations was best suited for this study, as real-life practice patterns were assessed.
Extracting cost information from an insurance database presents a number of challenges, which include absence of clinical information about patients, incorrect labeling of data, and incomplete claims information. Furthermore, over-the-counter medication cannot be determined from an insurance database review. Such factors may lead to overestimation or underestimation of data on costs. Despite these limitations, insurance databases are regarded as an objective and reliable source of data on health care costs.
Caution must be taken in generalizing study findings to national practice, as the findings of this study may only be applicable to a selected population. The present study was conducted on patients using telemedicine services, and costs were based on data from a single insurance provider. Moreover, the distribution of the type and number of health care providers in a geographic area can have an impact on the use of health care resources and treatment patterns. Future research may want to focus on specific treatment settings (eg, chiropractic and general practitioner clinics) to reduce the possibility of such bias.
Conclusion
Although spinal, hip, and shoulder pain patients had clinically comparable pain relief irrespective of the initial provider seen, overall health care costs were considerably lower if patients initiated care with DCs compared with those who initiated care with MDs. Moreover, patients initially consulting DCs had greater satisfaction levels with care compared with those initially consulting MDs. These findings should be confirmed in prospective studies because they may have important implications for patients, clinicians, and third-party payers.
References:
Altwegg, David, Andreani, Tania, Berrut, Sylvie et al.
Gesundheitsstatistik 2007.
Bundesamt für Statistik, ; 2012Muskuloskelettale Gesundheit—
Chronische Schmerzen: Synthesebericht der Leitungsgruppe.
Nationales Forschungsprogramm NFP 53, ; 2009Bundesgesetz über die Krankenversicherung:
Die Bundesversammlung der Schweizerischen Eidgenossenschaft. ;
2014Gilkey, D, Caddy, L, Keefe, T et al.
Colorado Workers' Compensation: Medical vs Chiropractic Costs for the Treatment of Lowback Pain
Journal of Chiropractic Medicine 2008 (Dec); 7 (4): 127–133Lauridsen, HH, Hartvigsen, J, Korsholm, L, Grunnet-Nilsson, N.
Choice of external criteria in back pain research: does it matter? Recommendations based on analysis of responsiveness.
Pain. 2007; 131: 112–120Garratt, AM, Helgeland, J, and Gulbrandsen, P.
Five-point scales outperform 10-point scales in a randomized comparison of item scaling for the patient experiences questionnaire.
J Clin Epidemiol. 2011; 64: 200–207Kovacs, FM, Abraira, V, Royuela, A et al.
Minimum detectable and minimal clinically important changes for pain in patients with nonspecific neck pain.
BMC Musculoskelet Disord. 2008; 9: 43Rubinstein, SM, Terwee, CB, Assendelft, WJ, de Boer, MR, and van Tulder, MW.
Spinal manipulative therapy for acute low back pain: an update of the Cochrane review.
Spine (Phila Pa 1976). 2013; 38: E158–E177Kanodia, AK, Legedza, AT, Davis, RB, Eisenberg, DM, and Phillips, RS.
Perceived benefit of complementary and alternative medicine (CAM) for back pain: a national survey.
J Am Board Fam Med. 2010; 23: 354–362Wolsko PM, Eisenberg DM, Davis RB, Kessler R, Phillips RS:
Patterns and Perceptions of Care for Treatment of Back
and Neck Pain: Results of a National Survey
Spine (Phila Pa 1976) 2003 (Feb 1); 28 (3): 292–297Adams, J, Sibbritt, D, Broom, A et al.
Complementary and alternative medicine consultations in urban and nonurban areas: a national survey of 1427 Australian women.
J Manipulative Physiol Ther. 2013; 36: 12–19Weigel PA, Hockenberry JM, Wolinsky FD.
Chiropractic Use in the Medicare Population: Prevalence, Patterns, and Associations
With 1-year Changes in Health and Satisfaction With Care
J Manipulative Physiol Ther 2014 (Mar); 37 (8): 542-551Hush, JM, Cameron, K, and Mackey, M.
Patient satisfaction with musculoskeletal physical therapy care: a systematic review.
Phys Ther. 2011; 91: 25–36Scott, NA, Moga, C, and Harstall, C.
Managing low back pain in the primary care setting: the know-do gap.
Pain Res Manag. 2010; 15: 392–400Haas M, Sharma R, Stano M.
Cost-effectiveness of Medical and Chiropractic Care for Acute and Chronic Low Back Pain
J Manipulative Physiol Ther 2005 (Oct); 28 (8): 555–563Stano, M, Haas, M, Goldberg, B, Traub, PM, and Nyiendo, J.
Chiropractic and medical care costs of low back care: results from a practice-based observational study.
Am J Manag Care. 2002; 8: 802–809The GP patient survey.
([Internet]) ([updated 2009 2011; cited 2012 Feb;
http://www.gp-patient.co.uk/
Department of Health, London; 2009
Return PEDIATRICS
Return to MEDICARE
Return to SHOULDER
Return to LOW BACK PAIN
Return to COST-EFFECTIVENESS
Return to PATIENT SATISFACTION
Return to INITIAL PROVIDER/FIRST CONTACT
Since 8-23-2015


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |