Radiculopathy and Chiropractic This section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org
| Jump to: | What is Radiculopathy | The Diagnosis of Radicular Pain | |
|
|
The Medical Approach | The Chiropractic Approach |




|
|
Conditions That Respond | Alternative Medicine Approaches to Disease |




What is Radicular Pain? (Radiculopathy)




The difference between the chiropractic and the medical approaches to health care
is never more apparent than with their treatment of radiculopathy.
The medical approach entails their version of “conservative” treatment, including pain medications, prolonged spinal injections, or perhaps a prescription for physical therapy. Then, if their “conservative” treatment does not alleviate the pain, decompressive surgery, such as laminectomy and/or discectomy/microdiscectomy, may be recommended.
Chiropractors aptly describe radiculopathy as “nerve root irritation”, and the chiropractic approach for resolution is quite straightforward.
Answer me this: If you have a rock in your shoe, and your foot hurts... do you need physical therapy, medications, or spinal injections? NO!!! You want your doctor (who is supposed to be the Sherlock Holmes of spinal diagnosis) to determine the CAUSE of the nerve root irritation (the rock), and to remove that obstacle from your path, so you may return to health.
Review the rest of this page to explore the real differences between these 2 approaches
to health care, and the difference in their success rates. The conclusions will surprise you!
Radiculopathy is characterized by motor and/or sensory changes in the neck and arms or the legs and feet, which results from extrinsic pressure on the nerve root. This pressure is typically caused by disc material, swelling, or osteophytes. A large study in Rochester, Minnesota, has reported the annual incidence of cervical radicular symptoms to be 83.2 per 100,000 population, and its prevalence most significant within a 50- to 54-year age group. In the study, 90 percent of patients were asymptomatic or only mildly incapacitated. Surgery is not often required for resolution of cervical radiculopathy symptoms.
Symptoms
Radicular pain, the characteristic symptom of cervical radiculopathy, is often confused with radiating pain in clinical practice. Because specific treatments are exclusively indicated for radicular pain, an accurate distinction is important. True radicular pain follows dermatomal patterns and is usually — though not always — unilateral. Onset is often insidious but may also be abrupt, and the pain is frequently aggravated by arm position and extension or lateral rotation of the head. [4]
There are three primary types of pain:
Local Pain is caused by irritation to the structures in the back including bone, muscles, ligaments and joints. The pain is usually steady, sharp or dull, felt in the effected area of the spine and may change with changes in position or activity.
Referred Pain can be pain caused by non-spinal pathology that is referred to the back, such as an abdominal aortic aneurysm. Referred pain can also be pain originating in the spine that is felt in distant structures. For instance upper lumbar pain is frequently felt in the upper thighs, and lower lumbar pain is felt in the lower buttocks. Sacroiliac joint pain is often referred to the inguinal and antero-lateral thigh area. Referred pain rarely extends below the knees, where as nerve root pain can be felt in the calf or foot.
Radicular Pain is caused by irritation of the nerve roots (radix) and is usually more severe than referred pain, and may have a more distal radiation. Radicular pain usually circumscribes the territory of innervation of the given nerve root (in a dermatomal distribution). This type of pain is often deep and steady, and can usually be reproduced with certain activities and positions, such as sitting or walking. [1] In addition, radicular pain is frequently exacerbated by any maneuver that raises the pressure of cerebrospinal fluid (or the interabdominal pressure), such as valsalva, sneezing, or cough. [2]
Radicular Pain Distribution
Radicular pain radiates into the extremity (thigh, calf, and occasionally the foot or to the arm, forearm or hand) directly along the course of a specific spinal nerve root. The most common symptom of radicular pain is sciatica (pain that radiates along the sciatic nerve – down the back of the thigh and calf into the foot) and arm pain and paresthesia of the hand. Sciatica is one of the most common forms of pain caused by compression of a spinal nerve in the low back. It may result from compression of the lower spinal nerve roots (L5 and S1). With this condition, the leg pain is typically much worse than the low back pain, and the specific areas of the leg and/or foot that are affected depends on which nerve in the low back is affected. Compression of higher lumbar nerve roots such as L2, L3 and L4 can cause radicular pain into the front of the thigh and the shin.




The Diagnosis of Radicular Pain




Radiculopathy is caused by compression, inflammation and/or injury to a spinal nerve root,
typically within the vertebral foramina.
Causes of Radicular Pain, in their order of prevalence, include:[2]
Herniated disc with nerve compression – by far the most common cause of radiculopathy
Foraminal stenosis (narrowing of the hole through which the spinal nerve exits due
to bone spurs or arthritis) – more common in elderly adults
Diabetes
Nerve root injuries (Traction injuries and Whiplash injuries)
Scar tissue from previous spinal surgery that is affecting the nerve root
Herpes Simplex Virus Type I Infection [3]
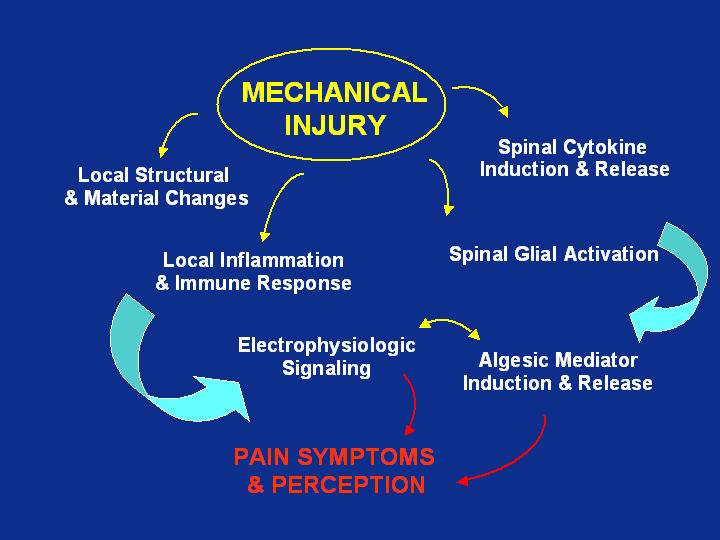
The cascade of events leading to radicular pain:
Thanks to the University of Pennsylvania for access to this slide!




The Treatment of Radicular Pain: The Medical Approach




It is usually recommended that a course of conservative treatment (such as physical therapy, medications, and selective spinal injections, among others) should be conducted for six to eight weeks. If conservative treatment does not alleviate the pain, decompressive surgery, such as laminectomy and/or discectomy/microdiscectomy, may be recommended. For patients with severe leg pain or other serious symptoms such as progressive muscle weakness, this type of surgery may be recommended prior to six weeks of non-surgical treatment. Back surgery for relief of radicular pain (leg pain) is much more reliable than for relief of low back pain.
Recent testing has demonstrated that treatment with Steroids offer no benefit compared with bupivacaine alone in chronic radicular pain. [5] Multiple adverse effects have been associated with prolonged steroid use, including suppression of the hypothalamic-pituitary-adrenal axis, immunosuppression, psuedotumor cerebri and psychoses, cataracts and increased intraocular pressure, osteoporosis, aseptic necrosis, gastric ulcers, fluid and electrolyte disturbances and hypertension, and impaired wound healing. [6]
Several surgical websites claim that surgery provides relief of radicular pain/leg pain for 83% to 90% of patients.
However, review of numerous peer-reviewed studies reveals that this is NOT the case.




The Treatment of Radicular Pain: The Chiropractic Approach





The McKenzie Method Page
A Chiro.Org article collection
The McKenzie Method is grounded in finding a cause and effect relationship between the positions the patient usually assumes while sitting, standing, or moving, and the generation of pain as a result of those positions or activities. The therapeutic approach requires a patient to move through a series of activities and test movements to gauge the patient's pain response. The approach then uses that information to develop an exercise protocol designed to centralize or alleviate the pain.

Patient Expectations and Levels of Satisfaction in
Chiropractic Treatment for Lumbar Radiculopathy.
A Mixed Methods Study
Chiropractic & Manual Therapies 2023 (May 19); 31: 13 ~ FULL TEXT
Overall, patients were satisfied with the standardised chiropractic care package for lumbar radiculopathy. From a patient’s perspective, satisfaction was linked to the chiropractor spending time on the consultation and offering a thorough examination, allowing the patient to feel in safe hands. Referral for MRI provided certainty and confidence by confirming the diagnosis. Information and guidance for patients related to variations in symptoms and expected prognosis were reassuring, and the interdisciplinary collaboration coordinated by the chiropractor (with GP, physiotherapist, and hospital referral) was highly valued.

Association Between Chiropractic Spinal Manipulation
~ FULL TEXT
and Lumbar Discectomy in Adults with Lumbar Disc
Herniation and Radiculopathy: Retrospective
Cohort Study Using United States' Data
BMJ Open 2022 (Dec 16); 12 (12): e068262
These findings suggest that patients receiving CSMT for newly diagnosed LDH and/or LSR without serious pathology, spinal deformity or absolute indications for surgery have significantly reduced odds of discectomy through 2-year follow-up after index diagnosis compared with those receiving other care. While socioeconomic variables were unavailable in the dataset, current data suggests these unmeasured variables would not completely explain our findings. However, given the possibility of residual confounding, the efficacy of CSMT for LDH/LSR should be explored further using a randomised controlled trial.

Reducing Cervical Retrolisthesis With Long-Term Monthly
~ FULL TEXT
Chiropractic Maintenance Care: A Case Report
J Med Cases 2022 (Jul); 13 (7): 359–364
The patient was diagnosed with right C5 radiculopathy associated with vertebral retrolisthesis. She was conservatively treated with multimodal chiropractic care comprising cervical manipulation applied to the affected segments, axial distraction, and isometric stretching. After 20 sessions over 3 months of therapy, the patient experienced complete relief of neck pain and radicular symptoms, and full cervical mobility. Because her complaints were characterized by relapsing episodes, she was enrolled in a monthly MC program to monitor and ensure the spine was functioning at its highest capacity. The MC program included disease monitoring, manipulation of dysfunctional segments, cervical strengthening exercises, and ergonomics coaching. Monthly care was shown to be successful in maintaining an asymptomatic status. Moreover, a gradual reduction in cervical retrolisthesis was observed during the 13–year MC period, and the ongoing MC ensured optimal spine functioning.

Observed Patterns of Cervical Radiculopathy: How Often Do They Differ From
a Standard, "Netter Diagram" Distribution?
Spine J. 2019 (Jul); 19 (7): 1137–1142 ~ FULL TEXT
In conclusion, standard patterns of cervical radiculopathy were found in only 54% of patients undergoing single level ACDF. This divergence from the accepted standard highlights the need for careful assessment of associated neurological, physical, radiological, and other findings, as a non-standard clinical pattern is frequently encountered. It is not only possible, but actually relatively common, for patients with C3–4 or C4–5 radiculopathy to complain of distal symptoms that seemingly do not make “sense.” Similarly, we found that it is also relatively common for patients with C5–6 or C6–7 radiculopathy to complain only of proximal symptoms. In order to appropriately treat patients presenting with cervical radiculopathy, practitioners must think broadly when identifying causative levels because they frequently do not adhere to the accepted standard in actual clinical practice.

Symptomatic, Magnetic Resonance Imaging-Confirmed Cervical Disk Herniation Patients:
~ FULL TEXT
A Comparative-Effectiveness Prospective Observational Study of 2 Age- and Sex-Matched
Cohorts Treated With Either Imaging-Guided Indirect Cervical Nerve Root Injections
or Spinal Manipulative Therapy
J Manipulative Physiol Ther. 2016 (Mar); 39 (3): 210–217
"Improvement" was reported in 86.5% of SMT patients and 49.0% of CNRI patients (P = .0001). Significantly more CNRI patients were in the subacute/chronic category (77%) compared with SMT patients (46%). A significant difference between the proportion of subacute/chronic CNRI patients (37.5%) and SMT patients (78.3%) reporting "improvement" was noted (P = .002).

Symptomatic, MRI Confirmed, Lumbar Disc Herniations:
A Comparison of Outcomes Depending on the Type and
Anatomical Axial Location of the Hernia in Patients
Treated With High-Velocity, Low-Amplitude
Spinal Manipulation
J Manipulative Physiol Ther. 2016 (Mar); 39 (3): 192–199 ~ FULL TEXT
The majority of patients in this study had either extruded or sequestered disc herniations. Patients with sequestered herniations treated with SMT to the level of herniation reported significantly higher levels of leg pain reduction at 1 month and a higher proportion reported improvement at all data collection time points compared to patients with extruded disc herniations but this did not reach statistical significance. Further investigation is needed to determine mechanisms for this finding. This also calls into question the seriousness of disc sequestration in determining appropriate treatment.

Does Cervical Spine Manipulation Reduce Pain in People
~ FULL TEXT
with Degenerative Cervical Radiculopathy? A Systematic
Review of the Evidence, and a Meta-analysis
Clinical Rehabilitation 2016 (Feb); 30 (2): 145-155
Three trials with 502 participants were included. Meta-analysis suggested that cervical spine manipulation (mean difference 1.28, 95% confidence interval 0.80 to 1.75; P < 0.00001; heterogeneity: Chi2 = 8.57, P = 0.01, I2 = 77%) improving visual analogue scale for pain showed superior immediate effects compared with cervical computer traction. The overall strength of evidence was judged to be moderate quality.

Pain Location Matters: The Impact of Leg Pain on
~ FULL TEXT
Health Care Use, Work Disability and Quality
of Life in Patients with Low Back Pain
European Spine Journal 2015 (Mar); 24 (3): 44–451
Patients with self-reported leg pain below the knee utilise more health care are more likely to be unemployed and have poorer quality of life than those with LBP only 12 months following primary care consultation. The presence of leg pain warrants early identification in primary care to explore if targeted interventions can reduce the impact and consequences of leg pain.

Function in Patients With Cervical Radiculopathy or Chronic
~ FULL TEXT
Whiplash-Associated Disorders Compared
With Healthy Volunteers
J Manipulative Physiol Ther 2014 (May); 37 (4): 211–218
Patient groups exhibited significantly lower performance than the healthy group in all physical measures (P < .0005) except for neck muscle endurance in flexion for women (P > .09). There was a general trend toward worse results in the CR group than the WAD group, with significant differences in neck active range of motion, left hand strength for women, pain intensity, Neck Disability Index, EuroQol 5-dimensional self-classifier, and Self-Efficacy Scale (P < .0001). Patients had worse values than healthy individuals in almost all physical measures. There was a trend toward worse results for CR than WAD patients.

Outcomes of Acute and Chronic Patients With Magnetic Resonance
~ FULL TEXT
Imaging–Confirmed Symptomatic Lumbar Disc Herniations
Receiving High-Velocity, Low-Amplitude, Spinal
Manipulative Therapy: A Prospective Observational
Cohort Study With One-Year Follow-Up
J Manipulative Physiol Ther 2014 (Mar); 37 (3): 155–163
Significant improvement for all outcomes at all time points was reported (P < .0001). At 3 months, 90.5% of patients were “improved” with 88.0% “improved” at 1 year. Although acute patients improved faster by 3 months, 81.8% of chronic patients reported “improvement” with 89.2% “improved” at 1 year. There were no adverse events reported.

Vertebral Artery Dissection as a Cause of Cervical Radiculopathy
~ FULL TEXT
Asian Spine J. 2013 (Dec); 7 (4): 335–338
We describe a case of vertebral artery dissection presenting as cervical radiculopathy in a previously healthy 43–year-old woman who presented with proximal left arm weakness and neck pain aggravated by movement. Cervical magnetic resonance imaging (MRI) and angiography revealed dissection of the left vertebral artery with an intramural hematoma compressing the left C5 and C6 nerve roots.

Outcomes From Magnetic Resonance Imaging–Confirmed Symptomatic
~ FULL TEXT
Cervical Disk Herniation Patients Treated With High-Velocity,
Low-Amplitude Spinal Manipulative Therapy: A Prospective
Cohort Study With 3-Month Follow-Up
J Manipulative Physiol Ther 2013 (Oct); 36 (8): 461–467
50 adult Swiss patients with neck pain and dermatomal arm pain; sensory, motor, or reflex changes corresponding to the involved nerve root; and at least 1 positive orthopaedic test for cervical radiculopathy were included. Magnetic resonance imaging-confirmed CDH linked with symptoms was required. At 2 weeks, 55.3% were "improved," 68.9% at 1 month and 85.7% at 3 months. Statistically significant decreases in neck pain, arm pain, and NDI scores were noted at 1 and 3 months compared with baseline scores (P < .0001). Of the subacute/chronic patients, 76.2% were improved at 3 months.

Predictors of Improvement in Patients With Acute and Chronic
~ FULL TEXT
Low Back Pain Undergoing Chiropractic Treatment
J Manipulative Physiol Ther. 2012 (Sep); 35 (7): 525–533
An important and unique finding in this current study is that although 123 (23%) of the patients with acute LBP and 71 (24%) of the patients with chronic LBP were diagnosed by their chiropractors as having radiculopathy, this finding was not a negative predictor of improvement. Radiculopathy was not simply defined as leg pain but required clinical signs of nerve root compression as determined by the examining chiropractor. Previous studies investigating outcomes from patients with LBP undergoing spinal manipulation have purposely excluded patients with radiculopathy, [2, 10, 29] and others have found that the presence of leg pain is a negative predictor of improvement. [12, 24, 30] This study purposely included these patients to evaluate this subgroup. It is quite common for patients with LBP experiencing radiculopathy to seek chiropractic care in Switzerland and to receive spinal manipulative therapy as one of the treatment options.

The Efficacy of Forward Head Correction on Nerve Root Function
and Pain in Cervical Spondylotic Radiculopathy: A Randomized Trial
Clin Rehabil. 2012 (Apr); 26 (4): 351–361 ~ FULL TEXT
Forward head posture correction using a posture corrective exercise programme in addition to ultrasound and infrared radiation decreased pain and craniovertebral angle and increased the peak-to-peak amplitude of dermatomal somatosensory evoked potentials for C6 and C7 in cases of lower cervical spondylotic radiculopathy.

Use of Post-isometric Relaxation in the Chiropractic Management
of a 55–year-old Man with Cervical Radiculopathy
Journal of the Canadian Chiropractic Association 2012 (Mar); 56 (1): 9–17 ~ FULL TEXT
Presented here was a patient with acute C7 radiculopathy that, despite MRI findings of a C6–7 disc protrusion with right-sided lateral canal stenosis, resolved following a course of chiropractic treatment that included SMT and cervical paraspinal PIR. The patient’s radiculopathy symptoms did not return in 3 years of follow-up.

Cervical Radiculopathy: A Systematic Review on Treatment by
Spinal Manipulation and Measurement with the Neck Disability Index
Journal of the Canadian Chiropractic Association 2012 (Mar); 56 (1): 18–28 ~ FULL TEXT
Cervical radiculopathy (CR), while less common than conditions with neck pain alone, can be a significant cause of neck pain and disability; thus the determination of adequate treatment options for patients is essential. Currently, inadequate scientific literature restricts specific conservative management recommendations for CR. Despite a paucity of evidence for high-velocity low-amplitude (HVLA) spinal manipulation in the treatment for CR, this strategy has been frequently labeled as contraindicated. Scientific support for appropriate outcome measures for CR is equally deficient. While more scientific data is needed to draw firm conclusions, the present review suggests that spinal manipulation may be cautiously considered as a therapeutic option for patients suffering from CR. With respect to outcome measures, the Neck Disability Index appears well-suited for spinal manipulative treatment of CR.

Manipulation or Microdiskectomy for Sciatica?
~ FULL TEXT
A Prospective Randomized Clinical Study
J Manipulative Physiol Ther. 2010 (Oct); 33 (8): 576–584
One hundred twenty patients presenting through elective referral by primary care physicians to neurosurgical spine surgeons were consecutively screened for symptoms of unilateral lumbar radiculopathy secondary to LDH at L3–4, L4–5, or L5–S1. Forty consecutive consenting patients who met inclusion criteria (patients must have failed at least 3 months of nonoperative management including treatment with analgesics, lifestyle modification, physiotherapy, massage therapy, and/or acupuncture) were randomized to either surgical microdiskectomy or standardized chiropractic spinal manipulation. Crossover to the alternate treatment was allowed after 3 months. Sixty percent of patients with sciatica who had failed other medical management benefited from spinal manipulation to the same degree as if they underwent surgical intervention. Of 40% left unsatisfied, subsequent surgical intervention confers excellent outcome. Patients with symptomatic LDH failing medical management should consider spinal manipulation followed by surgery if warranted.

Resolution of Low Back and Radicular Pain in a 40-year-old Male
~ FULL TEXT
United States Navy Petty Officer After Collaborative Medical
nd Chiropractic Care
J Chiropractic Medicine 2010 (Mar); 9 (1): 17–21
This article has described the case management of an active duty United States Navy Petty Officer who presented to his PCM with LBP and right leg pain. Radiologic studies confirmed posterior disk extrusion at L4/L5, abutting the right L5 nerve root, and posterior bulging of the L5/S1 disk. The primary purpose of this case report was to describe the interdisciplinary collaboration of chiropractic and medical services in a military setting. This article does not go into detail of the chiropractic treatments rendered, as several studies and trials on the use of manipulation and other forms of conservative care to treat patients with acute lumbar radiculopathy may be found in a systematic review by Lawrence et al. [21] Rather, it hoped to depict the unique inclusion of chiropractic management as part of available treatments within a military treatment facility.

A Nonsurgical Approach to the Management of Patients With
~ FULL TEXT
Lumbar Radiculopathy Secondary to Herniated Disk:
Prospective Observational Cohort
Study With Follow-Up
J Manipulative Physiol Ther 2009 (Nov); 32 (9): 723–733
A randomized trial by researchers at an outpatient rehabilitation department in Italy involving 210 patients with chronic, nonspecific low back pain compared the effects of spinal manipulation, physiotherapy and back school. The participants were 210 patients (140 women and 70 men) with chronic, non-specific low back pain, average age 59. Back school and individual physiotherapy were scheduled as 15 1-hour-sessions for 3 weeks. Back school included group exercise and education/ergonomics. Individual physiotherapy included exercise, passive mobilization and soft-tissue treatment. Spinal manipulation included 4–6 20-minute sessions once-a-week. Spinal manipulation provided better short and long-term functional improvement, and more pain relief in the follow-up than either back school or individual physiotherapy.

Pain Patterns and Descriptions in Patients with Radicular Pain:
Does the Pain Necessarily Follow a Specific Dermatome?
Chiropractic & Osteopathy 2009 (Sep 21); 17 (1): 9 ~ FULL TEXT
Two hundred twenty-six nerve roots in 169 patients were assessed. Overall, pain related to cervical nerve roots was non-dermatomal in over two-thirds (69.7%) of cases. In the lumbar spine, the pain was non-dermatomal in just under two-thirds (64.1%) of cases. The majority of nerve root levels involved non-dermatomal pain patterns except C4 (60.0% dermatomal) and S1 (64.9% dermatomal). The sensitivity (SE) and specificity (SP) for dermatomal pattern of pain are low for all nerve root levels with the exception of the C4 level (Se 0.60, Sp 0.72) and S1 level (Se 0.65, Sp 0.80), although in the case of the C4 level, the number of subjects was small (n=5). In most cases nerve root pain should not be expected to follow along a specific dermatome, and a dermatomal distribution of pain is not a useful historical factor in the diagnosis of radicular pain. The possible exception to this is the S1 nerve root, in which the pain does commonly follow the S1 dermatome.

Chiropractic Outcomes Managing Radiculopathy in a Hospital
~ FULL TEXT
Setting: A Retrospective Review of 162 Patients
J Chiropractic Medicine 2008 (Sep); 7 (3): 115—125
This is a retrospective review of 162 patients with a working diagnosis of radiculopathy who met the inclusion criteria (312 consecutive patients were screened to obtain the 162 cases). Data reviewed were collected initially, during, and at the end of active treatment. The treatment protocol included chiropractic manipulation, neuromobilization, and exercise stabilization. Of the 162 cases reviewed, 85.5% had resolution of their primary subjective radicular complaints. The treatment trial was 9 (mean) treatment sessions.

Cervical Myelopathy:
~ FULL TEXT
A Case Report of a “Near-Miss” Complication
to Cervical Manipulation
J Manipulative Physiol Ther 2008 (Sep); 31 (7): 553—557
Cases have been reported in which radiculopathy or myelopathy secondary to herniated disk has occurred after cervical manipulation. In each case, it is not possible to determine whether the neurologic symptoms and signs were directly caused by the manipulation or whether they developed as part of the natural history of the disorder. The purpose of this article is to report a case in which a patient with radiculopathy secondary to herniated disk was scheduled to receive manipulation but just before receiving this treatment developed acute myelopathy.

Physical Assessment of Lower Extremity Radiculopathy and Sciatica
~ FULL TEXT
J Chiropractic Medicine 2007 (Jun); 6 (2): 75–82
Several physical maneuvers are provocative to lumbosacral nerve roots or the sciatic nerve. Provocative maneuvers are intended to reproduce signs and symptoms of lower extremity radiculopathy/sciatica. Other maneuvers counter to the provocative maneuvers (palliative maneuvers) decrease nerve root and sciatic irritation and the related signs and symptoms (Figure 1).

Does Facet Joint Inflammation Induce Radiculopathy?
An Investigation Using a Rat Model of
Lumbar Facet Joint Inflammation
Spine (Phila Pa 1976) 2007 (Feb 15); 32 (4): 406–412
The association between lumbar facet joint inflammation and radiculopathy was investigated using behavioral, histologic, and immunohistochemical testing in rats. Both mechanical and chemical factors have been identified as important for inducing radiculopathy. In lumbar spondylosis, facet joint osteophytes may contribute to nerve root compression, which may induce radiculopathy. Furthermore, inflammation may occur in the facet joint, as in other synovial joints. Inflamed synovium may thus release inflammatory cytokines and induce nerve root injury with subsequent radiculopathy. (In this study) when inflammation was induced in a facet joint, inflammatory reactions spread to nerve roots, and leg symptoms were induced by chemical factors. These results support the possibility that facet joint inflammation induces radiculopathy.

Differentiating Radicular and Referred Pain
Chiropractic & Osteopathy 2007; 15: 1746—1340 ~ FULL TEXT
Similar upper extremity symptoms can present with varied physiologic etiologies. However, due to the multifaceted nature of musculoskeletal conditions, a definitive diagnosis using physical examination and advanced testing is not always possible. This report discusses the diagnosis and case management of a patient with two episodes of similar upper extremity symptoms of different etiologies.

Herniated Disc with Radiculopathy Following Cervical Manipulation:
Nonsurgical Management
Spine J 2006 (Jul); 6 (4): 459–463
This paper reports a case of a patient with radiculopathy secondary to multilevel disc herniations that appeared to be precipitated by cervical manipulation and who was treated nonsurgically with resolution of the problem. It is doubtful that the manipulation actually caused the disc herniations, but it is possible that it caused preexisting asymptomatic disc herniations to become symptomatic. Consideration should be given to nonsurgical referral of patients who have postmanipulative complications but do not need immediate surgery.

A Nonsurgical Approach to the Management of Patients With Cervical
~ FULL TEXT
Radiculopathy: A Prospective Observational Cohort Study
J Manipulative Physiol Ther. 2006 (May); 29 (4): 279–287
A prospective observational cohort study on consecutive patients with CR was performed. Data on 35 consecutive patients were collected at baseline, at the end of the active treatment, and at a minimum of 3 months after cessation of treatment. Disability was measured using the Bournemouth Disability Questionnaire. Pain intensity was measured using the Numerical Pain Rating Scale. Patients were also asked to self-rate their improvement. Complete outcome data were available for 31 of the 35 patients. Twenty-seven patients were reached for long-term follow-up. The mean number of months from last treatment to follow-up was 8.2 months. Seventeen patients (49%) reported their improvement as "excellent" and another 14 (40%) did so as "good." The mean patient-rated improvement was 88.2%.

Biomechanical and Neurophysiological Responses to
~ FULL TEXT
Spinal Manipulation in Patients With
Lumbar Radiculopathy
J Manipulative Physiol Ther. 2004 (Jan); 27 (1): 1–15
Because spinal manipulation (SM) is a mechanical intervention, it is inherently logical to assume that its mechanisms of therapeutic benefit may lie in the mechanical properties of the applied force (mechanical mechanisms), the body's response to such force (mechanical or physiologic mechanisms), or a combination of these and other factors. Basic science research, including biomechanical and neurophysiological investigations of the body's response to SM, therefore, should assist researchers, educators, and clinicians to understand the mechanisms of SM, to more fully develop SM techniques, to better train clinicians, and ultimately attempt to minimize risks while achieving better results with patients.

Cervical Radiculopathy Treated With Chiropractic Flexion Distraction
~ FULL TEXT
Manipulation: A Retrospective Study in a Private Practice Setting
J Manipulative Physiol Ther 2003 (Nov); 26 (9): E19
This study revealed a statistically significant reduction in pain as quantified by visual analogue scores. The mean number of treatments required was 13.2 +/- 8.2, with a range of 6 to 37. Only 3 persons required more treatments than the mean plus 1 standard deviation. The results of this study show promise for chiropractic and manual therapy techniques such as flexion distraction, as well as demonstrating that other, larger research studies must be performed for cervical radiculopathy.

Pain, Dizziness, and Central Nervous System Blood Flow
in Cervical Extension: Vascular Correlations to
Beauty Parlor Stroke Syndrome and
Salon Sink Radiculopathy
Am J Phys Med Rehabil 2002 (Jun); 81 (6): 395–399
Professional shampoos have previously been implicated in beauty parlor stroke syndrome and salon sink radiculopathy. The purpose of this study was to record pain, dizziness, and cervical blood flow while subjects were specifically placed into the salon sink position and to determine whether an additional cervical support would alter these symptoms and measurements.

Intermittent Cervical Traction for Cervical Radiculopathy
~ FULL TEXT
Caused by Large-volume Herniated Disks
J Manipulative Physiol Ther 2002 (Mar); 25 (3): 188–192
The treatment consisted of intermittent on-the-door cervical traction under the supervision of our physiotherapists. Complete symptom resolution for each patient occurred within 3 weeks. One patient who had an episode of recurrence 16 months after the first treatment was successfully managed again with cervical traction and physiotherapy. Cervical spine traction could be considered as a therapy of choice for radiculopathy caused by herniated disks, even in cases of large-volume herniated disks or recurrent episodes.

Rotary Manipulation for Cervical Radiculopathy:
Observations on the Importance of the
Direction of the Thrust
J Manipulative Physiol Ther 1997 (Nov); 20 (9): 622–627
Six of eight patients had a good outcome associated with receiving manipulation performed by contacting the cervical spine at the level of the radiculopathy, laterally flexing toward the side of radiculopathy, rotating the neck away from the side of the radiculopathy and applying a gentle high-velocity, low-amplitude thrust. Two patients had an exacerbation of arm pain and increased neurological deficit associated with manipulation performed with the neck rotated toward the side of radiculopathy. There is little compelling evidence supporting or disputing the use of manipulation for patients with cervical spine radiculopathy. In our patients, rotary manipulation was associated with a different outcome depending on the direction of neck rotation. Prospective time-series studies and randomized, blind trials are needed to identify the efficacy and effectiveness of different manipulation techniques for this condition.

Nonoperative Management Of Herniated Cervical
Intervertebral Disc With Radiculopathy
Spine (Phila Pa 1976). 1996 (Aug 15); 21 (16): 1877–1883
Although this study does NOT involve chiropractic care per se, it does entail many conservative components of chiropractic management. It is listed here because it makes a powerful care that non-surgical conservative care is highly effective.

Chiropractic Treatment of Cervical Radiculopathy
Caused by a Herniated Cervical Disc
J Manipulative Physiol Ther 1994 (Feb); 17 (2): 119–123
Treatment included chiropractic manipulative therapy, longitudinal cervical traction and interferential therapy. The patient began a regular schedule of treatments, which started on a daily basis but were gradually reduced as the patient progressed. By the third week of treatment, neck and shoulder pain was completely resolved. Subjective evaluation indicated the radicular pain to be improved by 60% within 6 wk. The patient's pain, numbness and grip strength returned to normal within 5 months.

Chiropractic Treatment of Cervical Radiculopathy Caused
by a Herniated Cervical Disc
J Manipulative Physiol Ther 1994 (Feb); 17 (2): 119–123
Treatment included chiropractic manipulative therapy, longitudinal cervical traction and interferential therapy. The patient began a regular schedule of treatments, which started on a daily basis but were gradually reduced as the patient progressed. By the third week of treatment, neck and shoulder pain was completely resolved. Subjective evaluation indicated the radicular pain to be improved by 60% within 6 wk. The patient's pain, numbness and grip strength returned to normal within 5 months. Conservative treatment including chiropractic manipulative therapy seems to be a reasonable alternative to surgery, for cervical radiculopathy caused by a herniated cervical disc. Clinical trials should be performed to evaluate long term success rate, risk of permanent disability, rate of recovery and cost effectiveness of this and other forms of treatment for cervical radiculopathy caused by herniated nucleus pulposus.
Return to the LINKS
Return to SPINAL PAIN MANAGEMENT
Return to DISC HERNIATION & CHIROPRACTIC
Since 3–03–2007
Updated 5-20-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |