

Worsening Trends in the Management and Treatment of Back Pain This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: JAMA Internal Medicine 2013 (Sep 23); 173 (17): 1573–1581 ~ FULL TEXT
OPEN ACCESS John N. Mafi, MD; Ellen P. McCarthy, PhD, MPH; Roger B. Davis, ScD; Bruce E. Landon, MD, MBA, MSc
Division of Primary Care and General Internal Medicine,
Department of Medicine,
Beth Israel Deaconess Medical Center,
Harvard Medical School,
Boston, Massachusetts.
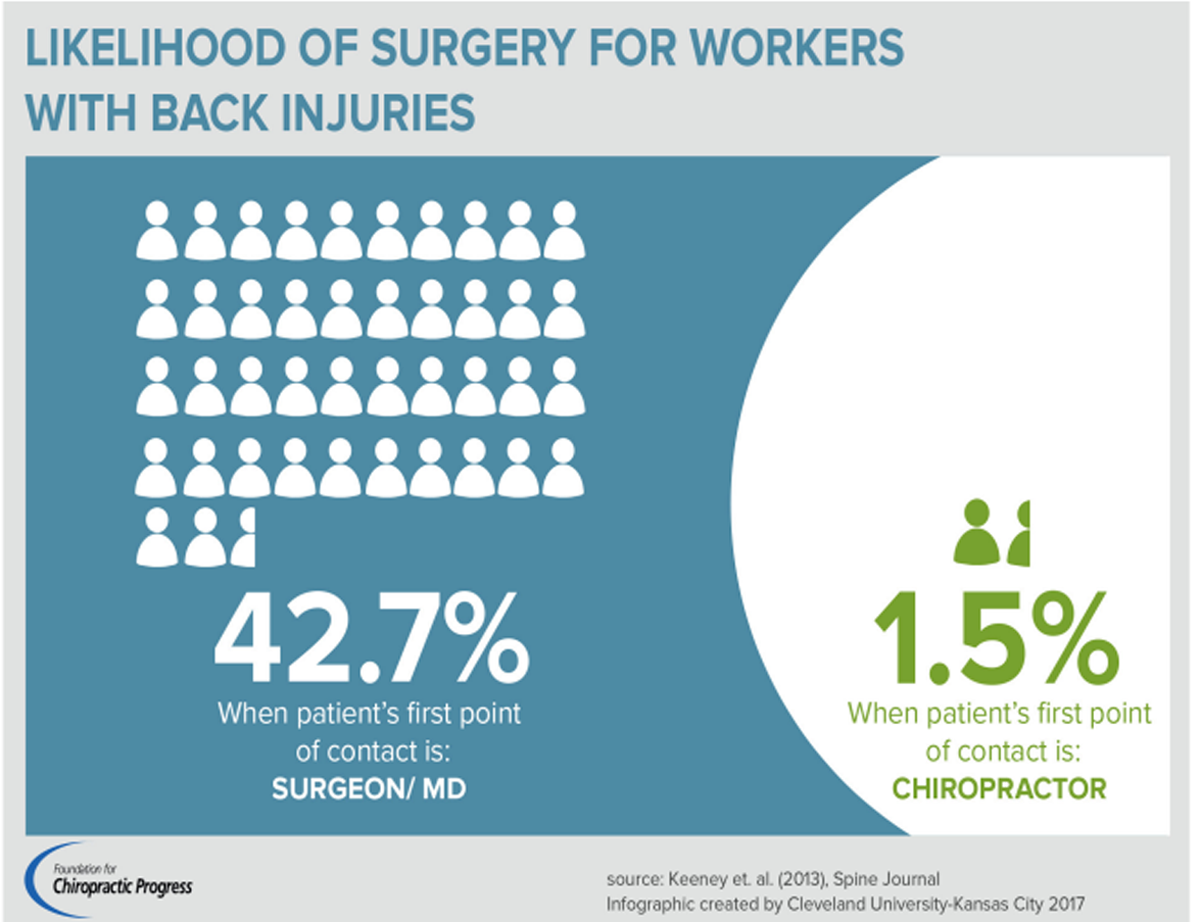
FROM: Keeney ~ Spine 2013 (May 15)Importance: Back pain treatment is costly and frequently includes overuse of treatments that are unsupported by clinical guidelines. Few studies have evaluated recent national trends in guideline adherence of spine-related care.
Objective: To characterize the treatment of back pain from January 1, 1999, through December 26, 2010.
Design, setting, and patients: Using nationally representative data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey, we studied outpatient visits with a chief symptom and/or primary diagnosis of back or neck pain, as well as those with secondary symptoms and diagnoses of back or neck pain. We excluded visits with concomitant "red flags," including fever, neurologic symptoms, or cancer. Results were analyzed using logistic regression adjusted for patient and health care professional characteristics and weighted to reflect national estimates. We also present adjusted results stratified by symptom duration and whether the health care professional was the primary care physician (PCP).
Main outcomes and measures : We assessed imaging, narcotics, and referrals to physicians (guideline discordant indicators). In addition, we evaluated use of nonsteroidal anti-inflammatory drugs or acetaminophen and referrals to physical therapy (guideline concordant indicators).
Results: We identified 23,918 visits for spine problems, representing an estimated 440 million visits. Approximately 58% of patients were female. Mean age increased from 49 to 53 years (P< .001) during the study period. Nonsteroidal anti-inflammatory drug or acetaminophen use per visit decreased from 36.9% in 1999–2000 to 24.5% in 2009–2010 (unadjusted P< .001). In contrast, narcotic use increased from 19.3% to 29.1% (P< .001). Although physical therapy referrals remained unchanged at approximately 20%, physician referrals increased from 6.8% to 14.0% (P< .001). The number of radiographs remained stable at approximately 17%, whereas the number of computed tomograms or magnetic resonance images increased from 7.2% to 11.3% during the study period (P< .001). These trends were similar after stratifying by short-term vs long-term presentations, visits to PCPs vs non-PCPs, and adjustment for age, sex, race/ethnicity, PCP status, symptom duration, region, and metropolitan location.
Conclusions and relevance: Despite numerous published clinical guidelines, management of back pain has relied increasingly on guideline discordant care. Improvements in the management of spine-related disease represent an area of potential cost savings for the health care system with the potential for improving the quality of care.
From the FULL TEXT Article:
Background
Spinal complaints are among the most common reasons for visiting a physician and significantly contribute to healthcare expenditures. Over 10% of visits to primary care physicians relate to back or neck pain (hereafter referred to as back pain)—representing the fifth most common reason for all doctor visits, and accounting for approximately $86 billion in health care spending annually. [1–3] Indirect costs related to lost productivity amount to an additional $20 billion per year, which likely is an underestimate as the prevalence of chronic back pain may be rising. [3–5] Moreover, spending for these conditions has increased more rapidly than overall health expenditures from 1997–2005. [6]
Well-established guidelines for routine back pain stress conservative management including use of non-steroidal anti-inflammatory drugs (NSAIDs) or acetaminophen, and physical therapy, but avoiding early imaging or other aggressive treatments except in rare cases such as those demonstrating acute neurological compromise or other “red flags” such as a history of malignancy. In the absence of these features, routine back pain will usually improve with such conservative treatments within 3 months. [7–9] Prior research among patients with back pain revealed significant increases in use of CT/MRI exams, outpatient surgical procedures, and narcotic prescriptions, but many of these studies are over a decade old, limited to specific populations (e.g., Medicare), or study different aspects of utilization such as surgeries or hospitalizations. [6, 10–15]
In this context, we used nationally representative data on outpatient visits to physicians to evaluate trends in use of diagnostic imaging, physical therapy, referrals to other physicians, and use of medications over the 12–year period from 1999 until 2010. We hypothesized that with the additional guidelines released over this period, [16–22] use of recommended treatments would increase and use of non-recommended treatments would decrease.
METHODS
Data Sources
We used nationally representative data on visits to physicians available from the National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS) for the time period 1999–2010. These surveys are designed to be combined to represent outpatient care in the United States. [23] NAMCS comprises a probability sample of outpatient visits to non-federal, office-based physician practices. Designed in parallel, NHAMCS consists of outpatient visits to hospital-based ambulatory departments, including outpatient clinics, and visits to emergency departments. NAMCS and NHAMCS share common design and survey variables and patient visit weights, and when analyzed together reflect national estimates. [24] Further documentation of survey methods are available at the NCHS website. [25]
Data Collection Procedures
Both NAMCS and NHAMCS use a multi-stage probability sample design to obtain nationally representative samples of ambulatory patient visits in the US. [23] In the first stage of sampling, 112 primary sampling units (PSUs) were selected from among those used in the National Health Interview Survey. For the second stage, physician practices or hospitals were selected from within these PSUs. Finally, in the last stage, physicians or clinics sampled a subset of visits in their practices over a pre-defined time period. This design enables calculation of national-level estimates and associated standard errors using survey weights provided by the NCHS. [25]
Data are collected using a standardized form completed during each patient visit. Both NAMCS and NHAMCS include data on the patient’s primary reason for visit (e.g., chief complaint) two other non-primary reasons for visit, up to 3 diagnoses derived from the International Classification of Diseases, Clinical Modification, Ninth Revision (ICD-9-CM), expected payer for the visit (e.g., Medicare, commercial insurance) various patient demographic characteristics, and medications listed during the visit.
Study Sample
To identify visits for spine-related conditions, we selected outpatient visits (excluding emergency department visits) with a chief complaint and/or a primary diagnosis of back or neck pain, as well as those with secondary complaints and diagnoses of back or neck pain, but unrelated primary reasons for the visit (e.g., hypertension). We used reason for visit codes from both NAMCS and NHAMCS to identify visits with a chief or secondary complaint of back pain (Table A1, Appendix).
In the subset of visits with a chief complaint of back or neck pain (just over 50% of visits in our sample) NAMCS and NHAMCS provide the duration or context of symptoms in five categories: (1) new onset (<3 months duration), (2) acute on chronic flare-up, (3) chronic routine (4) routine/preventative care visit, (5) pre or post-operative visit. This variable was missing 1.3% of the time. We defined ‘acute’ visits by combining those with new onset symptoms with those with acute on chronic flare-up. We then compared the ‘acute’ group’ with those with chronic routine symptoms. Of note, our results were not substantively different when the acute on chronic flare-up category was categorized as “chronic.”
We excluded visits with concomitant red-flag diagnoses or complaints including fever, weight loss, cachexia, neurologic symptoms, cancer, spinal fracture, myelopathy, or post-laminectomy syndrome that might be indicative of something other than routine musculoskeletal back pain.26–28 As a sensitivity analysis we also excluded visits with a coexistent diagnosis with similar treatment options (e.g., knee pain, spasm of muscle) as well as those with concomitant trauma, fracture, various abdominal, musculoskeletal, neurologic, pulmonary, and infectious diagnoses. When including these visits, however, the results were similar (Table A3, Appendix), so we included these visits in our final analyses.
Main Outcomes Measures
We focused on three types of measures: (1) referrals for physical therapy or to other physicians; (2) use of imaging, including both CT/MRI and plain x-ray; and (3) use of medications including non-steroidal anti-inflammatory drugs (NSAIDs, including COX-2 inhibitors), acetaminophen (including both prescription and over-the-counter NSAIDs and acetaminophen), narcotics, tramadol, benzodiazepines and muscle relaxants (e.g., cyclobenzaprine), and agents to treat “neuropathic” pain (e.g., gabapentin). We considered NSAIDs or acetaminophen use as guideline concordant, and considered narcotic prescriptions as guideline discordant.22 Before 2003, NAMCS and NHAMCS only collected data on up to 6 drugs; therefore, in order to maintain consistency over time, we limited analysis of all years to the first 6 drugs listed.
We considered referrals for physical therapy to be concordant with current guidelines, but referrals to other physicians, presumably for consideration of treatments such as injections or surgery to be discordant with current guidelines. We also considered use of imaging studies for routine back pain to be discordant with clinical guidelines. Although the American College of Physicians guidelines were published in 2007, clinical guideline recommendations have remained generally consistent across specialties and around the world since the 1990s (see also Tables A8 and A9, Appendix).29,30 Moreover, although some visits classified as guideline discordant might in fact be appropriate if additional clinical data (e.g., neurologic examination) were available, our focus is less on the proportion of guideline adherent treatments and more on trends over time, and we have no reason to suspect that the proportion of visits with indications for various procedures or treatments would have changed over time.
Finally, using logistic regression pooled across the entire study sample and including a control variable for year, we evaluated factors independently associated with ordering CT/MRI studies, narcotic medication use, and referring to another physician—the three outcomes we felt were most important.
Stratified Analyses
In order to evaluate the degree to which symptom duration affected our results, we analyzed the subset of visits with a chief complaint of back pain after stratifying by acute versus chronic presentations as defined above.
We also stratified our analyses of the full sample based on whether the provider identified herself as the patient’s PCP or not. We also assessed interactions between visit year and symptom duration, and visit year and PCP-status. Additionally, we stratified results by data from NAMCS versus NHAMCS (Table A10, Appendix). Finally, because comorbid conditions were not collected until 2005, we examined trends in the 14 comorbid conditions collected from 2005–2010 using ?2 tests.
Statistical Analysis
We assessed unadjusted trends using bivariable logistic regression where appropriate and evaluated categorical variables using ?2 tests. For each outcome measure, we report proportions of utilization for each time interval after pooling the survey data into 6 two-year intervals as recommended by the NCHS (1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, and 2009–2010). For adjusted and stratified analyses, we estimated logistic regression models for each outcome of interest focusing on a linear trend for each two-year interval, and adjusting for age, sex, race/ethnicity, insurance status, whether the provider was the PCP, location in a metropolitan area, region, and the duration of symptoms when available (of note, because physician specialty information was only available in NAMCS, this variable was not included in our models; however, sensitivity analyses in the NAMCS subset revealed that the presence of specialty variables did not alter our results). Race/ethnicity was defined by the providers completing the survey instruments. We divided race into three categories: White, Black, and Other, which includes persons of Asian, Native Hawaiian, Pacific Islander, American Indian, or multiple races. We then re-categorized patients of any race who were identified as Hispanic in order to create a single four-level race/ethnicity variable.
All analyses were performed using SAS-callable SUDAAN, version 10.0 (RTI, Research Triangle Park, North Carolina) to account for the complex survey sample design. As noted above, we followed the NCHS recommendations for combining the NAMCS and NHAMCS datasets.24 The Harvard Medical School Committee on Human Studies determined that this study was exempt from review.
RESULTS

Table 1 We identified 23,918 visits related to back pain, representing an estimated 440 million visits over the 12–year period, or an average of 73 million visits per year. The number of patient visits related to back pain increased over the time period from 3,350 visits in 1999–2000 (representing 61 million visits, or 3.1% of all visits) to 4,078 visits during 2009–2010 (representing 87 million visits or 3.5% of all visits). Table 1 summarizes trends in visit characteristics among patients presenting with back pain (Table A5 in the Appendix provides year-by-year trends). Mean age increased from 49 to 53 years (p<.001), while the proportion of females remained stable at 58%. Seventeen percent of visits were from Medicare enrollees in 1999–2000 as compared with 28% in 2009–2010 (p=.01). Among those with a chief complaint of back pain (51% of sample), the proportion with acute or new onset symptoms fell from 62% in 1999–2000 to 59% in 2009–2010, while those with chronic symptoms increased from 30% to 37% during the same time period (p<.01). Comorbidities did not significantly change with the exception of asthma, which increased from 3.6% in 2005–2006 to 6.5% in 2009–2010 (p<.01,Table A6, Appendix).
Unadjusted Trends in Utilization

Table 2 Medications Use of NSAIDs/acetaminophen fell from 37% in 1999–2000 to 25% in 2009–2010 (p<.001, Table 2). In contrast, use of narcotics increased from 19% to 29% during the same time period (p<.001 for trend). Muscle relaxants and benzodiazepines increased from 20% in 1999–2000 to 24% in 2009–2010 (p<.001) and use of neuropathic agents more than doubled, climbing from 3.4% to 7.9% during the same time period (p<.001).
Referrals and Imaging Referrals to physical therapy remained unchanged at approximately 20% across the study period, but referrals to other physicians rose from 6.8% in 1999–2000 to 14% in 2009–2010 (p<.001). There was no observed change in the use of plain radiographs (~17% across the study period), but use of MRI/CT scans increased from 7.2% in 1999–2000 to 11% in 2009–2010 (p<.001).
Adjusted and Stratified Trends in Utilization
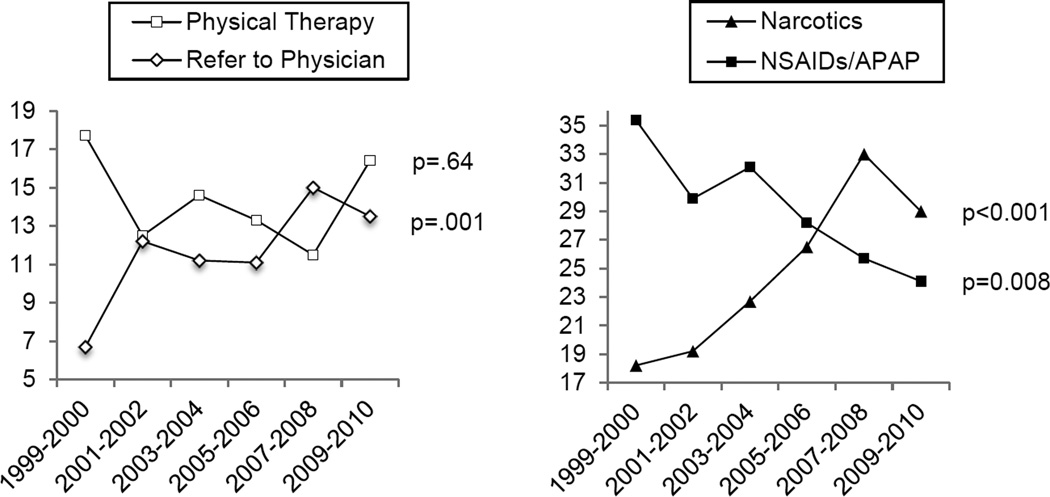
Figure 1

Table 3 After adjustment, trends in utilization did not differ substantively from the unadjusted findings. Figure 1 shows adjusted proportions of referrals to physical therapy, referrals to physicians, narcotic and NSAIDs/acetaminophen use over time.
Stratified analyses of visits with a chief complaint of back pain comparing visits with acute versus chronic pain revealed similar trends for the two groups over the study time period (Table 3). Among patients with chronic symptoms, however, referrals to other physicians increased more rapidly when compared to those with acute symptoms (p=.01 for interaction with time), with referrals to physicians increasing from 3% to 13% for chronic symptoms and from 6.8 to 11% for those with acute symptoms during the study period (p<.001 and p=.07 for trend respectively). Although changes in referrals to other physicians among patients with acute symptoms and CT/MRI use among patients with chronic symptoms did not achieve statistical significance, use of these indicators also increased over time for both groups.

Table 4 Comparing visits to PCPs and non-PCPs also revealed similar trends, albeit with a few exceptions (Table 4). Among non-PCPs, CT/MRI use increased somewhat more rapidly when compared to visits to PCPs, increasing from 4.9% to 6.6% among PCPs (p=.02) versus 9.5% to 14% for non-PCPs (p=.002) throughout the study period; however, interactions with time were non-significant. Finally, NSAIDs/acetaminophen medications declined by nearly one half among PCPs (p<.001 for trend) while remaining flat among non-PCPs (p=.47 for trend), and this difference was statistically significant (p=.01).
Correlates of Use
Table A7 in the Appendix presents the results of multivariable logistic regression models estimating use of CT/MRI studies, referrals to physicians, and narcotic prescriptions with visits pooled over the entire time period. Patients of Black, Hispanic, and other race/ethnicity had lower odds of receiving narcotic medications (0.77, 95% CI [0.65, 0.92], 0.60 [0.39, 0.95], and 0.51 [0.40, 0.65], respectively), as did female patients (0.86 [0.77, 0.96]). Uninsured patients had lower odds of being referred to other physicians (0.74 [0.57, 0.97]). A sub-analysis of specialists revealed that neurologists and orthopedic surgeons had higher odds of ordering CT and MRI exams (3.57 [2.60, 4.90]). Finally, providers in the Southern and Western U.S. had greater odds of prescribing narcotic medications (1.56 [1.21, 2.02] and 1.57 [1.22, 2.03] respectively).
Comment
In this nationally representative study of treatment patterns for patients presenting to physicians with back pain over the past decade, we observed several notable findings. First, we observed a significant rise in the frequency of treatments that are considered discordant with current guidelines including use of advanced imaging, such as CT or MRI, referrals to other physicians (presumably for procedures or surgery), and use of narcotics. Second, we also observed a decline in use of first-line medications such as NSAIDs or acetaminophen, but no change in referrals to physical therapy. Finally, although opiate prescriptions increased markedly over this time period, we also observed lower odds of receiving narcotics among female, Black, Hispanic, and other race/ethnicity patients, which may signify potential disparities in pain management that have also been noted previously. [31FONT>]
The 106% increase in referrals to other physicians is a previously unrecognized and important finding, as such referrals likely contributed to the recent rise in costly, morbid, and often ineffective outpatient spine surgeries observed in other studies. [32–35] Recent meta-analyses and research of lumbar fusion surgery have not revealed improvement in patient outcomes and demonstrate that these procedures lead to significant adverse consequences including 5.6% with life-threatening complications and 0.4% mortality. [36, 37>] Further, when comparing visits with the patient’s self-identified PCP versus those with another provider, we found that non-PCPs were much more likely to order advanced imaging. Presumably, this group includes those who perform procedures such as spinal surgery. Thus, these referrals from PCPs are likely to result in substantial downstream utilization that is not concordant with current guidelines.
We also found a 48% decline in first-line NSAIDs/acetaminophen use accompanied by a 53% rise in narcotic prescriptions, including a near doubling among patients presenting with chronic back pain. These results are not explained by a change in the frequency of acute versus chronic presentations or the extent to which patients were seen by their PCP versus another physician as similar trends were observed for each of these groups in our stratified analyses. Although some of the decrease in NSAIDs might have been due to the decline in use of COX-2 inhibitors, the dramatic fall in use of first-line therapies accompanied by the rapid rise in narcotic prescriptions raise significant concerns.
A recent meta-analysis revealed that narcotics provide little to no benefit in acute back pain, have no proven efficacy in chronic back pain, and found that 43% of patients had concurrent substance abuse disorders—with aberrant medication-taking disorders as high as 24% of cases of chronic back pain.38 Although we currently lack adequate data to make firm recommendations on narcotic medications, which may be indicated in certain circumstances, such increases in narcotic prescriptions may be contributing to a current crisis in public health: the rapid rise in narcotic overdose deaths parallels a reported 300% increase in the U.S. sales of prescription narcotics since the 1990s. In 2008, overdoses in narcotic analgesics led to an estimated 14,800 deaths—more than cocaine and heroin combined. [39–41]
Our findings also confirm an inappropriate rise in advanced diagnostic imaging that has been seen previously, [12–14, 42] with use of CT or MRI increasing by 53% in our study sample. Six randomized-controlled trials have shown that imaging in the acute setting provides neither clinical nor psychological benefit to patients with routine back pain26 and multiple prospective studies have shown the lack of serious pathology in the absence of red flag symptoms. [43] In addition to being low value, the overuse of diagnostic imaging leads to more exposure to ionizing radiation. In 2007, a projected 1,200 additional future cancers were created by the 2.2 million lumbar CT scans performed in the U.S. [44, 45] Finally, the dramatic rise in spine surgeries seen over the last decade is almost certainly related to the overuse of imaging. One study revealed that early MRI for acute back pain was associated with an eight-fold increased risk of surgery, while another found that regions with more MRIs do more surgeries, with 22% of the variability in spine surgery rates explained by rates of spine MRI use—more than twice the predictive power of patient characteristics. [46, 47]
Our study is subject to several limitations. Although we lacked complete data on the duration of symptoms, we present stratified results for acute versus chronic presentations that showed similar trends. Moreover, these visits comprised over half of our sample. Second, because NAMCS and NHAMCS are visit-level datasets, we lacked longitudinal data on treated patients. Consequently, we could not measure treatment patterns over time for individual patients. Because these visit-level data are collected in the same way each year, however, trends over time are likely to be reflective of changes in practice patterns and not to changes in the patient population presenting for treatment. A lack of major changes in most of our own population characteristics also supports this assessment, and those factors that did change (e.g., age, insurance status) were accounted for in our model. Furthermore, our analyses control for important potential confounders that might have changed over time such as the proportion of acute versus chronic visits and whether the visit was with a self-identified PCP. Finally, because comorbidity data were not collected until 2005, we could not use comorbidities in our adjusted analyses. However, our evaluation of trends in the 14 comorbid chronic conditions (including arthritis and depression) in our sample revealed significant increases only for asthma, which had very low prevalence rates that were unlikely to alter our results.
Despite numerous published national guidelines, management of routine back pain increasingly has relied on advanced diagnostic imaging, referrals to other physicians, and use of narcotics, with a concomitant decrease in NSAIDs or acetaminophen use and no change in physical therapy referrals. With healthcare costs soaring, improvements in the management of back pain represent an area of potential cost savings for the healthcare system while also improving the quality of care.
Supplementary Material
Acknowledgements
Dr. Mafi was supported by the NRSA training grant (T32HP12706) from the U.S. Health Services and Research Administration (HRSA) and the Ryoichi Sasakawa Fellowship Fund. Dr. Davis was supported by the Harvard Catalyst (NIH Award #UL1 RR 025758). Dr. Mafi had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
We gratefully acknowledge Edward Marcantonio, M.D., S.M., Christina Wee, M.D., M.P.H., John Orav, Ph.D., and John Ayanian, M.D., M.P.P. for their methodological and conceptual advice.
Disclosures:
None reported.
References:
Hart LG, Deyo RA, Cherkin DC.
Physician office visits for low back pain. Frequency, clinical evaluation,
and treatment patterns from a U.S. national survey.
Spine. 1995;20(1):11–19Deyo RA, Mirza SK, Martin BI.
Back pain prevalence and visit rates: estimates from US national surveys, 2002.
Spine. 2006;31(23):2724–2727.Martin BI, Turner JA, Mirza SK, et al.
Trends in Health Care Expenditures, Utilization, and Health Status Among US Adults
with Spine Problems, 1997–2006
Spine (Phila Pa 1976). 2009 (Sep 1); 34 (19): 2077–2084Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R.
Lost Productive Time and Cost Due to Common Pain Conditions in the US Workforce
JAMA 2003 (Nov 12); 290 (18): 2443–2454Freburger JK, Holmes GM, Agans RP, et al.
The Rising Prevalence of Chronic Low Back Pain.
Archives of Internal Medicine. 2009;169(3):251–258.Martin, BI, Deyo, RA, Mirza, SK et al.
Expenditures and Health Status Among Adults With Back and Neck Problems
JAMA 2008 (Feb 13); 299 (6): 656–664Pengel LHM, Herbert RD, Maher CG, Refshauge KM.
Acute low back pain: systematic review of its prognosis.
BMJ. 2003;327(7410):323.Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr., Shekelle P, Owens DK:
Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline
from the American College of Physicians and the American Pain Society
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 478–491Williams CM, Maher CG, Hancock MJ et al.
Low Back Pain and Best Practice Care:
A Survey of General Practice Physicians
Archives of Internal Medicine 2010 (Feb 8); 170 (3): 271–277Gray DT, Deyo RA, Kreuter W, et al.
Population-based trends in volumes and rates of ambulatory lumbar spine surgery.
Spine. 2006;31(17):1957–1963.Feuerstein M, Marcus SC, Huang GD.
National trends in nonoperative care for nonspecific back pain.
Spine J. 2004;4(1):56–63.Weiner DK, Kim Y-S, Bonino P, Wang T.
Low back pain in older adults: are we utilizing healthcare resources wisely?
Pain Med. 2006;7(2):143–150.Deyo RA, Mirza SK, Turner JA, Martin BI.
Overtreating Chronic Back Pain: Time to Back Off?
J Am Board Fam Med. 2009 (Jan); 22 (1): 62–68Mitchell JMJ.
Utilization trends for advanced imaging procedures: evidence from individuals with
private insurance coverage in California.
Medical care. 2008;46(5):460–466.Jackson JL, Browning R.
Impact of national low back pain guidelines on clinical practice.
South. Med. J. 2005;98(2):139–143.Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr., Shekelle P, Owens DK:
Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline
from the American College of Physicians and the American Pain Society
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 478–491van Tulder M, Becker A, Bekkering T, Breen A, Carter T, Gil del Real MT.
European Guidelines for the Management of Acute Nonspecific Low Back Pain in Primary Care
European Spine Journal 2006 (Mar); 15 Suppl 2: S169–191Airaksinen O, Brox JI, Cedraschi C, et al.
COST B13 Working Group on Guidelines for Chronic Low Back Pain Chapter 4.
European Guidelines for the Management of Chronic Nonspecific Low Back Pain
European Spine Journal 2006 (Mar); 15 Suppl 2: S192–300
See also the archived: European Guidelines Backpain Europe WebsiteGoertz M, Thorson D, Bonsell J, et al.
Adult Acute and Subacute Low Back Pain
Institute for Clinical Systems Improvement; Fifteenth Edition January 2012Davis PC, Wippold FJ, Brunberg JA, et al.
ACR Appropriateness Criteria on low back pain.
J Am Coll Radiol. 2009;6(6):401–407.Albright J, Allman R, Bonfiglio RP, et al.
Philadelphia Panel evidence-based clinical practice guidelines on selected
rehabilitation interventions for low back pain. 2001Chou R, Huffman LH;
Medications for Acute and Chronic Low Back Pain: A Review of the Evidence for an
American Pain Society/American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 505–514McCaig LF, McLemore T.
Plan and operation of the National Hospital Ambulatory Medical Survey. Series 1:
programs and collection procedures.
Vital Health Stat 1. 1994;(34):1–78.National Center for Health Statistics. Using ultimate cluster models.
[Accessed February 8, 2013];2004 :1–5. Available at:
http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htmNational Center for Health Statistics.
[Accessed February 25, 2013];Ambulatory Health Care Data. Available at:
http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htmChou R, Qaseem A, Owens DK, Shekelle P.
Diagnostic Imaging for Low Back Pain: Advice for High-Value Health Care From
the American College of Physicians.
Annals of internal medicine. 2011;154(3):181–189.National Committee for Quality Assurance.
Technical Specifications. Washington, DC: National Committee for Quality Assurance; 2010. HEDIS 2011:
Healthcare Effectiveness Data and Information Set, vol 2.Kale MS, Bishop TF, Federman AD, Keyhani S.
Trends in the Overuse of Ambulatory Health Care Services in the United States.
Arch Intern Med. 2012:1–7.Koes BW, van Tulder MW, Ostelo R, Kim Burton A, Waddell G.
Clinical Guidelines for the Management of Low Back Pain
in Primary Care: An International Comparison
Spine (Phila Pa 1976) 2001 (Nov 15); 26 (22): 2504–2513Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C.
An Updated Overview of Clinical Guidelines for the Management of
Non-specific Low Back Pain in Primary Care
European Spine Journal 2010 (Dec); 19 (12): 2075–2094Dominick KL, Bosworth HB, Dudley TK, Waters SJ, Campbell LC, Keefe FJ.
Patterns of opioid analgesic prescription among patients with osteoarthritis.
J Pain Palliat Care Pharmacother. 2004;18(1):31–46.Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES.
United States' trends and regional variations in lumbar spine surgery, 1992–2003.
Spine. 2006;31(23):2707–2714.Schafer J, O'Connor D, Feinglass S, Salive M.
Medicare Evidence Development and Coverage Advisory Committee Meeting on lumbar fusion surgery
for treatment of chronic back pain from degenerative disc disease.
Spine. 2007;32(22):2403–2404.Mirza SK, Deyo RA.
Systematic review of randomized trials comparing lumbar fusion surgery to nonoperative care
for treatment of chronic back pain.
Spine. 2007;32(7):816–823.Gray DT, Deyo RA, Kreuter W, et al.
Population-based trends in volumes and rates of ambulatory lumbar spine surgery.
Spine. 2006;31(17):1957–1963. discussion 1964.Gibson JNA, Waddell G.
Surgery for degenerative lumbar spondylosis: updated Cochrane Review.
Spine. 2005;30(20):2312–2320.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG.
Trends, Major Medical Complications, and Charges Associated
with Surgery for Lumbar Spinal Stenosis in Older Adults
JAMA 2010 (Apr 7); 303 (13): 1259–1265Martell BA, O'Connor PG, Kerns RD, et al.
Systematic review: opioid treatment for chronic back pain: prevalence,
efficacy, and association with addiction.
Ann. Intern. Med. 2007;146(2):116–127.Luo X, Pietrobon R, Hey L.
Patterns and trends in opioid use among individuals with back pain in the United States.
Spine. 2004;29(8):884–890. discussion 891.CDC - Prescription Painkiller Overdoses Policy Impact Brief -
Home and Recreational Safety - Injury Center. [Accessed February 24, 2013];NCHS. Available at:
http://www.cdc.gov/homeandrecreationalsafety/rxbrief/Dunn KM, Saunders KW, Rutter CM, et al.
Opioid prescriptions for chronic pain and overdose: a cohort study.
Ann. Intern. Med. 2010;152(2):85–92.Pham HH, Landon BE, Reschovsky JD, Wu B, Schrag D.
Rapidity and modality of imaging for acute low back pain in elderly patients.
Arch Intern Med. 2009;169(10):972–981.Deyo RA, Diehl AK.
Cancer as a cause of back pain.
Journal of general internal medicine. 1988Chou R, Deyo RA, Jarvik JG.
Appropriate Use of Lumbar Imaging for Evaluation of Low Back Pain.
Radiol Clin North Am 2012 Jul;50(4):569-85Berrington de González A, Mahesh M, Kim K-P, et al.
Projected cancer risks from computed tomographic scans performed in the United States in 2007.
Arch Intern Med. 2009;169(22):2071–2077.Webster BS, Cifuentes M.
Relationship of early magnetic resonance imaging for work-related acute low back pain
with disability and medical utilization outcomes.
J. Occup. Environ. Med. 2010;52(9):900–907.Lurie JD, Birkmeyer NJ, Weinstein JN.
Rates of advanced spinal imaging and spine surgery.
Spine. 2003;28(6):616–620.
Return to LOW BACK PAIN
Return to LOW BACK GUIDELINES
Return to CHIROPRACTIC CARE FOR VETERANS
Since 1-30-2021


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |