Severe Pain in Veterans: The Effect of Age and Sex,
and Comparisons with the General PopulationThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Pain 2017 (Mar); 18 (3): 247–254 ~ FULL TEXT
OPEN ACCESS Richard L. Nahin, Ph.D., M.P.H.
National Center for Complementary and Integrative Health,
National Institutes of Health,
Bethesda, Maryland
FROM: Nahin ~ Pain 2017This study provides national prevalence estimates of US military veterans with severe pain, and compares veterans with nonveterans of similar age and sex. Data used are from the 2010 to 2014 National Health Interview Survey on 67,696 adults who completed the Adult Functioning and Disability Supplement. Participants with severe pain were identified using a validated pain severity coding system imbedded in the National Health Interview Survey Adult Functioning and Disability Supplement.
Prevalence of severe pain, defined as that which occurs "most days" or "every day" and bothers the individual "a lot," is strikingly more common in veterans than in members of the general population, particularly in veterans who served during recent conflicts. Additional assistance may be necessary to help veterans cope with their pain.
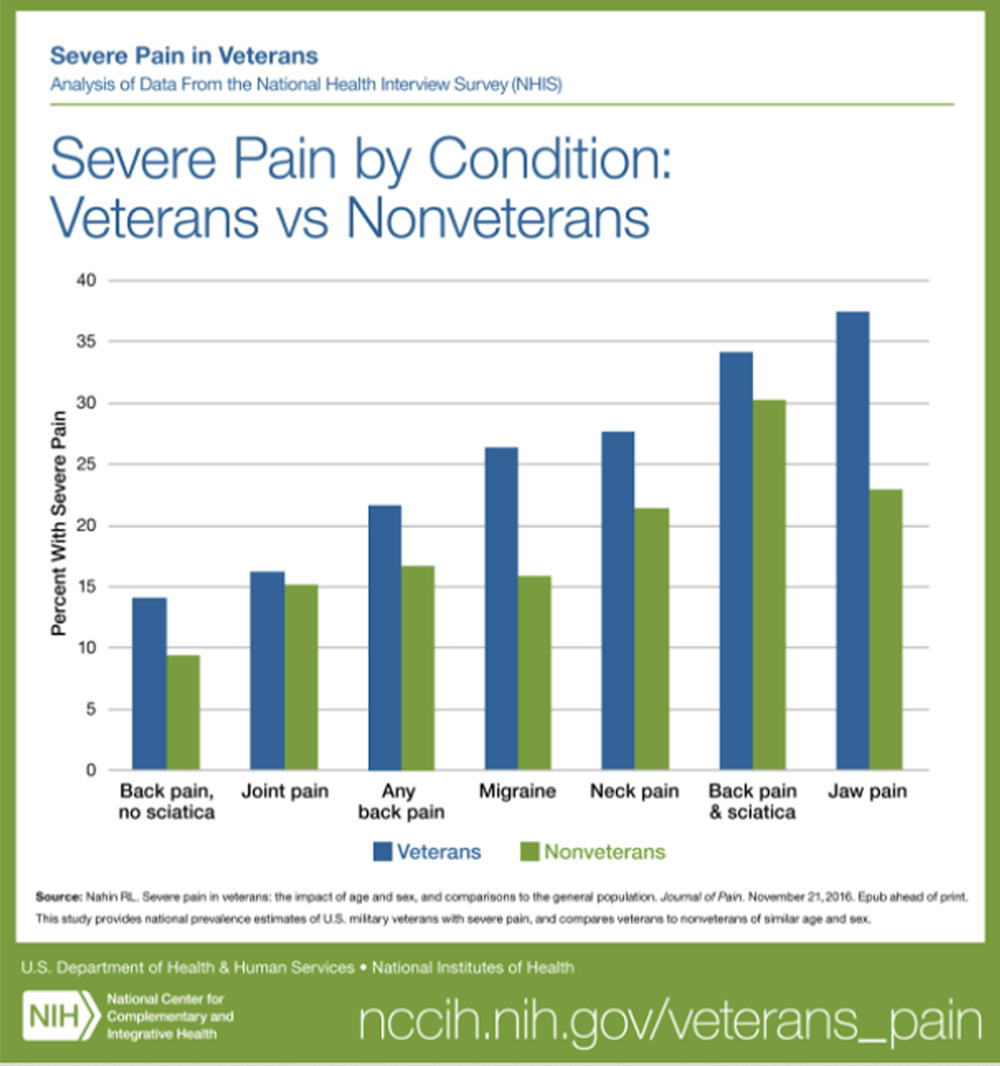
It was estimated that 65.5% of US military veterans reported pain in the previous 3 months, with 9.1% classified as having severe pain. Compared with veterans, fewer nonveterans reported any pain (56.4%) or severe pain (6.4%). Whereas veterans aged 18 to 39 years had significantly higher prevalence rates for severe pain (7.8%) than did similar-aged nonveterans (3.2%), veterans age 70 years or older were less likely to report severe pain (7.1%) than nonveterans (9.6%). Male veterans (9.0%) were more likely to report severe pain than male nonveterans (4.7%); however, no statistically significant difference was seen between the 2 female groups. The prevalence of severe pain was significantly higher in veterans with back pain (21.6%), jaw pain (37.5%), severe headaches or migraine (26.4%), and neck pain (27.7%) than in nonveterans with these conditions (respectively: 16.7%, 22.9%, 15.9%, and 21.4%). Although veterans (43.6%) were more likely than nonveterans (31.5%) to have joint pain, no difference was seen in the prevalence of severe pain associated with this condition.
Perspective:
Keywords Veteran; back pain; joint pain; migraine; pain severity.
From the FULL TEXT :
INTRODUCTION
Military Veterans make up approximately 9–10% of the US adult population, [46] and are unique in many ways. At the time of entering into military service, Veterans are generally healthier than the typical US adult of similar age because of the rigorous physical and mental screening requirements to join the military. Active duty military are required to maintain specified physical requirements throughout their service and have access to comprehensive medical care, including preventive care. However, during service they are at risk for both combat-related and unrelated physical injuries, and are often exposed to both environmental and mental stressors. Thus, research has shown that military Veterans have poorer overall health-related quality-of-life than nonveterans. [13, 18, 23, 25] Veterans are also more likely than age-matched nonveterans to have psychological distress and chronic health conditions (e.g., asthma, cancer, diabetes, emphysema, hypertension, heart disease, kidney disease). [23]
A number of reports have documented high prevalence of pain-related conditions in Veterans includingabdominal pain, [20, 43, 44]
arthritis, [8, 10, 12, 18, 22, 30]
back pain, [5, 16, 20–22]
fibromyalgia, [10]
headache, [31, 44] and
joint pain [7, 16, 20, 21, 31, 43, 44]especially among the Veterans of recent military conflicts in Iraq and Afghanistan. Veterans also score poorly on the SF-36 bodily pain scale [17, 21, 22, 40] and frequently report that their pain interferes with usual activities. [4, 6]
Several studies have directly compared pain in military Veterans to nonveterans using nationally representative data from the Behavioral Risk Factor Surveillance System (BRFSS). [4, 8, 18, 30] Three studies using the BRFSS examined the prevalence of arthritis in different years. [8, 18, 30] All three studies found higher prevalence of arthritis in Veterans (range: 31.5%–51.5%) than nonveterans (range: 21.5%–25.6%). A fourth BRFSS study [4] found higher prevalence of pain within the past 30 days among male Veterans (6.9%) than male nonveterans (3.6%).
Although this literature identifies the prevalence of pain-related health conditions among Veterans, to our knowledge no previous study has examined the severity of pain in a nationally representative population of Veterans, or examined the association of pain severity with specific pain-related conditions (i.e., back pain, jaw pain, joint pain, neck pain, and severe headaches or migraine).
The specific objectives of this study were, therefore, to:1) compare the 3-month prevalence of both any pain and severe pain between Veterans and nonveterans;
2) examine the relationship of age and sex with pain prevalence and severity in Veterans and nonveterans; and
3) compare the prevalence of severe pain associated with specific pain-related conditions in Veterans and nonveterans.Results from this study may help guide practitioners caring for Veterans and may be of value in future iterations of the Department of Veterans Affairs (VA) Pain Management Strategy. [47]
DISCUSSION
Combining data from five consecutive years of the NHIS permitted us to compare the prevalence of pain in a population sample of 6,647 Veterans and 61,049 non-veterans. More Veterans than nonveterans reported having pain in the previous 3 months (Veterans 65.6%, nonveterans 56.4%). The rate of severe pain was almost 50% higher in Veterans (9.1%) than in nonveterans (6.3%). The difference was particularly striking for younger Veterans (18–39), who were substantially more likely to report suffering from severe pain than nonveterans of similar ages even after controlling for underlying demographic characteristics. This younger group of Veterans is undoubtedly over-represented by those who served during the time of the wars in Afghanistan and Iraq. While previous studies have identified painful health conditions as a significant burden among veterans, to our knowledge only three studies directly compared Veterans and nonveterans, and these studies have only looked at arthritis. [8, 18, 30] Thus, the present data comparing the prevalence rates of back pain (with and without sciatica), jaw pain, joint pain (which only partially overlaps with arthritis pain), severe headaches and migraine, and neck pain in Veterans and non-Veterans are all unique observations. Also, while previous studies have compared overall health among US Military Veterans and nonveterans, this is the first study to directly compare the severity associated with painful health conditions amongst these groups. In this regard, the data address a need recognized in the US National Pain Strategy [35] to go beyond simple studies of disease prevalence and instead “identify high-impact pain in both the general population and for anatomically defined painful conditions.”
The NHIS data does not permit inferences about whether differences in health care may contribute to the high prevalence of severe pain in younger Veterans. Increasing evidence is accumulating for the effectiveness of multidisciplinary pain management strategies, [11, 14, 15, 24, 36, 41, 42] including the VA’s own stepped care pain management approach, [3] to manage severe chronic pain. In this regard, it is noted that younger Veterans are both less likely to have health insurance and less likely to receive care in Veteran’s administration facilities than older Veterans. [1, 45] These factors may limit the availability of multidisciplinary pain management strategies to younger Veterans.
Prospective studies have suggested that individuals with musculoskeletal injuries who are receiving disability compensation have worse outcomes than those not receiving compensation. [2] A recent systematic review concluded that there was an association between compensation (and related factors) and poorer health after a musculoskeletal injury. [29] Since, the NHIS does not capture information on whether individuals received any financial compensation for work- or service-related injuries, we were unable to explore the impact of these variables in our regression model. In particular, it would be informative to compare the prevalence with which Veterans receive compensation for service-related injuries versus compensation for work-related injuries in nonveterans. Depending on these two prevalence rates, our regression analysis might have either over- or under-estimated the differences in severe pain between Veterans and nonveterans.
This report not only offers important information on pain in Veterans from a large nationally representative dataset, but also provides some insights into pain severity associated with common pain-related conditions. In this regard, we are aware of only one other nationally representative survey that compared pain severity among different painful health conditions. Johannes et al. [19] reported that 32% of individuals with lower back pain and 29% of those with arthritis had severe pain (defined as a score of 7+ on an 11-point Likert-type pain scale) in the last 3 months versus 16.6%–21.6% for back pain and 15.2%–16.2% for joint pain in the present study. However, the two studies had very different methodologies that might explain these differences. For instance, Johannes et al. [19] was an Internet-based study with questions on pain severity and underlying health conditions limited to those who had pain lasting at least 6 months (which they defined as chronic pain). It is reasonable to expect that a cohort of individuals with chronic pain would report more severe pain than a cohort of the general population. Future studies using the Washington Group pain questions might directly assess the relationship between pain severity in individuals with either acute or chronic pain.
LIMITATIONS
For the combined years 2010–2014, the NHIS had a relatively high response rate of 62% for the randomly chosen “sample adult.” However, analyzes have shown that NHIS responders and non-responders differ on many characteristics.5 Some of these characteristics, such as older age (current analysis) and self-identifying as white, [32] are related to both increasing levels of pain in the general population and to Veteran status (data not shown). While our regression analysis allowed us to control for confounding in responders, it did not mitigate any bias resulting from differential levels of pain in non-responders. The direction of this bias is unknown.
The current study has several limitations beyond those already mentioned. First, the data are cross-sectional and cannot prospectively assess clinical outcomes associated with pain severity. Second, since the NHIS did not collect pain treatment information, we were unable to determine whether differences in treatment could have further explained the difference in pain experiences of the participants. Third, although the NHIS sampling design allows for unbiased estimates of national trends, the data are limited to a noninstitutionalized population. Future research should consider nationally representative pain assessment for persons in VA facilities, nursing homes, hospices, and other residential healthcare facilities, since these persons are likely to be disproportionately affected with pain-related conditions. Fourth, the NHIS data do not identify any specific aspects of military service including whether a veteran had served in a combat role, their military occupation and rank, years of military service, and their branch of the armed forces (i.e., Army, Navy, Air Force, Marines). These factors likely impact pain prevalence and severity. It is also not possible to distinguish Veterans who were receiving outpatient care at VA facilities versus those who were not. It is known that Veterans using VA facilities have poorer health status (i.e., number of medical conditions, number of outpatient physician visits, number of hospital admissions) than Veterans not using these facilities. [1]
CONCLUSIONS
US military Veterans had higher pain prevalence and severity than nonveterans. These discrepancies appear particularly prominent among the youngest Veterans who likely served during the recent wars in Iraq and Afghanistan. The increased pain suffered by Veterans suggest that more attention should be paid to helping this population cope with their pain. It may be that some Veterans would benefit from a revised pain management plan that addresses the full range of biological, psychological, and social effects of pain on the individual. [35] For others, additional services may be needed to help manage the impact of severe pain and related disability on daily activities. Successful implementation of the National Pain Strategy35 might facilitate both of these outcomes.
Highlights
National estimates of severe pain are presented for U.S. Military veterans
Severe pain was about 50% higher in veterans than nonveterans
Veterans aged 18–39 were twice as likely to have severe pain than nonveterans
Veterans with back, jaw and migraine pain reported more severe pain than nonveterans
Acknowledgments
The author does not have a conflict to disclose. The author’s time and effort on this project were supported as part of his official duties as a federal employee. No other sources of funding were involved. The data contained within this report have not been previously reported in any other manuscript or meeting abstract.
The author thanks Ms. Danita Byrd-Clark, B.B.A., of Social & Scientific Systems, for her programming skills, and the many NCCIH staff who read and commented on earlier versions of this work.
References:
Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160:3252–3257
Atlas SJ, Chang Y, Keller RB, Singer DE, Wu YA, Deyo RA. The impact of disability compensation on long-term treatment outcomes of patients with sciatica due to a lumbar disc herniation. Spine (Phila Pa 1976) 2006;31:3061–9
Bair MJ, Ang D, Wu J, Outcalt SD, Sargent C, Kempf C, Froman A, Schmid AA, Damush TM, Yu Z, Davis LW, Kroenke K. Evaluation of stepped care for chronic pain (ESCAPE) in veterans of the Iraq and Afghanistan conflicts: a randomized clinical trial. JAMA Intern Med. 2015;175:682–689
Barrett DH, Boehmer TK, Boothe VL, Flanders WD, Barrett DH. Health-related quality of life of US military personnel: a population-based study. Mil Med. 2003;168:941–947
Dahlhamer JM, Simile CM. Proceedings of the Government Statistics Section, American Statistical Association. American Statistical Association; Washington, D.C: 2009. Subunit nonresponse in the National Health Interview Survey (NHIS): An exploration using paradata; pp. 262–276
Dobscha SK, Clark ME, Morasco BJ, Freeman M, Campbell R, Helfand M. Systematic review of the literature on pain in patients with polytrauma including traumatic brain injury. Pain Med. 2009;10:1200–1217
Doebbeling BN, Clarke WR, Watson D, Torner JC, Woolson RF, Voelker MD, Barrett DH, Schwartz DA. Is there a Persian Gulf War syndrome? Evidence from a large population-based survey of veterans and nondeployed controls. Am J Med. 2000;108:695–704
Dominick KL, Golightly YM, Jackson GL. Arthritis prevalence and symptoms among US nonveterans, veterans, and veterans receiving Department of Veterans Affairs healthcare. J Rheumatol. 2006;33:348–354
Economic and Social Commission for Asian and the Pacific. Results of the testing of the ESCAP/WG extended question set on disability. United Nations; [Accessed on May 26, 2016]. Available at:
http://www.cdc.gov/nchs/data/washington_group/resultsofthetestingoftheescap
-wgquestionsetondisability.pdfEisen SA, Kang HK, Murphy FM, Blanchard MS, Reda DJ, Henderson WG, Toomey R, Jackson LW, Alpern R, Parks BJ, Klimas N, Hall C, Pak HS, Hunter J, Karlinsky J, Battistone MJ, Lyons MJ Gulf War Study Participating Investigators. Gulf War veterans’ health: medical evaluation of a US cohort. Ann Intern Med. 2005;142:881–890
Flor H, Fydrich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: a meta-analytic review. Pain. 1992;49:221–230
Golightly YM, Dominick KL. Racial variations in self-reported osteoarthritis symptom severity among veterans. Aging Clin Exp Res. 2005;17:264–269
Grossbard JR, Lehavot K, Hoerster KD, Jakupack M, Seal KH. Relationships among veteran status, gender, and key health indicators in a national young adult sample. Psychiatr Serv. 2013;64:547–553
Gunreben-Stempfle B, Griessinger N, Lang E, Muehlhans B, Sittl R, Ulrich K. Effectiveness of an intensive multidisciplinary headache treatment program. Headache. 2009;49:990–1000
Haldorsen EM, Grasdal AL, Skouen JS, Risa AE, Kronholm K, Ursin H. Is there a right treatment for a particular patient group? Comparison of ordinary treatment, light multidisciplinary treatment, and extensive multidisciplinary treatment for long-term sick-listed employees with musculoskeletal pain. Pain. 2002;95:49–63
Haskell SG, Ning Y, Krebs E, Goulet J, Mattocks K, Kerns R, Brandt C. Prevalence of painful musculoskeletal conditions in female and male veterans in 7 years after return from deployment in Operation Enduring Freedom/Operation Iraqi Freedom. Clin J Pain. 2012;28:163–167
Helmer DA, Chandler HK, Quigley KS, Blatt M, Teichman R, Lange G. Chronic widespread pain, mental health, and physical role function in OEF/OIF veterans. Pain Med. 2009;10:1174–1182
Hoerster KD, Lehavot K, Simpson T, McFall M, Reider G, Nelson KM. Health and health behavior differences: US military, veteran, and civilian men. Am J Prev Med. 2012;43:483–9
Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010;11:1230–1239
Kang HK, Mahan CM, Lee KY, Magee CA, Murphy FM. Illnesses among United States veterans of the Gulf War: a population-based survey of 30,000 veterans. J Occup Environ Med. 2000;42:491–501
Kazis LE, Miller DR, Clark J, Skinner K, Lee A, Rogers W, Spiro A, 3rd, Payne S, Fincke G, Selim A, Linzer M. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998;158:626–632
Kazis LE, Ren XS, Lee A, Skinner K, Rogers W, Clark J, Miller DR. Health status in VA patients: results from the Veterans Health Study. Am J Med Qual. 1999;14:28–38
Kramarow EA, Pastor PN. The health of male veterans and nonveterans aged 25–64: United States, 2007–2010. NCHS Data Brief. 2012;101:1–8
Lang E, Liebig K, Kastner S, Neundörfer B, Heuschmann P. Multidisciplinary rehabilitation versus usual care for chronic low back pain in the community: effects on quality of life. Spine J. 2003;3:270–276
Luncheon C, Zack M. Health-related quality of life among US veterans and civilians by race and ethnicity. Prev Chronic Dis. 2012;9:E108
Madans JH, Loeb M. Methods to improve international comparability of census and survey measures of disability. Disabil Rehabil. 2013;35:1070–1073
Madans JH, Loeb ME, Altman BM. Measuring disability and monitoring the UN Convention on the Rights of Persons with Disabilities: the work of the Washington Group on Disability Statistics. BMC Public Health. 2011;11(suppl 4):S4
Miller K, Loeb M. Mixed-method assessment of validity and cross-subgroup comparability. AAPOR 69th Annual Conference; Anaheim, CA. 2014. [Accessed September 27, 2016]. Available at: http://www.aapor.org/Conference-Events/Recent-Conferences.aspx. [Google Scholar]
Murgatroyd DF, Casey PP, Cameron ID, Harris IA. The effect of financial compensation on health outcomes following musculoskeletal injury: systematic review. PLoS One. 2015;10:e0117597
Murphy LB, Helmick CG, Allen KD, Theis KA, Baker NA, Murray GR, Qin J, Hootman JM, Brady TJ, Barbour KE Centers for Disease Control and Prevention. Arthritis among veterans - United States, 2011–2013. MMWR Morb Mortal Wkly Rep. 2014;63:999–1003
Murphy FM, Kang H, Dalager NA, Lee KY, Allen RE, Mather SH, Kizer KW. The health status of Gulf War veterans: lessons learned from the Department of Veterans Affairs Health Registry. Mil Med. 1999;164:327–331
Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16:769–780
Nahin RL. Categorizing the severity of pain using questions from the 2012 National Health Interview Survey. J Pain Res. 2016;9:105–113
National Center for Health Statistics. Data File Documentation, National Health Interview Survey, 2012. National Center for Health Statistics, Centers for Disease Control and Prevention; Hyattsville, Maryland: 2013. [Google Scholar]
Office of the Assistant Secretary for Health.
National Pain Strategy: A Comprehensive Population
Health-Level Strategy for Pain
Washington, DC: US Department of Health and Human Services,
National Institutes of Health; 2016.Patrick LE, Altmaier EM, Found EM. Long-term outcomes in multidisciplinary treatment of chronic low back pain: results of a 13-year follow-up. Spine (Phila Pa 1976) 2004;29:850–855
Portenoy RK, Ugarte C, Fuller I, Haas G. Population-based survey of pain in the United States: differences among white, African American, and Hispanic subjects. J Pain. 2004;5:317–328
Reyes-Gibby CC, Aday LA, Todd KH, Cleeland CS, Anderson KO. Pain in aging community-dwelling adults in the United States: non-Hispanic whites, non-Hispanic blacks, and Hispanics. J Pain. 2007;8:75–84
Riskowski JL. Associations of socioeconomic position and pain prevalence in the United States: findings from the National Health and Nutrition Examination Survey. Pain Med. 2014;15:1508–1521
Rogers WH, Kazis LE, Miller DR, Skinner KM, Clark JA, Spiro A, 3rd, Fincke RG. Comparing the health status of VA and non-VA ambulatory patients: the Veterans’ Health and Medical Outcomes Studies. J Ambul Care Manage. 2004;27:249–262
Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology (Oxford) 2008;47:670–678
Skouen JS, Grasdal AL, Haldorsen EM, Ursin H. Relative cost-effectiveness of extensive and light multidisciplinary treatment programs versus treatment as usual for patients with chronic low back pain on long-term sick leave: randomized controlled study. Spine (Phila Pa 1976) 2002;27:901–909
Steele L. Prevalence and patterns of Gulf War illness in Kansas veterans: association of symptoms with characteristics of person, place, and time of military service. Am J Epidemiol. 2000;152:992–1002
Stuart JA, Murray KM, Ursano RJ, Wright KM. The Department of Defense’s Persian Gulf War registry year 2000: an examination of veterans’ health status. Mil Med. 2002;167:121–128
Tsai J, Rosenheck R. Uninsured veterans who will need to obtain insurance coverage under the patient protection and affordable care act. Am J Public Health. 2014;104:e57–62
U.S. Census Bureau. [Accessed on May 26, 2016];2008–2010 American Community Survey. Available at:
http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.
xhtml?pid=ACS_13_3YR_S0201&prodType=tableVeterans Health Administration. [Accessed on May 6, 2016];Pain Management Strategy. Available at:
http://www.va.gov/PAINMANAGEMENT/VHA_Pain_Management_Strategy.asp[Accessed September 27, 2016];Washington Group on Disability Statistics. Available at:
http://www.cdc.gov/nchs/washington_group.htm
Return to SPINAL PAIN MANAGEMENT
Return NON-PHARMACOLOGIC THERAPY
Return to CHIROPRACTIC CARE FOR VETERANS
Since 2-09-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |