

Trends in Chiropractic Care and Physical Rehabilitation
Use Among Adults with Low Back Pain in
the United States, 2002 to 2018This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Gen Intern Med. 2023 (Oct 19); 39 (4): 578–586 ~ FULL TEXT
OPEN ACCESS Eric J Roseen • Kushang V Patel • Rachel Ward • Xinyao de Grauw
Steven J Atlas • Stephen Bartels • Julie J Keysor • Jonathan F Bean
Section of General Internal Medicine,
Department of Medicine, Boston University,
Chobanian & Avedision School of Medicine and
Boston Medical Center,
Boston, MA, USA.

Background While nonpharmacologic treatments are increasingly endorsed as first-line therapy for low back pain (LBP) in clinical practice guidelines, it is unclear if use of these treatments is increasing or equitable.
Objective Examine national trends in chiropractic care and physical rehabilitation (occupational/physical therapy (OT/PT)) use among adults with LBP.
Design/Setting Serial cross-sectional analysis of the National Health Interview Survey, 2002 to 2018.
Participants 146,087 adults reporting LBP in prior 3 months.
Methods We evaluated the association of survey year with chiropractic care or OT/PT use in prior 12 months. Logistic regression with multilevel linear splines was used to determine if chiropractic care or OT/PT use increased after the introduction of clinical guidelines. We also examined trends in use by age, sex, race, and ethnicity. When trends were similar over time, we present differences by these demographic characteristics as unadjusted ORs using data from all respondents.
Results Between 2002 and 2018, less than one-third of adults with LBP reported use of either chiropractic care or OT/PT. Rates did not change until 2016 when uptake increased with the introduction of clinical guidelines (2016–2018 vs 2002–2015, OR` =` 1.15; 95% CI: 1.10–1.19). Trends did not differ significantly by sex, race, or ethnicity (p for interactions` >` 0.05). Racial and ethnic disparities in chiropractic care or OT/PT use were identified and persisted over time. For example, compared to non-Hispanic adults, either chiropractic care or OT/PT use was lower among Hispanic adults (combined OR` =` 0.62, 95% CI: 0.65–0.73). By contrast, compared to White adults, Black adults had similar OT/PT use (OR` =` 0.98; 95% CI: 0.94–1.03) but lower for chiropractic care use (OR` =` 0.50; 95% CI: 0.47–0.53).
Conclusions Although use of chiropractic care or OT/PT for LBP increased after the introduction of clinical guidelines in 2016, only about a third of US adults with LBP reported using these services between 2016 and 2018 and disparities in use have not improved.
From the FULL TEXT Article:
INTRODUCTION
Low back pain (LBP) is a leading cause of disability and healthcare costs in the United States (US). [1, 2] Recommendations for the management of LBP have changed significantly over the last 20 years, increasingly recommending early use of nonpharmacologic treatments. For example, the American College of Physicians (ACP) guidelines for managing LBP endorsed nonpharmacologic treatments (e.g., massage, therapeutic exercise, spinal manipulation) as evidence-based second-line therapy in 2007 and then as first-line therapy in their current 2017 guideline. [3, 4] The ACP guidelines, as well as the 2016 CDC guidelines for opioid prescribing [5], if adopted, should have increased use of nonpharmacologic approaches for LBP over time. Moreover, the 2022 CDC guidelines for opioid prescribing continue to emphasize the importance of nonpharmacologic alternatives to opioids for pain management. [6] However, the extent of uptake of LBP treatment guidelines in the US is not known.
Chiropractic care, occupational therapy (OT), and physical therapy (PT) are widely available and typically involve one or more nonpharmacologic approaches that are recommended for chronic LBP (e.g., spinal manipulation, therapeutic exercise). [3, 4, 7–9] In a recent analysis of the Medical Expenditure Panel Survey (MEPS), which found that from 2011 to 2019 use of nonpharmacologic treatments increased for non-cancer chronic pain, chiropractic care and OT/PT were the most accessed nonpharmacologic approaches. [10] However, the MEPS sample [10] of adults with non-cancer chronic pain excluded adults with acute, subacute, or recurrent LBP for whom nonpharmacologic treatments are also recommended (e.g., massage, spinal manipulation). [7]
While the collective workforce of chiropractors, OTs, and PTs is large and trained to deliver evidence-based reimbursable nonpharmacologic treatments [11–13], it is unlikely this workforce can meet demand. [14] Prior studies suggest utilization varies by number of providers in a particular region or community [15–17] Cross-sectional studies from the 2012 and 2017 NHIS show Black and Hispanic adults are less likely than White adults to use chiropractic care and other complementary and integrative health approaches. [18, 19] These analyses did not include data on PT. Additional research is needed to understand whether access to nonpharmacologic treatments for LBP has become more equitable over time.
To address these knowledge gaps, we evaluated chiropractic and OT/PT utilization among adults reporting LBP from 2002 to 2018, in the yearly National Health Interview Survey (NHIS). We hypothesized that use of these approaches would increase over the 17-year period among adults with LBP, particularly following CDC and ACP guidelines in 2016 and 2017, respectively. [3, 4] We also examined differences in use by age, sex, race, and ethnicity and whether disparities changed over time.
METHODS
Study Design and Dataset
This is a serial cross-sectional analysis of the primary adult questionnaire of the annual NHIS, from 2002 to 2018, the most recent data on chiropractic care and OT/PT use. The NHIS survey is conducted each year by the CDC’s National Center for Health Statistics (NCHS), with data being collected from a nationally representative sample of the US population. We also used data from the Adult Complementary and Alternative Medicine (ACAM) supplement to NHIS, which estimates the prevalence and reasons for use of complementary and integrative therapies. The ACAM supplement began as part of the 2002 NHIS survey and occurs every 5 years. All data were downloaded from the Integrated Public Use Microdata Series (IPUMS), an online platform at the University of Minnesota that preserves and harmonizes publicly available data. [20]
Study Population
We included participants with recent LBP defined as a “yes” response to the following question which was asked each year: “Have you experienced low back pain in the last three months?” Additionally, participants with LBP were asked if pain “spread down either leg to areas below the knees” during the past 3 months. Participants who answered “yes” were classified as having back-related leg pain.
Exposure
Survey year was the primary exposure, i.e., 2002 to 2018.
Use of Nonpharmacologic Treatment
Our primary outcomes were use of nonpharmacologic treatments. The definition for “use” of chiropractic care was a yes response to the question, “Have you saw/talked to a chiropractor in the past 12 months?” Similarly, OT/PT “use” was defined as a “yes” response to the question, “Have you saw/talked to a physical therapist or occupational therapist in the past 12 months?” A composite outcome was created to identify participants who receive at least one of these, i.e., chiropractic or OT/PT use.
Sociodemographic Characteristics
The main subgroups of interest included age in years (18–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75` +), sex, race (White, Black, American Indian/Native Alaskan, Asian/Pacific Islander, Other), and ethnicity (Hispanic, non-Hispanic).
Additional characteristics were observed to aid interpretation of potential differences in nonpharmacologic treatment use by age, sex, race, or ethnicity.
These included the following:education (< high school, high school, some college, ≥college graduate),
income relative to poverty line (Below, 1–2 times, > 2 times, > 5 time poverty threshold),
U.S. Census region (Northeast, Midwest, South, and West),
Citizenship (U.S. Citizen, non-Citizen),
nativity (US Born, Born outside of US), and
health insurance status (no insurance, public health insurance only (Medicare, Medicaid, military insurance, Indian health services), private insurance only, and both public and private insurance).Statistical Analysis
Trends in Utilization
The proportion of adults with LBP who report chiropractic or OT/PT use was estimated for each year using population-based weights. Weighted proportions and their 95% confidence intervals (CIs) were plotted over time and visually inspected for trends. Multilevel logistic regression with a linear spline was used to determine if chiropractic care or OT/PT use increased after the introduction of clinical guidelines in 2016, adjusting for age and sex. [4, 5, 21] A knot at 2016 compares the slope of chiropractic or OT/PT use between 2002–2015 and 2016–2018. All analyses were weighted to account for survey nonresponse and the complex sampling design of the NHIS. Taylor series linearization was used for variance estimation.
Stratified Trends in Utilization
Use was plotted over time by age, sex, race, and ethnicity groups. Figures were visually inspected for trends. Differences in trends were formally evaluated by including an interaction term for survey year and each sociodemographic variable.
Estimates of Inequities in Utilization
When there was no interaction, weighted univariate logistic regression models and data from all respondents were used to estimate unadjusted odds ratios (ORs) and 95% CIs. Thus, estimates of disparities did not adjust for downstream socioeconomic factors thought to be the potential underlying mechanism of observed differences. [22, 23]Sensitivity Analyses
We evaluated additional questions on chiropractic use from the 2002, 2007, and 2012 ACAM supplement. First, participants were asked, “during the past 12 months, did you see a practitioner for chiropractic or osteopathic manipulation?” We compared estimates of self-reported chiropractic use from ACAM supplement to those from primary analysis.
Second, participants were asked, “For what health problems, symptoms, or conditions did you see a chiropractor?” We identified participants indicating use was for “back pain or problem” and compared findings to main results, i.e., proportion that use chiropractic for LBP vs adults with LBP reporting chiropractic use.
Lastly, some participants not currently using chiropractic care may have tried it in the past, i.e., they are aware of it as a treatment option. In 2002, participants were asked “Have you ever seen a provider or practitioner for any of the following for your own health?” and responded yes/no to each provider type listed including “chiropractor.” In 2007 and 2012, participants were asked, “Have you ever seen a provider or practitioner for any of the following therapies for yourself?” and reported yes/no to “chiropractic or osteopathic manipulation”. [24, 25]
Additional Subgroup Analyses
Back-related leg pain generally refers to sciatica or neurogenic claudication. The former is more common in individuals under 50 years of age and may be associated with a lumbar disc herniation. The latter is more common in older individuals and may be associated with lumbar spinal stenosis. While evidence suggests that nonpharmacologic treatments are effective for back-related leg pain [24, 25], national trends in use of these treatments for this subgroup remain unknown. Analyses described above were repeated among adults reporting back-related leg pain. We hypothesized that utilization would be higher as back-related leg pain has a worse prognosis. [26]
RESULTS

Table 1
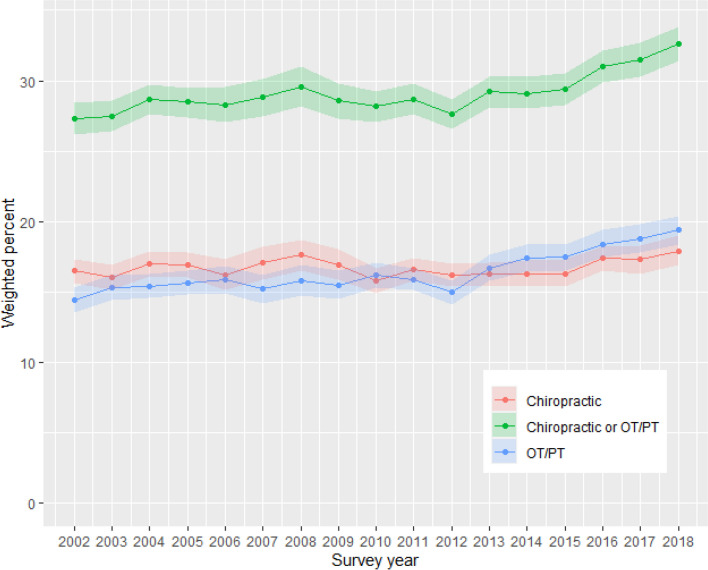
Figure 1

Table 2 From 2002 to 2018, we identified 146,087 adults who reported LBP in the prior 3 months including 52,644 who reported back-related leg pain (Supplementary Figure 1). Characteristics of participants with LBP are shown in Table 1 and those with back-related leg pain are described in Supplementary Table 2.
Trends in Utilization Among Adults with LBP
From 2002 to 2018, among adults with LBP, less than one-third of participants reported using either chiropractic care or OT/PT, and utilization of each individual therapy remained below 20% (Figure 1, Table 2). The logistic regression spline model showed that there was a statistically significant inflection in 2016, when CDC guidelines were introduced. To aid interpretation, the age- and sex-adjusted OR comparing chiropractic or PT/OT use in 2016–2018 vs 2002–2015 was 1.15 (95% CI: 1.10–1.19). When examined separately, the increase in use of PT/OT services (OR = 1.19, 95% CI: 1.14–1.24) was larger than the increase in use of chiropractic care (OR = 1.09, 95% CI: 1.04–1.15) after CDC and ACP guidelines were released.
Stratified Trends
Trends in chiropractic and OT/PT use stratified by age, sex, race, and ethnicity are shown in Supplementary Figs. 2a–d. Upon visual inspection of figures, differences by these sociodemographic groups generally remained consistent over time. Indeed, the logistic regression with linear spline models did not identify any effect modification by sex, race, or ethnicity (p for interactions > 0.05) in the use of chiropractic or OT/PT over time. However, there was statistically significant interaction by age. Younger adults had larger increases in use of chiropractic care or OT/PT services than older adults after the introduction of clinical guidelines (2016–2018 vs 2002–2015, OR in age 18–44 years = 1.19, 95% CI: 1.11–1.27; OR in age 45–64 years = 1.13, 95% CI: 1.07–1.20; and OR in age ? 65 years = 1.13, 95% CI: 1.05–1.20).
Use of Chiropractic Care or OT/PT by Age, Sex, Race, and Ethnicity
The prevalence of chiropractic or OT/PT use among all participants in various subgroups is shown in Table 2. Chiropractic use was least common among adults over age 75 and most common among adults aged 35 to 44 years (11.5% and 19.8%, respectively). By contrast, OT/PT use was most common among adults over age 75 and least common among those aged 18–24 years (23.4% vs 9.2%, respectively). Chiropractic use was similar among men and women and OT/PT use was slightly higher among women. Compared to White adults, chiropractic use was lower among Black, Native American, and Asian adults. Compared to White adults, OT/PT use was similar among Black and Native Americans but lower among Asian adults. Compared non-Hispanic adults, OT/PT use was lower in Hispanic adults.
Use of Chiropractic Care or OT/PT by Other Characteristics
While use of chiropractic care was lowest among those without a degree and those with an income below the poverty line, gaps in use by these characteristics were smaller for OT/PT use. Compared to private health insurance, use of chiropractic care was lower and OT/PT use was higher among adults with public insurance coverage. Access to chiropractic or OT/PT services was lowest for individuals without health insurance.
Sensitivity Analyses

Table 3 Estimates of chiropractic use in the past year were slightly lower in ACAM supplement than base NHIS survey (e.g., 14.6% vs 16.2% in 2012) (Table 3). The proportion of adults with LBP who reported chiropractic use for LBP ranged from 71% in 2002 to 49% in 2012. Roughly a third of adults with LBP reported ever seeing a chiropractor in the past in 2002, 2007, and 2012.
Additional Subgroup Analyses
Results were similar among adults with back-related leg pain (Appendix Table 2) although use of chiropractic care or OT/PT tended to be higher, e.g., up to 37.5% use of either approach in 2018.
DISCUSSION
Our study found that approximately one-third of adults who had LBP in the prior 3 months reported seeing either a chiropractor or OT/PT in the prior year. Use of both increased after CDC (2016) and ACP (2017) guidelines were released, with larger increases seen for OT/PT than chiropractic care. Racial and ethnic disparities in care identified over the entire study period did not improve. Chiropractic or OT/PT use was less likely among Hispanic versus non-Hispanic adults with LBP. Black Americans were as likely as White Americans to access OT/PT but half as likely to access chiropractic care. Similarly, while access to OT/PT was generally similar among Americans with various incomes and insurance providers, chiropractic use was low among low-income adults and those with public health insurance.
Our findings of increased use of nonpharmacologic treatments are consistent with a recent analysis of the MEPS from 2011 to 2019, where nonpharmacologic treatments use for non-cancer chronic pain increased from 2016 to 2019. [10] However, our findings suggest higher utilization of chiropractic and OT/PT use among adults with LBP than the MEPS study did for chronic non-cancer pain. [10] This might be explained by our inclusion of adults with acute/subacute LBP where chiropractic and OT/PT use is common or absence of participants with other chronic pain conditions where chiropractic or OT/PT care is rare, e.g., abdominal pain. We also observed a more modest increase in use of chiropractic and OT/PT care among adults with LBP than the MEPS study did for non-cancer chronic pain. We do not know if slower increases in chiropractic or OT/PT care among adults with LBP suggest a more rapid uptake for other pain condition such as neck pain, osteoarthritis, or fibromyalgia.
One might anticipate higher use of nonpharmacologic treatments among older adults [27, 28], particularly older women [29], due to increased prevalence. Use of OT/PT was highest in older adults, and slightly higher among women. By contrast, chiropractic care was less common among older adults than among middle-aged or younger adults. Older adults, or their providers [30], may hold concerns that adverse events are common with chiropractic care, despite main components of chiropractic care (e.g., joint manipulation/mobilization, therapeutic exercise) also being frequently delivered in OT/PT care. [7, 8] These concerns/beliefs may be addressed through dissemination on safety and effectiveness of chiropractic care for LBP from clinical trials that enrolled older adults. [31-33] Dissemination of practice guidelines specific to older adults, which endorse nonpharmacologic approaches, may also be needed. [24, 34]
Less chiropractic care among minority racial/ethnic groups is consistent with prior cross-sectional analyses of the 2012 and 2017 NHIS ACAM supplement. [18, 19] While inequities in OT/PT use were observed, they tended to be smaller, and there was no difference in OT/PT use between Black and White adults. Disparities in access to first-line treatment may contribute to observed disparities in health outcomes among adults with LBP. [23] Racial and ethnic disparities may relate to differences in other downstream factors. We found that income and insurance type were generally not associated with OT/PT use, except for adults without health insurance, where use was much lower. By contrast, chiropractic care was strongly associated with all measures of income and health insurance, with lowest access among adults with public health insurance, adults with no health insurance, and low-income adults. Differences in chiropractic and OT/PT access by insurance type could relate to actual or perceived variations in insurance coverage. [11, 35] A recent study of 45 US-based public/private healthcare plans found that PT, OT, and chiropractic care were covered for LBP in most plans (98%, 96%, and 89% of plans, respectively). [11] Recent expansion of Medicaid in Oregon increased utilization of chiropractic care and other nonpharmacologic treatments in the state. [36] Expanding coverage, promoting coverage, and/or reducing cost-sharing (co-payments, deductible costs) may further expand use.
The clinical implications of our study hinge on the optimal rate at which patients with LBP should pursue chiropractic or OT/PT care. Two-thirds of adults with LBP do not report receiving chiropractic care or OT/PT. Adults with mild LBP that does not limit physical function may self-manage and not seek healthcare, particularly if they follow guidance to stay active and avoid bedrest. [3, 4] However, some would benefit from first-line nonpharmacologic treatment, e.g., adults with chronic, severe, or activity-limiting pain, or those who are actively seeking healthcare. While primary care providers ought to describe and recommend nonpharmacologic treatments to patients who are seeking treatment for LBP, prescribing a pain medication may be a more familiar or preferred practice. [37-39] Implementation efforts to expand access to nonpharmacologic treatments should consider the even lower rates of use among racial and ethnic minorities.
Our study has several limitations. First, we treated OT/PT as a single category based on a single question in NHIS asking about OT and PT use. While this limits our ability to understand access to these unique types of providers, the prior study by Pritchard et al. was able to separate the two therapies in some years of MEPS, with the majority of OT/PT use being PT use. [10] Second, while ACP/CDC guidelines recommend specific treatments for LBP (e.g., spinal manipulation, therapeutic exercise), we cannot be sure that patients who have been seen by a chiropractor and OT/PT received these treatments. Third, we evaluated the use of chiropractic and OT/PT among Americans with LBP rather than use of chiropractic or OT/PT explicitly for LBP. Sensitivity analysis suggested that this resulted in a modest overestimate of the use of chiropractic care, i.e., the true use for LBP would be even lower. Fourth, we assessed chiropractic or OT/PT use in the past 12 months among patients who report LBP in the previous 3 months (rather than LBP in the previous 12 months). We do not know if participants who have had LBP in the past year but not the past 3 months would be more or less likely to report chiropractic or OT/PT use. Our assumption that presence of LBP preceded treatment would not hold in some cases, e.g., if an adult develops low back pain after seeking care for another health condition. In this potential scenario, we would also expect that the true estimate of nonpharmacologic treatment use for LBP is even lower than what we report here.
CONCLUSIONS
Although use of chiropractic care or OT/PT for LBP increased after the introduction of clinical guidelines in 2016, only about a third of US adults with LBP reported using these services between 2016 and 2018. Racial and ethnic disparities in care identified did not improve over the study period. Future implementation should target sociodemographic groups with the lowest access to nonpharmacologic treatments to achieve equitable access.
Supplementary Material
Supplementary File 1
Trends in chiropractic care and physical rehabilitation use among adults with low back pain or back-related leg pain in the United States, 2002 to 2018
Supplemental Tables and Figures (294.3KB, docx)Author Contribution
Authors Roseen and deGrauw had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Roseen, Patel, Ward, Bartels, Keysor, and Bean.
Acquisition, analysis, or interpretation of data: Roseen, Patel, Ward, deGrauw, Bartels, Keysor, and Bean.
Critical revision of the manuscript for important intellectual content: Roseen, Patel, Ward, Bartels, Keysor, and Bean.
Statistical analysis: Roseen, Patel, deGrauw, and Ward.
Obtained funding: n/a.
Administrative, technical, or material support: Roseen.
Study supervision: Roseen, Patel, and Bean.
Funding
This work was supported in part by the National Institutes of Health (NIH) under award numbers K23 AT010487-04 and K24 AG069176-06.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Role of the Funder/Sponsor
The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of NIH, the Department of Veterans Affairs, or the United States Government.
References:
Dieleman JL, Cao J, Chapin A, et al.
US Health Care Spending by Payer and Health Condition, 1996-2016
JAMA 2020 (Mar 3); 323 (9): 863–884.Disease Injury, Incidence Prevalence, Collaborators.
Global, regional, and national incidence, prevalence, and years lived
with disability for 310 diseases and injuries, 1990–2015:
a systematic analysis for the Global Burden
of Disease Study 2015.
Lancet. 2016;388(10053):1545–1602.
doi: 10.1016/S0140-6736(16)31678-6.Chou R, Qaseem A, Snow V, et al.
Diagnosis and Treatment of Low Back Pain: A Joint Clinical
Practice Guideline from the American College of Physicians
and the American Pain Society
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 478–491Qaseem A, Wilt TJ, McLean RM, et al.
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Dowell D, Haegerich TM, Chou R.
CDC Guideline for Prescribing Opioids for Chronic Pain-
United States, 2016.
JAMA. 2016;315(15):1624–1645.
doi: 10.1001/jama.2016.1464.Dowell D, Ragan KR, Jones CM, et al.
CDC Clinical Practice Guideline for Prescribing Opioids
for Pain - United States, 2022.
MMWR Recomm Rep. 2022;71(3):1–95.
doi: 10.15585/mmwr.rr7103a1.Beliveau PJH, Wong JJ, Sutton DA, et al.
The Chiropractic Profession: A Scoping Review of Utilization Rates,
Reasons for Seeking Care, Patient Profiles, and Care Provided
Chiropractic & Manual Therapies 2017 (Nov 22); 25: 35George SZ, Fritz JM, Silfies SP, et al.
Interventions for the Management of Acute and Chronic
Low Back Pain: Revision 2021.
J Orthop Sports Phys Ther. 2021;51(11):CPG1–CPG60.
doi: 10.2519/jospt.2021.0304.Goertz CM, Long CR, Vining RD, et al.
Effect of Usual Medical Care Plus Chiropractic Care
vs Usual Medical Care Alone on Pain and Disability
Among US Service Members With Low Back Pain
JAMA Network Open. 2018 (May 18); 1 (1): e180105Pritchard KT, Baillargeon J, Lee WC, et al.
Trends in the Use of Opioids vs Nonpharmacologic Treatments in Adults With Pain, 2011–2019.
JAMA Netw Open. 2022;5(11):e2240612.
doi: 10.1001/jamanetworkopen.2022.40612.Heyward J, Jones CM, Compton WM, et al. Trends in the Use of Opioids vs Nonpharmacologic Coverage of Nonpharmacologic Treatments for Low Back Pain Among US Public and Private Insurers. Trends in the Use of Opioids vs Nonpharmacologic JAMA Network Open. 2018;1(6)
doi:10.1001/jamanetworkopen.2018.3044.Stochkendahl MJ, Rezai M, Torres P, et al.
The chiropractic workforce: a global review.
Chiropr Man Therap. 2019;27(36),
doi:10.1186/s12998-019-0255-x.Davis MA, Mackenzie TA, Coulter ID, et al.
The United States Chiropractic Workforce:
An Alternative or Complement to Primary Care?
Chiropractic & Manual Therapies 2012 (Nov 21); 20: 35Jesus TS, Landry MD, Brooks D, et al.
Physical Rehabilitation Needs per Condition Type:
Results from the Global Burden of Disease study 2017
Archives of Physical Medicine and Rehabilitation 2020 (Feb 5)Davis MA, Yakusheva O, Gottlieb DJ, et al.
Regional Supply of Chiropractic Care and Visits to
Primary Care Physicians for Back and Neck Pain
J American Board of Family Medicine 2015 (Jul); 28 (4): 481–490Whedon JM, Haldeman S, Petersen CL, et al.
Temporal Trends and Geographic Variations in the Supply
of Clinicians Who Provide Spinal Manipulation to
Medicare Beneficiaries: A Serial Cross-Sectional Study
J Manipulative Physiol Ther 2021 (Mar); 44 (3): 177–185Whedon JM, Song Y, Davis MA, et al.
Use of Chiropractic Spinal Manipulation in Older Adults
is Strongly Correlated with Supply
Spine (Phila Pa 1976). 2012 (Sep 15); 37 (20): 1771–1777Adams J, Peng W, Cramer H, et al.
The Prevalence, Patterns, and Predictors of
Chiropractic Use Among US Adults: Results
From the 2012 National Health Interview Survey
Spine (Phila Pa 1976) 2017 (Dec 1); 42 (23): 1810–1816Ghildayal N, Johnson PJ, Evans RL, et al.
Complementary and Alternative Medicine Use in the
US Adult Low Back Pain Population.
Glob Adv Health Med. 2016;5(1):69–78.
doi: 10.7453/gahmj.2015.104.Lynn A. Blewett, Julia A. Rivera Drew, Miriam L. King, Kari C.W. Williams.
IPUMS Health Surveys: National Health Interview Survey,
Version 7.2 . Minneapolis, MN: IPUMS, 2022.
10.18128/D070.V7.2.Tilling K, Macdonald-Wallis C, Lawlor DA, et al.
Modelling childhood growth using fractional
polynomials and linear splines.
Ann Nutr Metab. 2014;65(2–3):129–138.
doi: 10.1159/000362695.Jackson JW.
Meaningful Causal Decompositions in Health Equity Research:
Definition, Identification, and Estimation
Through a Weighting Framework.
Epidemiology. 2021;32(2):282–290.
doi: 10.1097/EDE.0000000000001319.Roseen EJ, Smith CN, Essien UR, et al.
Racial and ethnic disparities in the incidence of high-impact chronic
pain among primary care patients with acute low back pain: A cohort study.
Pain Med. 2022
doi: 10.1093/pm/pnac193.Bussieres A, Cancelliere C, Ammendolia C, et al.
Non-Surgical Interventions for Lumbar Spinal Stenosis Leading
To Neurogenic Claudication: A Clinical Practice Guideline
J Pain 2021 (Sep); 22 (9): 1015–1039Bronfort G, Hondras MA, Schulz CA, et al.
Spinal Manipulation and Home Exercise with Advice
for Subacute and Chronic Back-related Leg Pain:
A Trial With Adaptive Allocation
Annals of Internal Medicine 2014 (Sep 16); 161 (6): 381—391Chou R, Shekelle P.
Will this patient develop persistent disabling low back pain?
JAMA. 2010;303(13):1295–1302.
doi: 10.1001/jama.2010.344.Patel KV, Guralnik JM, Dansie EJ, et al.
Prevalence and impact of pain among older adults in the United States:
findings from the 2011 National Health and Aging Trends Study.
Pain. 2013;154(12):2649–2657.
doi: 10.1016/j.pain.2013.07.029.Di Iorio A, Abate M, Guralnik JM, et al.
From chronic low back pain to disability, a multifactorial
mediated pathway: the InCHIANTI study.
Spine (Phila Pa 1976) 2007;32(26):E809–15.
doi: 10.1097/BRS.0b013e31815cd422.Makris UE, Fraenkel L, Han L, et al.
Epidemiology of restricting back pain in
community-living older persons.
J Am Geriatr Soc. 2011;59(4):610–614.
doi: 10.1111/j.1532-5415.2011.03329.x.Busse JW, Pallapothu S, Vinh B, et al.
Attitudes Towards Chiropractic: A Repeated Cross-sectional
Survey of Canadian Family Physician
BMC Family Practice 2021 (Sep 15); 22 (1): 188Ammendolia C, Cote P, Southerst D, et al.
Comprehensive Nonsurgical Treatment Versus Self-directed Care to Improve
Walking Ability in Lumbar Spinal Stenosis: A Randomized Trial.
Arch Phys Med Rehabil. 2018;99(12):2408–2419 e2.
doi: 10.1016/j.apmr.2018.05.014.Schneider MJ, Ammendolia C, Murphy DR, et al.
Comparative Clinical Effectiveness of Nonsurgical Treatment Methods
in Patients With Lumbar Spinal Stenosis: A Randomized Clinical Trial
JAMA Netw Open 2019 (Jan 4); 2 (1): e186828Hawk C, Schneider MJ, Haas M, et al.
Best Practices for Chiropractic Care for Older Adults:
A Systematic Review and Consensus Update
J Manipulative Physiol Ther 2017 (May); 40 (4): 217–229Weiner DK, Marcum Z, Rodriguez E.
Deconstructing Chronic Low Back Pain in Older Adults:
Summary Recommendations.
Pain Med. 2016;17(12):2238–2246.
doi: 10.1093/pm/pnw267.Cherkin DC, Deyo RA, Goldberg H.
Time to Align Coverage with Evidence for Treatment of Back Pain
J General Internal Medicine 2019 (Sep); 34 (9): 1910–1912Choo EK, Charlesworth CJ, Gu Y, et al.
Increased Use of Complementary and Alternative Therapies for Back Pain
Following Statewide Medicaid Coverage Changes in Oregon.
J Gen Intern Med. 2021;36(3):676–682.
doi: 10.1007/s11606-020-06352-6.Roseen EJ, Conyers FG, Atlas SJ, et al.
Initial Management of Acute and Chronic Low Back Pain:
Responses from Brief Interviews of Primary Care Providers
J Altern Complement Med 2021 (Mar); 27 (S1): S106–S114Stevans JM, Delitto A, Khoja SS, et al.
Risk Risk Factors Associated With Transition From Acute
to Chronic Low Back Pain in US
Patients Seeking Primary Care
JAMA Network Open 2021 (Feb 1); 4 (2): e2037371Kamper SJ, Logan G, Copsey B, et al.
What is Usual Care for Low Back Pain? A Systematic Review
of Health Care Provided to Patients with Low Back Pain
in Family Practice and Emergency Departments
Pain. 2020 (Apr); 161 (4): 694–702
Return to LOW BACK PAIN
Since 4-15-2025


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |