U.S. Physician Recommendations to Their Patients
About the Use of Complementary Health ApproachesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Altern Complement Med 2020 (Jan); 26 (1): 25-33 ~ FULL TEXT
OPEN ACCESS Barbara J. Stussman, BA, Richard R. Nahin, PhD, MPH, Patricia M. Barnes, MA, and Brian W. Ward, PhD
National Center for Complementary and Integrative Health (NCCIH),
National Institutes of Health,
Bethesda, Maryland.
FROM: National Health Statistics Report 2015Objective: There are no nationally representative studies using a probability sample that have been published examining whether physicians recommend complementary health approaches (CHAs) to their patients, as previous research has focused only on selected medical specialties or a particular U.S. region. This article fills a void in the current literature for robust data on recommendations for CHAs by office-based physicians in the United States.
Design: Descriptive statistics and multivariable regression analyses of physician-level data were from the 2012 Physician Induction Interview of the National Ambulatory Medical Care Survey (NAMCS PII), a nationally representative survey of office-based physicians. Weighted response rate among eligible physicians sampled for the 2012 NAMCS PII was 59.7%.
Setting/Location: United States.
Outcome measures: Recommendations by physicians to their patients for any CHA, and individual CHAs: massage therapy, herbs/nonvitamin supplements, chiropractic/osteopathic manipulation, yoga, acupuncture, and mind–body therapies. Differences in recommendations by physician demographic characteristics were identified.
Results: Massage therapy was the most commonly recommended CHA (30.4%), followed by chiropractic/osteopathic manipulation (27.1%), herbs/nonvitamin supplements (26.5%), yoga (25.6%), and acupuncture (22.4%). The most commonly recommended CHAs by general/family practice physicians were chiropractic/osteopathic manipulation (54.0%) and massage therapy (52.6%). Of all U.S. physicians, 53.1% recommended at least one CHA to patients during the previous 12 months. Multivariable analyses found physician's sex, race, specialty, and U.S. region to be significant predictors of CHA recommendations. Female physicians were more likely than male physicians to recommend massage therapy (adjusted odds ratio [aOR] = 1.76, 95% confidence interval [CI] = 1.40–2.20), herbs/nonvitamin supplements (aOR = 1.85, 95% CI = 1.46–2.35), yoga (aOR = 2.16, 95% CI = 1.70–2.75), acupuncture (aOR = 1.65, 95% CI = 1.27–2.13), and mind–body therapies (aOR = 2.63, 95% CI = 2.02–3.41) to patients. Psychiatrists (aOR = 0.13, 95% CI = 0.07–0.23), OB/GYNs (aOR = 0.38, 95% CI = 0.24–0.60), and pediatricians (aOR = 0.26, 95% CI = 0.18–0.38) were all less likely to recommend chiropractic/osteopathic manipulation than general and family practitioners.
Conclusions: Overall, more than half of office-based physicians recommended at least one CHA to their patients. Female physicians recommended every individual CHA at a higher rate than male physicians except for chiropractic and osteopathic manipulation. These findings may enable consumers, physicians, and medical schools to better understand potential differences in use of CHAs with patients.
Keywords: complementary health, U.S. physicians, National Ambulatory Medical Care Survey, chiropractic, yoga, massage therapy, nondietary supplements
From the FULL TEXT Article:
Introduction
Complementary and integrative health practices, interventions, and natural products include mind–body interventions such as massage therapy, acupuncture, and yoga, and natural products such as fish oil or probiotics, [1] and are widely used by U.S. adults. [2, 3] Despite data on use of complementary health approaches (CHAs) by adults, [3–6] there are no nationally representative data using a probability sample collected on the recommendations for CHAs by U.S. office-based physicians.
Studies in this area have been limited to certain medical specialties (e.g., rheumatology, pediatrics, and family practice), [7–14] U.S. regions, [15–17] or types of CHAs (e.g., mind–body therapies and chiropractic). [8, 18, 19]
These have found recommendation rates by physicians for different CHAs were relatively high. For example, a national survey of rheumatologists found a majority were likely to recommend body work (65%), meditation (64%), and acupuncture (54%) for chronic lower back and joint pain, [7] 67% of pediatricians in a Seattle hospital reported recommending CHAs to patients, [15] more than half of physicians in the Chesapeake area referred patients to practitioners of biofeedback and chiropractic, [20] and 25% of physicians from the Hawaii Medical Service Association had/would refer patients for CHAs. [16]
Previous adult population data have shown use of CHAs is more prevalent among women than men. [3–6] This study examines whether similar differences by sex also occur between female and male physicians in their CHA recommendations. A handful of previous studies have examined sex differences in recommendations/referrals for specific CHAs by U.S. physicians of certain medical specialties. [7, 9] For example, a 2007 national survey of rheumatologists found (after controlling for other factors) female physicians were more willing to recommend CHAs to manage chronic back and joint pain. [7]
However, lacking are studies presenting national data across office-based medical specialties showing physicians' recommendations for multiple CHAs, and how these vary by physician's characteristics. Data from the Physician Induction Interview of the National Ambulatory Medical Care Survey (NAMCS) were used, which is representative of U.S. office-based physicians, to examine recommendations for CHAs by selected physician characteristics, including medical specialty and sex.
The aim of this study is to fill an existing void in the current literature for robust data on recommendations for CHAs by office-based physicians in the United States. Specifically, the authors identify which CHAs physicians recommend most often, and whether differences exist across physicians' medical specialty, sex, and other demographic characteristics.
Materials and Methods
Data
The 2012 NAMCS Physician Induction Interview (NAMCS PII) data were used, which was approved by the National Center for Health Statistics (NCHS) Ethics Review Board (Protocol #2010-02). NAMCS PII is conducted annually, and is representative of nonfederal office-based physicians in the United States (i.e., 50 states and the District of Columbia). This interview consists of questions that screen for survey eligibility of the physician and collect data on physician/practice characteristics. It precedes the portion of NAMCS that collects patient visit data. The 2012 NAMCS PII data are available from the NCHS Research Data Center.
Verbal consent was received from all physician participants. Weighted response rate among eligible physicians sampled for the 2012 NAMCS PII was 59.7%. [21, 22] The 2012 NAMCS PII data are unique, as only during this year were the National Center for Complementary and Integrative Health-funded supplemental survey questions on physician recommendations of CHA asked.
Measures
For the “any CHA” category, a “yes” response to the question was included, “During the past 12 months, did you recommend any of the following therapies or practices to your patients?” Therapies asked included massage therapy, herbs/other nonvitamin supplements, chiropractic/osteopathic manipulation, yoga, acupuncture, mind–body therapies (i.e., guided imagery, meditation, and progressive muscle relaxation, not including prayer), naturopathic treatment, biofeedback/hypnosis, and homeopathic treatment.
Based on the literature, demographic characteristics included in the analysis were physician age, sex, race, and medical specialty (general/family practice, internal medicine, psychiatry, obstetrics/gynecology, pediatrics, and all other specialties combined), type of physician (doctor of medicine [MD] or doctor of osteopathic medicine [DO]), medical school location (United States or foreign), metropolitan statistical area (MSA)/non-MSA, and U.S. Census region (Northeast, Midwest, South, and West). [7–11, 15, 23, 24] Ethnicity was not included as there were not enough Hispanic respondents to produce reliable statistics.
Because several therapies had small cell sizes prohibiting subgroup analyses, the majority of analyses were restricted to the six most prevalent individual therapies (i.e., massage therapy, herbs/nonvitamin supplements, chiropractic/osteopathic manipulation, yoga, acupuncture, and mind–body therapies), but included all nine in the “any CHA” category. To avoid small cell sizes and present statistically reliable estimates, physician's age was collapsed into 4 categories (<45, 45–54, 55–64, and ≥65 years), race into 3 categories (white, Asian, and other), and 12 physician specialties (general surgery, orthopedic surgery, cardiovascular diseases, dermatology, urology, neurology, ophthalmology, otolaryngology, oncologists, allergists, pulmonologist, and other specialties) into 1 “other specialty” category.
Statistical analysis
Characteristics of U.S. physicians in the analyses were provided. Bivariate analyses examined relationships between physician characteristics and recommendations for individual CHAs. Wald Chi-square or Breslow–Day tests were used to test for significant differences. Finally, seven individual multivariable logistic regression analyses were performed to identify associations among medical specialty, physician's sex, and other demographic characteristics, and recommendations for CHAs. Variables in the regression included age, race, specialty, physician type, medical school location, MSA status, and Census region. Analyses were conducted using SUDAAN 11.0, weighted to be representative of U.S. physicians in office-based settings, and used survey design variables and proper subsetting to account for covariance resulting from NAMCS complex cluster design. Percentages are accompanied by Korn–Graubard 95% confidence intervals (CIs), which are recommended for complex surveys, and meet NCHS standards. [25]
Results
Physician characteristics

Table 1 There were 5,622 physicians who provided data for these analyses, representing 338,627 physicians in the United States. Among nonfederal office-based U.S. physicians, 72.3% were male and 27.7% were female (Table 1). Excluding the “other” category, the most commonly observed specialty for male physicians was general/family practice (16.0%), followed by internal medicine (13.0%). For female physicians it was general/family practice (20.0%) and pediatrics (19.7%). The majority of physicians (94.1%) were MDs and three-quarters (75.2%) attended U.S. medical schools. Most physicians (92.7%) practiced in MSAs. Approximately 35.2% practice in the South, 24.4% in the West, 21.5% in the Northeast and 18.9% in the Midwest.
Bivariate analyses

Figure 1

Figure 2 Figure 1 and Supplementary Table S1 show the percentage of physicians who recommended any CHA, and each of the nine individual CHAs, to patients during the previous 12 months. Overall, 53.1% of physicians recommended a CHA to patients. Massage therapy was the most commonly observed recommended CHA (30.4%), followed by chiropractic/osteopathic manipulation (27.1%), herbs/nonvitamin supplements (26.5%), yoga (25.6%), and acupuncture (22.4%) (p = 0.0000). Looking at recommendations by sex, female physicians recommended at least one CHA to patients during the previous 12 months more often than male physicians (63.2% vs. 49.3%, p = 0.0000). Female physicians also recommended each CHA more often than male physicians except for chiropractic/osteopathic manipulation (41.2 vs. 26.4% for massage therapy, p = 0.0000; 37.0% vs. 22.7% for herbs/nonvitamin supplements, p = 0.0000; 38.6% vs. 20.8 for yoga, p = 0.0000; 29.5% vs. 19.7% for acupuncture, p = 0.0000; 34.0% vs. 15.7% for mind–body therapies, p = 0.0000; 23.0% vs. 12.6% for biofeedback or hypnosis, p = 0.0000; 19.44% vs. 10.1% for homeopathic treatment, p = 0.0000; and 16.3% vs. 8.2% for naturopathic treatment, p = 0.0000).
Figure 2 and Supplementary Table S2 show recommendations of any CHA and the six overall most prevalent individual CHAs by specialty. The most commonly observed CHAs recommended by general/family practice physicians were chiropractic/osteopathic manipulation (54.0%) and massage therapy (52.6%), while the least observed was mind–body therapies (27.8%, p = 0.0000). In contrast, psychiatrists recommended mind–body therapies the most, with over half recommending their use (53.1%, p = 0.0000). Pediatricians recommended herbs/other nonvitamin supplements most (27.2%) and acupuncture least (13.1%) (p = 0.0000).
Multivariable logistic regression

Table 2 A

Table 2 B Logistic regression found physician's age, sex, specialty, type, medical school location, MSA status, and region all significantly associated with CHA recommendations (Table 2). Female physicians had higher odds of having recommended any CHA (adjusted odds ratio [aOR] = 1.56, 95% CI = 1.25–1.95), massage therapy (aOR = 1.76, 95% CI = 1.40–2.20), herbs/other nonvitamin supplements (aOR = 1.85, 95% CI = 1.46–2.35), yoga (aOR = 2.16, 95% CI = 1.70–2.75), acupuncture (aOR = 1.65, 95% CI = 1.27–2.13), and mind–body therapies (aOR = 2.63, CI = 2.02–3.41) than male physicians. Age had little effect, with two exceptions: physicians ≥65 years were less likely than physicians <45 years to refer patients to yoga (aOR = 0.64, 95% CI = 0.43–0.94) or massage therapy (aOR = 0.65, 95% CI = 0.46–0.92). A number of specialties had lower odds of having recommended any CHA and individual CHAs than general/family practitioners. For example, pediatricians had lower odds than general/family practitioners in recommending each individual CHA (ranging from acupuncture [aOR = 0.22, 95% CI = 0.14–0.37] to herbal/nonvitamin supplements [aOR = 0.51, 95% CI = 0.35–0.75]). The same trend was also found for obstetrics/gynecology, psychiatry, and other specialties for the following CHAs: massage therapy, chiropractic/osteopathic manipulation, herbal/nonvitamin supplements, and acupuncture.
DOs had higher odds of having recommended any CHA (aOR = 1.78, 95% CI = 1.25–2.54), massage therapy (aOR = 1.57, 95% CI = 1.09–2.26), and chiropractic/osteopathic manipulation (aOR = 3.13, 95% CI = 2.18–4.49) than MDs, even after controlling for physician characteristics including specialty. Physicians practicing in the West had higher odds of having recommended all individual CHAs as well as any CHA than physicians in other regions, with the exception of physicians in the Northeast for recommendation of chiropractic/osteopathic manipulation. Supplementary Table S3 presents sex-stratified bivariate comparisons of physician recommendations of CHAs by physician characteristics.
Discussion
This study sought to fill an existing void in the literature for recommendations for CHAs by office-based physicians, and to explore whether differences exist across certain specialties and other physician demographic characteristics. The data show that 53.1% of U.S. physicians recommended any CHA to patients during the previous 12 months, and female physicians recommended every individual CHA at a higher rate than male physicians, except chiropractic/osteopathic manipulation. General/family practitioners were more likely to have recommended any CHA and individual CHAs than several physician specialties; pediatricians were less likely. Looking at recommendations by specialty, it was found that general/family practitioners recommended chiropractic/osteopathic manipulation and massage therapy at a higher rate than acupuncture, yoga, or mind–body therapies. Psychiatrists recommended mind–body therapies more frequently than any other CHAs, and pediatricians most frequently recommended herbs and nonvitamin supplements.
Previous studies examined U.S. physicians' recommending CHAs to patients, [15, 17] or referring patients to CHA providers, [14, 16, 20] using CHAs in their practices, [16] and willingness/intent to recommend/refer patients to CHAs. [7–11] However, all but Berman et al. [14] were specific to one U.S. region, one CHA, and/or one to two medical specialties. Berman et al. [14] mailed surveys to a sample of physicians from the 1994 American Medical Association membership list about using 19 different CHAs in their practice. In both Berman et al. and this study, physicians had higher recommendation (current study) or usage [14] rates for massage therapy than chiropractic, acupuncture, or herbal supplements (30.4% recommendation rate in this study; 33.7% usage rate in Berman et al.). This study found herbs/nonvitamin supplements were recommended as often as chiropractic/osteopathic manipulation (26.5% vs. 27.1%, respectively), whereas Berman et al. found herbs were used twice as often as chiropractic (19.2% vs. 8.2%, respectively). This difference could be due to Berman et al. using a more restrictive definition of the approach (“herbal medicine” vs. “herbs/other nonvitiamin supplements” in this study).
Current findings expand on scarce research on physician recommendations for CHAs, which mainly focus on rheumatologists. A 2007 survey [7] mailed to a sample of rheumatologists found body work, such as massage therapy, had the highest perceived benefit among rheumatologists (65% were “very/somewhat likely” to recommend it). Another national study [13] of physician members of the American College of Rheumatology found 50% had referred patients for acupuncture, biofeedback, dietary supplements, and massage therapy, consistent with current findings that massage therapy, herbs/nonvitamin supplements, and acupuncture were among the top five most commonly recommended CHAs. Another observation seen when comparing previous national studies with current findings is the high use of acupuncture by rheumatologists. Two previous studies found rheumatologists prefer acupuncture over chiropractic manipulation when recommending treatment for their patients, [10, 15] whereas this study found chiropractic/osteopathic manipulation was recommended more than acupuncture by physicians overall, and CHA usage data show chiropractic manipulation is used more than acupuncture by the public. [3] Recent evidence-based guidelines and review articles showing benefit of acupuncture for pain management may be impacting physician recommendations. [26, 27]
This study was more comprehensive than previous national studies in that it examined recommendations by several medical specialties. That general/family practitioners recommend chiropractic/osteopathic manipulation most frequently could be related to high rates of health insurance coverage for this approach in the general population [28] and in the Medicare population, [29] and/or to primary care physicians' high use of and referral rates for complementary approaches for patients with relatively stable chronic musculoskeletal problems such as back pain, headache, or pain management. [9] The high rate of recommendations for mind–body therapies by psychiatrists may be due to findings in previous research that confirms benefit of relaxation techniques, mediation, and mindfulness-based stress reduction for psychological conditions such as post-traumatic stress disorder, anxiety, and depression. [30, 31] In addition, that pediatricians recommend herbs and nonvitamin supplements most commonly may be explained by the relatively high use of fish oil, melatonin, probiotics, and echinacea in children. [32] Future research should explore reasons for varying recommendation rates across medical specialties.
National surveys have also been used to explore CHAs is pediatrics. A mail survey sent to a random sample of fellows from the American Academy of Pediatricians explored willingness to refer patients to CHAs [11] and found the most commonly referred CHAs were biofeedback (52.5%), massage therapy (39.0%), acupuncture/acupressure (34.0%), yoga/meditation (32.0%), hypnosis (29.0%), and chiropractic (25.0%). Rank ordering for pediatricians' recommendations of CHAs in this study yields a somewhat different pattern, with the most commonly recommended CHAs being herbs/nonvitamin supplements (27.2%), massage therapy (22.8%), and chiropractic/osteopathic manipulation (20.9%), and acupuncture as the least commonly recommended (13.1%). However, these differences are likely due to methodological differences between the studies, including question wording. For example, Sawni and Thomas [11] asked about North American and Chinese herbs, whereas this study asked about herbs/nonvitamin supplements (including probiotics).
Furthermore, other differences exist (e.g., mode of administration, sampling procedures). The relatively low recommendation rates by pediatricians for CHAs in this study may be due to lower rates of health conditions in children. [33] For instance, using NAMCS data, investigators have found that routine or preventive visits are the most frequent reason that children see office-based physicians. [34] However, CHA use is higher among children with cancer, [35] mental health issues, [36] and musculoskeletal conditions. [37]
The current findings add to the literature by showing physician-based national estimates regarding sex differences in recommendations of CHA. Female physicians recommended CHAs at a higher rate than male physicians (63.2% vs. 49.3%, respectively), with this difference remaining even when controlling for additional characteristics. Furthermore, female physicians were approximately twice as likely to recommend each individual therapy, except chiropractic/osteopathic manipulation. These findings confirm and expand upon prior studies that found female physicians more likely to talk to patients about CHAs [9] or recommend CHAs. [8] Likely related to female physician recommendations is the fact previous studies have consistently found higher usage rates of CHAs among U.S. women than among men, [5, 6] and likewise found physicians who report personal usage of CHAs more likely to recommend CHAs to patients. [8, 15] Furthermore, previous research has found that U.S. health care workers, and, in particular, health care providers, are more likely to use CHAs than workers in other occupations. [38] Given the rising rate of female physicians in the United States, [39] there is reason to expect that recommendations for CHAs will increase over time.
This study also found increasing age was associated with lower rates of recommendations for yoga and massage therapy for physicians ≥65 years. Several studies have found younger physicians more likely to refer their patients for CHAs, [12, 40] use CHAs in their practices, [16, 41] or have positive attitudes toward CHAs. [23, 42, 43] Possible reasons why younger physicians may be more likely to recommend CHAs are the incorporation of CHAs into the curricula of U.S. medical schools, [44] and a higher percentage of older physicians being male. [45]
The current finding that DOs are more likely than MDs to recommend any CHA, massage therapy, and chiropractic/osteopathic manipulation is consistent with previous research. Berman et al. [14] found DOs more likely than MDs to use several CHAs including massage, acupressure, chiropractic, herbal medicines, homeopathy, and megavitamins. Another study found referral rates by DOs for acupuncture, biofeedback, and massage therapy were >40%. [9] That DOs are more likely than MDs to recommend chiropractic/osteopathic manipulation is not surprising given osteopathic manipulation is a key feature of the osteopathic profession. [24] In addition, a holistic approach to medicine is a key difference between osteopathic and allopathic doctors. [9, 24] Finally, the finding that physicians practicing in the West were more likely to recommend every CHA than physicians practicing in the South is consistent with previous national data on usage in the general population. [5, 6, 46] For instance, in 2015 the state with the largest number of acupuncturists was California. [38] Another study found low concentration of chiropractors in the South compared with other regions. [47]
As with any study, this study has limitations. The scope of data analyzed includes only nonfederal office-based physicians. Physicians in hospitals, jails, prisons, Veterans Affairs' medical facilities, and other nonoffice-based locations are not included. Owing to small cell sizes, estimates for some individual therapies, specialties, and physician/practice characteristics cannot be presented. In addition, the types of physician specialties surveyed and the specificity of groups were limited. For example, the authors were unable to look at rheumatologists as a separate group, even though pain is important in rheumatic diseases [48] and CHAs are commonly used for pain conditions. [5] Furthermore, data do not tell us the number of patients for whom physicians recommended CHAs, nor the specific demographics of the patients to whom they are recommended. Multiple comparisons without adjustment were made in this study, which could increase the possibility of type I error. Finally, the 2012 NAMCS PII data were used as these are (to the authors' knowledge) the only nationally representative data available for examining CHA recommendations by physicians; however, there is a possibility the percentages of physicians making CHA recommendations have changed since this time. Despite these limitations, this study is the first in over a decade to examine physician recommendations across specialties using a national sample, and the first in the literature to use a large probability sample of office-based physicians.
Conclusions
This study analyses show that physicians often recommend CHAs, with 53.1% of office-based U.S. physicians recommending at least one to their patients in the past 12 months. Recommendation rates were higher among female physicians than among male physicians and varied by medical specialty. General/family practitioners and internists recommended CHAs at higher rates than pediatricians, and more than half of psychiatrists recommended mind–body therapies, compared with <30% of physicians from other specialties. Understanding practice patterns of U.S. physicians related to recommendations for CHAs, and their differences across medical specialties and physician sex, could inform consumers, physicians, and medical schools.
Supplementary Material
Supplementary Table S1 (27K, pdf)
Supplementary Table S2 (30K, pdf)
Supplementary Table S3 (40K, pdf)Disclaimer Statement
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Center for Health Statistics or the Centers for Disease Control and Prevention.
Author Disclosure Statement
No competing financial interests exist.
Funding Statement
All employees were employed by the U.S. Federal Government. No additional funding was provided.
References:
National Center for Complementary and Integrative Health.
Strategic Plan
NIH Publication No. 16-AT-7643 D504; June 2016Clarke TC, Barnes PM, Black LI, et al..
Use of yoga, meditation, and chiropractors among
U.S. adults aged 18 and over.
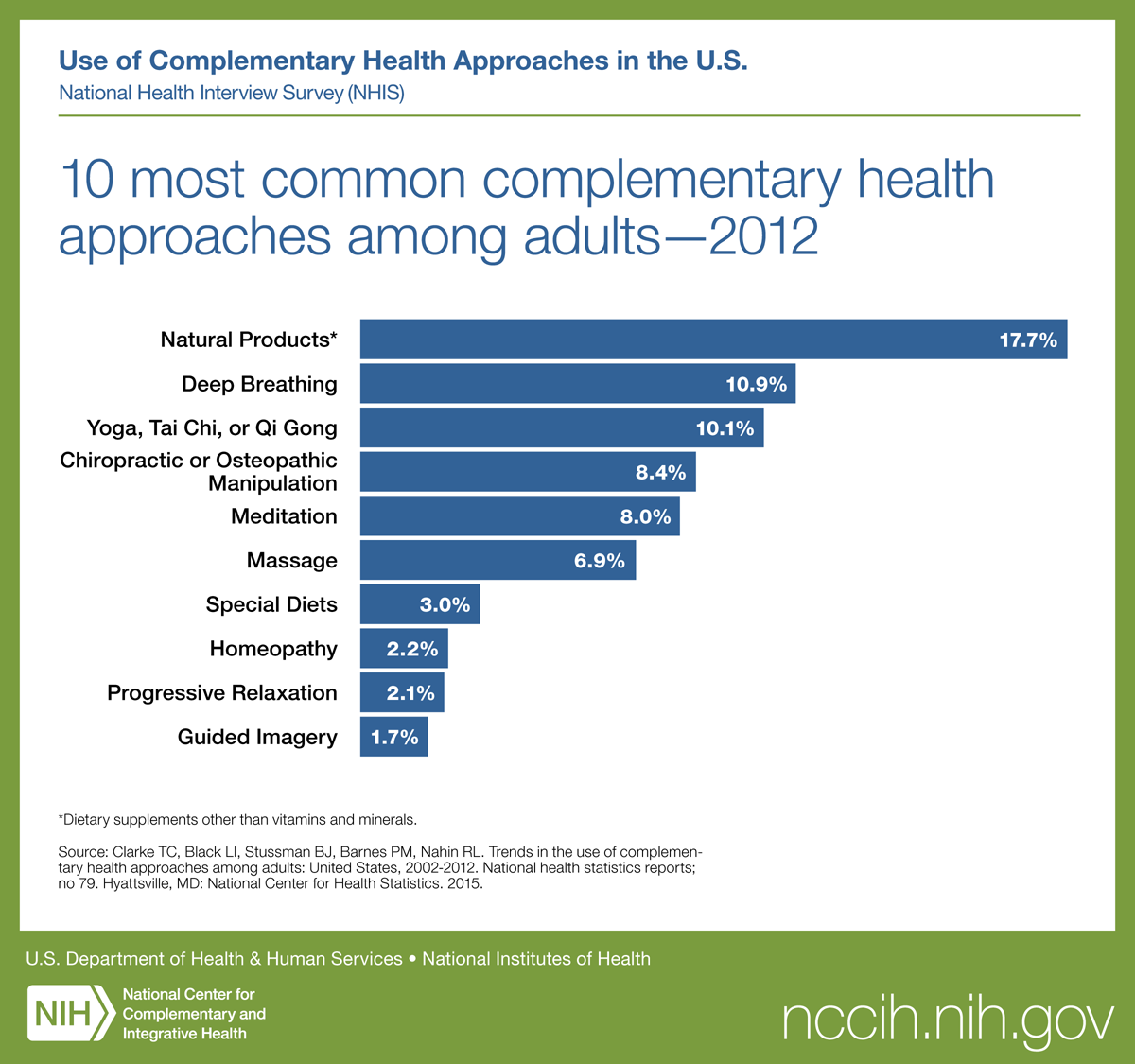
NCHS Data Brief 2018:1–8Clarke TC, Black LI, Stussman BJ, et al..
Trends in the Use of Complementary Health Approaches Among Adults:
United States, 2002-2012
National Health Statistics Report 2015 (Feb 10); (78): 1–16Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC.
Trends in Alternative Medicine Use in the United States, 1990 to 1997:
Results of a Follow-up National Survey
JAMA 1998 (Nov 11); 280 (18): 1569–1575Barnes PM , Powell-Griner E , McFann K , Nahin RL:
Complementary and Alternative Medicine Use Among Adults:
United States, 2002
Advance Data 2004 (May 27); 343: 1–19Barnes PM , Bloom B , Nahin RL:
Complementary and Alternative Medicine Use Among Adults and Children:
United States, 2007
National Health Statistics Report 2008 (Dec); 12: 1-24Manek NJ, Crowson CS, Ottenberg AL, et al..
What rheumatologists in the United States think of complementary
and alternative medicine: Results of a national survey.
BMC Complement Altern Med 2010;10:5.Sierpina V, Levine R, Astin J, Tan A.
Use of mind-body therapies in psychiatry and family medicine faculty
and residents: Attitudes, barriers, and gender differences.
Explore (NY) 2007;3:129–135Kurtz ME, Nolan RB, Rittinger WJ.
Primary care physicians' attitudes and practices
regarding complementary and alternative medicine.
J Am Osteopath Assoc 2003;103:597–602Rhode JM, Patel DA, Sen A, et al..
Perception and use of complementary and alternative
medicine among gynecologic oncology care providers.
Int J Gynaecol Obstet 2008;103:111–115Sawni A, Thomas R.
Pediatricians' attitudes, experience and referral patterns regarding
Complementary/Alternative Medicine: A national survey.
BMC Complement Altern Med 2007;7:18.Berman BM, Bausell RB, Lee WL.
Use and referral patterns for 22 complementary and alternative medical therapies
by members of the American College of Rheumatology: Results of a national survey.
Arch Intern Med 2002;162:766–770Kemper KJ, O'Connor KG.
Pediatricians' recommendations for complementary and
alternative medical (CAM) therapies.
Ambul Pediatr 2004;4:482–487Berman BM, Singh BB, Hartnoll SM, et al..
Primary care physicians and complementary-alternative medicine:
Training, attitudes, and practice patterns.
J Am Board Fam Pract 1998;11:272–281Kundu A, Tassone RF, Jimenez N, et al..
Attitudes, patterns of recommendation, and communication of pediatric
providers about complementary and alternative medicine
in a large metropolitan children's hospital.
Clin Pediatr (Phila) 2011;50:153–158Chan PS, Wong MM.
Physicians and complementary-alternative medicine:
Training, attitudes, and practices in Hawaii.
Hawaii Med J 2004;63:176–181Greene BR, Smith M, Allareddy V, Haas M.
Referral patterns and attitudes of primary care physicians towards chiropractors.
BMC Complement Altern Med 2006;6:5.Zodet MW, Stevans JM.
The 2008 prevalence of chiropractic use in the US adult population.
J Manipulative Physiol Ther 2012;35:580–588Stevans JM, Zodet MW.
Clinical, demographic, and geographic determinants of variation in
chiropractic episodes of care for adults using the
2005–2008 Medical Expenditure Panel Survey.
J Manipulative Physiol Ther 2012;35:589–599Berman BM, Singh BK, Lao L, Singh BB, Ferentz KS, Hartnoll SM.
Physicians' Attitudes Toward Complementary
or Alternative Medicine: A Regional Survey
J Am Board Fam Pract 1995 (Sep); 8 (5): 361-366National Center for Health Statistics.
2012 NAMCS Mirco-Data File Documentation.
Hyattsvile, MD: National Center for Health Statistics, 2015Hing E, Shimizu IM, Talwalkar A.
Nonresponse bias in estimates from the 2012 National Ambulatory Medical Care Survey.
Vital Health Stat 2016;2:1–42Sikand A, Laken M.
Pediatricians' experience with and attitudes toward
complementary/alternative medicine.
Arch Pediatr Adolesc Med 1998;152:1059–1064Johnson SM, Kurtz ME.
Perceptions of philosophic and practice differences between
US osteopathic physicians and their allopathic counterparts.
Soc Sci Med 2002;55:2141–2148Parker JD, Talih M, Malec D, et al..
National Center for Health Statistics data presentation standards for proportions.
Vital Health Stat 2017;2:1–14Nahin RL, Boineau R, Khalsa PS, et al..
Evidence-Based Evaluation of Complementary Health
Approaches for Pain Management in the United States
Mayo Clin Proc. 2016 (Sep); 91 (9): 1292–1306Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Nahin RL, Barnes PM, Stussman BJ.
Insurance Coverage for Complementary Health Approaches
Among Adult Users: United States, 2002 and 2012
NCHS Data Brief 2016 (Jan): 234: 1–8Heyward J, Jones CM, Compton WM, et al.
Coverage of Nonpharmacologic Treatments for Low Back Pain
Among US Public and Private Insurers
JAMA Network Open 2018 (Oct 5); 1 (6): e183044Boyd JE, Lanius RA, McKinnon MC.
Mindfulness-based treatments for posttraumatic stress disorder:
A review of the treatment literature and neurobiological evidence.
J Psychiatry Neurosci 2018;43:7–25. Review.Hofmann SG, Gómez AF.
Mindfulness-based interventions for anxiety and depression.
Psychiatr Clin North Am 2017;40:739–749Black, LI, Clarke, TC, Barnes, PM, Stussman, BJ, and Nahin, RL.
Use of Complementary Health Approaches Among Children Aged
4–17 Years in the United States: National Health
Interview Survey, 2007–2012
National Health Statistics Report 2015 (Feb 10); (78): 1–19Department of Health and Human Services.
Healthy People 2020: Objectives for Improving Health
Washington, DC.Valderas JM, Starfield B, Forrest CB, et al..
Routine care provided by specialists to children and
adolescents in the United States (2002–2006).
BMC Health Serv Res 2009;9:221.Bishop FL, Prescott P, Chan YK, et al..
Prevalence of complementary medicine use in pediatric cancer:
A systematic review.
Pediatrics 2010;125:768–776Wang C, Preisser J, Chung Y, Li K.
Complementary and alternative medicine use among children with mental health issues:
Results from the National Health Interview Survey.
BMC Complement Altern Med 2018;18:241.Cohen EM, Dossett ML, Mehta DH, et al..
Factors associated with complementary medicine use in pediatric
musculoskeletal conditions: Results from a national survey.
Complement Ther Med 2017;31:53–58Johnson PJ, Ward A, Knutson L, Sendelbach S.
Personal use of complementary and alternative medicine (CAM) by U.S. health care workers.
Health Serv Res 2012;47(1 Pt 1):211–227Young A, Chaudhry HJ, Thomas JV, Dugan M.
A census of actively licensed physicians in the United States, 2012.
J Med Regul 2013;99:11–24Wahner-Roedler DL, Lee MC, Chon TY, et al..
Physicians' attitudes toward complementary and alternative medicine
and their knowledge of specific therapies: 8-year follow-up
at an academic medical center.
Complement Ther Clin Pract 2014;20:54–60Fan AY, Faggert S.
Distribution of licensed acupuncturists and educational institutions
in the United States in early 2015.
J Integr Med 2018;16:1–5Milden SP, Stokols D.
Physicians' attitudes and practices regarding complementary and alternative medicine.
Behav Med 2004;30:73–82Furlow ML, Patel DA, Sen A, Liu JR.
Physician and patient attitudes towards complementary and
alternative medicine in obstetrics and gynecology.
BMC Complement Altern Med 2008;8:35.Cowen VS, Cyr V.
Complementary and alternative medicine in US medical schools.
Adv Med Educ Pract 2015;6:113–117Young A, Chaudhry HJ, Xiaomei P, et al..
A Census of Actively Licensed Physicians in the United States, 2014.
J Med Regul 2015;101:7–22Peregoy JA, Clarke TC, Jones LI, et al..
Regional variation in use of complementary health approaches by U.S. adults.
NCHS Data Brief 2014:1–8Davis MA, Mackenzie TA, Coulter ID, et al..
The United States Chiropractic Workforce:
An alternative or complement to primary care?
Chiropr Man Therap 2012;20:35Kazis LE, Meenan RF, Anderson JJ.
Pain in the rheumatic diseases. Investigation of a key health status component.
Arthritis Rheum 1983;26:1017–1022
Return to ALT-MED/CAM ABSTRACTS
1-18-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |